Radiological Screening of Atlantoaxial Instability in Children with Trisomy 21: A Systematic Review and Evidence-Based Recommendations
Abstract
1. Introduction
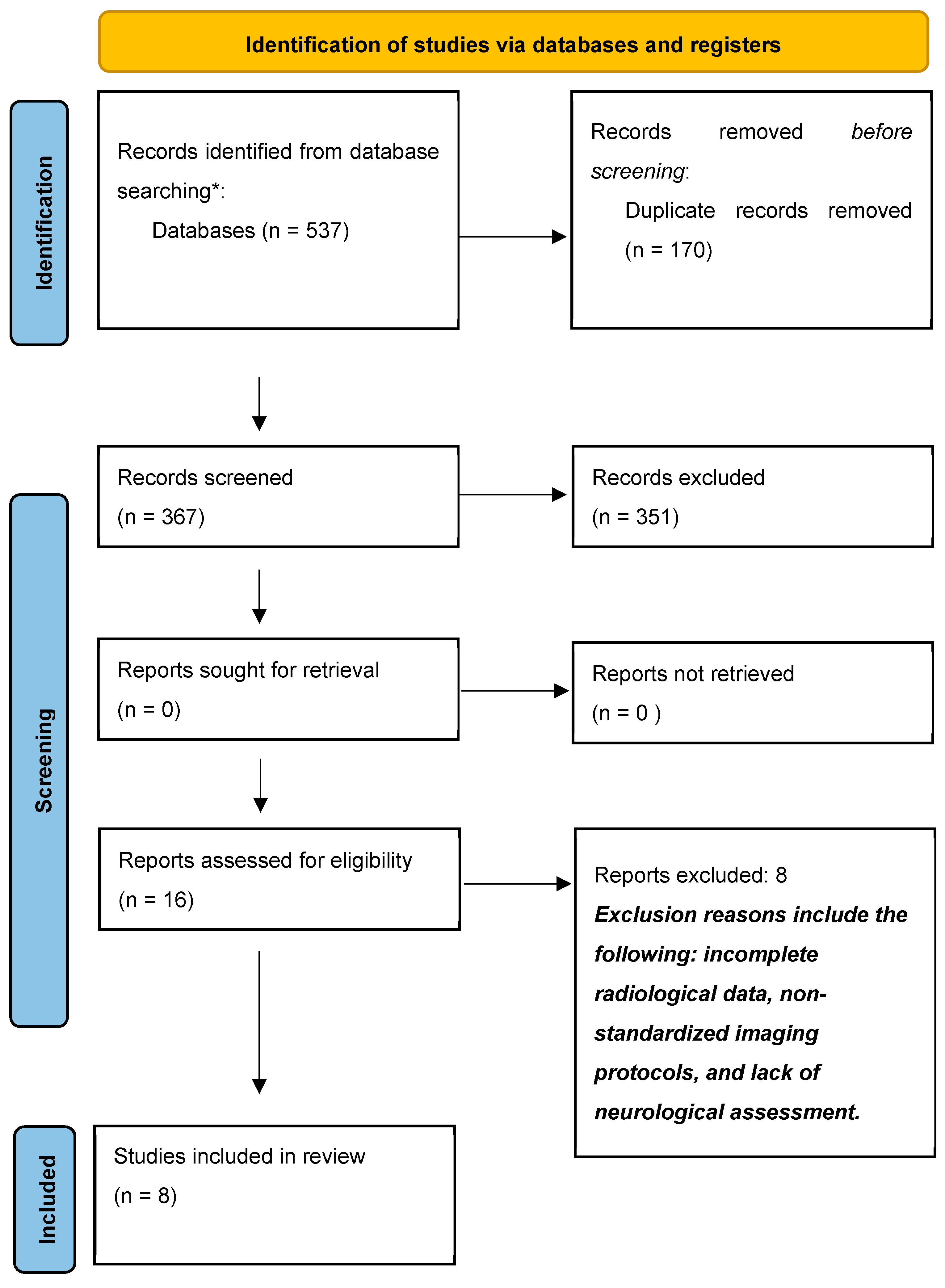
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
2.2. Study Selection
- The study explicitly discussed whether screening was recommended.
- The study clearly defined the radiological definition of AAI.
- The study reported at least 2 cases of children with AAI. This threshold was chosen to ensure that studies included a minimum level of patient data for meaningful analysis, reducing bias from isolated case reports.
- The study only included participants under 25 years old, with a mean age under 18.
- The study only included participants with a confirmed diagnosis of Trisomy 21.
2.3. Data Collection Process
- Study design (case reports, case–control, double-blind studies, prospective or retrospective studies);
- Demographic data (age, biological sex);
- Definition of AAI used by the authors;
- Identified biases;
- Screening implementation (yes or no);
- Types of screening methods.
