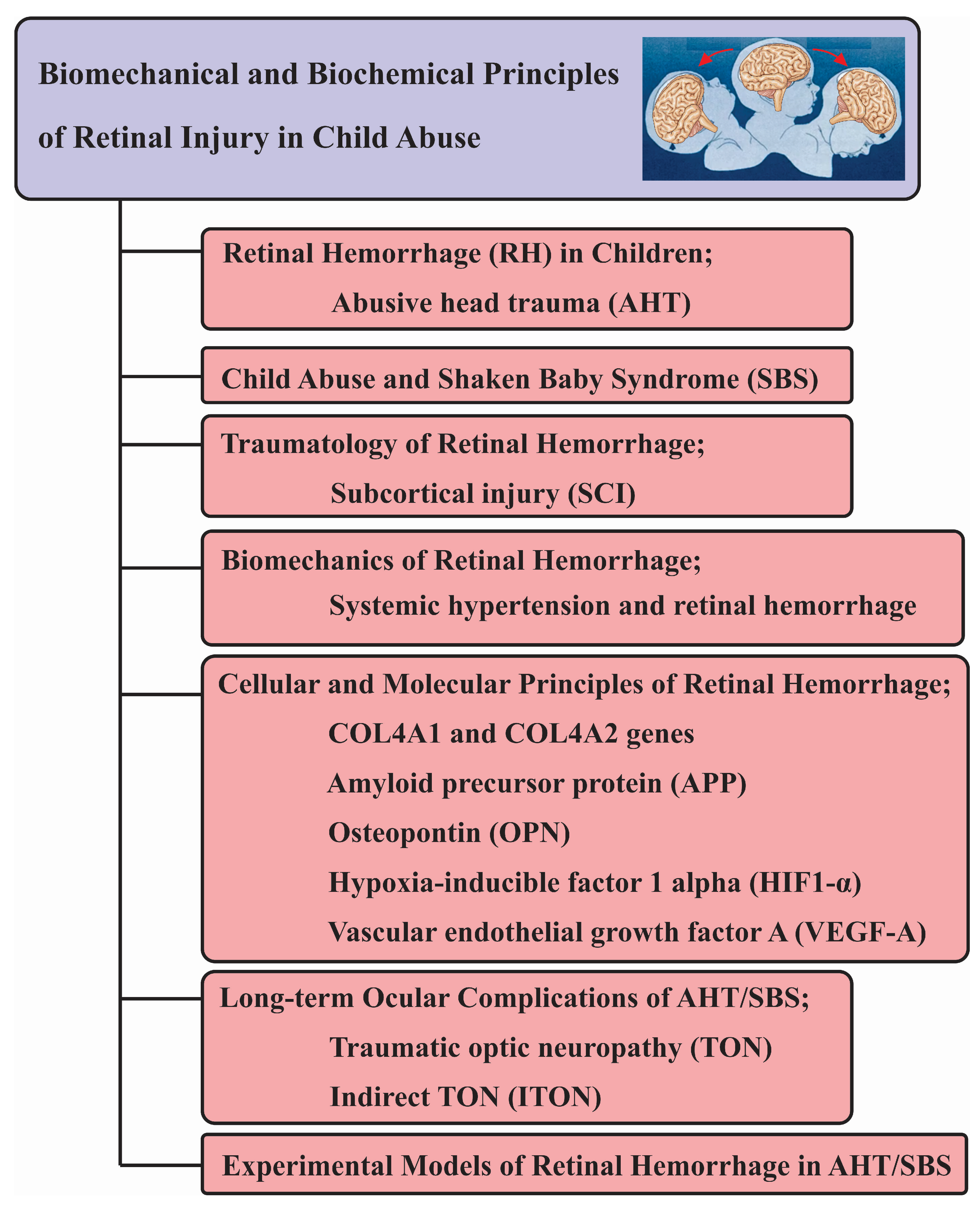
An Update to Biomechanical and Biochemical Principles of Retinal Injury in Child Abuse
Abstract
1. Abusive Head Trauma and Shaken Baby Syndrome
- Damage to the contents of the skull or intracranial region in infants or children under the age of 5, commonly caused by forceful shaking or blunt impact.
- The Centers for Disease Control and Prevention (CDC) and the American Academy of Pediatrics advise adopting the term “abusive head trauma” to encompass injuries arising from various conditions, such as shaking, blunt impact, suffocation, and strangulation.
- “Injuries resulting from dropping and throwing a child are also considered within the category of “abusive head trauma”. The term refers to the nature of the injury rather than the specific mechanism”.
- The legal implications of “abusive head injury” are tied to the precise method of harm inflicted. Diagnosing a child with “shaken baby syndrome” can limit the admissibility of evidence related to alternative injuries, potentially complicating legal proceedings. The majority of abusive head trauma cases are typically under a year old, frequently falling within the age range of 3 to 8 months. However, these injuries can extend to children up to 5 years of age.
- Abusive head trauma stands as the leading cause of fatality and impairment in infants and young children affected by child abuse. Child abuse has been pinpointed as the predominant cause of brain injuries in one-fourth of children aged two and older.
- Abusive head trauma characterized by a distinct pattern of injuries may manifest with retinal hemorrhages and consistent patterns of brain injury. Additionally, fractures of ribs and the ends of long bones are commonly observed.
