Children at Risk of Specific Learning Disorder: A Study on Prevalence and Risk Factors
Abstract
:1. Introduction
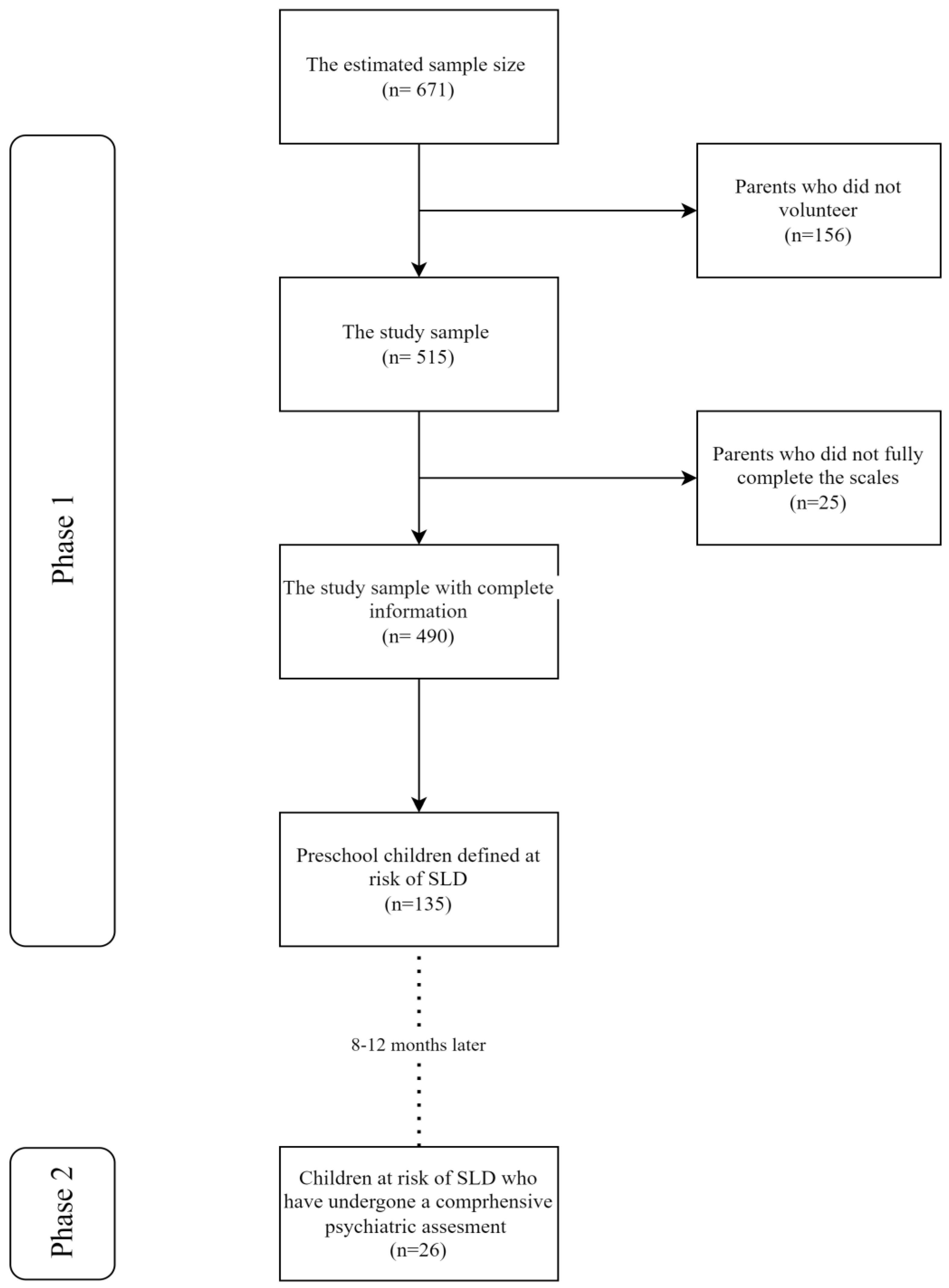
2. Materials and Methods
2.1. Assessment Tools
2.2. Statistical Analysis
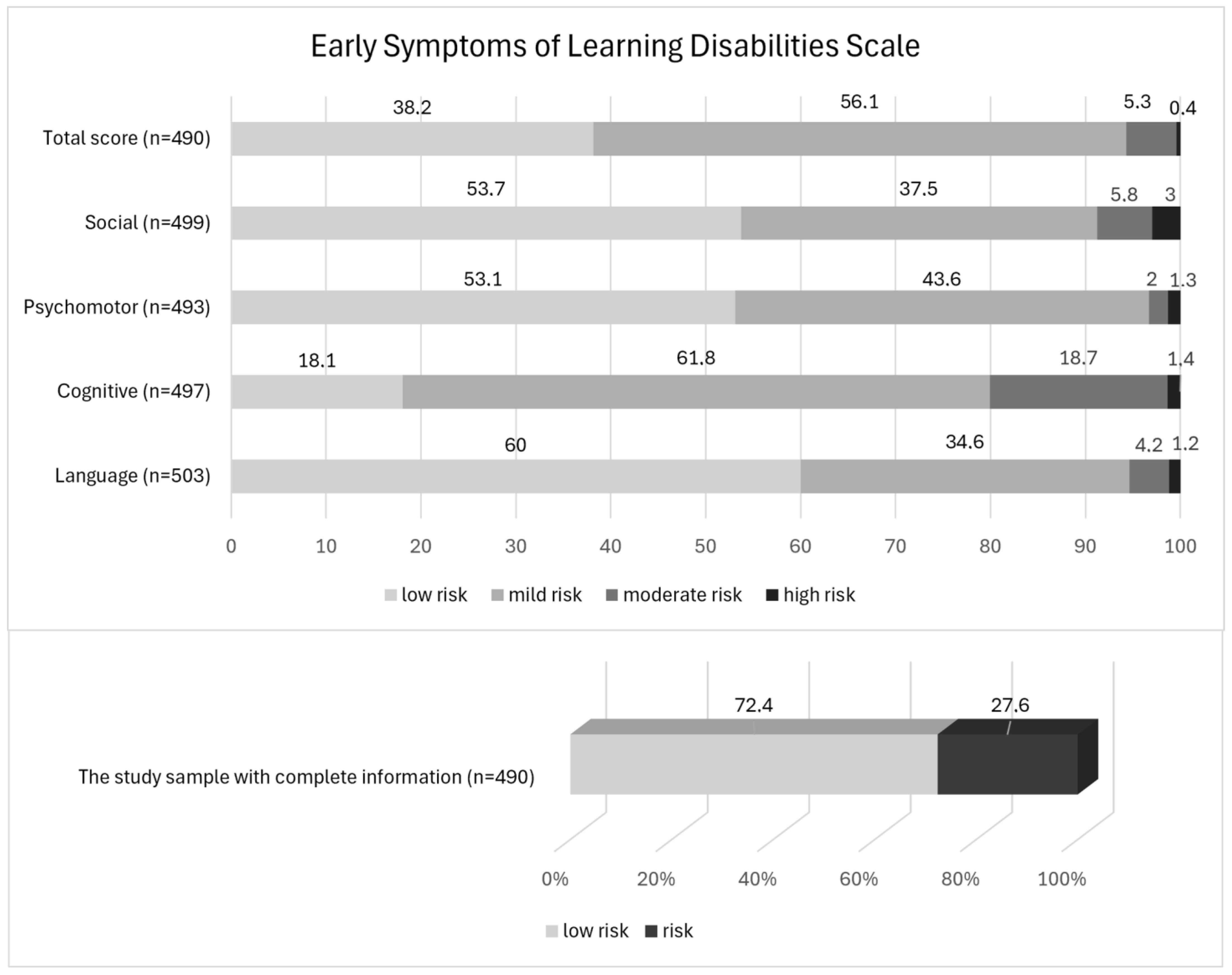
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Al-Yagon, M.; Cavendish, W.; Cornoldi, C.; Fawcett, A.J.; Grünke, M.; Hung, L.-Y.; Jiménez, J.E.; Karande, S.; van Kraayenoord, C.E.; Lucangeli, D. The proposed changes for DSM-5 for SLD and ADHD: International perspectives—Australia, Germany, Greece, India, Israel, Italy, Spain, Taiwan, United Kingdom, and United States. J. Learn. Disabil. 2013, 46, 58–72. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Scaria, L.M.; Bhaskaran, D.; George, B. Prevalence of Specific Learning Disorders (SLD) among children in India: A systematic review and meta-analysis. Indian J. Psychol. Med. 2023, 45, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Altarac, M.; Saroha, E. Lifetime prevalence of learning disability among US children. Pediatrics 2007, 119 (Suppl. S1), 77–83. [Google Scholar] [CrossRef] [PubMed]
- Fortes, I.S.; Paula, C.S.; Oliveira, M.C.; Bordin, I.A.; de Jesus Mari, J.; Rohde, L.A. A cross-sectional study to assess the prevalence of DSM-5 specific learning disorders in representative school samples from the second to sixth grade in Brazil. Eur. Child Adolesc. Psychiatry 2016, 25, 195–207. [Google Scholar] [CrossRef] [PubMed]
- Mustard, J.F. Early Child Development and the Brain-the Base for Health, Learning, and Behavior Throughout Life. In From Early Child Development to Human Development: Investing in Our Children’s Future; Young, M., Ed.; World Bank: Washington, DC, USA, 2002; pp. 23–61. [Google Scholar]
- Balikci, O.S.; Melekoglu, M.A. Early signs of specific learning disabilities in early childhood. Int. J. Early Child. Spec. Educ. 2020, 12, 84–95. [Google Scholar] [CrossRef]
- Aslan, K. Review on Early Symptoms of Specific Learning Disability and Early Intervention Practices. Hacet. Univ. Fac. Health Sci. J. 2015, 1, 577–588. [Google Scholar]
- Firat, T.; Bildiren, A. Developmental characteristics of children with learning disabilities aged 0–6 based on parental observations. Curr. Psychol. 2024, 43, 2909–2921. [Google Scholar] [CrossRef]
- Şentürk Gülhan, N.; Burak, Y. Investigation of the Relationship between Early Symptoms of Learning Disability of Preschool Children and Early Literacy and Executive Functioning Skills. J. Mother Tongue Educ. 2023, 11, 707–729. [Google Scholar]
