Abstract
Pediatric basilar skull fractures (BSFs) are a rare type of traumatic head injury that can cause debilitating complications without prompt treatment. Here, we sought to review the literature and characterize the clinical features, management, and outcomes of pediatric BSFs. We identified 21 relevant studies, excluding reviews, meta-analyses, and non-English articles. The incidence of pediatric BSFs ranged from 0.0001% to 7.3%, with falls from multi-level heights and traffic accidents being the primary causes (9/21). The median presentation age ranged from 3.2 to 12.8 years, and the mean age of patients across all studies was 8.68 years. Up to 55% of pediatric BSFs presented with intracranial hematoma/hemorrhage, along with pneumocephalus and edema. Cranial nerve palsies were a common complication (9/21), with the facial nerve injured most frequently (7/21). While delayed cranial nerve palsy was reported in a few studies (4/21), most resolved within three months post-admission. Other complications included CSF leaks (10/21) and meningitis (4/21). Management included IV fluids, antiemetics, and surgery (8/21) to treat the fracture directly, address a CSF leak, or achieve cranial nerve compression. Despite their rarity, pediatric skull base fractures are associated with clinical complications, including CSF leaks and cranial nerve palsies. Given that some of these complications may be delayed, patient education is critical.
1. Introduction
Pediatric head trauma is one of the leading causes of disability and death in children and can be caused by motor vehicle accidents, blunt trauma, falls from heights, and child abuse [1,2,3,4]. It has been reported that, in the United States, pediatric traumatic brain injuries result in nearly 60,000 hospitalizations and over 500,000 emergency department visits [5]. Left untreated, pediatric head trauma has the potential to cause lasting complications, including cognitive impairment and long-term neurological deficits [6,7,8].