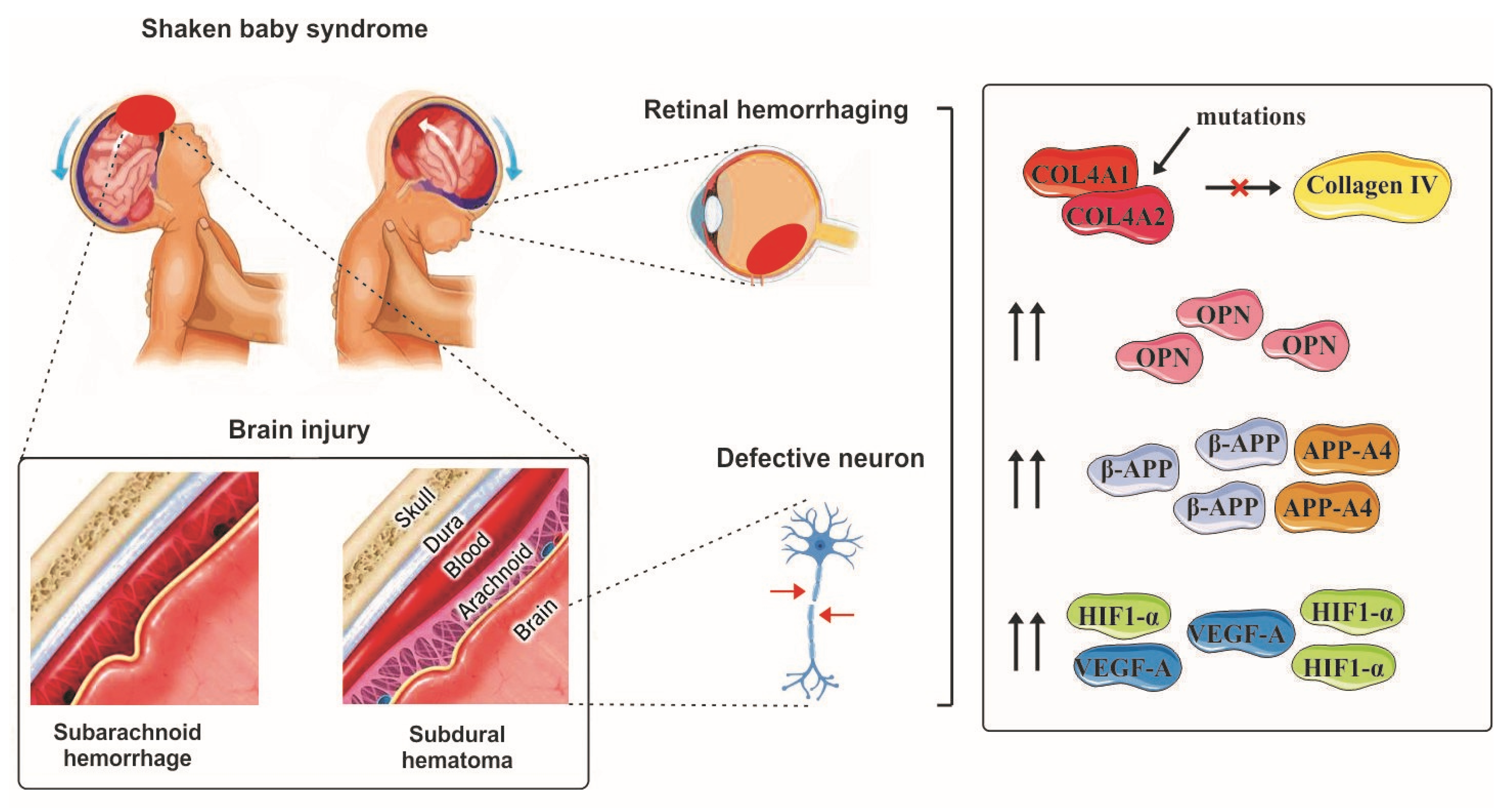
- The term “shaken baby syndrome” is employed to characterize symptoms of brain injury that align with the forceful shaking of an infant or small child. These injuries typically involve unilateral or bilateral subdural hemorrhage, bilateral retinal hemorrhages, and diffuse brain injury. Although children can sustain injuries from shaking alone, there is frequently accompanying evidence of blunt trauma. Therefore, a more comprehensive term, “shaken impact syndrome”, may be utilized to encompass both shaking and associated blunt trauma.
- The SBS triad comprises encephalopathy accompanied by a subdural hematoma and retinal hemorrhage. However, the diagnosis of pediatric abusive head trauma requires a comprehensive medical examination and thorough testing. Relying solely on the presence of these three findings is not sufficient for an accurate diagnosis.
2. Retinal Hemorrhage in Children
3. Retinal Hemorrhage in Abusive vs. Non-Abusive Head Trauma
4. Shaken Baby Syndrome from the Ophthalmologists’ Perspective
5. Links between Intracranial Injury and Retinal Injury in Infantile AHT
6. Biomechanics of Retinal Hemorrhage
7. Ocular Hypertension and Retinal Hemorrhage
8. Cellular and Molecular Markers of Retinal Hemorrhage
9. Long-Term Ocular Complications of AHT/SBS
10. Less Explored Risk Factors of Retinal Hemorrhage in the Context of AHT
11. Experimental Models of Retinal Hemorrhage in AHT/SBS
12. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thau, A.; Saffren, B.; Zakrzewski, H.; Anderst, J.D.; Carpenter, S.L.; Levin, A. Retinal Hemorrhage and Bleeding Disorders in Children: A Review. Child Abus. Negl. 2021, 112, 104901. [Google Scholar] [CrossRef] [PubMed]
- Chhablani, P.P.; Ambiya, V.; Nair, A.G.; Bondalapati, S.; Chhablani, J. Retinal Findings on OCT in Systemic Conditions. Semin. Ophthalmol. 2018, 33, 525–546. [Google Scholar] [CrossRef] [PubMed]
- Saunders, D.; Raissaki, M.; Servaes, S.; Adamsbaum, C.; Choudhary, A.K.; Moreno, J.A.; van Rijn, R.R.; Offiah, A.C. Throwing the Baby out with the Bath Water—Response to the Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU) Report on Traumatic Shaking. Pediatr. Radiol. 2017, 47, 1386–1389. [Google Scholar] [CrossRef] [PubMed]
- Giannakakos, V.P.; Dosakayala, N.; Huang, D.; Yazdanyar, A. Predictive Value of Non-Ocular Findings for Retinal Haemorrhage in Children Evaluated for Non-Accidental Trauma. Acta Ophthalmol. 2022, 100, 312–321. [Google Scholar] [CrossRef] [PubMed]
- Su, M.; Taylor, K.; Stoutin, J.; Shaver, C.; Recko, M. Evidence-Based Screening to Optimize the Yield of Positive Ophthalmologic Examinations in Children Evaluated for Suspected Child Abuse. J. Pediatr. Ophthalmol. Strabismus 2022, 59, 310–319. [Google Scholar] [CrossRef] [PubMed]
- Vaslow, D.F. Chronic Subdural Hemorrhage Predisposes to Development of Cerebral Venous Thrombosis and Associated Retinal Hemorrhages and Subdural Rebleeds in Infants. Neuroradiol. J. 2022, 35, 53–66. [Google Scholar] [CrossRef] [PubMed]
- Thiblin, I.; Andersson, J.; Wester, K.; Högberg, G.; Högberg, U. Retinal Haemorrhage in Infants Investigated for Suspected Maltreatment Is Strongly Correlated with Intracranial Pathology. Acta Paediatr. Int. J. Paediatr. 2022, 111, 800–808. [Google Scholar] [CrossRef] [PubMed]
- Wood, E.H.; Capone, A.; Drenser, K.A.; Berrocal, A.; Hubbard, G.B.; Callaway, N.F.; Kychenthal, A.; Ells, A.; Harper, C.A.; Besirli, C.G.; et al. Referable Macular Hemorrhage-A Clinically Meaningful Screening Target in Newborn Infants. Position Statement of the Association of Pediatric Retina Surgeons. Ophthalmic Surg. Lasers Imaging Retin. 2022, 53, 3–6. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Hu, R.; Chen, J.; Lu, Y.; Guo, Y.; Liu, Y.; Yu, R.; Jin, G. Prevalence, Characteristics, and Risk Factors of Retinal Hemorrhage among Full-Term Neonates in Southern China. Int. J. Environ. Res. Public Health 2022, 19, 13927. [Google Scholar] [CrossRef]
- Shah, Y.S.; Iftikhar, M.; Justin, G.A.; Canner, J.K.; Woreta, F.A. A National Analysis of Ophthalmic Features and Mortality in Abusive Head Trauma. JAMA Ophthalmol. 2022, 140, 227–234. [Google Scholar] [CrossRef]