- Schneider, W.; Ennemoser, M.; Roth, E.; Küspert, P. Kindergarten Prevention Od Dyslexia:Does Training İn Phonological Awareness Work For Everybody. J. Learn. Disabil. 1999, 32, 429–436. [Google Scholar] [CrossRef]
- Metwally, A.M.; Aboulghate, A.; Elshaarawy, G.A.; Abdallah, A.M.; Abdel Raouf, E.R.; El-Din, E.M.S.; ElRifay, A.S. Prevalence and Risk Factors of Disabilities among Egyptian Preschool Children: A Community-based Population Study. BMC Psychiatry 2023, 23, 689. [Google Scholar] [CrossRef]
- Mercer, C.D. Students with Learning Disabilities; Merrill: St Princeton, NC, USA, 1997. [Google Scholar]
- Görker, I.; Bozatli, L.; Korkmazlar, Ü.; Karadağ, M.Y.; Ceylan, C.; Söğüt, C.; Aykutlu, H.C.; Subay, B.; Turan, N. The Probable Prevalence and Sociodemographic Characteristics of Specific Learning Disorder in Primary School Children in Edirne. Arch. Neuropsychiatry 2017, 54, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, J.; Birmaher, B.; Brent, D.; Rao, U.M.A.; Flynn, C.; Moreci, P.; Williamson, D.; Ryan, N. Schedule for Affective Disorders and Schizophrenia for School-age Children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. J. Am. Acad. Child. Adolesc. Psychiatry 1997, 36, 980–988. [Google Scholar] [CrossRef] [PubMed]
- Ünal, F.; Öktem, F.; Çetin Çuhadaroğlu, F.; Çengel Kültür, S.E.; Akdemir, D.; Foto Özdemir, D.; Çak, H.T.; Ünal, D.; TIRAŞ, K.; Aslan, C.; et al. Reliability and Validity of the Schedule for Affective Disorders and Schizophrenia for School-age Children-present and lifetime version, DSM-5 November 2016-Turkish adaptation (K-SADS-PL-DSM-5-T). Turk Psikiyatr. Derg. 2019, 30, 1–8. [Google Scholar] [CrossRef]
- Okur, M. Determination of Psychometric Properties of Learning Disability Early Symptoms Screenıng Scale. Master’s Thesis, Department of Special Education Anadolu University, Graduate School of Educational Sciences, Eskisehir, Türkiye, 2019. [Google Scholar]
- Kausar, N.; Farhat, N.; Maqsood, F.; Qurban, H. Specific learning disorder among primary school children of Sarai Alamgir. JPMA 2021, 71, 1193. [Google Scholar]
- Kumari, R.; Ojha, A.A.R.P.; Dubey, G. Prevalence of Learning Disability among Tribal, Rural and Urban School Going Children of Eastern Uttar Pradesh. J. Nehru Gram Bharati Univ. 2018, 7, 1–10. [Google Scholar]
- Beri, N.; Singh, K.U.V. Learning Disability in India: A Review. Ensemble 2021, 1, 67–71. [Google Scholar]