3. Results
4. Discussion
4.1. Biases and Limitations
4.2. Clinical Implications
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
| AAI | Atlantoaxial instability |
| OO | Os odontoidum |
| SAC | Space available for cord |
| ADI | Atlanto-dental interval |
| BAI | Basion-axial interval |
References
- Morris, J.K.; Mutton, D.E.; Alberman, E. Revised estimates of the maternal age specific live birth prevalence of Down’s syndrome. J. Med. Screen. 2002, 9, 2–6. [Google Scholar] [PubMed]
- d’Ardhuy, X.L.; Edgin, J.O.; Bouis, C.; de Sola, S.; Goeldner, C.; Kishnani, P.; Nöldeke, J.; Rice, J.; Sacco, S.; Squassante, L.; et al. Assessment of Cognitive Scales to Examine Memory, Executive Function and Language in Individuals with Down Syndrome: Implications of a 6-month Observational Study. Front. Behav. Neurosci. 2015, 9, 300. [Google Scholar]
- Bergström, S.; Carr, H.; Petersson, G.; Stephansson, O.; Bonamy, A.-K.E.; Dahlström, A.; Halvorsen, C.P.; Johansson, S. Trends in Congenital Heart Defects in Infants with Down Syndrome. Pediatrics 2016, 138, e20160123. [Google Scholar] [CrossRef] [PubMed]
- Antonarakis, S.E.; Skotko, B.G.; Rafii, M.S.; Strydom, A.; Pape, S.E.; Bianchi, D.W.; Sherman, S.L.; Reeves, R.H. Down syndrome. Nat. Rev. Dis. Primers 2020, 6, 9. [Google Scholar] [CrossRef] [PubMed]
- LaCombe, J.M.; Roper, R.J. Skeletal dynamics of Down syndrome: A developing perspective. Bone 2020, 133, 115215. [Google Scholar] [PubMed]
- Stein, S.M.; Kirchner, S.G.; Horev, G.; Hernanz-Schulman, M. Atlanto-occipital subluxation in Down syndrome. Pediatr. Radiol. 1991, 21, 121–124. [Google Scholar] [PubMed]
- Wong-Chung, J.; Ryan, M.; O’Brien, T. Movement of the femoral head after Salter osteotomy for acetabular dysplasia. J. Bone Jt. Surg. Br. Vol. 1990, 72, 563–567. [Google Scholar]
- Bouchard, M.; Bauer, J.M.; Bompadre, V.; Krengel, W.F. An Updated Algorithm for Radiographic Screening of Upper Cervical Instability in Patients with Down Syndrome. Spine Deform. 2019, 7, 950–956. [Google Scholar] [CrossRef] [PubMed]
- Bull, M.J. Committee on Genetics. Health supervision for children with Down syndrome. Pediatrics 2011, 128, 393–406. [Google Scholar] [CrossRef] [PubMed]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; the PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 350, g7647. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, N.; Inaba, Y.; Oba, M.; Aota, Y.; Morikawa, Y.; Ata, Y.; Machida, J.; Saito, T. Novel 2 radiographical measurements for atlantoaxial instability in children with Down syndrome. Spine 2014, 39, E1566–E1574. [Google Scholar] [PubMed]
- Nakamura, N.; Inaba, Y.; Aota, Y.; Oba, M.; Machida, J.; Aida, N.; Kurosawa, K.; Saito, T. New radiological parameters for the assessment of atlantoaxial instability in children with Down syndrome: The normal values and the risk of spinal cord injury. Bone Jt. J. 2016, 98, 1704–1710. [Google Scholar]
- Bauer, J.M.; Dhaliwal, V.K.B.; Browd, S.R.; Krengel, W.F.I. Repeat Pediatric Trisomy 21 Radiographic Exam: Does Atlantoaxial Instability Develop Over Time? J. Pediatr. Orthop. 2021, 41, e646–e650. [Google Scholar] [PubMed]
- Hengartner, A.C.; Whelan, R.; Maj, R.; Wolter-Warmerdam, K.; Hickey, F.; Hankinson, T.C. Evaluation of 2011 AAP cervical spine screening guidelines for children with Down Syndrome. Childs Nerv. Syst. 2020, 36, 2609–2614. [Google Scholar] [CrossRef] [PubMed]
- Morton, R.E.; Khan, M.A.; Murray-Leslie, C.; Elliott, S. Atlantoaxial instability in Down’s syndrome: A five year follow up study. Arch. Dis. Child. 1995, 72, 115–119. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Cremers, M.J.; Ramos, L.; Bol, E.; van Gijn, J. Radiological assessment of the atlantoaxial distance in Down’s syndrome. Arch. Dis. Child. 1993, 69, 347–350. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Selby, K.A.; Newton, R.W.; Gupta, S.; Hunt, L. Clinical predictors and radiological reliability in atlantoaxial subluxation in Down’s syndrome. Arch. Dis. Child. 1991, 66, 876–878. [Google Scholar] [PubMed]
- Cremers, M.J.; Bol, E.; de Roos, F.; van Gijn, J. Risk of sports activities in children with Down’s syndrome and atlantoaxial instability. Lancet 1993, 342, 511–514. [Google Scholar] [CrossRef] [PubMed]