Skull base fractures, also known as basilar skull fractures (BSF), are a type of traumatic head injury that involves a break in one or more bones of the base of the skull. The skull base forms the floor of the cranial cavity and is composed of five bones: the temporal, occipital, sphenoid, frontal, and ethmoid bones. With high-velocity blunt force, the bones of the skull base can break, leading to substantial complications, such as cerebrospinal fluid (CSF) leakage and cranial nerve palsies [9,10]. While the epidemiology of skull base fractures is not well characterized, it is reported that between 4 and 20% of children with head trauma will suffer from such an injury [11].
Given the relative rarity of pediatric skull base fractures, their clinical features and management have not been well elucidated. Here, we sought to perform a comprehensive review of the current literature to establish the risk factors, complications, and management options for pediatric skull base fractures. Our goal was to consolidate findings regarding the pathology and obtain a clearer understanding of how it can be best managed.
2. Materials and Methods
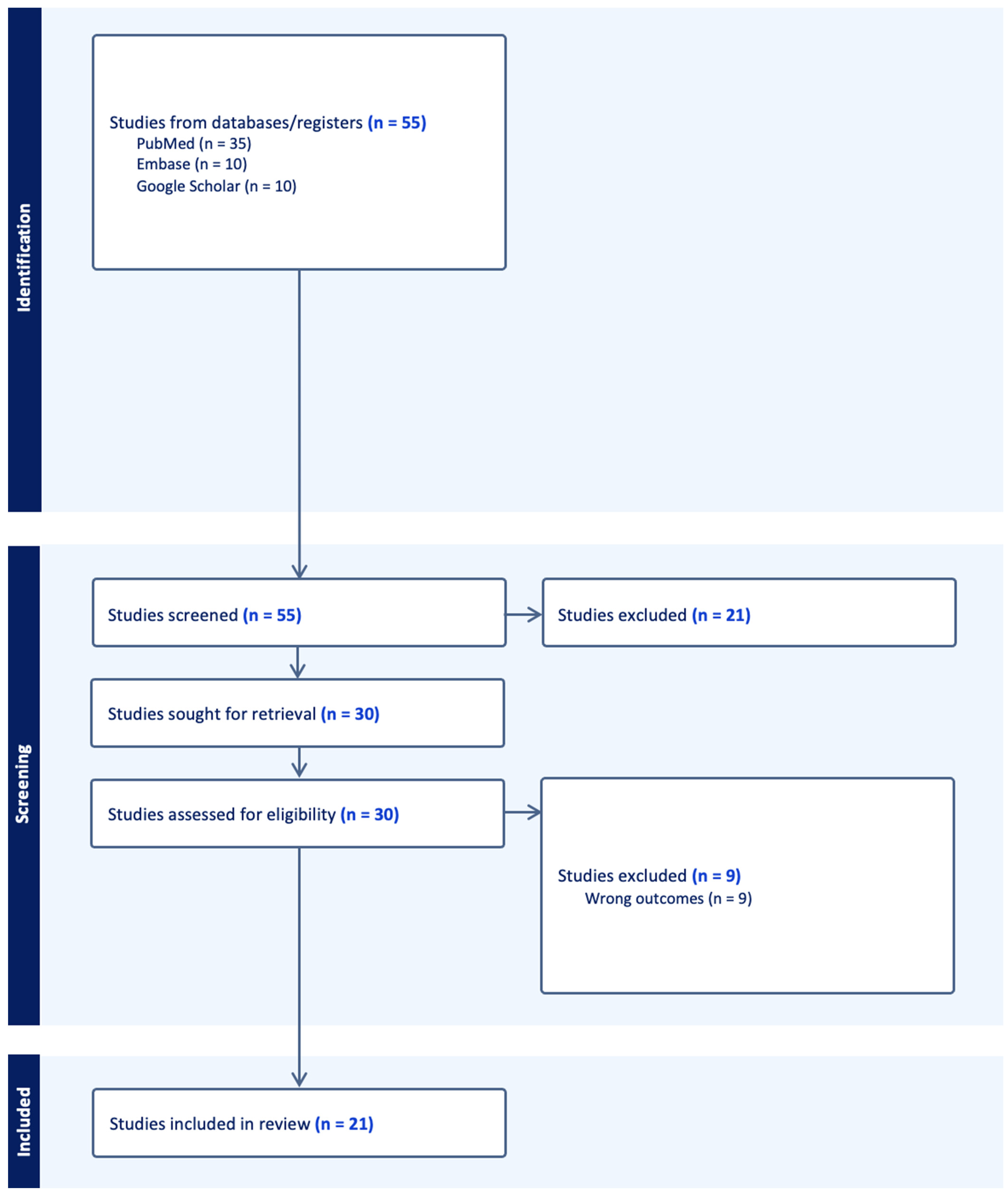
This review followed the criteria for reporting systematic literature reviews and meta-analyses as defined by the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) 2020 statement (Supplementary Materials). An organized literature search was performed on PubMed, Embase, and Google Scholar using the following key words: “pediatric”, “skull fracture”, and “basilar skull fracture”. Selected citations were uploaded into Covidence (Cochrane, London, UK). Relevant studies were also obtained from the reference lists of studies obtained from the literature search. Studies were included if they investigated patients under 18 years of age who experienced trauma to the skull base. Articles not written in English, as well as reviews and/or meta-analyses, were excluded from review. Abstract screening, full-text review, and data extraction were then conducted in accordance with the PRISMA guidelines. Figure 1 illustrates the PRISMA flowchart used to guide the systematic review process.
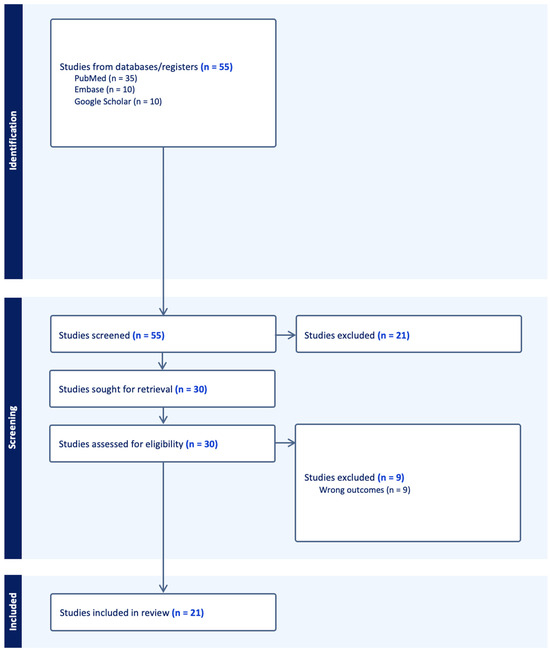
Figure 1.
PRISMA flow diagram of the systematic literature search performed (n = number of studies).