- Doğan, O.; Ersan, E.; Doğan, S. The Probable Learning Disorders in Primary School Students: A preliminary study. Anadolu Psikiyatr. Derg.-Anatol. J. Psychiatry 2009, 10, 62–70. [Google Scholar]
- Visser, L.; Linkersdörfer, J.; Hasselhorn, M. The Role of ADHD Symptoms in the Relationship between Academic Achievement and Psychopathological Symptoms. Res. Dev. Disabil. 2020, 97, 103552. [Google Scholar] [CrossRef] [PubMed]
- Cantwell, D.P.; Baker, L. Association between Attention Deficit-Hyperactivity Disorder and Learning Disorders. J. Learn. Disabil. 1991, 24, 88–95. [Google Scholar] [CrossRef]
- Batstra, L.; Hadders-Algra, M.; Neeleman, J. Effect of Antenatal Exposure to Maternal Smoking on Behavioural Problems and Academic Achievement in Childhood: Prospective Evidence from a Dutch Birth Cohort. Early Hum. Dev. 2003, 75, 21–33. [Google Scholar] [CrossRef]
- Gustavson, K.; Ystrom, E.; Stoltenberg, C.; Susser, E.; Surén, P.; Magnus, P.; Knudsen, G.P.; Smith, G.D.; Langley, K.; Rutter, M. Smoking in Pregnancy and Child ADHD. Pediatrics 2017, 139, e20162509. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Chen, J.; Zhu, L.H.; Hua, L.L.; Ke, F.F. Maternal Smoking During Pregnancy and ADHD: Results from a Systematic Review and Meta-analysis of Prospective Cohort Studies. J. Atten. Disord. 2020, 24, 1637–1647. [Google Scholar] [CrossRef] [PubMed]
- Braun, J.M.; Daniels, J.L.; Kalkbrenner, A.; Zimmerman, J.; Nicholas, J.S. The Effect of Maternal Smoking During Pregnancy on Intellectual Disabilities among 8-Year-Old Children. Paediatr. Perinat. Epidemiol. 2009, 23, 482–491. [Google Scholar] [CrossRef] [PubMed]
- Fergusson, D.M.; Woodward, L.J.; Horwood, L.J. Maternal Smoking during Pregnancy and Psychiatric Adjustment in Late Adolescence. Arch. Gen. Psychiatry 1998, 55, 721–727. [Google Scholar] [CrossRef] [PubMed]
- McCoy, D.C.; Zuilkowski, S.S.; Fink, G. Poverty, Physical Stature, and Cognitive Skills: Mechanisms Underlying Children’s School Enrollment in Zambia. Dev. Psychol. 2015, 51, 600–614. [Google Scholar] [CrossRef] [PubMed]
- McCoy, D.C.; Peet, E.D.; Ezzati, M.; Danaei, G.; Black, M.M.; Sudfeld, C.R.; Fawzi, W.; Fink, G. Early Childhood Developmental Status in Low-and Middle-Income Countries: National, Regional, and Global Prevalence Estimates Using Predictive Modeling. PLoS Med. 2016, 13, e1002034. [Google Scholar] [CrossRef] [PubMed]
