Relationship between Baseline Serum Potassium and 1-Year Readmission in Pediatric Patients with Heart Failure: A Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Clinical Data and Laboratory Values
2.3. Study Outcome
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics of the Patients
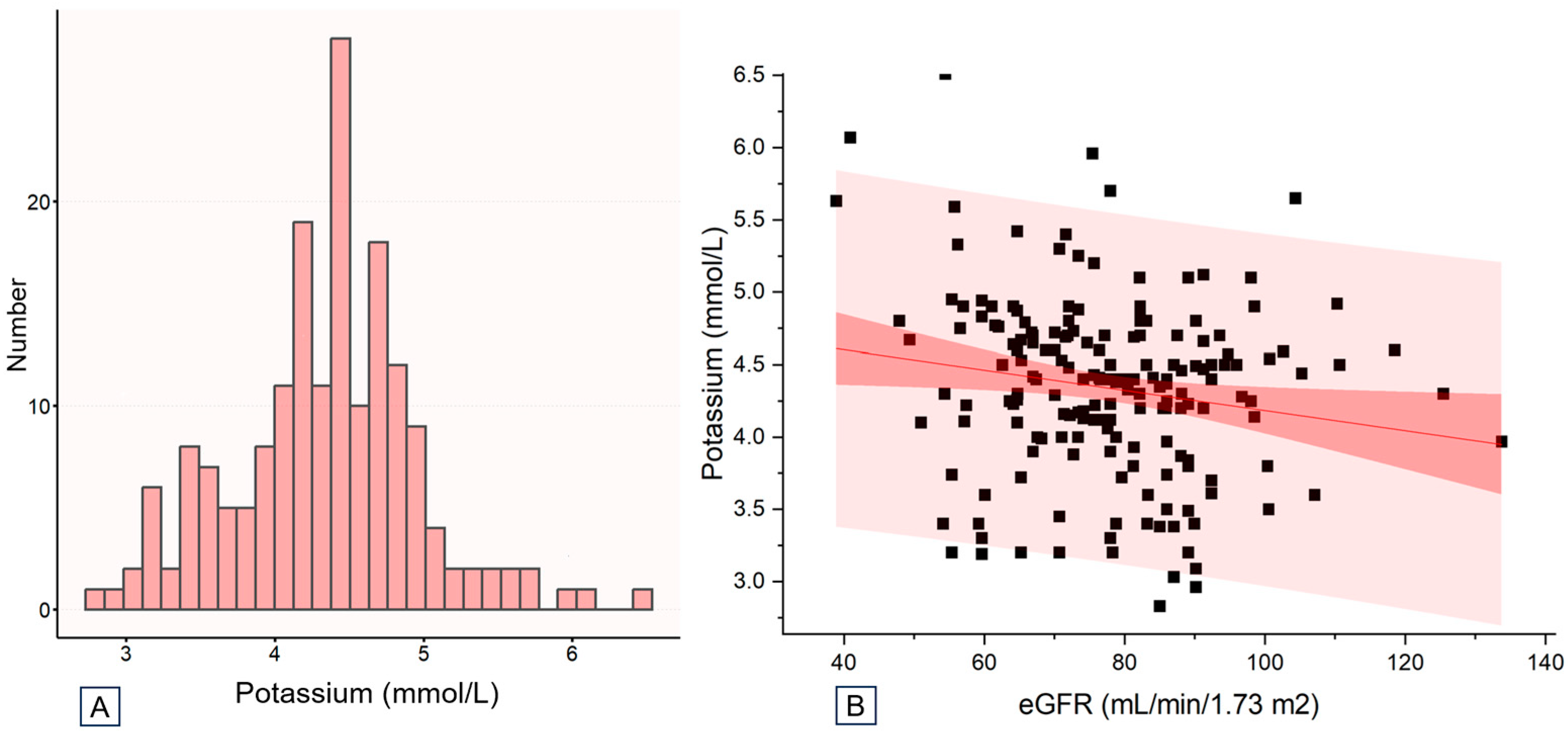
3.2. Distribution of Baseline Potassium Levels
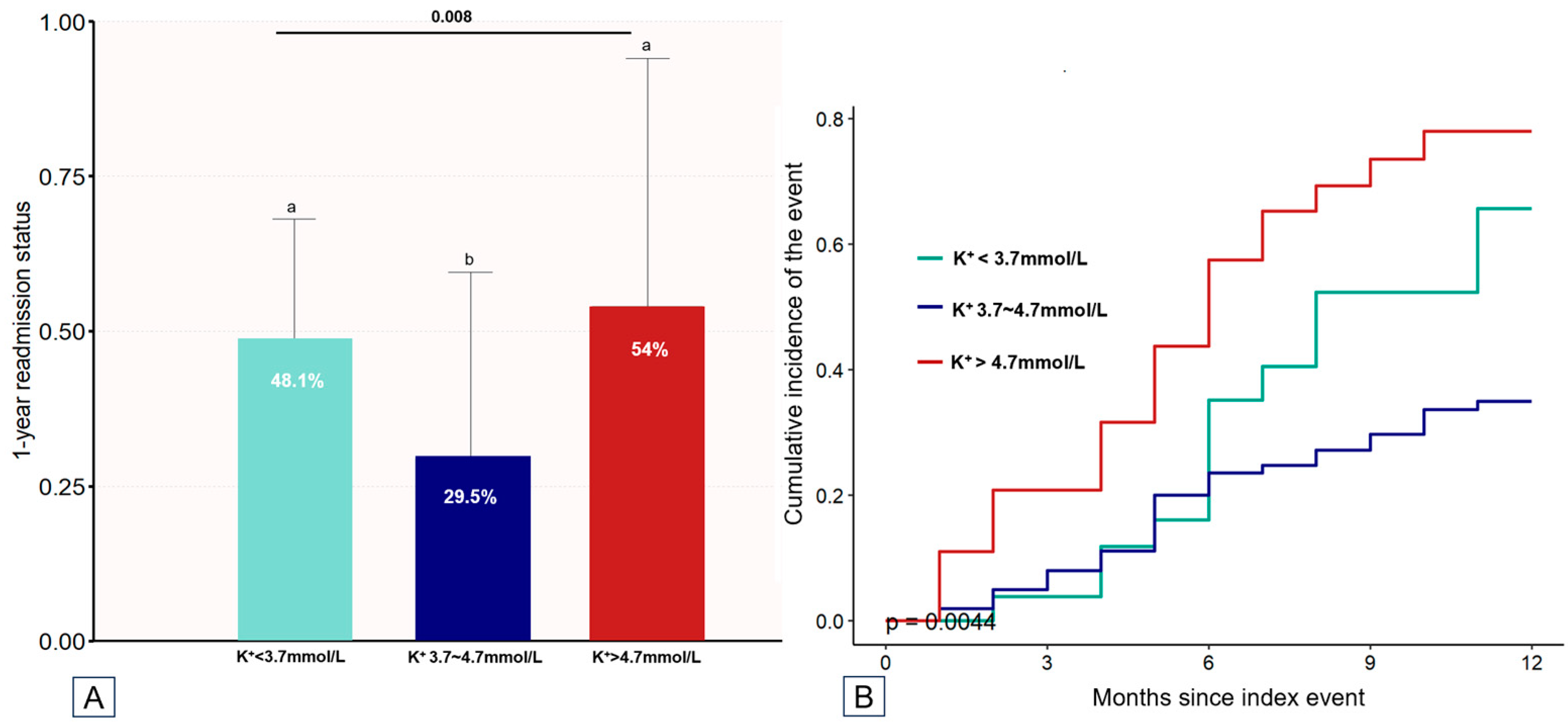
3.3. Endpoint Event Rates Stratified by Baseline Potassium Levels
3.4. Association between Baseline Potassium Levels and Outcomes
3.5. Other Risk Factors for 1-Year HF Readmission in Pediatric Patients with HF
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rossano, J.W.; Kim, J.J.; Decker, J.A.; Price, J.F.; Zafar, F.; Graves, D.E.; Morales, D.L.; Heinle, J.S.; Bozkurt, B.; Towbin, J.A.; et al. Prevalence, morbidity, and mortality of heart failure-related hospitalizations in children in the United States: A population-based study. J. Card. Fail. 2012, 18, 459–470. [Google Scholar] [CrossRef]
- Das, B.B.; Moskowitz, W.B.; Butler, J. Current and Future Drug and Device Therapies for Pediatric Heart Failure Patients: Potential Lessons from Adult Trials. Children 2021, 8, 322. [Google Scholar] [CrossRef]
- Fadl, S.; Wåhlander, H.; Fall, K.; Cao, Y.; Sunnegårdh, J. The highest mortality rates in childhood dilated cardiomyopathy occur during the first year after diagnosis. Acta Paediatr. 2018, 107, 672–677. [Google Scholar] [CrossRef]
- Jammal Addin, M.B.; Young, D.; McCarrison, S.; Hunter, L. Dilated cardiomyopathy in a national paediatric population. Eur. J. Pediatr. 2019, 178, 1229–1235. [Google Scholar] [CrossRef] [PubMed]
- Bichali, S.; Malorey, D.; Benbrik, N.; Le Gloan, L.; Gras-Le Guen, C.; Baruteau, A.E.; Launay, E. Measurement, consequences and determinants of time to diagnosis in children with new-onset heart failure: A population-based retrospective study (DIACARD study). Int. J. Cardiol. 2020, 318, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, D.; Rosano, G.; Herzog, C.A. Management of Heart Failure Patient with CKD. Clin. J. Am. Soc. Nephrol. 2021, 16, 1131–1139. [Google Scholar] [CrossRef] [PubMed]