3. Results
A total of 55 studies were obtained from the initial search query. Following abstract screening and full-text review, 21 studies were deemed eligible for data extraction and analysis based on the defined inclusion and exclusion criteria.
Table 1 summarizes the inclusion criteria and demographics of each included study. Approximately 64% of the included patients were male, while 36% of patients were female, as averaged across 12 studies. Four of the 21 studies further stratified their study samples by race, with White and Hispanic patients comprising the majority of the analyzed patients. The median age of patients ranged from 3.2 to 12.8 years, with a mean age of 8.68 years. There was notable variance in the incidence of pediatric basilar skull fractures across the 21 studies, with rates as low as 0.0001% and as high as 7.3%. Grigorian et al. (2019) and Ugalde et al. (2018) noted high incidence rates of basilar skull fractures in patients with evidence of cerebrovascular injury (53.2% and 33.9%, respectively) [12,13].

Table 1.
Study characteristics.
Table 2 outlines the diagnostic findings and criteria utilized by each study to define pediatric skull base fractures. Notable mechanisms of injury were traffic accidents, falls from pre-defined heights, impact from hard objects, and violence, with fall injuries and traffic accidents being noted as the most common causes across nine of the 21 studies. The fracture classification across the 21 studies was highly variable depending on the granularity of the diagnosis. However, temporal bone fractures were reported as the most common in five studies, at rates of approximately 60%, followed by anterior frontal base fractures.

Table 2.
Diagnosis and classification of pediatric BSFs.
The most dominant tool for diagnosis was a CT scan, as reported by 11 of the 21 studies. Four studies supplemented CT scans with plain film and physical exam findings for a more holistic diagnosis. Common physical exam findings reported across the 21 studies included hemotympanum, Battle’s sign, and raccoon eye. Other reported signs were tympanic membrane rupture, epistaxis, altered mental status, loss of consciousness, and scalp hematoma. Eight of the 21 studies noted intracranial hematoma/hemorrhage as the most common concomitant injury observed in pediatric patients with basilar skull fractures, including epidural, subdural, and subarachnoid hemorrhage types. Other observed concomitant injuries included brain contusion, pneumocephalus, and edema.
Table 3 highlights the reported complications associated with pediatric basilar skull fractures, as well as their management and prognosis. Cranial nerve damage was reported as a common complication, with facial nerve palsy reported in seven of the 21 studies. Of the seven studies, four reported the delayed onset of facial nerve palsy following hospital discharge, with full resolution occurring within three months for most cases. Other observed cranial nerve palsies included olfactory, optic, oculomotor, abducens, glossopharyngeal, and vagus. Moreover, 10 of the 21 studies reported findings of a CSF leak via otorrhea or rhinorrhea, while four studies reported the incidence of in-patient or delayed meningitis. The CSF leak rates were approximately 25%, while the meningitis rates were substantially lower at around 1%. Other noted complications included blunt cerebrovascular injury, hearing loss, eye injuries, central diabetes insipidus, and permanent neurological deficits.

Table 3.
Complications and management of pediatric BSFs.
Management was divided into conservative and surgical treatments. Conservative options included IV fluids and antiemetics to stabilize nausea and vomiting, acetazolamide to reduce the intracranial pressure, corticosteroids to treat cranial nerve palsies, and prophylactic antibiotics against meningitis. Surgical treatment was reported in eight of the 21 studies to address the fracture directly or treat complications such as CSF leaks or cranial nerve compression. The average hospital length of stay ranged from 5 to 17 days, with the majority of patients returning to baseline function after 2–3 months. However, approximately 1–5% of patients experienced poor outcomes such as transfer to chronic care facilities and/or a comatose state. Death rates were marginal at approximately 1%, usually in the first week following injury due to massive intracranial hemorrhage.
4. Discussion
Pediatric head trauma is one of the leading causes of disability and death in children and can involve underlying trauma to the skull. While pediatric head trauma and its consequences have been well characterized in the literature, there is a noticeable paucity of information regarding pediatric skull base fractures. Furthermore, there is a high degree of variability in the injury characteristics, complications, and management among the few studies that have examined the topic. As such, this review provides a concise and consolidated summary of pediatric basilar skull fractures to guide management for providers and caretakers.