- Nader-Sepahi, A.; Casey, A.T.H.; Hayward, R.; Crockard, H.A.; Thompson, D. Symptomatic atlantoaxial instability in Down syndrome. J. Neurosurg. Pediatr. 2005, 103, 231–237. [Google Scholar] [CrossRef] [PubMed]
| Database | Code | Filter | Date | Found |
|---|---|---|---|---|
| Medline (Pubmed) | (“Down Syndrome”[MeSH] OR “down syndrome”[tiab] OR Mongolism OR “47,XY,+21”[tiab] OR “Trisomy G”[tiab] OR “47,XX,+21”[tiab] OR “Down’s Syndrome”[tiab] OR “Downs Syndrome”[tiab] OR Trisomy 21[tiab]) AND (“Atlanto-Axial Joint”(5) OR (“Cervical Vertebrae”(5) AND “Joint Instability”[Mesh]) OR Atlanto-Axial[tiab] OR Atlantoaxial[tiab] OR AAI[tiab]) | Child: Birth–18 years Result by year: 1990–2024 | 2 May 2024 | 161 |
| Embase | (‘Down syndrome’/exp OR ((down* NEAR/3 (syndrome* OR disease OR langdon)) OR (trisomy* NEAR/1 (g OR 21)) OR “47,X?,+21”):ab,ti,kw) AND (‘atlantoaxial joint’/exp OR ‘atlantoaxial dislocation’/exp OR (‘cervical vertebra’/exp AND ‘joint instability’/de) OR (Atlanto-Axial OR Atlantoaxial OR AAI OR (atlas NEAR/3 (disloca* OR luxat* OR instab*))):ab,ti,kw) NOT (‘adult’/exp NOT (‘child’/exp OR ‘adolescent’/exp)) | Publication year: 1990–2024 | 2 May 2024 | 276 |
| Google Scholar | Down|trisomy atlantoaxial|atlanto-axial | The first 100 suggestions | 2 May 2024 | 100 |
| Total | 537 |
| Author (Year) | Study Design | Included Patients | Mean Age (Years) (Range) | Sex Ratio (M/F) | Radiological Definition of AAI | Biases | Screening Implementation (Yes or No) | Type of Screening Method |
|---|---|---|---|---|---|---|---|---|
| Selby et al. (1991) [17] | Observational prospective study | 135 | 9.3 (6–14) | Not reported | ADI ≥ 4.5 mm | No patient with clear neurological deficit. | No | Not reported |
| Cremers et al. (1993) [16] | Cohort prospective study | 91 | Not reported (4–20) | 65/26 | ADI ≥ 4 mm | None | No | Not reported |
| Morton et al. (1995) [15] | Cohort retrospective study | 90 | Not reported (4–19) | Not reported | ADI ≥ 4 mm | Average age unspecified, distribution of ADI measures unspecified. | Yes | Lateral cervical spine X-ray in flexion position at 4–5 years old |
| Nakamura et al. (2014) [11] | Case–control retrospective study | 50 | 3.1 (0.4–17) | 24/26 | 1/4SAC 1 ratio < 0.86, C1 inclination 2 >10° | None | Yes | Lateral cervical spine X-ray in neutral position |
| Nakamura et al. (2016) [12] | Case–control retrospective study | 272 | 5.5 (2–12) | 156/116 | 1/4SAC 1 ratio < 0.86, C1 inclination 2 >10° | None | Yes | Lateral cervical spine X-ray in neutral position |
| Bouchard et al. (2019) [8] | Observational retrospective study | 172 | 8.33 (0–25) | Not reported | ADI > 6 mm, SAC < 14 m, BAI > 12 mm | None | Yes | Lateral cervical spine X-ray in neutral position at 3 years old |
| Hengartner et al. (2020) [14] | Observational retrospective study | 1566 | Not reported | Not reported | ADI > 4.5 mm | None | No | Not reported |
| Bauer et al. (2021) [13] | Observational retrospective study | 160 | 7.4 (3–20.8) | 88/72 | ADI > 6 mm, SAC < 14 mm, BAI > 12 mm | None | Yes | Lateral cervical spine X-ray in neutral position at 3 years old |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cattarinussi, L.; Bregou, A.; Newman, C.J.; Merckaert, S.R. Radiological Screening of Atlantoaxial Instability in Children with Trisomy 21: A Systematic Review and Evidence-Based Recommendations. Children 2025, 12, 421. https://doi.org/10.3390/children12040421
Cattarinussi L, Bregou A, Newman CJ, Merckaert SR. Radiological Screening of Atlantoaxial Instability in Children with Trisomy 21: A Systematic Review and Evidence-Based Recommendations. Children. 2025; 12(4):421. https://doi.org/10.3390/children12040421
Chicago/Turabian StyleCattarinussi, Leo, Aline Bregou, Christopher J. Newman, and Sophie R. Merckaert. 2025. "Radiological Screening of Atlantoaxial Instability in Children with Trisomy 21: A Systematic Review and Evidence-Based Recommendations" Children 12, no. 4: 421. https://doi.org/10.3390/children12040421
APA StyleCattarinussi, L., Bregou, A., Newman, C. J., & Merckaert, S. R. (2025). Radiological Screening of Atlantoaxial Instability in Children with Trisomy 21: A Systematic Review and Evidence-Based Recommendations. Children, 12(4), 421. https://doi.org/10.3390/children12040421