- Zhao, K.; Zheng, Q.; Zhou, J.; Zhang, Q.; Gao, X.; Liu, Y.; Li, S.; Shan, W.; Liu, L.; Guo, N.; et al. Associations between serum electrolyte and short-term outcomes in patients with acute decompensated heart failure. Ann. Med. 2023, 55, 155–167. [Google Scholar] [CrossRef] [PubMed]
- Senekovič Kojc, T.; Marčun Varda, N. Novel Biomarkers of Heart Failure in Pediatrics. Children 2022, 9, 740. [Google Scholar] [CrossRef]
- Aldahl, M.; Jensen, A.C.; Davidsen, L.; Eriksen, M.A.; Møller Hansen, S.; Nielsen, B.J.; Krogager, M.L.; Køber, L.; Torp-Pedersen, C.; Søgaard, P. Associations of serum potassium levels with mortality in chronic heart failure patients. Eur. Heart J. 2017, 38, 2890–2896. [Google Scholar] [CrossRef]
- Fan, Y.; Wu, M.; Li, X.; Zhao, J.; Shi, J.; Ding, L.; Jiang, H.; Li, Z.; Zhang, W.; Ma, T.; et al. Potassium levels and the risk of all-cause and cardiovascular mortality among patients with cardiovascular diseases: A meta-analysis of cohort studies. Nutr. J. 2024, 23, 8. [Google Scholar] [CrossRef]
- Ferreira, J.P.; Mogensen, U.M.; Jhund, P.S.; Desai, A.S.; Rouleau, J.L.; Zile, M.R.; Rossignol, P.; Zannad, F.; Packer, M.; Solomon, S.D.; et al. Serum potassium in the PARADIGM-HF trial. Eur. J. Heart Fail. 2020, 22, 2056–2064. [Google Scholar] [CrossRef]
- Linde, C.; Qin, L.; Bakhai, A.; Furuland, H.; Evans, M.; Ayoubkhani, D.; Palaka, E.; Bennett, H.; McEwan, P. Serum potassium and clinical outcomes in heart failure patients: Results of risk calculations in 21 334 patients in the UK. ESC Heart Fail. 2019, 6, 280–290. [Google Scholar] [CrossRef] [PubMed]
- Lipshultz, S.E.; Law, Y.M.; Asante-Korang, A.; Austin, E.D.; Dipchand, A.I.; Everitt, M.D.; Hsu, D.T.; Lin, K.Y.; Price, J.F.; Wilkinson, J.D.; et al. Cardiomyopathy in Children: Classification and Diagnosis: A Scientific Statement From the American Heart Association. Circulation 2019, 140, e9–e68. [Google Scholar] [CrossRef] [PubMed]