We found that the incidence of pediatric basilar skull fractures ranged from 0.0001 to 7.3%, with the most common mechanisms of injury being traffic-related accidents and fall injuries. In patients with evidence of cerebrovascular injury, however, the incidence rates were significantly higher (between 33.9% and 53.2%). This could be explained by the anatomical location of the skull base relative to the major cerebrovascular blood supply routes within the cranial cavity. In regard to demographics, male patients had a higher incidence of fracture compared to female patients. While this finding may be attributable to the samples of each study, the relationship between sex and the basilar fracture incidence in children may be a worthwhile investigation.
The fracture classification across the 21 studies was highly variable, but the majority of studies reported temporal bone fractures as the most common fracture pattern in pediatric basilar skull injuries, followed by anterior frontal base fractures. This contrasts with adult basilar skull fractures, where anterior frontal base fractures are reported to be the most common. This difference in presentation in the pediatric population may be explained by anatomical differences in the skull shape and structure. As posited by Leibu et al. (2017), the ratio of the skull to facial volume is 1:8 in children and decreases to 1:2.5 by adulthood, thereby increasing the odds of anterior frontal base fractures and decreasing the odds of temporal bone fractures [20]. Furthermore, the maxillary and frontal sinuses are still in development in children, rendering them particularly susceptible to fracture if subjected to blunt trauma.
While most of the studies included in our analysis reported CT as the primary diagnosis tool, there was notable debate about the efficacy of CT scans versus physical exam findings such as Battle’s sign and raccoon eyes. Yildirim et al. (2005) found that only 26% of the patients in their cohort with positive CT findings of a basilar skull fracture displayed identifiable physical exam findings [31]. They argue that Battle’s sign and raccoon eyes were neither sensitive nor specific to basilar skull fractures, thus making CT the ideal tool for diagnosis. In contrast, Tunik et al. (2016) and Kadish and Schunk (1995) emphasized the importance of physical examination [18,30]. They found that only 50% of pediatric patients with basilar skull fractures had positive findings on the CT scan; thus, a strong physical exam can identify patients who have negative findings on imaging. Regardless of their sensitivity in detecting basilar skull fractures, CT scans still are still vital in pediatric patients presenting with signs and symptoms due to the likelihood of associated intracranial injuries that may not be detected by physical examination alone.
A notable correlation between basilar skull fractures and concomitant intracranial hematoma/hemorrhage was noted in our analysis. Though these findings depend on the severity of the injury, the anatomical proximity of major cerebrovascular routes to the skull base likely predisposes patients to epidural, subdural, or subarachnoid hemorrhages in the event of a skull base fracture. Given that pediatric patients with brain bleeds such as these are at a heightened risk of rapid decompensation and death, CT or MRI is recommended for any child presenting with signs of skull fracture, regardless of the location [27].
CSF leakage via otorrhea or rhinorrhea was a reported complication in 10 of the 21 studies in our analysis. Leibu et al. (2017) reported the usage of continuous drainage for management, with reoperation if necessary for repair [20]. Four studies reported the onset of meningitis as another complication, with all suggesting the infection as a sequela of CSF leakage [20,22,25,27]. Given the high rates of meningitis in adult patients with basilar skull fractures, they recommend administering prophylactic antibiotics to pediatric patients to protect against meningeal manifestations. However, given the low incidence rate of around 1% of meningitis infections that we observed in our review, we question the need for prophylactic antibiotics in pediatric patients presenting with skull base fractures.
Cranial nerve palsies were another commonly reported complication of pediatric skull base fractures, with the facial nerve being the most commonly involved nerve. Injury to the facial nerve is likely due to direct damage to the petrous temporal bone, where the nerve commonly tracks. Of note, four studies reported the delayed onset of facial nerve palsy following discharge [20,22,29,31]. As a result, patients should be educated on the signs and symptoms of facial nerve palsy to ensure prompt follow-up if symptoms manifest. Additionally, a syndrome known as Jugular Foramen syndrome was reported by Toledo-Gotor et al. (2021) and Yildirim et al. (2005) [29,31]. Jugular Foramen syndrome is the paralysis of cranial nerves IX–XI as they pass through the jugular foramen, manifesting as dysphagia, hoarseness, and dizziness. While the syndrome is not extensively discussed in the literature, it is a noteworthy complication that providers should consider when providing discharge counseling for patients and their families.