- Maguire, S.A.; Watts, P.O.; Shaw, A.D.; Holden, S.; Taylor, R.H.; Watkins, W.J.; Mann, M.K.; Tempest, V.; Kemp, A.M. Retinal Haemorrhages and Related Findings in Abusive and Non-Abusive Head Trauma: A Systematic Review. Eye 2013, 27, 28–36. [Google Scholar] [CrossRef]
- Levin, A.V.; Cordovez, J.A.; Leiby, B.E.; Pequignot, E.; Tandon, A. Retinal Hemorrhage in Abusive Head Trauma: Finding a Common Language. Trans. Am. Ophthalmol. Soc. 2014, 112, 1–10. [Google Scholar]
- Bechtel, K.; Stoessel, K.; Leventhal, J.M.; Ogle, E.; Teague, B.; Lavietes, S.; Banyas, B.; Allen, K.; Dziura, J.; Duncan, C. Characteristics That Distinguish Accidental from Abusive Injury in Hospitalized Young Children with Head Trauma. Pediatrics 2004, 114, 165–168. [Google Scholar] [CrossRef]
- Agrawal, S.; Peters, M.J.; Adams, G.G.W.; Pierce, C.M. Prevalence of Retinal Hemorrhages in Critically Ill Children. Pediatrics 2012, 129, e1388–e1396. [Google Scholar] [CrossRef]
- Khosravi, P.; Huck, N.A.; Shahraki, K.; Hunter, S.C.; Danza, C.N.; Kim, S.Y.; Forbes, B.J.; Dai, S.; Levin, A.V.; Binenbaum, G.; et al. Deep Learning Approach for Differentiating Etiologies of Pediatric Retinal Hemorrhages: A Multicenter Study. Int. J. Mol. Sci. 2023, 24, 15105. [Google Scholar] [CrossRef]
- Levin, A.V. Retinal Hemorrhages: Advances in Understanding. Pediatr. Clin. N. Am. 2009, 56, 333–344. [Google Scholar] [CrossRef]
- Gilles, E.E.; McGregor, M.L.; Levy-Clarke, G. Retinal Hemorrhage Asymmetry in Inflicted Head Injury: A Clue to Pathogenesis? J. Pediatr. 2003, 143, 494–499. [Google Scholar] [CrossRef]
- Forbes, B.J.; Cox, M.; Christian, C.W. Retinal Hemorrhages in Patients with Epidural Hematomas. J. AAPOS 2008, 12, 177–180. [Google Scholar] [CrossRef]
- Kivlin, J.D.; Currie, M.L.; Greenbaum, V.J.; Simons, K.B.; Jentzen, J. Retinal Hemorrhages in Children Following Fatal Motor Vehicle Crashes: A Case Series. Arch. Ophthalmol. 2008, 126, 800–804. [Google Scholar] [CrossRef]
- Watts, P.; Obi, E. Retinal Folds and Retinoschisis in Accidental and Non-Accidental Head Injury. Eye 2008, 22, 1514–1516. [Google Scholar] [CrossRef]
- Findley, K.A.; Michael Risinger, D.; Barnes, P.D.; Mack, J.A.; Moran, D.A.; Scheck, B.C.; Bohan, T.L. Feigned Consensus: Usurping the Law in Shaken Baby Syndrome/ Abusive Head Trauma Prosecutions. Wis. L. Rev. 2019, 2019, 1211. [Google Scholar] [CrossRef]
- Vinchon, M. Shaken Baby Sundrome, a Serious Abuse. Sages-Femmes 2023, 22, 12–17. [Google Scholar] [CrossRef]
- Choi, E.H.; Hong, J.D.; Suh, S.; Menezes, C.R.; Walker, K.R.; Bui, J.; Storch, A.; Torres, D.; Espinoza, J.; Shahraki, K.; et al. Exploring Pediatric Vision Care: Insights from Five Years of Referral Cases in the UCI Eye Mobile and Implications of COVID-19. J. Pediatr. Ophthalmol. Strabismus 2024, 1–8. [Google Scholar] [CrossRef]
- Marcinkowska, U.; Paniczek, M.; Ledwoń, M.; Tyrała, K.; Skupnik, R.; Jośko-Ochojska, J. Shaken Baby Syndrome Awareness of the Parents and Medical Staff in Poland. Pediatr. Pol. 2015, 90, 204–209. [Google Scholar] [CrossRef]
- Orozco-Gómez, L.P.; Martínez-Almada, J.; Moreno-Ferreyra, L.G.; Hernández-Salazar, L.; Orozco-Moguel, A.; Dávila-Bárcena, A.; Medina-Díaz, J.C. Ocular repercussions of suspected abusive head trauma. Rev. Mex. Oftalmol. 2021, 95, 20–27. [Google Scholar] [CrossRef]
- Wright, J.; Painter, S.; Kodagali, S.S.; Jones, N.R.; Roalfe, A.; Jayawant, S.; Elston, J.; Anand, G. Disability and Visual Outcomes Following Suspected Abusive Head Trauma in Children under 2 Years. Arch. Dis. Child. 2021, 106, 590–593. [Google Scholar] [CrossRef]
- Moskwa, R.; Todeschi, J.; Wiedemann-Fode, A.; Stella, I.; Joud, A.; Klein, O. Ophthalmological Lesions in Shaken Baby Syndrome: A Retrospective Analysis of 133 Consecutive Cases (1992–2018). Neurochirurgie 2022, 68, 367–372. [Google Scholar] [CrossRef]
- Kanya Iyer, A.; Lemos, N.P. Are We Looking for Retinal Haemorrhages? Med. Sci. Law 2019, 59, 70–71. [Google Scholar] [CrossRef]
- Abed Alnabi, W.; Tang, G.J.; Eagle, R.C.; Gulino, S.; Thau, A.; Levin, A.V. Pathology of Perimacular Folds Due to Vitreoretinal Traction in Abusive Head Trauma. Retina 2019, 39, 2141–2148. [Google Scholar] [CrossRef]
- Nuño, M.; Ugiliweneza, B.; Bardini, R.L.; Ozturk, A.; Stephenson, J.T.; Magaña, J.N. Age-Related Mortality in Abusive Head Trauma. J. Trauma Acute Care Surg. 2019, 87, 827–835. [Google Scholar] [CrossRef] [PubMed]