- Toledo, C.C.; Vellosa Schwartzmann, P.; Miguel Silva, L.; da Silva Ferreira, G.; Bianchini Cardoso, F.; Citelli Ribeiro, V.; Paim, L.R.; Antunes-Correa, L.M.; Carvalho Sposito, A.; Matos Souza, J.R.; et al. Serum potassium levels provide prognostic information in symptomatic heart failure beyond traditional clinical variables. ESC Heart Fail. 2021, 8, 2133–2143. [Google Scholar] [CrossRef]
- Shang, G.; Gao, Y.; Liu, K.; Wang, X. Serum potassium in elderly heart failure patients as a predictor of readmission within 1 year. Heart Vessels 2023, 38, 507–516. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Zhang, Y.; Chen, M.; Dai, J.; Song, A.; Chen, J.; Tao, X. The Association Between Variability in Electrolytes and the In-Hospital Mortality in Critically Ill Children in Pediatric Intensive Care Units. Front. Pediatr. 2021, 9, 692894. [Google Scholar] [CrossRef]
- Haider, M.; Hameed, A.; Fatima, S.; Afroze, M.; Noor, N.; Arshad, U. Frequency of Electrolyte Disorders and Its Effect On Mortality Among Children Admitted In Pediatric Intensive Care Unit. J. Bahria Univ. Med. Dent. Coll. 2021, 10, 115–119. [Google Scholar] [CrossRef]
- Ferreira, J.P.; Butler, J.; Rossignol, P.; Pitt, B.; Anker, S.D.; Kosiborod, M.; Lund, L.H.; Bakris, G.L.; Weir, M.R.; Zannad, F. Abnormalities of Potassium in Heart Failure: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2020, 75, 2836–2850. [Google Scholar] [CrossRef]
- Savarese, G.; Xu, H.; Trevisan, M.; Dahlström, U.; Rossignol, P.; Pitt, B.; Lund, L.H.; Carrero, J.J. Incidence, Predictors, and Outcome Associations of Dyskalemia in Heart Failure With Preserved, Mid-Range, and Reduced Ejection Fraction. JACC Heart Fail. 2019, 7, 65–76. [Google Scholar] [CrossRef]
- Schnaubelt, S.; Niederdoeckl, J.; Schoergenhofer, C.; Cacioppo, F.; Schuetz, N.; Spiel, A.O.; Hecking, M.; Domanovits, H. Hyperkalemia: A persisting risk. A case report and update on current management. Clin. Case Rep. 2020, 8, 1748–1753. [Google Scholar] [CrossRef]
- Lopez-López, A.; Franco-Gutiérrez, R.; Pérez-Pérez, A.J.; Regueiro-Abel, M.; Elices-Teja, J.; Abou-Jokh-Casas, C.; González-Juanatey, C. Impact of Hyperkalemia in Heart Failure and Reduced Ejection Fraction: A Retrospective Study. J. Clin. Med. 2023, 12, 3595. [Google Scholar] [CrossRef] [PubMed]