- Jeong, J.; McCoy, D.C.; Fink, G. Pathways between Paternal and Maternal Education, Caregivers’ Support for Learning, and Early Child Development in 44 Low-and Middle-Income Countries. Early Child. Res. Q. 2017, 41, 136–148. [Google Scholar] [CrossRef]
- Resnick, M.B.; Gomatam, S.V.; Carter, R.L.; Ariet, M.; Roth, J.; Kilgore, K.L.; Bucciarelli, R.L.; Mahan, C.S.; Curran, J.S.; Eitzman, D.V. Educational Disabilities of Neonatal Intensive Care Graduates. Pediatrics 1998, 102, 308–314. [Google Scholar] [CrossRef]
- Sell, E.J.; Gaines, J.A.; Gluckman, C.; Williams, E. Early Identification of Learning Problems in Neonatal Intensive Care Graduates. Am. J. Dis. Child. 1985, 139, 460–463. [Google Scholar] [CrossRef]
- Hamamy, H.; Antonarakis, S.E.; Cavalli-Sforza, L.L.; Temtamy, S.; Romeo, G.; Ten Kate, L.P.; Bennett, R.L.; Shaw, A.; Megarbane, A.; Van Duijn, C. Consanguineous Marriages, Pearls and Perils: Geneva International Consanguinity Workshop Report. Genet. Med. 2011, 13, 841–847. [Google Scholar] [CrossRef]
- Lakhan, R.; Bipeta, R.; Yerramilli, S.S.; Nahar, V.K. A Family Study of Consanguinity in Children with Intellectual Disabilities in Barwani, India. J. Neurosci. Rural Pract. 2017, 8, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Saad, H.A.; Elbedour, S.; Hallaq, E.; Merrick, J.; Tenenbaum, A. Consanguineous Marriage and Intellectual and Developmental Disabilities among Arab Bedouins Children of The Negev Region in Southern Israel: A Pilot Study. Front. Media 2014, 2, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Jaber, L.; Merlob, P.; Gabriel, R.; Shohat, M. Effects of Consanguineous Marriage on Reproductive Outcome in an Arab Community in Israel. J. Med. Genet. 1997, 34, 1000–1002. [Google Scholar] [CrossRef] [PubMed]
- Talaat, F.M. The Effect of Consanguineous Marriage on Reading Disability Based on Deep Neural Networks. Multimed. Tools Appl. 2023, 83, 51787–51807. [Google Scholar] [CrossRef]
- Cerniglia, L.; Cimino, S.; Ammaniti, M. What are The Effects of Screen Time on Emotion Regulation and Academic Achievements? A Three-Wave Longitudinal Study on Children From 4 to 8 Years of Age. J. Early Child. Res. 2021, 19, 145–160. [Google Scholar] [CrossRef]
- Canadian Paediatric Society. Screen Time and Young Children: Promoting Health and Development in a Digital World. Paediatr. Child Health 2017, 461–468. [Google Scholar]
- Santos, R.M.S.; Mendes, C.G.; Marques Miranda, D.; Romano-Silva, M.A. The Association between Screen Time and Attention in Children: A Systematic Review. Dev. Neuropsychol. 2022, 47, 175–192. [Google Scholar] [CrossRef]