- Félez-Moliner, I.; García-Íñiguez, J.P.; Lafuente-Hidalgo, M.; López-Pisón, J. Abusive Head Trauma. A Review of Our Experience. Rev. Neurol. 2022, 74, 15–21. [Google Scholar] [CrossRef]
- Hymel, K.P.; Boos, S.C.; Armijo-Garcia, V.; Musick, M.; Weeks, K.; Haney, S.B.; Marinello, M.; Herman, B.E.; Frazier, T.N.; Carroll, C.L.; et al. An Analysis of Physicians’ Diagnostic Reasoning Regarding Pediatric Abusive Head Trauma. Child Abuse Negl. 2022, 129, 105666. [Google Scholar] [CrossRef]
- Weiss, R.; He, C.H.; Khan, S.; Parsikia, A.; Mbekeani, J.N. Ocular Injuries in Pediatric Patients Admitted with Abusive Head Trauma. Pediatr. Neurol. 2022, 127, 11–18. [Google Scholar] [CrossRef]
- Eddahabi, C.; Djalali-Talab, Y.; Banaschak, S.; Feld, K. Unusual Eye Injury Related to Abusive Head Trauma. Rechtsmedizin 2021, 31, 457–462. [Google Scholar] [CrossRef]
- Flugt, A.; Frost, L.; Søndergaard, C.; Milidou, I. Lethal Abusive Head Trauma in Infancy in Denmark from 2000 to 2011. Dan. Med. J. 2021, 68, A08200604. [Google Scholar] [PubMed]
- Oruç, M.; Dündar, A.S.; Okumuş, H.; Görmez, M.; Şamdancı, E.T.; Celbiş, O. Shaken Baby Syndrome Resulting in Death: A Case Series. Turk. J. Pediatr. 2021, 63, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Barth, T.; Altmann, M.; Batzlsperger, C.; Jägle, H.; Helbig, H. Unilateral Retinal Hemorrhage in Infants—Two Cases of Shaken Baby Syndrome? Ophthalmologe 2020, 117, 1033–1036. [Google Scholar] [CrossRef]
- Donaldson, L.; Isaza, G.; Baird, B.; Chaudhary, V. Ophthalmology Referral as Part of a Multidisciplinary Approach to Suspected Abusive Head Trauma. Can. J. Ophthalmol. 2020, 55, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Ksiaa, I.; Ghachem, M.; Besbes, H.; Khochtali, S.; Chouchane, S.; Khairallah, M. Swept-Source OCT Findings in Shaken Baby Syndrome: Case Report. BMC Ophthalmol. 2020, 20, 396. [Google Scholar] [CrossRef]
- Thiblin, I.; Andersson, J.; Wester, K.; Wikström, J.; Högberg, G.; Högberg, U. Medical Findings and Symptoms in Infants Exposed to Witnessed or Admitted Abusive Shaking: A Nationwide Registry Study. PLoS ONE 2020, 15, e0240182. [Google Scholar] [CrossRef]
- Kelly, P.; Vincent, A.; Nolan, M.; Bastin, S. Retinal Haemorrhage in a Child with Optic Neuritis and Acute Disseminated Encephalomyelitis. BMJ Case Rep. 2019, 12, e227211. [Google Scholar] [CrossRef]
- Tripathy, B.; Dean, S.; De Jong, D.; Schmidt, C.; Castellani, R. Is Rotational Trauma the Only Relevant Pathogenic Mechanism in Hemorrhagic Retinopathy of Shaken Baby Syndrome? J. Forensic Sci. Med. 2018, 4, 104–107. [Google Scholar] [CrossRef]
- Wu, A.L.; See, L.C.; Hsia, S.H.; Tu, H.T.; Wang, N.K.; Huang, J.L.; Hwang, Y.S.; Lai, C.C.; Wu, W.C. Pediatric Abusive Head Trauma in Taiwan: Clinical Characteristics and Risk Factors Associated with Mortality. Graefe’s Arch. Clin. Exp. Ophthalmol. 2018, 256, 997–1003. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Petrak, M.; Holz, F.G.; Müller, A.; Krohne, T.U. Retinal Hemorrhages in Shaken Baby Syndrome. J. Pediatr. 2019, 207, 256. [Google Scholar] [CrossRef]
- Burge, L.R.; Van Horne, B.S.; Bachim, A.; Bhatt, A.R.; Donaruma, M. Timely Recognition of Retinal Hemorrhage in Pediatric Abusive Head Trauma Evaluation. J. AAPOS 2021, 25, 89.e1–89.e7. [Google Scholar] [CrossRef] [PubMed]
- Casar Berazaluce, A.M.; Moody, S.; Jenkins, T.; Farooqui, Z.; Shebesta, K.; Kotagal, M.; Falcone, R.A. Catching the Red Eye: A Retrospective Review of Factors Associated with Retinal Hemorrhage in Child Physical Abuse. J. Pediatr. Surg. 2021, 56, 1009–1012. [Google Scholar] [CrossRef]
- Burns, J.; Rohl, S.; Marth, D.; Proctor, D.; Amin, R.; Sekhon, C. Which Clinical Features of Children on Initial Presentation to the Emergency Department with Head Injury Are Associated with Clinically Important Traumatic Brain Injury, Classification as Abuse, and Poor Prognosis? Pediatr. Emerg. Care 2022, 38, E254–E258. [Google Scholar] [CrossRef]
- Even, K.M.; Hymel, K.P.; Armijo-Garcia, V.; Musick, M.; Weeks, K.; Haney, S.B.; Marinello, M.; Herman, B.E.; Frazier, T.N.; Carroll, C.L.; et al. The Association of Subcortical Brain Injury and Abusive Head Trauma. Child Abuse Negl. 2022, 134, 105917. [Google Scholar] [CrossRef]
