The Etiology of Neuromuscular Hip Dysplasia and Implications for Management: A Narrative Review
Abstract
:1. Introduction
2. Materials and Methods
3. Results
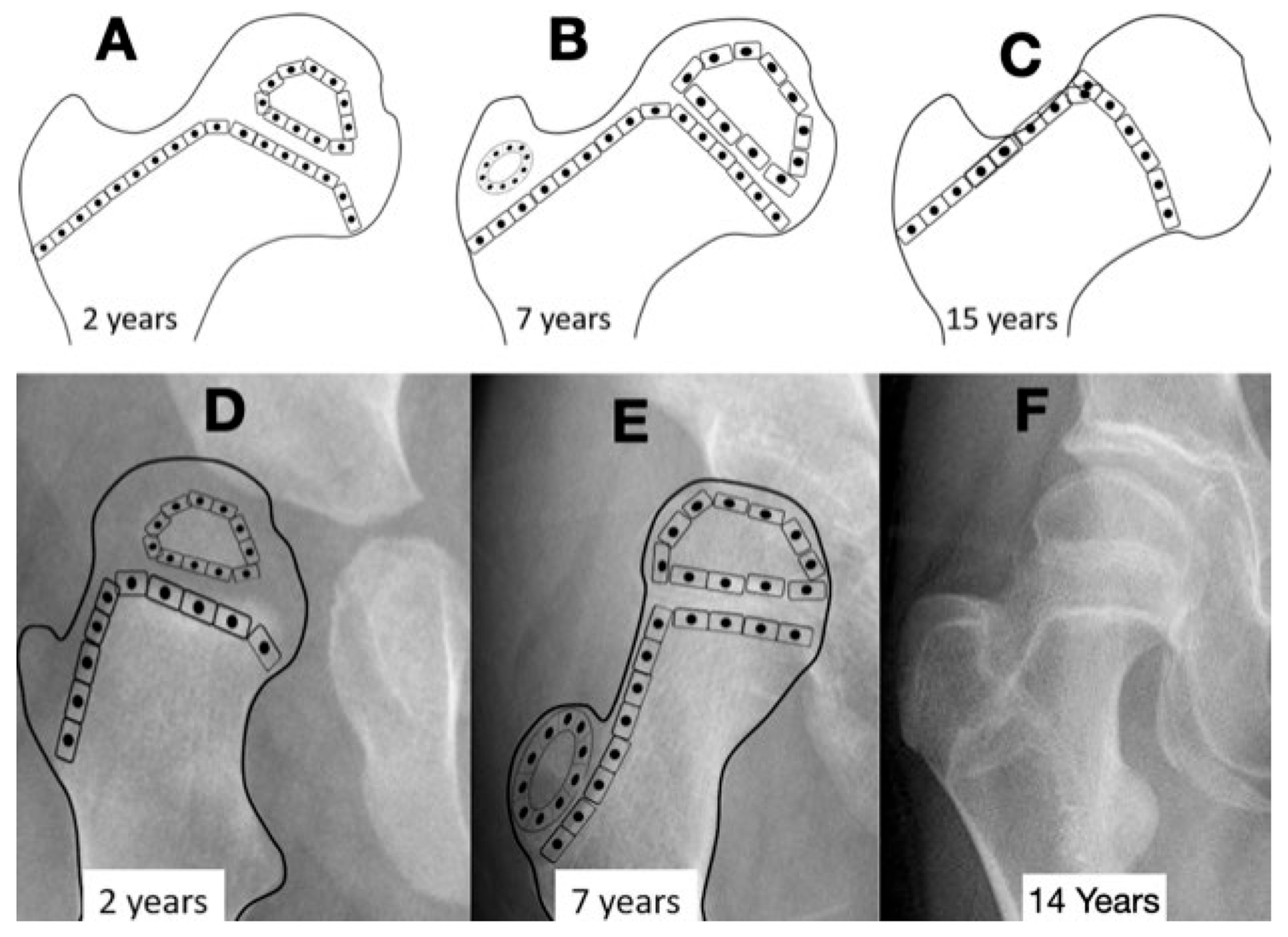
3.1. Normal Hip Development
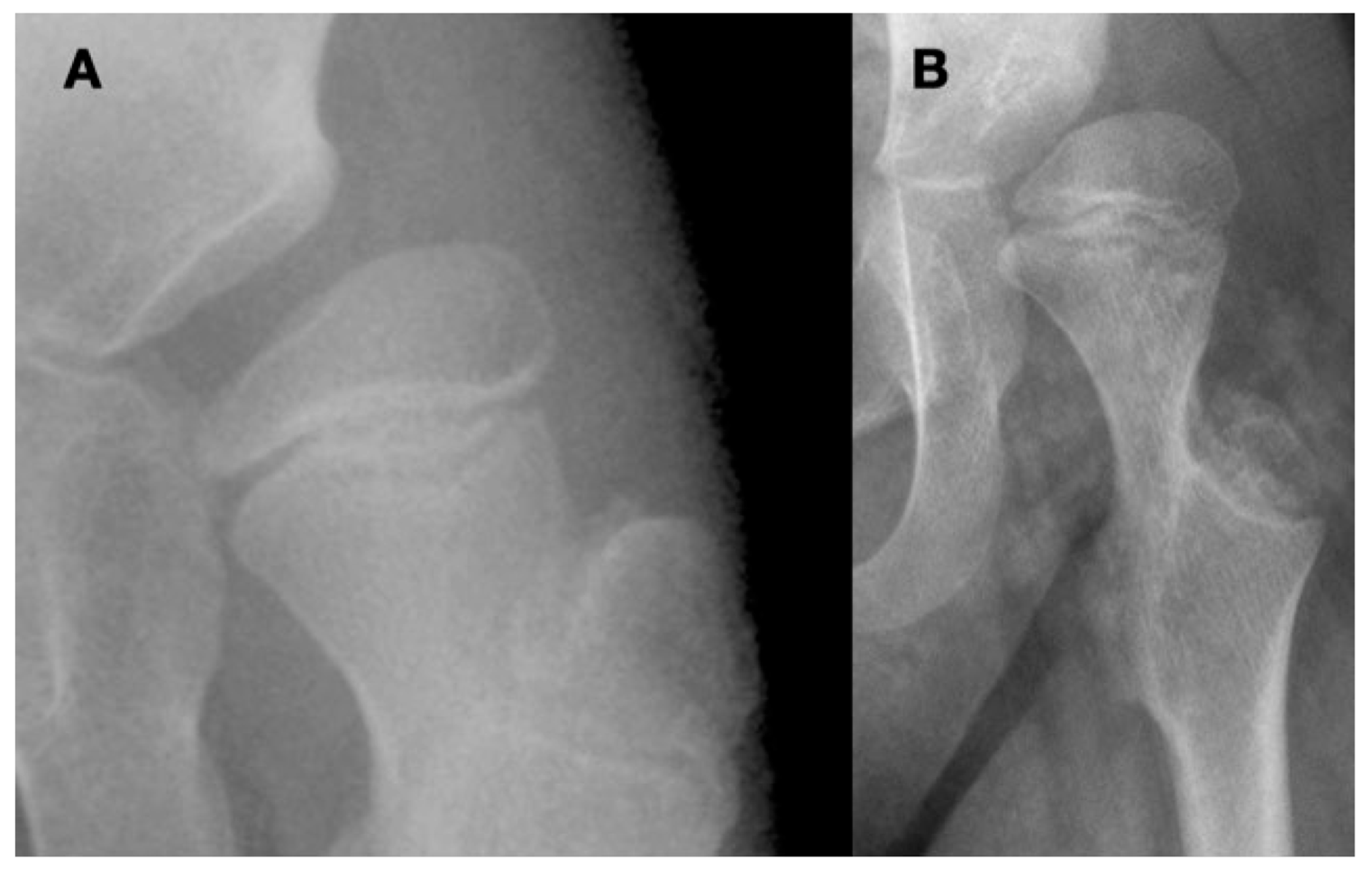
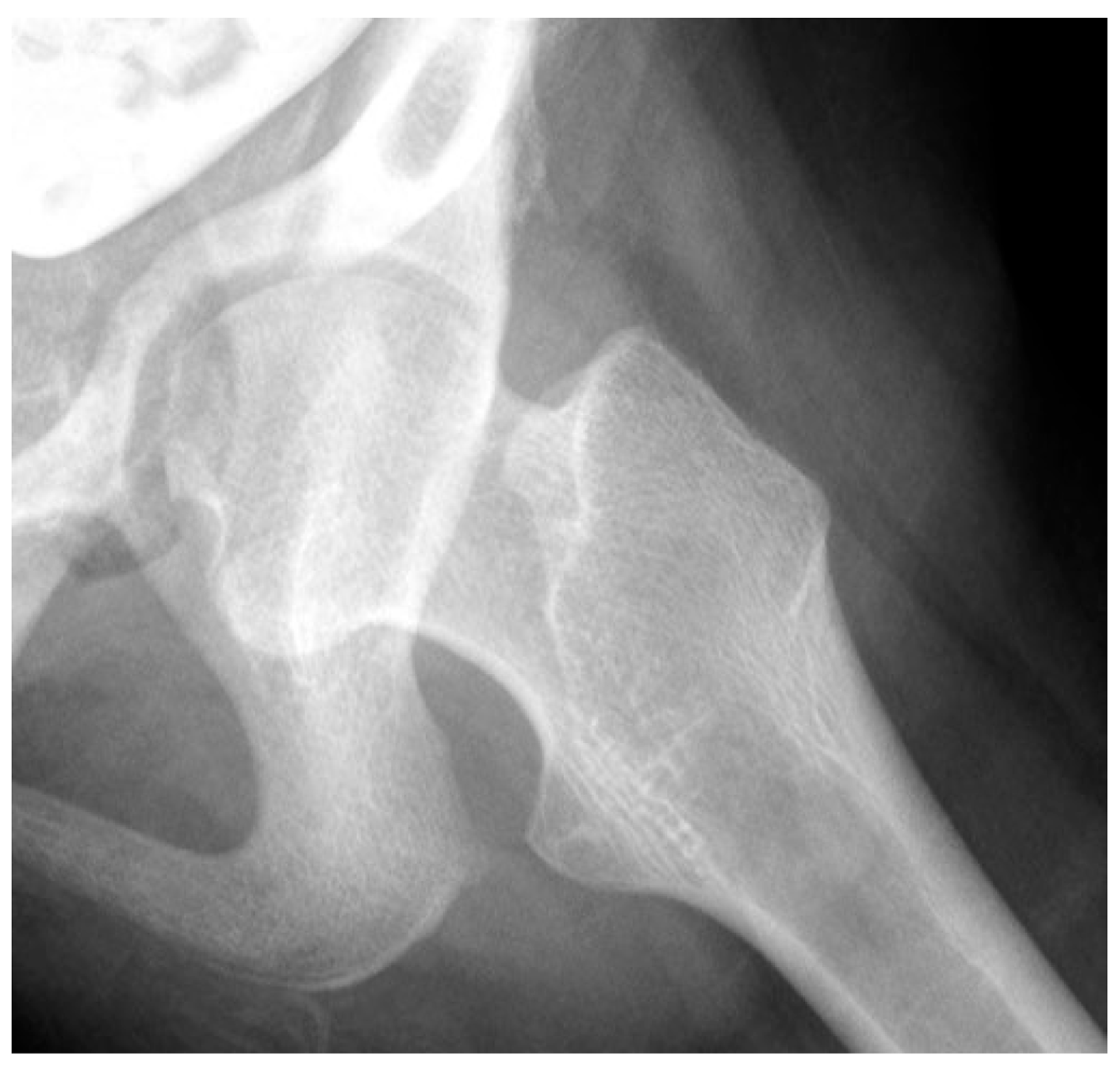
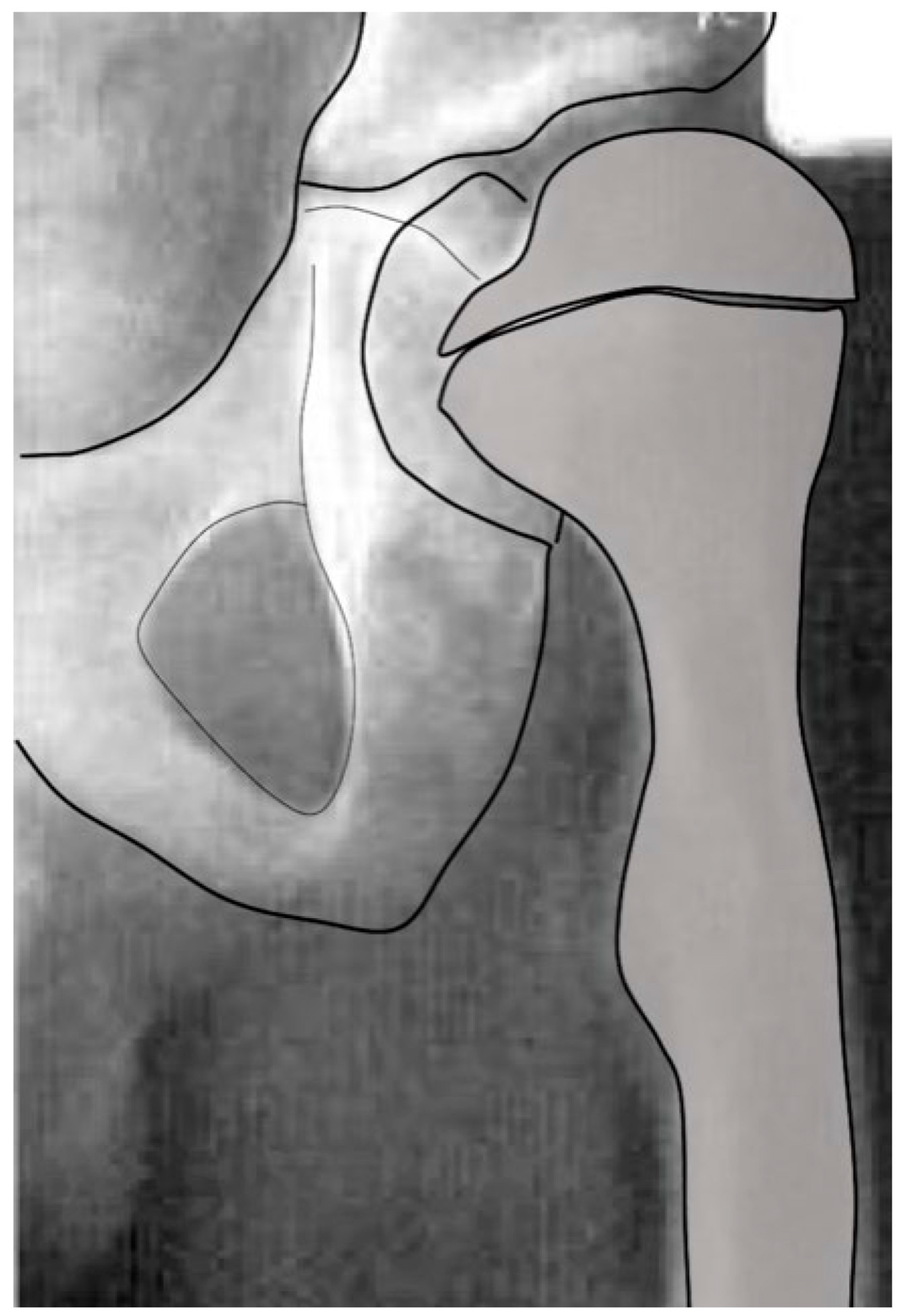
3.1.1. Proximal Femoral Development
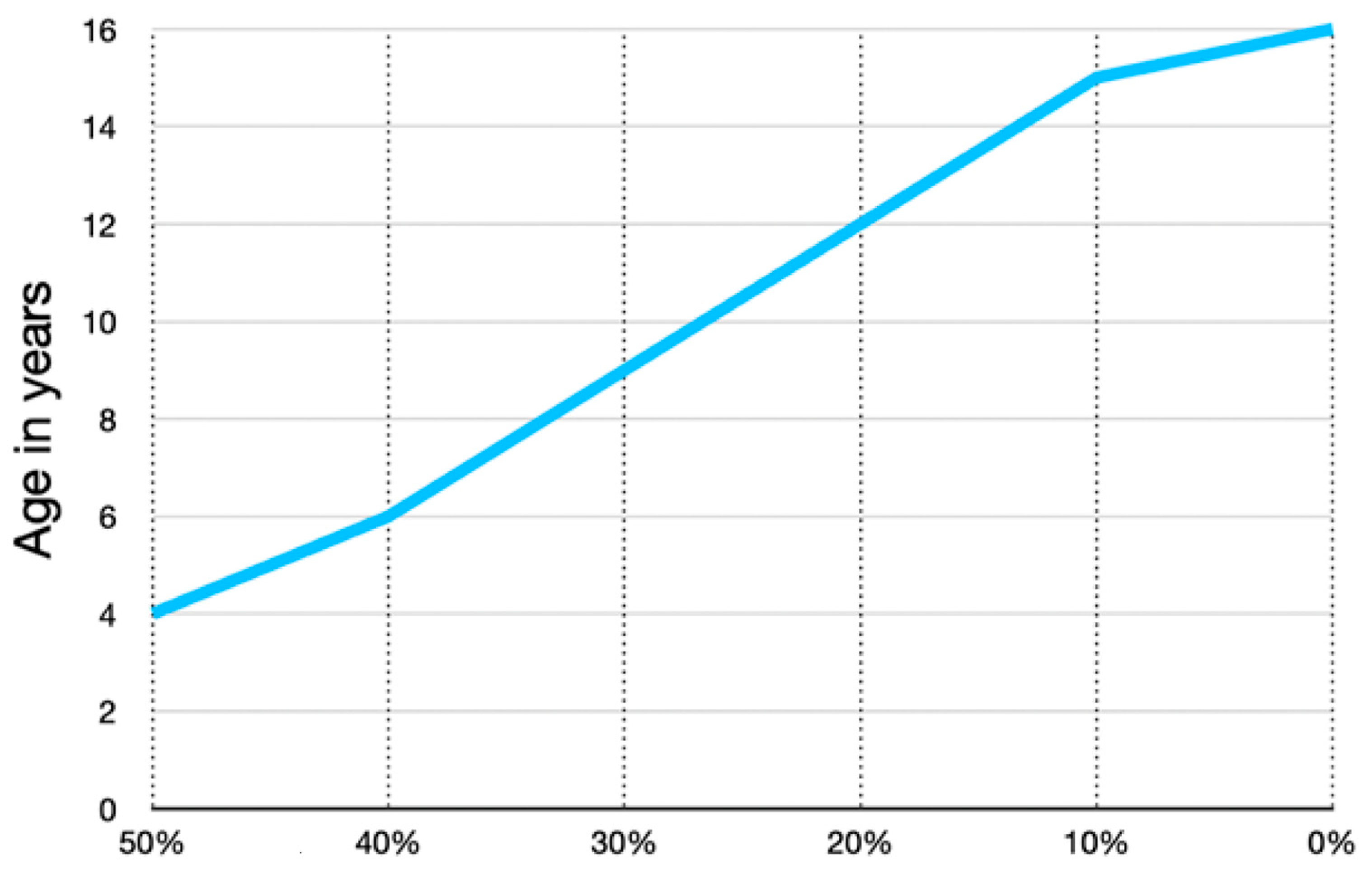
3.1.2. Development of Anteversion
3.1.3. Acetabular Development
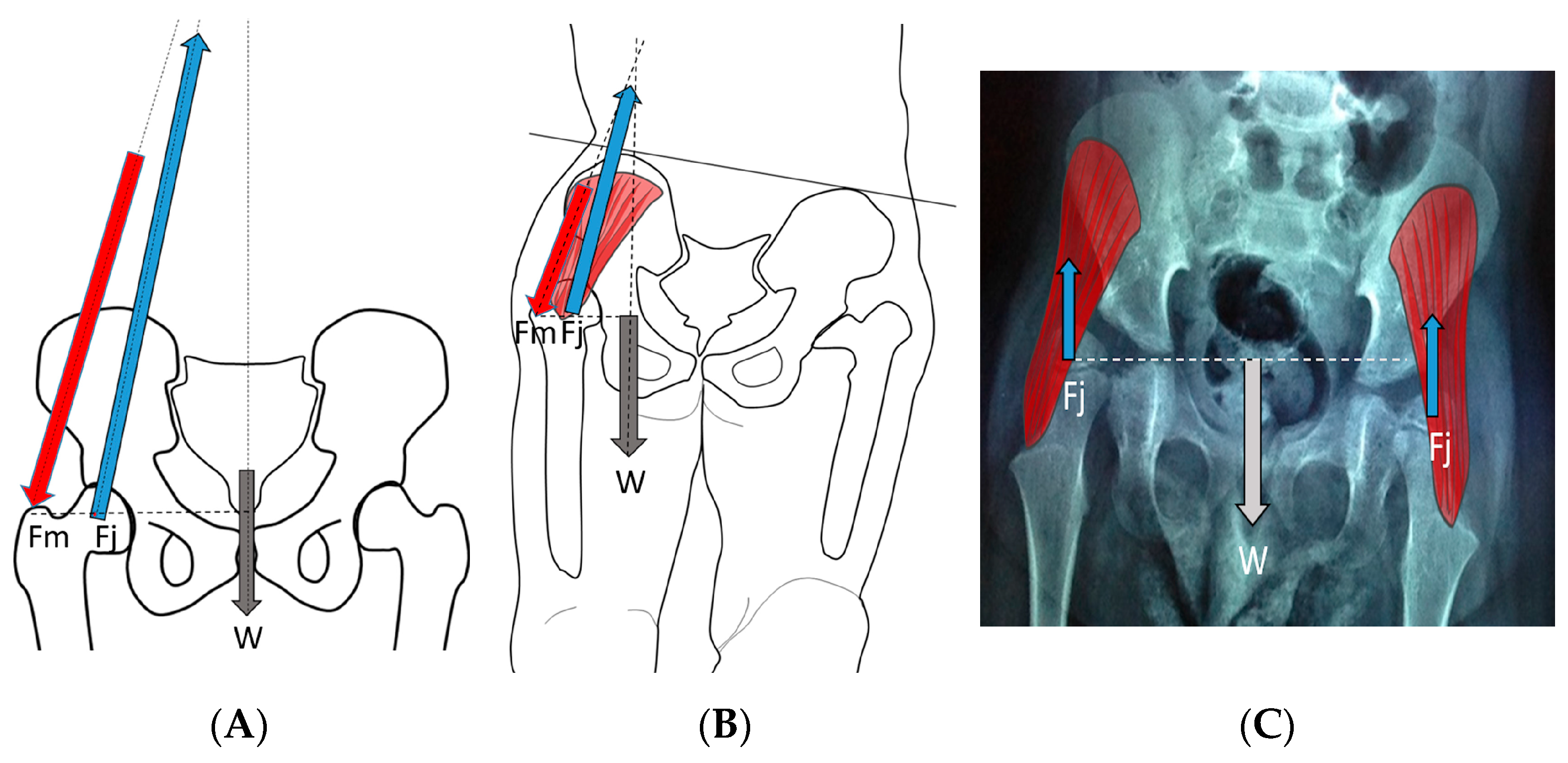
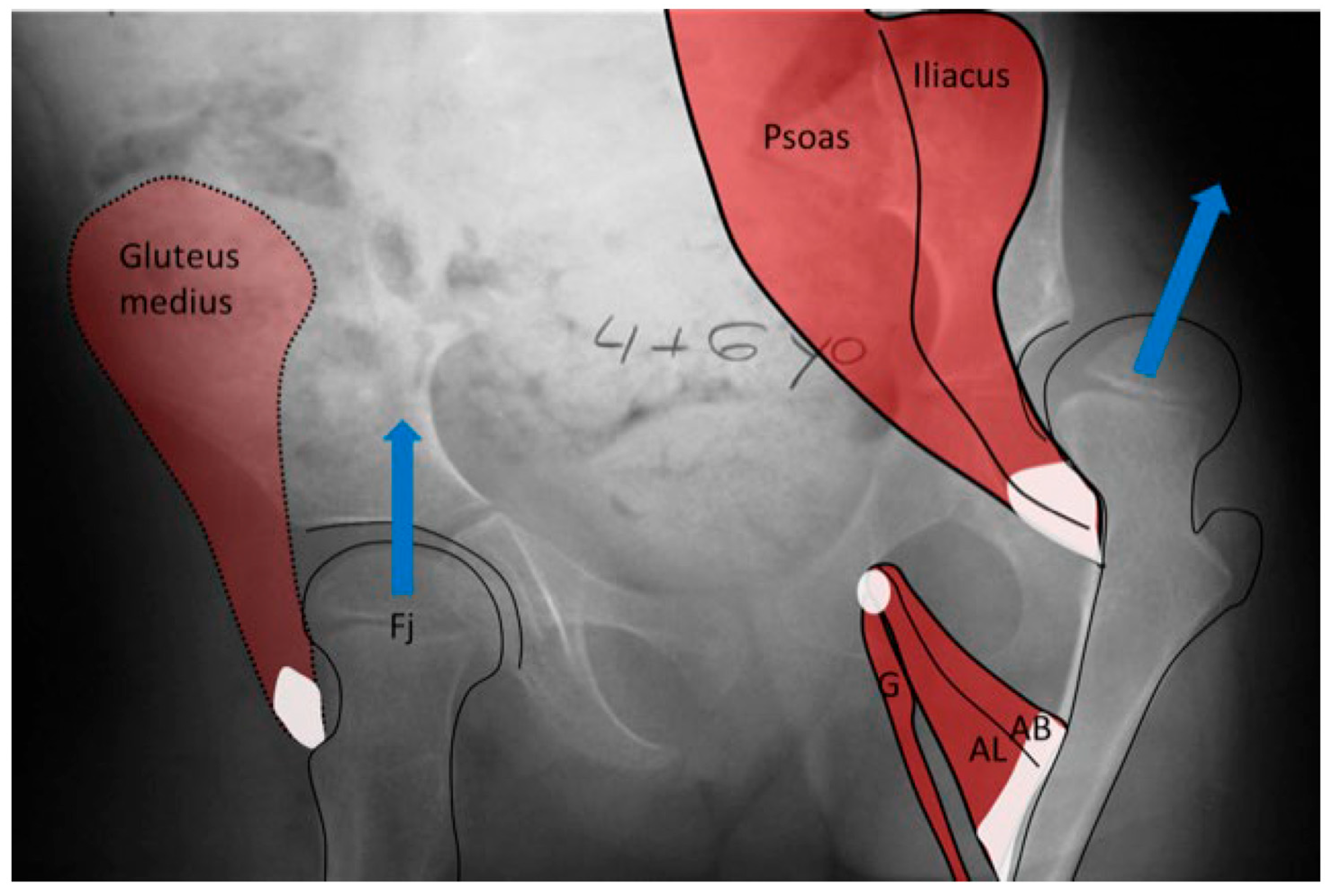
3.2. Biomechanical Considerations
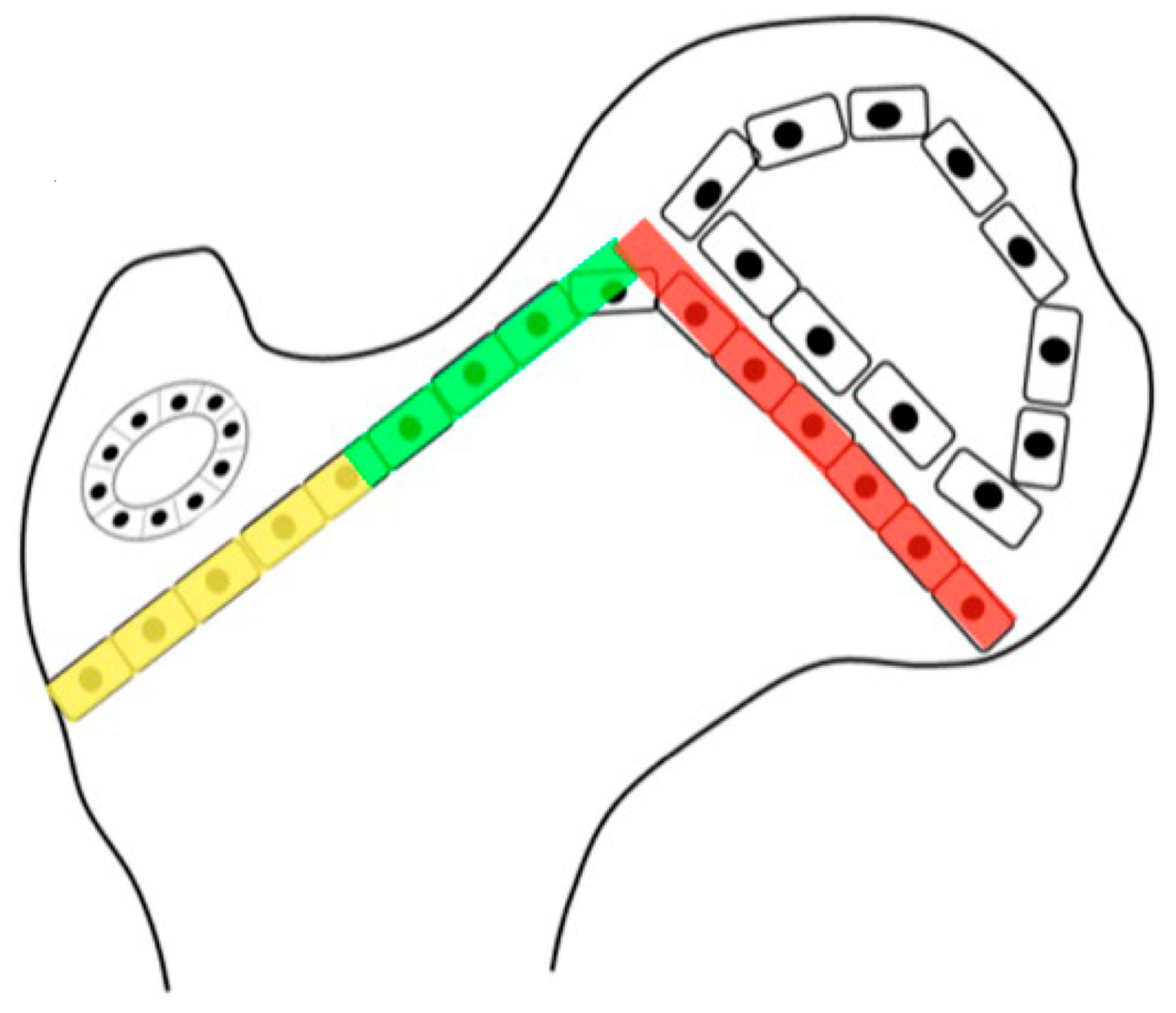
3.2.1. Normal Development
3.2.2. Biomechanical Principles Driving Femoral Shape Development
3.3. Abnormal Hip Development in Children with CP and CP-like Conditions
3.3.1. Impact of Abnormal Motor Function on Hip Development in Ambulatory Children
3.3.2. Pathology of Hip Development in Nonambulatory Children
3.3.3. Pathology of Hip Development in Children with Low Tone and Muscle Weakness
3.4. Femoral Factors Influencing Hip Pathology
3.4.1. Pathologic Role of Femoral Anteversion
3.4.2. Pathologic Role of Coxa Valga and the Impact of its Correction on Spastic Hips
4. Discussion
4.1. Principles for Management Based on Considering Primary Etiology
4.1.1. Management of the Hip with High Pathologic Force Environment
4.1.2. Pathologic Role of Coxa Valga and the Impact of its Correction in Weak and Hypotonic Hips
4.1.3. Pathologic Role of Coxa Valga and Treatment Options in Paralytic Hips
4.2. New Treatment Options
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| HJRF | hip joint reaction force |
| DDH | developmental hip dysplasia |
| CP | cerebral palsy |
| NSA | neck–shaft angle |
| HSA | head–shaft angle |
| MP | migration percentage |
| FA | femoral anteversion |
| CS | Carnegie stage |
| GMFCS | Gross Motor Function Classification System |
| SMA | spinal muscular atrophy |
References