The treatment of pediatric basilar skull fractures included the conservative medical management of associated symptoms and/or surgical intervention to correct deformities or manage bleeding or leakage. Dunnick et al. (2019) reported acetazolamide usage to manage elevated intracranial pressure [16]. Despite being uncommonly used in pediatric patients, acetazolamide was used due to evidence of papilledema as well as temporary therapeutic relief seen with lumbar puncture. Treatment was started in the hospital and continued after discharge, with symptom resolution reported after 60 days. Liu-Shindo and Hawkins (1989) reported corticosteroid usage to manage cranial nerve palsies; however, corticosteroids in patients with TBI have been associated with negative effects such as the exacerbation of critical illness-related corticosteroid insufficiency [22,32]. However, these effects were often seen with high-dose corticosteroid administration and during the first 24–48 h of TBI. Therefore, in pediatric patients who may present with delayed cranial nerve palsies following discharge, corticosteroid treatment remains a viable treatment option.
Surgical intervention was often indicated for patients with intracranial hemorrhage, a CSF leak, or cranial nerve compression. Craniotomies were performed in patients with elevated intracranial pressure to elevate the depressed fracture fragments compressing the cranium. Leibu et al. (2017) reported surgical drain placement as a treatment for patients with CSF leaks via rhinorrhea [20]. Liu-Shindo and Hawkins (1989) performed facial nerve decompression in several patients to relieve cranial nerve palsies from fracture fragments, as well as frontal sinus obliteration and anterior fossa dura repair to treat CSF rhinorrhea [22].
The present study was not without limitations. First, there was inherent variability across the 21 studies in regard to the study design, sample patient population, and outcome measurements. The reported outcomes varied from paper to paper, as some studies did not include variables such as the fracture classification, management, or prognosis. Lastly, there were limitations attached to the study’s search strategy; some relevant studies could have been excluded due to the omission of certain terms in our preliminary search.
Overall, the studies in this review outline the etiology, manifestations, and complications associated with pediatric skull base fractures. Despite their relative rarity, pediatric skull base fractures are associated with significant clinical complications, including CSF leaks and cranial nerve palsies. Our clinical recommendations regarding management include a thorough physical examination alongside rapid imaging to confirm the diagnosis, as well as patient education on delayed cranial nerve palsies that can manifest after discharge.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/children11050564/s1, Table S1: PRISMA 2020 Checklist. Reference [33] are cited in the Supplementary Materials.
Author Contributions
Conceptualization: G.J., J.X. and A.J.K.; methodology: G.J., J.X. and A.J.K.; writing—original draft preparation: G.J., J.X., H.R., M.G., M.K., E.B.-W., T.K., R.F., A.P. and P.S.; writing—review and editing: all authors; supervision: A.J.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Garcia-Rodriguez, J.A.; Thomas, R.E. Office management of mild head injury in children and adolescents. Can. Fam. Physician 2014, 60, 523–531.e294–e303. [Google Scholar]
- Geyer, K.; Meller, K.; Kulpan, C.; Mowery, B.D. Traumatic brain injury in children: Acute care management. Pediatr. Nurs. 2013, 39, 283–289. [Google Scholar]