- Kato, M.; Nonaka, M.; Akutsu, N.; Narisawa, A.; Harada, A.; Park, Y.-S. Correlations of Intracranial Pathology and Cause of Head Injury with Retinal Hemorrhage in Infants and Toddlers: A Multicenter, Retrospective Study by the J-HITs (Japanese Head Injury of Infants and Toddlers Study) Group. PLoS ONE 2023, 18, e0283297. [Google Scholar] [CrossRef]
- Snelling, P.J.; Aruljoe Thanasingam, A.; Jones, P.; Connors, J. Comparison of Abusive Head Trauma versus Non-Inflicted Subdural Haematoma in Infants: A Retrospective Cohort Study. EMA-Emerg. Med. Australas. 2022, 34, 968–975. [Google Scholar] [CrossRef]
- Zelinsky, D.G. Brain Injury Rehabilitation: Cortical and Subcortical Interfacing via Retinal Pathways. PM R 2010, 2, 852–857. [Google Scholar] [CrossRef]
- Gjerde, H.; Mantagos, I.S. Charting the Globe: How Technologies Have Affected Our Understanding of Retinal Findings in Abusive Head Trauma/Shaken Baby Syndrome. Semin. Ophthalmol. 2021, 36, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Mian, M.; Shah, J.; Dalpiaz, A.; Schwamb, R.; Miao, Y.; Warren, K.; Khan, S. Shaken Baby Syndrome: A Review. Fetal Pediatr. Pathol. 2015, 34, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Suh, D.W.; Song, H.H.; Mozafari, H.; Thoreson, W.B. Determining the Tractional Forces on Vitreoretinal Interface Using a Computer Simulation Model in Abusive Head Trauma. Am. J. Ophthalmol. 2021, 223, 396–404. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, A.; Izaki, R.; Fujita, H.; Harada, K.; Ozaki, H.; Kadonosono, K.; Uchio, E. Finite Element Analysis of Changes in Tensile Strain and Deformation by Airbag Impact in Eyes of Various Axial Lengths. Int. Ophthalmol. 2023, 43, 2143–2151. [Google Scholar] [CrossRef] [PubMed]
- Lu, S.; Fan, X.; Liu, S.; Liu, X.; Wang, L. Biomechanism of Resistance to Retinal Injury in Woodpecker’s Eyes. Sci. China Life Sci. 2020, 63, 592–598. [Google Scholar] [CrossRef] [PubMed]
- Wullink, B.; Pas, H.H.; Van der Worp, R.J.; Kuijer, R.; Los, L.I. Type VII Collagen Expression in the Human Vitreoretinal Interface, Corpora Amylacea and Inner Retinal Layers. PLoS ONE 2015, 10, e0145502. [Google Scholar] [CrossRef] [PubMed]
- Umstead, C.; Barhorst, A.; Kasemsri, T.; Mitchell, K. Modeling Hypertension as a Contributor to Retinal Hemorrhaging from Abusive Head Trauma. J. Healthc. Eng. 2020, 2020, 4714927. [Google Scholar] [CrossRef]
- Shah, C.; Sen, P.; Tabani, S.; Prasad, K.; Peeush, P.; Jain, E. Clinical Features of Early-Onset Pediatric Traumatic Glaucoma and Predictive Factors for the Need of Early Glaucoma Surgery. Indian J. Ophthalmol. 2023, 71, 967–972. [Google Scholar] [CrossRef]
- Kletke, S.N.; Mills, M.D.; Tomlinson, L.A.; Yu, Y.; Ying, G.S.; Binenbaum, G. Pediatric Glaucoma Suspects: Characteristics and Outcomes. J. AAPOS 2022, 26, 236.e1–236.e6. [Google Scholar] [CrossRef]
- Kalamkar, C.; Mukherjee, A. Incidence, Clinical Profile, and Short-Term Outcomes of Post-Traumatic Glaucoma in Pediatric Eyes. Indian J. Ophthalmol. 2019, 67, 509–514. [Google Scholar] [CrossRef]
- Buffon, F. Clinical Spectrum of COL4A1 and COL4A2 Mutations. Sang Thromb. Vaiss. 2019, 31, 159–163. [Google Scholar] [CrossRef]
- Scalais, E.; Ceuterick-de Groot, C.; Martin, J.J.; Maugeri, A.; Varlet, P.; Devaux, B.; De Meirleir, L. Cortical Dysplasia, Antenatal Porencephaly, Recurrent Retinal Hemorrhages: Different Insults at Different Times-COL4A1 Deficiency and Environmental Factors. Ann. Neurol. 2015, 78, S198, (Abstract). [Google Scholar]
- Bais, B.; Kubat, B.; Motazedi, E.; Verdijk, R.M. β-Amyloid Precursor Protein and Ubiquitin Immunohistochemistry Aid in the Evaluation of Infant Autopsy Eyes with Abusive Head Trauma. Am. J. Ophthalmol. 2015, 160, 1285–1295.e6. [Google Scholar] [CrossRef] [PubMed]
- Minckler, D.S.; Brown, D.J.; Nalbandian, A.; Suh, D.W. Amyloid Precursor Protein in Abusive Head Trauma Suspects. Am. J. Ophthalmol. 2022, 240, 58–66. [Google Scholar] [CrossRef]
- Chen, J.; Sun, J.; Hu, Y.; Wan, X.; Wang, Y.; Gao, M.; Liang, J.; Liu, T.; Sun, X. MicroRNA-191-5p Ameliorates Amyloid-β1–40–Mediated Retinal Pigment Epithelium Cell Injury by Suppressing the NLRP3 Inflammasome Pathway. FASEB J. 2021, 35, e21184. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Tang, Y. jie Sulforaphane Ameliorates Amyloid-β-Induced Inflammatory Injury by Suppressing the PARP1/SIRT1 Pathway in Retinal Pigment Epithelial Cells. Bioengineered 2021, 12, 7079–7089. [Google Scholar] [CrossRef] [PubMed]