- Ito, M.; Negishi, T.; Funayama, S.; Murakami, S.; Iizuka, S. Early detection and treatment of congenital cataracts using fetal ultrasound: A case of a newborn with a family history of congenital cataracts. Cureus 2024, 16, e53189. [Google Scholar] [CrossRef]
- Solebo, A.L.; Rahi, J.S.; British Congenital Cataract Interest Group. Delayed diagnosis of congenital cataract in preterm infants: Findings from the IoLunder2 cohort study. PLoS ONE 2023, 18, e0287658. [Google Scholar] [CrossRef] [PubMed]
- Wojciech, K.; Dudek, P.; Pulik, Ł.; Łęgosz, P. Screening of developmental dysplasia of the hip in Europe: A systematic review. Children 2024, 11, 97. [Google Scholar] [CrossRef]
- Chen, X.; Liu, J.; Xue, M.; Zou, C.; Lu, J.; Wang, X.; Teng, Y. Risk factors of developmental dysplasia of the hip in infants: A meta-analysis based on cohort studies. Orthop. Traumatol. Surg. Res. 2024, 110, 103836. [Google Scholar] [CrossRef] [PubMed]
- Hägglund, G.; Lauge-Pedersen, H.; Wagner, P. Characteristics of children with hip displacement in cerebral palsy. BMC Musculoskelet. Disord. 2007, 8, 101. [Google Scholar] [CrossRef] [PubMed]
- Dobson, F.; Boyd, R.N.; Parrott, J.; Nattrass, G.R.; Graham, H.K. Hip surveillance in children with cerebral palsy. Impact on the surgical management of spastic hip disease. J. Bone Jt. Surg. Br. 2002, 84, 720–726. [Google Scholar] [CrossRef]
- Pruszczynski, B.; Sees, J.; Miller, F. Risk factors for hip displacement in children with cerebral palsy: Systematic review. J. Pediatr. Orthop. 2016, 36, 829–833. [Google Scholar] [CrossRef] [PubMed]
- Robin, J.; Graham, H.K.; Selber, P.; Dobson, F.; Smith, K.; Baker, R. Proximal femoral geometry in cerebral palsy: A population-based cross-sectional study. J. Bone Jt. Surg. Br. 2008, 90, 1372–1379. [Google Scholar] [CrossRef] [PubMed]
- Reimers, J. The stability of the hip in children. A radiological study of the results of muscle surgery in cerebral palsy. Acta Orthop. Scand. Suppl. 1980, 184, 1–100. [Google Scholar] [CrossRef]