- Lauricella, A.R.; Wartella, E.; Rideout, V.J. Young Children’s Screen Time: The Complex Role of Parent and Child Factors. J. Appl. Dev. Psychol. 2015, 36, 11–17. [Google Scholar] [CrossRef]
- Xu, H.; Wen, L.M.; Rissel, C. Associations of Parental Influences with Physical Activity and Screen Time among Young Children: A systematic review. J. Obes. 2015, 546925. [Google Scholar] [CrossRef]
- Tang, S.; Werner-Seidler, A.; Torok, M.; Mackinnon, A.J.; Christensen, H. The Relationship between Screen Time and Mental Health in Young People: A Systematic Review of Longitudinal Studies. Clin. Psychol. Rev. 2021, 86, 102021. [Google Scholar] [CrossRef]
- Blake, R.A. Parents of Children with Learning Disabilities: Attitudes toward Education. Master’s Thesis, The College at Brockport, Brockport, NY, USA, 1997. [Google Scholar]
| Age | Month | 72.5 ± 5.6 |
| Sex | Boy | 49.3% (n = 254) |
| Girl | 50.7% (n = 261) | |
| Parents who filled out the form | Mother | 88.9% (n = 458) |
| Father | 11.1% (n = 57) | |
| Siblings | Yes | 69.3% (n = 357) |
| No | 30.7% (n = 158) | |
| Number of siblings | 1 (1–3) | |
| First-born | 53.2% (n = 274) | |
| Second-born | 41% (n = 211) | |
| Third-born | 5.2% (n = 27) | |
| Fourth-born | 0.6% (n = 3) | |
| Marital Status | Together | 93.2% (n = 480) |
| Divorced | 3.5% (n = 18) | |
| Separated | 1% (n = 5) | |
| Death | 0.4% (n = 2) | |
| Missing value | 1.9% (n = 10) | |
| Number of people living in the home | 4 (2–7) | |
| Mother’s age | 35.6 ± 5.1 | |
| Mother’s job | Working | 40% (n = 298) |
| Not working | 57.9% (n = 298) | |
| Missing value | 2.1% (n = 11) | |
| Mother’s education | Illiterate | 0.4% (n = 2) |
| Literate | 0.6% (n = 3) | |
| Primary school | 6% (n = 31) | |
| Secondary school | 12% (n = 62) | |
| High school | 36.7% (n = 189) | |
| University | 42.5% (n = 219) | |
| Missing value | 1.7% (n = 9) | |
| Father’s age | 38.77 ± 5.41 | |
| Father’s job | Working | 94.4% (n = 486) |
| Not working | 3.5% (n = 18) | |
| Missing value | 2.1% (n = 11) | |
| Father’s education | Illiterate | 0.2% (n = 1) |
| Primary school | 5.4% (n = 28) | |
| Secondary school | 15.1% (n = 78) | |
| High school | 38.4% (n = 198) | |
| University | 38.7% (n = 199) | |
| Missing value | 2.1% (n = 11) | |
| Family income | Less than 5000 TL | 21.7 (n = 112) |
| 5–10,000 TL | 41.9% (n = 216) | |
| 10–15,000 TL | 21.6% (n = 111) | |