- Hunter, R.W.; Bailey, M.A. Hyperkalemia: Pathophysiology, risk factors and consequences. Nephrol. Dial. Transplant. 2019, 34, iii2–iii11. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Zhao, D.; Wang, M.; Qi, Y.; Sun, J.; Liu, J.; Li, Y.; Liu, J. Association of Serum Potassium Levels with Mortality and Cardiovascular Events: Findings from the Chinese Multi-provincial Cohort Study. J. Gen. Intern. Med. 2022, 37, 2446–2453. [Google Scholar] [CrossRef] [PubMed]


| Variables | Total (n = 180) | Baseline Serum Potassium (mmol/L) | p Value | ||
|---|---|---|---|---|---|
| <3.7 (n = 27) | 3.7–4.7 (n = 105) | ≥4.7 (n = 48) | |||
| Age, year | 7.0 ± 5.6 | 6.9 ± 5.4 | 6.6 ± 5.4 | 7.8 ± 6.1 | 0.488 |
| Sex, male, n (%) | 106 (58.9) | 16 (59.3) | 59 (56.2) | 31 (64.6) | 0.691 |
| Ethnicity, n (%) | 0.993 | ||||
| Han | 79 (43.9) | 13 (48.1) | 46 (43.8) | 20 (41.7) | |
| Zhuang | 87 (48.3) | 13 (48.1) | 50 (47.6) | 24 (50) | |
| Miao | 8 (4.4) | 1 (3.7) | 5 (4.8) | 2 (4.2) | |
| Other | 6 (3.3) | 0 (0) | 4 (3.8) | 2 (4.2) | |
| Preexisting HF, n (%) | 31 (17.2) | 3 (11.1) | 14 (13.3) | 14 (29.2) | 0.043 |
| NYHA/Ross classification, n (%) | 0.046 | ||||
| II | 76 (42.2) | 13 (48.1) | 50 (47.6) | 13 (27.1) | |
| III/IV | 104 (57.8) | 14 (51.9) | 55 (52.4) | 35 (72.9) | |
| Hospital length of stay, days | 11.4 ± 6.8 | 11.6 ± 6.5 | 10.7 ± 6.3 | 12.7 ± 7.9 | 0.252 |
| Etiology of HF, n (%) | 31 (17.2) | 3 (11.1) | 14 (13.3) | 14 (29.2) | 0.951 |
| Dilated cardiomyopathy | 121 (67.2) | 19 (70.4) | 70 (66.7) | 32 (66.7) | |
| Myocarditis | 34 (18.9) | 4 (14.8) | 20 (19) | 10 (20.8) | |
| Anomalous origin of coronary artery | 7 (3.9) | 0 (0) | 6 (5.7) | 1 (2.1) | |
| Kawasaki disease | 11 (6.1) | 2 (7.4) | 6 (5.7) | 3 (6.2) | |
| Hypertensive disease | 4 (2.2) | 1 (3.7) | 2 (1.9) | 1 (2.1) | |
| Other | 3 (1.7) | 1 (3.7) | 1 (1) | 1 (2.1) | |
| BUN, mmol/L | 6.1 ± 3.3 | 6.3 ± 2.6 | 5.7 ± 2.6 | 7.0 ± 4.6 | 0.054 |
| SCr, µmol/L | 46.3 ± 23.9 | 47.3 ± 20.6 | 43.3 ± 21.6 | 52.5 ± 29.2 | 0.084 |
| eGFR, mL/min/1.73 m2 | 77.8 ± 15.1 | 79.1 ± 14.3 | 80.0 ± 14.5 | 72.3 ± 15.6 | 0.012 |
| SUA, µmol/L | 375.1 ± 157.8 | 389.1 ± 158.2 | 369.5 ± 153.8 | 379.7 ± 168.6 | 0.826 |