- Hermanson, M.; Hägglund, G.; Riad, J.; Wagner, P. Head-shaft angle is a risk factor for hip displacement in children with cerebral palsy. Acta Orthop. 2015, 86, 229–232. [Google Scholar] [CrossRef]
- Southwick, W.O. Osteotomy through the lesser trochanter for slipped capital femoral epiphysis. J. Bone Jt. Surg. Am. 1967, 49, 807–835. [Google Scholar] [CrossRef]
- Van der List, J.P.; Witbreuk, M.M.; Buizer, A.I.; van der Sluijs, J.A. The head-shaft angle of the hip in early childhood: A comparison of reference values for children with cerebral palsy and normally developing hips. Bone Jt. J. 2015, 97-B, 1291–1295. [Google Scholar] [CrossRef]
- Foroohar, A.; McCarthy, J.J.; Yucha, D.; Clarke, S.; Brey, J. Head-shaft angle measurement in children with cerebral palsy. J. Pediatr. Orthop. 2009, 29, 248–250. [Google Scholar] [CrossRef] [PubMed]
- Ohuma, E.O.; Papageorghiou, A.T.; Villar, J.; Altman, D.G. Estimation of gestational age in early pregnancy from crown-rump length when gestational age range is truncated: The case study of the INTERGROWTH-21st Project. BMC Med. Res. Methodol. 2013, 13, 151. [Google Scholar] [CrossRef]
- Suzuki, Y.; Matsubayashi, J.; Ji, X.; Yamada, S.; Yoneyama, A.; Imai, H.; Matsuda, T.; Aoyama, T.; Takakuwa, T. Morphogenesis of the femur at different stages of normal human development. PLoS ONE 2019, 14, e0221569. [Google Scholar] [CrossRef]
- Watanabe, R.S. Embryology of the human hip. Clin. Orthop. Relat. Res. 1974, 98, 8–26. [Google Scholar] [CrossRef]
- Bobroff, E.D.; Chambers, H.G.; Sartoris, D.J.; Wyatt, M.P.; Sutherland, D.H. Femoral anteversion and neck-shaft angle in children with cerebral palsy. Clin. Orthop. Relat. Res. 1999, 364, 194–204. [Google Scholar] [CrossRef] [PubMed]
- Zippel, H. Normal development of the structural elements of the hip joint in adolescence. Beitr. Orthop. Traumatol. 1971, 18, 255–270. [Google Scholar]
- Scorcelletti, M.; Reeves, N.D.; Rittweger, J.; Ireland, A. Femoral anteversion: Significance and measurement. J. Anat. 2020, 237, 811–826. [Google Scholar] [CrossRef]