- Tsao, S.W.; Gabriel, R.; Thaker, K.; Kuppermann, B.D.; Kenney, M.C. Effects of Brimonidine on Retinal Pigment Epithelial Cells and Müller Cells Exposed to Amyloid-Beta 1–42 Peptide in Vitro. Ophthalmic Surg. Lasers Imaging Retin. 2018, 49, S23–S28. [Google Scholar] [CrossRef]
- Blackwell, L.S.; Martinez, M.; Fournier-Goodnight, A.; Figueroa, J.; Appert, A.; Vats, A.; Wali, B.; Sayeed, I.; Reisner, A. Patterns of Osteopontin Expression in Abusive Head Trauma Compared with Other Causes of Pediatric Traumatic Brain Injury. J. Pediatr. 2020, 227, 170–175. [Google Scholar] [CrossRef]
- Puñal, V.M.; Paisley, C.E.; Brecha, F.S.; Lee, M.A.; Perelli, R.M.; Wang, J.; O’Koren, E.G.; Ackley, C.R.; Saban, D.R.; Reese, B.E.; et al. Large-Scale Death of Retinal Astrocytes during Normal Development Is Non-Apoptotic and Implemented by Microglia. PLoS Biol. 2019, 17, e3000492. [Google Scholar] [CrossRef]
- Zhao, M.; Toma, K.; Kinde, B.; Li, L.; Patel, A.K.; Wu, K.-Y.; Lum, M.R.; Tan, C.; Hooper, J.E.; Kriegstein, A.R.; et al. Osteopontin Drives Retinal Ganglion Cell Resiliency in Glaucomatous Optic Neuropathy. Cell Rep. 2023, 42, 113038. [Google Scholar] [CrossRef]
- Ruzafa, N.; Pereiro, X.; Aspichueta, P.; Araiz, J.; Vecino, E. The Retina of Osteopontin Deficient Mice in Aging. Mol. Neurobiol. 2018, 55, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.W.; Kim, H.I.; Kim, G.H.; Park, S.J.; Kim, I.B. Increased Expression of Osteopontin in Retinal Degeneration Induced by Blue Light-Emitting Diode Exposure in Mice. Front. Mol. Neurosci. 2016, 9, 58. [Google Scholar] [CrossRef] [PubMed]
- Duan, X.; Qiao, M.; Bei, F.; Kim, I.J.; He, Z.; Sanes, J.R. Subtype-Specific Regeneration of Retinal Ganglion Cells Following Axotomy: Effects of Osteopontin and Mtor Signaling. Neuron 2015, 85, 1244–1256. [Google Scholar] [CrossRef] [PubMed]
- Echegaray, J.J.; Iyer, P.; Acon, D.; Negron, C.; El Hamichi, S.; Berrocal, A.M. Superficial and Deep Capillary Plexus Nonperfusion in Nonaccidental Injury on OCTA. J. Vitreoretin. Dis. 2023, 7, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Liu, J.; Zhang, Y.; Zha, X.; Zhang, H.; Tang, Y.; Zhao, X. MiR-181d-5p Protects against Retinal Ganglion Cell Death after Blunt Ocular Injury by Regulating NFIA-Medicated Astrocyte Development. Mediat. Inflamm. 2022, 2022, 5400592. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.; Gao, Y.; Li, J.M.; Bao, Y.K.; Nie, C.; Yin, P.; Lyu, X.; Ding, X.Y.; Lu, R. Analysis of Retinal Vasculature Changes in Indirect Traumatic Optic Neuropathy Using Optic Coherence Tomography Angiography. Int. J. Ophthalmol. 2022, 15, 1344–1351. [Google Scholar] [CrossRef] [PubMed]
- Hetzer, S.M.; Shalosky, E.M.; Torrens, J.N.; Evanson, N.K. Chronic Histological Outcomes of Indirect Traumatic Optic Neuropathy in Adolescent Mice: Persistent Degeneration and Temporally Regulated Glial Responses. Cells 2021, 10, 3343. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.-T.; Wen, Y.-T.; Desai, T.D.; Tsai, R.-K. Intravitreal Injection of Long-Acting Pegylated Granulocyte Colony-Stimulating Factor Provides Neuroprotective Effects via Antioxidant Response in a Rat Model of Traumatic Optic Neuropathy. Antioxidants 2021, 10, 1934. [Google Scholar] [CrossRef]
- Balsak, S.; Deveci, E. Effects of Hesperidin on the Changes Made in the Retinal Damage Induced by Traumatic Head Injury. Anal. Quant. Cytopathol. Histopathol. 2021, 43, 337–344. [Google Scholar]
- Hetzer, S.M.; Guilhaume-Correa, F.; Day, D.; Bedolla, A.; Evanson, N.K. Traumatic Optic Neuropathy Is Associated with Visual Impairment, Neurodegeneration, and Endoplasmic Reticulum Stress in Adolescent Mice. Cells 2021, 10, 996. [Google Scholar] [CrossRef]
- Xu, Q.; Rydz, C.; Nguyen Huu, V.A.; Rocha, L.; Palomino La Torre, C.; Lee, I.; Cho, W.; Jabari, M.; Donello, J.; Lyon, D.C.; et al. Stress Induced Aging in Mouse Eye. Aging Cell 2022, 21, e13737. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Saha, P.; Sen, T.; Sen, N. An Augmentation in Histone Dimethylation at Lysine Nine Residues Elicits Vision Impairment Following Traumatic Brain Injury. Free Radic. Biol. Med. 2019, 134, 630–643. [Google Scholar] [CrossRef] [PubMed]