| ALB, g/L | 39.8 ± 4.3 | 40.2 ± 4.0 | 39.7 ± 4.7 | 39.8 ± 3.7 | 0.894 |
| HB, g/L | 120.4 ± 20.2 | 118.5 ± 19.4 | 120.7 ± 18.7 | 121.0 ± 23.8 | 0.863 |
| Serum sodium, mmol/L | 135.4 ± 4.8 | 136.0 ± 5.2 | 135.7 ± 4.3 | 134.5 ± 5.5 | 0.249 |
| LVEF, % | 32.0 ± 10.0 | 32.4 ± 8.7 | 32.0 ± 10.1 | 31.9 ± 10.7 | 0.029 |
| Discharge medication | |||||
| Digoxin, n (%) | 109 (60.6) | 18 (66.7) | 59 (56.2) | 32 (66.7) | 0.336 |
| Captopril, n (%) | 82 (45.6) | 14 (51.9) | 40 (38.1) | 28 (58.3) | 0.051 |
| Hydrochlorothiazide, n (%) | 113 (62.8) | 15 (55.6) | 67 (63.8) | 31 (64.6) | 0.699 |
| Spironolactone, n (%) | 129 (71.7) | 20 (74.1) | 72 (68.6) | 37 (77.1) | 0.531 |
| Metoprolol, n (%) | 55 (30.6) | 10 (37) | 32 (30.5) | 13 (27.1) | 0.668 |
| Outcome | |||||
| 1 or more 1-year readmissions for HF, n (%) | 70 (38.9) | 13 (48.1) | 31 (29.5) | 26 (54.2) | 0.008 |
| ≥2 admissions for HF, n (%) | 32 (17.8) | 5 (18.5) | 11 (10.5) | 16 (33.3) | 0.005 |
| Variable | Unadjusted Model | Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|---|---|
| HR_95% CI | p Value | HR_95% CI | p Value | HR_95% CI | p Value | HR_95% CI | p Value | |
| Potassium per 1 mmol/L increase | 1.85 (1.19−2.87) | 0.006 | 1.83 (1.19−2.82) | 0.006 | 1.36 (0.9−2.05) | 0.141 | 1.3 (0.85−2.01) | 0.227 |
| Potassium < 3.7 mmol/L | 1.71 (0.9−3.28) | 0.103 | 1.63 (0.84−3.14) | 0.146 | 1.55 (0.81−2.97) | 0.19 | 1.72 (0.89−3.32) | 0.109 |
| Potassium 3.7−4.7 mmol/L | 1 (Ref) | 1 (Ref) | 1 (Ref) | 1 (Ref) | ||||
| Potassium ≥ 4.7 mmol/L | 2.34 (1.39−3.94) | 0.001 | 2.02 (1.16−3.53) | 0.013 | 2.03 (1.17−3.51) | 0.012 | 1.91 (1.09−3.35) | 0.024 |
| Variables | Univariate Cox Analyses HR (95% CI) | p Value | Multivariable Cox Analyses HR (95% CI) | p Value |
|---|---|---|---|---|
| Potassium ˂ 3.7 mmol/L | 1.71 (0.9−3.28) | 0.103 | - | |
| Potassium 3.7−4.7 mmol/L | Ref | |||
| Potassium ≥ 4.7 mmol/L | 2.34 (1.39−3.94) | 0.001 | 1.87 (1.08−3.26) | 0.026 |
| Age, year | 1.05 (1−1.09) | 0.032 | 0.98 (0.93−1.04) | 0.512 |
| Sex, male | 0.79 (0.48−1.28) | 0.327 | - | |
| Hospital length of stay, day | 1.03 (1−1.07) | 0.051 | - | |