- Pritchett, J.W. Longitudinal growth and growth-plate activity in the lower extremity. Clin. Orthop. Relat. Res. 1992, 275, 274–279. [Google Scholar] [CrossRef]
- Vafaeian, B.; Zonoobi, D.; Mabee, M.; Hareendranathan, A.; El-Rich, M.; Adeeb, S.; Jaremko, J. Finite element analysis of mechanical behavior of human dysplastic hip joints: A systematic review. Osteoarthr. Cartil. 2017, 25, 438–447. [Google Scholar] [CrossRef] [PubMed]
- Yadav, P.; Fernandez, M.P.; Gutierrez-Farewik, E.M. Influence of loading direction due to physical activity on proximal femoral growth tendency. Med. Eng. Phys. 2021, 90, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Brien, E.W.; Lane, J.M.; Healey, J. Progressive coxa valga after childhood excision of the hip abductor muscles. J. Pediatr. Orthop. 1995, 15, 95–97. [Google Scholar] [CrossRef] [PubMed]
- Teichtahl, A.J.; Wluka, A.E.; Wijethilake, P.; Wang, Y.; Ghasem-Zadeh, A.; Cicuttini, F.M. Wolff’s law in action: A mechanism for early knee osteoarthritis. Arthritis Res. Ther. 2015, 17, 207. [Google Scholar] [CrossRef] [PubMed]
- Carriero, A.; Jonkers, I.; Shefelbine, S.J. Mechanobiological prediction of proximal femoral deformities in children with cerebral palsy. Comput. Methods Biomech. Biomed. Engin. 2011, 14, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Yadav, P.; Shefelbine, S.J.; Pontén, E.; Gutierrez-Farewik, E.M. Influence of muscle groups’ activation on proximal femoral growth tendency. Biomech. Model. Mechanobiol. 2017, 16, 1869–1883. [Google Scholar] [CrossRef] [PubMed]
- Stokes, I.A.F. Mechanical effects on skeletal growth. J. Musculoskelet. Neuronal Interact. 2002, 2, 277–280. [Google Scholar] [PubMed]
- Bosmans, L.; Wesseling, M.; Desloovere, K.; Molenaers, G.; Scheys, L.; Jonkers, I. Hip contact force in presence of aberrant bone geometry during normal and pathological gait. J. Orthop. Res. 2014, 32, 1406–1415. [Google Scholar] [CrossRef] [PubMed]
- Bombelli, R.; Gerundini, M.; Aronson, J. The biomechanical basis for osteotomy in the treatment of osteoarthritis of the hip: Results in younger patients. Hip 1984, 18–42. [Google Scholar]