- Alexiou, G.A.; Sfakianos, G.; Prodromou, N. Pediatric head trauma. J. Emerg. Trauma Shock 2011, 4, 403–408. [Google Scholar] [CrossRef]
- Adirim, T.A.; Wright, J.L.; Lee, E.; Lomax, T.A.; Chamberlain, J.M. Injury surveillance in a pediatric emergency department. Am. J. Emerg. Med. 1999, 17, 499–503. [Google Scholar] [CrossRef]
- Chen, C.; Peng, J.; Sribnick, E.A.; Zhu, M.; Xiang, H. Trend of Age-Adjusted Rates of Pediatric Traumatic Brain Injury in U.S. Emergency Departments from 2006 to 2013. Int. J. Environ. Res. Public Health 2018, 15, 1171. [Google Scholar]
- Araki, T.; Yokota, H.; Morita, A. Pediatric Traumatic Brain Injury: Characteristic Features, Diagnosis, and Management. Neurol. Med. Chir. 2017, 57, 82–93. [Google Scholar] [CrossRef]
- Elsamadicy, A.A.; Koo, A.B.; David, W.B.; Lee, V.; Zogg, C.K.; Kundishora, A.J.; Hong, C.; Reeves, B.C.; Sarkozy, M.; Kahle, K.T.; et al. Post-traumatic seizures following pediatric traumatic brain injury. Clin. Neurol. Neurosurg. 2021, 203, 106556. [Google Scholar] [CrossRef]
- Chadwick, L.; Roth, E.; Minich, N.M.; Taylor, H.G.; Bigler, E.D.; Cohen, D.M.; Bacevice, A.; Mihalov, L.K.; Bangert, B.A.; Zumberge, N.A.; et al. Cognitive Outcomes in Children with Mild Traumatic Brain Injury: An Examination Using the National Institutes of Health Toolbox Cognition Battery. J. Neurotrauma 2021, 38, 2590–2599. [Google Scholar] [CrossRef]
- Baugnon, K.L.; Hudgins, P.A. Skull base fractures and their complications. Neuroimaging Clin. N. Am. 2014, 24, 439–465. [Google Scholar] [CrossRef] [PubMed]
- Wamkpah, N.S.; Kallogjeri, D.; Snyder-Warwick, A.K.; Buss, J.L.; Durakovic, N. Incidence and Management of Facial Paralysis After Skull Base Trauma, an Administrative Database Study. Otol. Neurotol. 2022, 43, e1180–e1186. [Google Scholar] [CrossRef]
- Astafyeva, L.; Sidneva, Y.; Badmaeva, I.; Kalinin, P.; Latyshev, S.; Marshintsev, A. Permanent central diabetes insipidus after traumatic brain injury. Case report and literature review. Zhurnal Vopr. Neirokhirurgii Imeni N. N. Burdenko 2022, 86, 112–118. [Google Scholar] [CrossRef]
- Grigorian, A.; Dolich, M.; Lekawa, M.; Fujitani, R.M.; Kabutey, N.-K.; Kuza, C.M.; Bashir, R.; Nahmias, J.M. Analysis of blunt cerebrovascular injury in pediatric trauma. J. Trauma Acute Care Surg. 2019, 87, 1354–1359. [Google Scholar] [CrossRef] [PubMed]
- Ugalde, I.T.; Claiborne, M.K.; Cardenas-Turanzas, M.; Shah, M.N.; Langabeer, J.R., 2nd; Patel, R. Risk Factors in Pediatric Blunt Cervical Vascular Injury and Significance of Seatbelt Sign. West. J. Emerg. Med. 2018, 19, 961–969. [Google Scholar] [CrossRef]
- Barba, P.; Stramiello, J.A.; Nardone, Z.; Walsh-Blackmore, S.; Nation, J.; Ignacio, R.; Magit, A. Pediatric basilar skull fractures from multi-level falls: A systematic review and retrospective analysis. Int. J. Pediatr. Otorhinolaryngol. 2022, 162, 111291. [Google Scholar] [CrossRef] [PubMed]
- Bressan, S.; Eapen, N.; Phillips, N.; Gilhotra, Y.; Kochar, A.; Dalton, S.; Cheek, J.A.; Furyk, J.; Neutze, J.; Williams, A.; et al. PECARN algorithms for minor head trauma: Risk stratification estimates from a prospective PREDICT cohort study. Acad. Emerg. Med. 2021, 28, 1124–1133. [Google Scholar] [CrossRef]
- Dunnick, J.; Gesteland, P. Isolated Increased Intracranial Pressure and Unilateral Papilledema in an Infant with Traumatic Brain Injury and Nondepressed Basilar Skull Fracture. Pediatr. Emerg. Care 2019, 35, e198–e200. [Google Scholar] [CrossRef]
- Garcia, T.A.; McGetrick, B.A.; Janik, J.S. Spectrum of ocular injuries in children with major trauma. J. Trauma 2005, 59, 169–174. [Google Scholar] [CrossRef]