| More than 15,000 TL | 10.5% (n = 54) | |
| Missing value | 4.3% (n = 22) |
| Low-Risk Group Median (Min–Max) (n = 355) | Risk Group Median (Min–Max) (n = 135) | p a | |
|---|---|---|---|
| Language Development and Communication Skills | 3 (1–9) | 6 (1–20) | <0.001 |
| Cognitive Skills | 6 (1–9) | 10 (1–19) | <0.001 |
| Psychomotor Skills | 3 (1–9) | 6 (1–20) | <0.001 |
| Social–Emotional Skills | 3 (1–19) | 7 (1–19) | <0.001 |
| Total Score | 87 (4–131) | 120 (20–247) | <0.001 |
| Low-Risk Group (n = 355) | Risk Group (n = 135) | p | ||
|---|---|---|---|---|
| Age | Month | 72 (IQR = 6) | 71 (IQR = 7) | 0.510 MU |
| Sex | Boy | 48.2% (n = 171) | 52.6% (n = 71) | 0.382 CS |
| Girl | 51.8% (n = 184) | 47.4% (n = 64) | ||
| Siblings | Yes | 68.5% (n = 243) | 69.6% (n = 94) | 0.801 CS |
| No | 31.5% (n = 112) | 30.4% (n = 41) | ||
| Number of siblings | 1 (IQR = 0) | 1 (IQR = 0) | 0.728 MU | |
| Marital Status | Together | 94% (n = 330) | 97.7% (n = 130) | 0.325 CS |
| Divorced | 4.3% (n = 15) | 2.3% (n = 3) | ||
| Separated | 1.4% (n = 5) | 0% | ||
| Parental loss | 0.3% (n = 1) | 0% | ||
| Number of people living in the home | 4 (IQR = 1) | 4 (IQR = 1) | 0.685 MU | |
| Mother’s age | 35 (IQR = 7) | 35 (IQR = 7) | 0.370 MU | |
| Mother’s job | Working | 42.9% (n = 150) | 38.6% (n = 51) | 0.402 CS |
| Not working | 57.1% (n = 200) | 61.4% (n = 81) | ||
| Mother’s education | Low | 6.3% (n = 22) | 9.8% (n = 13) | 0.216 CS |
| Medium | 47.4% (n = 167) | 51.1% (n = 68) | ||
| High | 46.3% (n = 163) | 39.1% (n = 52) | ||
| Father’s age | 38 (IQR = 7) | 38 (IQR = 7) | 0.708 MU | |
| Father’s job | Working | 96% (n = 336) | 97.7% (n = 129) | 0.580 f |
| Not working | 4% (n = 14) | 2.3% (n = 3) | ||
| Father’s education | Low | 3.4% (n = 12) | 9.8% (n = 13) | 0.017 CS |
| Medium | 54.9% (n = 192) | 53.4% (n = 71) | ||
| High | 41.7% (n = 146) | 36.8% (n = 49) | ||
| Family income | Low | 19.6% (n = 67) | 29% (n = 38) | 0.087 CS |
| Medium | 69.6% (n = 238) | 61.1% (n = 80) | ||
| High | 10.8% (n = 37) | 9.9% (n = 13) | ||
| Planned pregnancy | yes | 81.4% (n = 289) | 79.3% (n = 107) | 0.589 CS |
| no | 18.6% (n = 66) | 20.7% (n = 28) | ||
| Assisted reproductive techniques | yes | 7.4% (n = 26) | 5.9% (n = 8) | 0.566 CS |
| no | 92.6% (n = 325) | 94.1% (n = 127) | ||
| Threat of miscarriage | yes | 15.3% (n = 54) | 16.4% (n = 22) | 0.761 CS |
| no | 84.7% (n = 299) | 83.6% (n = 112) | ||