- Miller, F.; Slomczykowski, M.; Cope, R.; Lipton, G.E. Computer modeling of the pathomechanics of spastic hip dislocation in children. J. Pediatr. Orthop. 1999, 19, 486–492. [Google Scholar] [CrossRef]
- Chang, C.H.; Wang, Y.C.; Ho, P.C.; Hwang, A.W.; Kao, H.K.; Lee, W.C.; Yang, W.E.; Kuo, K.N. Determinants of hip displacement in children with cerebral palsy. Clin. Orthop. Relat. Res. 2015, 473, 3675–3681. [Google Scholar] [CrossRef] [PubMed]
- Owiny, J.R.; Vandewoude, S.; Painter, J.T.; Norrdin, R.W.; Veeramachaneni, D.N. Hip dysplasia in rabbits: Association with nest box flooring. Comp. Med. 2001, 51, 85–88. [Google Scholar] [PubMed]
- Shefelbine, S.J.; Carter, D.R. Mechanobiological predictions of growth front morphology in developmental hip dysplasia. J. Orthop. Res. 2004, 22, 346–352. [Google Scholar] [CrossRef]
- Heimkes, B.; Posel, P.; Plitz, W.; Zimmer, M. Age-related force distribution at the proximal end of the femur in normally growing children. Z. Orthopädie Grenzgeb. 1997, 135, 17–23. [Google Scholar] [CrossRef]
- Heimkes, B.; Posel, P.; Plitz, W. Biomechanics of the hip joint in children. Z. Orthop. Grenzgeb. 1995, 133, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Heimkes, B.; Posel, P.; Plitz, W.; Jansson, V. Forces acting on the juvenile hip joint in the one-legged stance. J. Pediatr. Orthop. 1993, 13, 431–436. [Google Scholar] [CrossRef]
- Palisano, R.J.; Hanna, S.E.; Rosenbaum, P.L.; Russell, D.J.; Walter, S.D.; Wood, E.P.; Raina, P.S.; Galuppi, B.E. Validation of a model of gross motor function for children with cerebral palsy. Phys. Ther. 2000, 80, 974–985. [Google Scholar] [CrossRef] [PubMed]
- Gose, S.; Sakai, T.; Shibata, T.; Murase, T.; Yoshikawa, H.; Sugamoto, K. Morphometric analysis of the femur in cerebral palsy: 3-dimensional CT study. J. Pediatr. Orthop. 2010, 30, 568–574. [Google Scholar] [CrossRef]
- Brunner, R.; Picard, C.; Robb, J. Morphology of the acetabulum in hip dislocations caused by cerebral palsy. J. Pediatr. Orthop. B 1997, 6, 207–211. [Google Scholar] [CrossRef]