- Kadish, H.A.; Schunk, J.E. Pediatric basilar skull fracture: Do children with normal neurologic findings and no intracranial injury require hospitalization? Ann. Emerg. Med. 1995, 26, 37–41. [Google Scholar] [CrossRef]
- Kopelman, T.R.; Berardoni, N.E.; O’Neill, P.J.; Hedayati, P.; Vail, S.J.; Pieri, P.G.; Feiz-Erfan, I.; Pressman, M.A. Risk factors for blunt cerebrovascular injury in children: Do they mimic those seen in adults? J. Trauma 2011, 71, 559–564, 559–564; discussion 564. [Google Scholar] [CrossRef]
- Leibu, S.; Rosenthal, G.; Shoshan, Y.; Benifla, M. Clinical Significance of Long-Term Follow-Up of Children with Posttraumatic Skull Base Fracture. World Neurosurg. 2017, 103, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Leraas, H.J.; Kuchibhatla, M.; Nag, U.P.; Kim, J.; Ezekian, B.; Reed, C.R.; Rice, H.E.; Tracy, E.T.; Adibe, O.O. Cervical seatbelt sign is not associated with blunt cerebrovascular injury in children: A review of the national trauma databank. Am. J. Surg. 2019, 218, 100–105. [Google Scholar] [CrossRef]
- Liu-Shindo, M.; Hawkins, D.B. Basilar skull fractures in children. Int. J. Pediatr. Otorhinolaryngol. 1989, 17, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Magit, A.; Stramiello, J.A.; Good, R.; Nation, J. Pediatric Basilar Skull Fracture Mechanisms and Trends from 2007 to 2018. Otolaryngol. Head Neck Surg. 2021, 164, 1307–1313. [Google Scholar] [CrossRef]
- Mallicote, M.U.; Isani, M.A.; Golden, J.; Ford, H.R.; Upperman, J.S.; Gayer, C.P. Screening for blunt cerebrovascular injuries in pediatric trauma patients. J. Pediatr. Surg. 2019, 54, 1861–1865. [Google Scholar] [CrossRef] [PubMed]
- McCutcheon, B.A.; Orosco, R.K.; Chang, D.C.; Salazar, F.R.; Talamini, M.A.; Maturo, S.; Magit, A. Outcomes of isolated basilar skull fracture: Readmission, meningitis, and cerebrospinal fluid leak. Otolaryngol. Head Neck Surg. 2013, 149, 931–939. [Google Scholar] [CrossRef]
- Perheentupa, U.; Kinnunen, I.; Grénman, R.; Aitasalo, K.; Karhu, J.O.; Mäkitie, A.A. Post-traumatic morbidity is frequent in children with frontobasilar fractures. Int. J. Pediatr. Otorhinolaryngol. 2012, 76, 670–674. [Google Scholar] [CrossRef] [PubMed]
- Perheentupa, U.; Kinnunen, I.; Grénman, R.; Aitasalo, K.; Mäkitie, A.A. Management and outcome of pediatric skull base fractures. Int. J. Pediatr. Otorhinolaryngol. 2010, 74, 1245–1250. [Google Scholar] [CrossRef] [PubMed]
- Ryan, S.; Hewes, H.; Fenton, S.F.; Russell, K.; Hansen, K.; Brockmeyer, D.L.; Robison, J. Ten-Year Analysis of Complications Related to Simple Basilar Skull Fractures in Children Presenting to a Trauma Center. Pediatr. Emerg. Care 2024, 40, 137–140. [Google Scholar] [CrossRef] [PubMed]
- Toledo-Gotor, C.; Gorría, N.; Oscoz, M.; Llano, K.; Rodríguez-de la Fuente, P.; Aguilera-Albesa, S. Posttraumatic Delayed Jugular Foramen Syndrome in a Toddler. Neuropediatrics 2021, 52, 403–405. [Google Scholar] [CrossRef] [PubMed]
- Tunik, M.G.; Powell, E.C.; Mahajan, P.; Schunk, J.E.; Jacobs, E.; Miskin, M.; Zuspan, S.J.; Wootton-Gorges, S.; Atabaki, S.M.; Hoyle, J.D.; et al. Clinical Presentations and Outcomes of Children with Basilar Skull Fractures After Blunt Head Trauma. Ann. Emerg. Med. 2016, 68, 431–440.e1. [Google Scholar] [CrossRef]
- Yildirim, A.; Gurelik, M.; Gumus, C.; Kunt, T. Fracture of skull base with delayed multiple cranial nerve palsies. Pediatr. Emerg. Care 2005, 21, 440–442. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Zhao, Z.; Zhou, Y.; Chen, X.; Li, Y.; Liu, X.; Lu, H.; Zhang, Y.; Zhang, J. High-dose glucocorticoid aggravates TBI-associated corticosteroid insufficiency by inducing hypothalamic neuronal apoptosis. Brain Res. 2013, 1541, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).