| Medical illness in mother during pregnancy | yes | 8.2% (n = 29) | 9.6% (n = 13) | 0.618 CS |
| no | 91.8% (n = 324) | 90.4% (n = 122) | ||
| Medication use in pregnancy | yes | 28% (n = 98) | 26.1% (n = 35) | 0.678 CS |
| no | 72% (n = 252) | 73.9% (n = 99) | ||
| Smoking before pregnancy | yes | 29.6% (n = 105) | 37.8% (n = 51) | 0.082 CS |
| no | 70.4% (n = 250) | 62.2% (n = 84) | ||
| Smoking during pregnancy | yes | 5.6% (n = 20) | 13.3% (n = 18) | 0.004 CS |
| no | 94.4% (n = 335) | 86.7% (n = 117) | ||
| Alcohol use during pregnancy | yes | 0% | 0.8% (n = 1) | 0.274 f |
| no | 100% (n = 352) | 99.2% (n = 132) | ||
| Supplementary use in pregnancy | yes | 86.7% (n = 301) | 90.8% (n = 119) | 0.221 CS |
| no | 13.3% (n = 46) | 9.2% (n = 12) | ||
| Gestation | week | 38 (IQR = 1) | 38 (IQR = 1.3) | 0.627 MU |
| Birth length | cm | 50 (IQR = 4) | 50 (IQR = 3) | 0.496 MU |
| Birth weight | gr | 3300 (IQR = 680) | 3350 (IQR = 742.5) | 0.620 MU |
| Postpartum intensive care unit hospitalisation | yes | 9.1% (n = 32) | 15.6% (n = 21) | 0.039 CS |
| no | 90.9% (n = 321) | 84.4% (n = 114) | ||
| Breastfeeding | month | 18 (IQR = 18) | 18 (IQR = 18) | 0.858 MU |
| Walking milestone | month | 12 (IQR = 2) | 12 (IQR = 2.3) | 0.058 MU |
| Sentence formation milestone | month | 18 (IQR = 11.8) | 18 (IQR = 12) | 0.860 MU |
| History of epilepsy | yes | 2% (n = 7) | 3% (n = 4) | 0.506 CS |
| no | 98% (n = 346) | 97% (n = 131) | ||
| History of surgery | yes | 10.2% (n = 36) | 11.9% (n = 16) | 0.585 CS |
| no | 89.8% (n = 316) | 88.1% (n = 118) | ||
| History of head trauma | yes | 0.3% (n = 1) | 1.5% (n = 2) | 0.187 f |
| no | 99.7% (n = 351) | 98.5% (n = 133) | ||
| Hand preference | right | 84.7% (n = 300) | 88.1% (n = 119) | 0.565 CS |
| left | 10.5% (n = 37) | 8.9% (n = 12) | ||
| both | 4.8% (n = 17) | 3% (n = 4) | ||
| Screen time | minute | 180 (IQR = 120) | 210 (IQR = 150) | 0.009 MU |
| Mother’s reading milestone | 1st class with peers | 98.3% (n = 343) | 96.1% (n = 124) | 0.555 CS |
| 1st class later than peers | 0.9% (n = 3) | 1.6% (n = 2) | ||
| 2nd class | 0.6% (n = 2) | 1.6% (n = 2) | ||
| 3rd class or later | 0.3% (n = 1) | 0.8% (n = 1) | ||
| Father’s reading milestone | 1st class with peers | 98% (n = 342) | 97.7% (n = 128) | 0.750 CS |
| 1st class later than peers | 0.9% (n = 3) | 1.5% (n = 2) | ||
| 2nd class | 0.6% (n = 2) | 0.8% (n = 1) | ||
| 3rd class or later | 0.6% (n = 2) | 0% | ||
| Kinship | Yes | 1.4% (n = 5) | 5.3% (n = 7) | 0.023 f |