- Ulusaloglu, A.C.; Asma, A.; Rogers, K.J.; Shrader, M.W.; Graham, H.K.; Howard, J.J. The influence of tone on proximal femoral and acetabular geometry in neuromuscular hip displacement: A comparison of cerebral palsy and spinal muscular atrophy. J. Child. Orthop. 2022, 16, 121–127. [Google Scholar] [CrossRef]
- Simon, A.L., Jr.; Presedo, A.; Ilharreborde, B.; Mallet, C.; Mazda, K.; Penneçot, G.F. Can turned inward patella predict an excess of femoral anteversion during gait in spastic diplegic children? J. Pediatr. Orthop. 2014, 34, 405–410. [Google Scholar] [CrossRef]
- Cho, Y.; Park, E.S.; Park, H.K.; Park, J.E.; Rha, D.W. Determinants of hip and femoral deformities in children with spastic cerebral palsy. Ann. Rehabil. Med. 2018, 42, 277–285. [Google Scholar] [CrossRef]
- Lindén, O.; Hägglund, G.; Rodby-Bousquet, E.; Wagner, P. The development of spasticity with age in 4162 children with cerebral palsy: A register-based prospective cohort study. Acta Orthop. 2019, 90, 286–291. [Google Scholar] [CrossRef]
- Chougule, S.; Dabis, J.; Petrie, A.; Daly, K.; Gelfer, Y. Is head-shaft angle a valuable continuous risk factor for hip migration in cerebral palsy? J. Child. Orthop. 2016, 10, 651–656. [Google Scholar] [CrossRef]
- Hanna, S.E.; Rosenbaum, P.L.; Bartlett, D.J.; Palisano, R.J.; Walter, S.D.; Avery, L.; Russell, D.J. Stability and decline in gross motor function among children and youth with cerebral palsy aged 2 to 21 years. Dev. Med. Child. Neurol. 2009, 51, 295–302. [Google Scholar] [CrossRef]
- Shore, B.J.; Yu, X.; Desai, S.; Selber, P.; Wolfe, R.; Graham, H.K. Adductor surgery to prevent hip displacement in children with cerebral palsy: The predictive role of the Gross Motor Function Classification System. J. Bone Jt. Surg. Am. 2012, 94, 326–334. [Google Scholar] [CrossRef]
- Presedo, A.; Oh, C.W.; Dabney, K.W.; Miller, F. Soft-tissue releases to treat spastic hip subluxation in children with cerebral palsy. J. Bone Jt. Surg. Am. 2005, 87, 832–841. [Google Scholar] [CrossRef]