| SCr, µmol/L | 1.01 (1.01−1.02) | 0.002 | 1 (0.99−1.01) | 0.906 |
| BUN, mmol/L | 1.16 (1.1−1.23) | <0.001 | 1.09 (1.01−1.18) | 0.029 |
| eGFR, per 10 mL/min/1.73 m2 increase | 0.79 (0.66−0.94) | 0.006 | 0.93 (0.77−1.13) | 0.467 |
| SUA, per 10 µmol/L increase | 1.02 (1−1.03) | 0.041 | 1.01 (0.99−1.02) | 0.425 |
| ALB, g/L | 0.94 (0.89−0.99) | 0.019 | 0.95 (0.89−1.01) | 0.077 |
| Serum sodium, mmol/L | 0.94 (0.9−0.98) | 0.013 | 0.99 (0.94−1.05) | 0.757 |
| HB, per 10 g/L increase | 1.02 (0.91−1.14) | 0.776 | - | |
| LVEF, % | 0.98 (0.95−1) | 0.06 | - | |
| Preexisting HF ≥ 6 months | 1.7 (0.97−2.97) | 0.077 | - | |
| NYHA/Ross classification, III/IV | 2.39 (1.41−4.05) | 0.001 | 1.94 (1.09−3.46) | 0.025 |
| Digoxin at discharge | 0.79 (0.43−1.46) | 0.455 | - | |
| Captopril at discharge | 1.34 (0.73−2.45) | 0.34 | - | |
| Hydrochlorothiazide at discharge | 0.89 (0.55−1.44) | 0.645 | ||
| Spironolactone at discharge | 1.43 (0.82−2.51) | 0.191 | ||
| Metoprolol at discharge | 0.61 (0.31−1.19) | 0.147 | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, Y.; Huang, Y.; Su, D.; Liu, D.; Chen, C.; Pang, Y. Relationship between Baseline Serum Potassium and 1-Year Readmission in Pediatric Patients with Heart Failure: A Retrospective Cohort Study. Children 2024, 11, 725. https://doi.org/10.3390/children11060725
Han Y, Huang Y, Su D, Liu D, Chen C, Pang Y. Relationship between Baseline Serum Potassium and 1-Year Readmission in Pediatric Patients with Heart Failure: A Retrospective Cohort Study. Children. 2024; 11(6):725. https://doi.org/10.3390/children11060725
Chicago/Turabian StyleHan, Yong, Yuqin Huang, Danyan Su, Dongli Liu, Cheng Chen, and Yusheng Pang. 2024. "Relationship between Baseline Serum Potassium and 1-Year Readmission in Pediatric Patients with Heart Failure: A Retrospective Cohort Study" Children 11, no. 6: 725. https://doi.org/10.3390/children11060725
APA StyleHan, Y., Huang, Y., Su, D., Liu, D., Chen, C., & Pang, Y. (2024). Relationship between Baseline Serum Potassium and 1-Year Readmission in Pediatric Patients with Heart Failure: A Retrospective Cohort Study. Children, 11(6), 725. https://doi.org/10.3390/children11060725