| No | 98.6% (n = 346) | 94.7% (n = 126) | ||
| Degree of kinship | 1st | 20% (n = 1) | 16.7% (n = 1) | 0.946 CS |
| 2nd | 40% (n = 2) | 33.3% (n = 2) | ||
| 3rd | 40% (n = 2) | 50% (n = 3) |
| B | S.E. | Wald | df | Sig. | Exp(B) | 95% I. for Exp(B) | |||
|---|---|---|---|---|---|---|---|---|---|
| Lower | Lower | ||||||||
| Father’s education | Low | 3.015 | 2 | 0.222 | |||||
| Medium | −0.887 | 0.512 | 3.001 | 1 | 0.083 | 0.412 | 0.151 | 1.124 | |
| High | −0.793 | 0.536 | 2188 | 1 | 0.139 | 0.452 | 0.158 | 1.294 | |
| Family income | Low | 0.951 | 2 | 0.622 | |||||
| Medium | −0.230 | 0.294 | 0.614 | 1 | 0.433 | 0.794 | 0.447 | 1.413 | |
| High | 0.033 | 0.449 | 0.005 | 1 | 0.941 | 1.034 | 0.429 | 2.493 | |
| Smoking before pregnancy (yes) | 0.114 | 0.272 | 0.176 | 1 | 0.674 | 1.121 | 0.658 | 1.909 | |
| Smoking during pregnancy (yes) | 0.191 | 0.456 | 0.176 | 1 | 0.675 | 1.211 | 0.496 | 2.958 | |
| Postpartum intensive care unit hospitalistion (yes) | 0.375 | 0.343 | 1.192 | 1 | 0.275 | 1.454 | 0.742 | 2.850 | |
| Walking milestone | 0.004 | 0.042 | 0.008 | 1 | 0.929 | 1.004 | 0.925 | 1.090 | |
| Screentime | 0.002 | 0.001 | 4.527 | 1 | 0.033 | 1.002 | 1.000 | 1.004 | |
| Kinship (yes) | 1.792 | 0.729 | 6.040 | 1 | 0.014 | 6.000 | 1.437 | 25.043 | |
| Constant | −0.683 | 0.783 | 0.760 | 1 | 0.383 | 0.505 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bozatlı, L.; Aykutlu, H.C.; Sivrikaya Giray, A.; Ataş, T.; Özkan, Ç.; Güneydaş Yıldırım, B.; Görker, I. Children at Risk of Specific Learning Disorder: A Study on Prevalence and Risk Factors. Children 2024, 11, 759. https://doi.org/10.3390/children11070759
Bozatlı L, Aykutlu HC, Sivrikaya Giray A, Ataş T, Özkan Ç, Güneydaş Yıldırım B, Görker I. Children at Risk of Specific Learning Disorder: A Study on Prevalence and Risk Factors. Children. 2024; 11(7):759. https://doi.org/10.3390/children11070759
Chicago/Turabian StyleBozatlı, Leyla, Hasan Cem Aykutlu, Açelya Sivrikaya Giray, Tuğçe Ataş, Çisem Özkan, Burcu Güneydaş Yıldırım, and Işık Görker. 2024. "Children at Risk of Specific Learning Disorder: A Study on Prevalence and Risk Factors" Children 11, no. 7: 759. https://doi.org/10.3390/children11070759
APA StyleBozatlı, L., Aykutlu, H. C., Sivrikaya Giray, A., Ataş, T., Özkan, Ç., Güneydaş Yıldırım, B., & Görker, I. (2024). Children at Risk of Specific Learning Disorder: A Study on Prevalence and Risk Factors. Children, 11(7), 759. https://doi.org/10.3390/children11070759