- Khoobyar, A.; Penkova, A.N.; Humayun, M.S.; Sadhal, S.S. Mathematical Model of Macromolecular Drug Transport in a Partially Liquefied Vitreous Humor. J. Heat Transfer 2022, 144, 031208. [Google Scholar] [CrossRef] [PubMed]
- Shukla, V.V.; Sawalakhe, P.V.; Shende, P. FEA of Contact between Scleral Buckle and Human Eye Tissues. Asia-Pacific J. Sci. Technol. 2022, 27, APST-27-01-15. [Google Scholar] [CrossRef]
- Sornalingam, K.; Borman, A.D.; Ashworth, J. Nonaccidental Injury Presenting as Unilateral Retinal Detachment in Two Infants. J. AAPOS 2018, 22, 231–233. [Google Scholar] [CrossRef] [PubMed]
- Santos, M.; Araujo, A.; Barbeiro, S.; Caramelo, F.; Correia, A.; Marques, M.I.; Pinto, L.; Serranho, P.; Bernardes, R.; Morgado, M. Simulation of Cellular Changes on Optical Coherence Tomography of Human Retina. In Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society, EMBS, Milan, Italy, 25–29 August 2015; Volume 2015-Novem, pp. 8147–8150. [Google Scholar]
- Weedn, V.W.; Mansour, A.M.; Nichols, M.M. Retinal Hemorrhage in an Infant After Cardiopulmonary Resuscitation. Am. J. Forensic Med. Pathol. 1990, 11, 79–82. [Google Scholar] [CrossRef] [PubMed]
- Watts, P.; Maguire, S.; Kwok, T.; Talabani, B.; Mann, M.; Wiener, J.; Lawson, Z.; Kemp, A. Newborn Retinal Hemorrhages: A Systematic Review. J. AAPOS 2013, 17, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Ballabh, P. Pathogenesis and Prevention of Intraventricular Hemorrhage. Clin. Perinatol. 2014, 41, 47–67. [Google Scholar] [CrossRef] [PubMed]
- Mansour, A.M.; Lee, J.W.; Yahng, S.A.; Kim, K.S.; Shahin, M.; Hamerschlak, N.; Belfort, R.N.; Kurup, S.K. Ocular Manifestations of Idiopathic Aplastic Anemia: Retrospective Study and Literature Review. Clin. Ophthalmol. 2014, 8, 777–787. [Google Scholar] [CrossRef]
- Shokrollahi, Y.; Dong, P.; Lam, M.; Suh, D.W.; Gu, L. Eye Protection for Mitigating Soccer-Related Ocular Injuries: A Finite Element Approach. J. Eng. Sci. Med. Diagn. Ther. 2022, 5, 041003. [Google Scholar] [CrossRef]
- Lam, M.R.; Dong, P.; Shokrollahi, Y.; Gu, L.; Suh, D.W. Finite Element Analysis of Soccer Ball-Related Ocular and Retinal Trauma and Comparison with Abusive Head Trauma. Ophthalmol. Sci. 2022, 2, 100129. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, M.; Yamazaki, J.; Mizunuma, H. A Finite Element Analysis of the Retinal Hemorrhages Accompanied by Shaken Baby Syndrome/Abusive Head Trauma. J. Biomech. 2014, 47, 3454–3458. [Google Scholar] [CrossRef] [PubMed]
- Song, H.H.; Thoreson, W.B.; Dong, P.; Shokrollahi, Y.; Gu, L.; Suh, D.W. Exploring the Vitreoretinal Interface: A Key Instigator of Unique Retinal Hemorrhage Patterns in Pediatric Head Trauma. Korean J. Ophthalmol. 2022, 36, 253–263. [Google Scholar] [CrossRef] [PubMed]
- Stray-Pedersen, A.; Strisland, F.; Rognum, T.O.; Schiks, L.A.H.; Loeve, A.J. Violent Infant Surrogate Shaking: Continuous High-Magnitude Centripetal Force and Abrupt Shift in Tangential Acceleration May Explain High Risk of Subdural Hemorrhage. Neurotrauma Rep. 2021, 2, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Nadarasa, J.; Deck, C.; Meyer, F.; Bourdet, N.; Raul, J.S.; Willinger, R. Development of a Finite-Element Eye Model to Investigate Retinal Hemorrhages in Shaken Baby Syndrome. Biomech. Model. Mechanobiol. 2018, 17, 517–530. [Google Scholar] [CrossRef]
- Yamazaki, J.; Yoshida, M.; Mizunuma, H. Experimental Analyses of the Retinal and Subretinal Haemorrhages Accompanied by Shaken Baby Syndrome/Abusive Head Trauma Using a Dummy Doll. Injury 2014, 45, 1196–1206. [Google Scholar] [CrossRef]
| Study | Year | Country | Type | Presentation | Tools | Observations | Ref. |
|---|---|---|---|---|---|---|---|
| Felez-Moliner et al. | 2022 | Spain | Retrospective cohort | Seizure | CCT Fundoscopy | RH (15, 79%) SDH (15, 79%) | [31] |
| Hymel et al. | 2022 | USA | Case series | Respiratory compromise Circulatory compromise Seizure | CCT Fundoscopy | Bilateral SDH (41, 71.4%) Retinoschisis (12, 21.4%) RH (21, 35.7%) | [32] |
| Moskwa et al. | 2022 | France | Retrospective cohort | Crying Seizure | CCT Fundoscopy | IVH (9, 6.7%) Macular lesions (11, 8.2%) Papilledema (15, 11.1%) RH (126, 94.4%) | [27] |