- Kiapekos, N.; Broström, E.; Hägglund, G.; Åstrand, P. Primary surgery to prevent hip dislocation in children with cerebral palsy in Sweden: A minimum 5-year follow-up by the national surveillance program (CPUP). Acta Orthop. 2019, 90, 495–500. [Google Scholar] [CrossRef]
- Davids, J.R.; Gibson, T.W.; Pugh, L.I.; Hardin, J.W. Proximal femoral geometry before and after varus rotational osteotomy in children with cerebral palsy and neuromuscular hip dysplasia. J. Pediatr. Orthop. 2013, 33, 182–189. [Google Scholar] [CrossRef]
- Minaie, A.; Gordon, J.E.; Schoenecker, P.; Hosseinzadeh, P. Failure of hip reconstruction in children with cerebral palsy: What are the risk factors? J. Pediatr. Orthop. 2022, 42, e78–e82. [Google Scholar] [CrossRef]
- Braatz, F.; Staude, D.; Klotz, M.C.; Wolf, S.I.; Dreher, T.; Lakemeier, S. Hip-joint congruity after Dega osteotomy in patients with cerebral palsy: Long-term results. Int. Orthop. 2016, 40, 1663–1668. [Google Scholar] [CrossRef]
- Chen, B.J.P.; Çobanoğlu, M.; Sees, J.P.; Rogers, K.J.; Miller, F. Recurrent hip instability after hip reconstruction in cerebral palsy children with spastic hip disease. J. Orthop. Sci. 2023, 28, 156–160. [Google Scholar] [CrossRef]
- Chang, F.M.; Ma, J.; Pan, Z.; Ingram, J.D.; Novais, E.N. Acetabular remodeling after a varus derotational osteotomy in children with cerebral palsy. J. Pediatr. Orthop. 2016, 36, 198–204. [Google Scholar] [CrossRef]
- Nowlan, N.C.; Chandaria, V.; Sharpe, J. Immobilized chicks as a model system for early-onset developmental dysplasia of the hip. J. Orthop. Res. 2014, 32, 777–785. [Google Scholar] [CrossRef]
- Yadav, P.; Shefelbine, S.J.; Gutierrez-Farewik, E.M. Effect of growth plate geometry and growth direction on prediction of proximal femoral morphology. J. Biomech. 2016, 49, 1613–1619. [Google Scholar] [CrossRef]
- Sporer, S.M.; Smith, B.G. Hip dislocation in patients with spinal muscular atrophy. J. Pediatr. Orthop. 2003, 23, 10–14. [Google Scholar] [CrossRef]