| Weiss et al. | 2022 | USA | Retrospective cohort | Crying Eye contusion Seizure | CCT Fundoscopy | Retinal edema (1512, 59.3%) RH (135, 5.3%) SAH (584, 22.9%) SDH (1856, 72.8%) | [33] |
| Eddahabi et al. | 2021 | Germany | Case report | Paroxysmal crying Paused breathing Seizure | Fundoscopy | Bilateral RH ILM hemorrhage IVH PVR | [34] |
| Flugt et al. | 2021 | Denmark | Case series | Contusion Crying Rib fractures Skull fractures | CCT Fundoscopy | Cerebral edema (7, 87.5%) SAH (8, 100%) RH (6, 75%) SDH (6, 75%) | [35] |
| Oruç et al. | 2021 | Turkey | Retrospective cohort | Cardiopulmonary arrest Seizure | CCT Fundoscopy | Bilateral RH (6, 75%) Unilateral RH (2, 25%) SAH + EDH (1, 12.5%) SAH + SDH (3, 37.5%) SAH + SDH + ICH (4, 50%) | [36] |
| Barth et al. | 2020 | Germany | Case series | Loss of consciousness Paroxysmal crying Seizure | CCT Fundoscopy | Periorbital petechiae (2, 100%) SDH (2, 100%) Unilateral RH (2, 100%) | [37] |
| Donaldson et al. | 2020 | Canada | Retrospective cohort | Loss of consciousness Paroxysmal crying Seizure | CCT Fundoscopy MRI | ICH (21, 72.4%) Retinoschisis (5, 18.8%) RH (16, 55.2%) | [38] |
| Ksiaa et al. | 2020 | Tunisia | Case report | Loss of consciousness Paroxysmal crying | CCT SSOCT | Bilateral SDH Bilaterally poor PLR Bilateral pRH Bilateral iRH Bilateral pMH Bilateral ILM detachment | [39] |
| Thilbin et al. | 2020 | Sweden | Retrospective cohort | Contusion Crying Rib fractures | CCT MRI X-ray | Bilateral RH (1, 2.7%) Unilateral RH (1, 2.7%) | [40] |
| Alnabi et al. | 2019 | USA | Case series | Loss of consciousness Respiratory compromise Seizure | CCT Fundoscopy | Bilateral RH (4, 80%) VRT (5, 100%) PMF (5, 100%) ILM detachment (5, 100%) | [29] |
| Kelly et al. | 2019 | New Zealand | Case report | Acute visual loss Dilated pupils Lethargy | CCT MRI Fundoscopy | Bilateral RH | [41] |
| Tripathy et al. | 2018 | USA | Case report | Cardiovascular collapse | Fundoscopy MRI | Bilateral SDH ILM hemorrhage Retinoschisis SAH Subhyaloid hemorrhage | [42] |
| Wu et al. | 2018 | Taiwan | Retrospective cohort | Crying Loss of consciousness Vomiting Respiratory compromise | CCT Fundoscopy | Retinoschisis (20, 26.7%) RH (69, 92%) | [43] |
| Study | Year | Country | Experimental Material | Model | Stress Type | Stress Magnitude | Ref. |
|---|---|---|---|---|---|---|---|
| Song et al. | 2022 | USA | Primate eye Sheep eye | FEM | Linear acceleration Angular acceleration Repetitive shaking | Vitreoretinal detachment: 1–5 kPa Cyclic tension range: 3–16 kP | [95] |
| Lam et al. | 2022 | USA | − | FEM | Linear acceleration Angular acceleration | Preretinal: 0–1.6 kPa Intraretinal: 0–1.4 kPa Subretinal: 0–1.4 kPa | [93] |
| Stray-Pedersen et al. | 2021 | Norway | Dummy equivalent of 1-month-old infant | Human perpetrator | Repetitive shaking | Acceleration (X axis): 6.5–36.2 g Acceleration (Y axis): 2.6–11.7 g Acceleration (Z axis): 5.2–44.0 g | [96] |
| Nadarasa et al. | 2018 | France | Dummy equivalent of 6-week-old infant | FEM | Linear acceleration Rotational acceleration Repetitive shaking | Choroid: 10.7–16 kPa Retina: 1.4–2.0 kPa | [97] |
| Yoshida et al. | 2014 | Japan | Agar gel (used for modeling vitreous) | FEM | Linear acceleration Rotational acceleration Repetitive shaking | Abusive shake (per cycle): 101 Pa/s Abusive impact: 36 Pa/s | [94] |
| Yamazaki et al. | 2014 | Japan | Dummy doll | FEM | Cyclic acceleration–deceleration | Shaking (per cycle): 107 Pa/s Fall (per cycle): 60–73 Pa/s | [98] |
| FEM: finite element model. | |||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shahraki, K.; Suh, D.W. An Update to Biomechanical and Biochemical Principles of Retinal Injury in Child Abuse. Children 2024, 11, 586. https://doi.org/10.3390/children11050586
Shahraki K, Suh DW. An Update to Biomechanical and Biochemical Principles of Retinal Injury in Child Abuse. Children. 2024; 11(5):586. https://doi.org/10.3390/children11050586
Chicago/Turabian StyleShahraki, Kourosh, and Donny W. Suh. 2024. "An Update to Biomechanical and Biochemical Principles of Retinal Injury in Child Abuse" Children 11, no. 5: 586. https://doi.org/10.3390/children11050586
APA StyleShahraki, K., & Suh, D. W. (2024). An Update to Biomechanical and Biochemical Principles of Retinal Injury in Child Abuse. Children, 11(5), 586. https://doi.org/10.3390/children11050586