- Thompson, R.M.; Foley, J.; Dias, L.; Swaroop, V.T. Hip status and long-term functional outcomes in spina bifida. J. Pediatr. Orthop. 2019, 39, e168–e172. [Google Scholar] [CrossRef]
- Carson, V.J.; Young, M.; Brigatti, K.W.; Robinson, D.L.; Reed, R.M.; Sohn, J.; Petrillo, M.; Farwell, W.; Miller, F.; Strauss, K.A. Nusinersen by subcutaneous intrathecal catheter for symptomatic spinal muscular atrophy patients with complex spine anatomy. Muscle Nerve 2022, 65, 51–59. [Google Scholar] [CrossRef]
- Hsu, C.M.; Sheu, H.; Lee, W.C.; Kao, H.K.; Yang, W.E.; Chang, C.H. Soft tissue releases with simultaneous guided growth decrease risk of spastic hip displacement recurrence. J. Pediatr. Orthop. 2023, 43, e707–e712. [Google Scholar] [CrossRef]
- Lebe, M.; van Stralen, R.A.; Buddhdev, P. Guided growth of the proximal femur for the management of the ‘hip at risk’ in children with cerebral palsy-a systematic review. Children 2022, 9, 609. [Google Scholar] [CrossRef] [PubMed]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Presedo, A.; Rutz, E.; Howard, J.J.; Shrader, M.W.; Miller, F. The Etiology of Neuromuscular Hip Dysplasia and Implications for Management: A Narrative Review. Children 2024, 11, 844. https://doi.org/10.3390/children11070844
Presedo A, Rutz E, Howard JJ, Shrader MW, Miller F. The Etiology of Neuromuscular Hip Dysplasia and Implications for Management: A Narrative Review. Children. 2024; 11(7):844. https://doi.org/10.3390/children11070844
Chicago/Turabian StylePresedo, Ana, Erich Rutz, Jason J. Howard, Michael Wade Shrader, and Freeman Miller. 2024. "The Etiology of Neuromuscular Hip Dysplasia and Implications for Management: A Narrative Review" Children 11, no. 7: 844. https://doi.org/10.3390/children11070844
APA StylePresedo, A., Rutz, E., Howard, J. J., Shrader, M. W., & Miller, F. (2024). The Etiology of Neuromuscular Hip Dysplasia and Implications for Management: A Narrative Review. Children, 11(7), 844. https://doi.org/10.3390/children11070844






