Changes in Couple Relationship Dynamics among Low-Income Parents in a Relationship Education Program Are Associated with Decreases in Their Children’s Mental Health Symptoms
Abstract
:1. Introduction
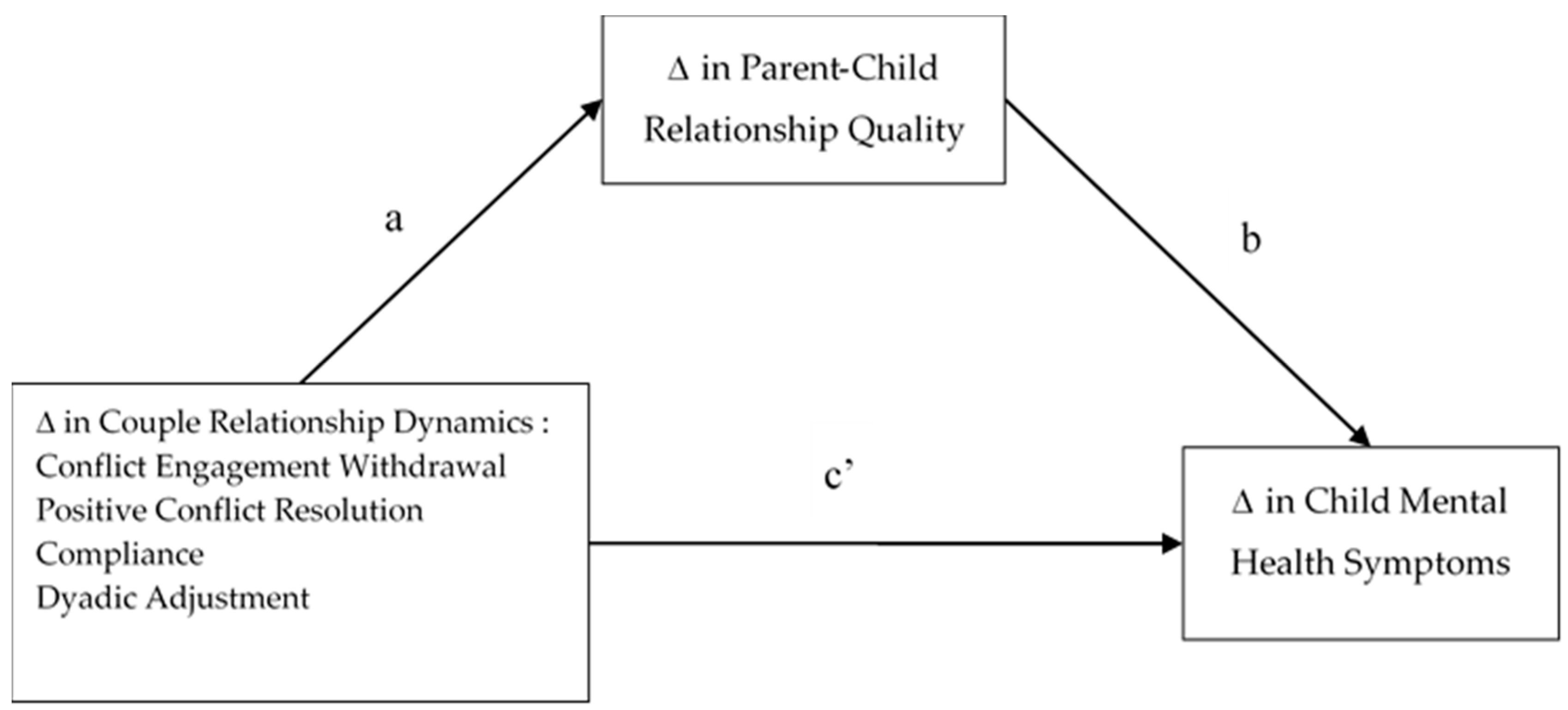
- Are changes in conflict-related behaviors and relationship quality associated with changes in child mental health symptoms among children of parents involved in a relationship education preventive intervention?
- Do changes in parent–child relationship quality mediate the association between changes in couple dynamics and child mental health symptoms?
2. Materials and Methods
2.1. Design
2.2. Sample
2.3. Measures
2.3.1. Relationship Dynamics-Conflict Behaviors
2.3.2. Child Mental Health Symptoms
2.4. Data Analysis
3. Results
3.1. Descriptive Statistics
3.2. Bivariate Correlations
3.3. Multiple Linear Regression
3.4. Mediation Analyses
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Hamby, S.; Finkelhor, D.; Turner, H.; Ormrod, R. Children’s Exposure to Intimate Partner Violence and Other Family Violence; Office of Juvenile Justice and Delinquency Prevention: Washington, DC, USA, 2011.
- Galano, M.M.; Grogan-Kaylor, A.C.; Clark, H.M.; Liendo, N.M.; Graham-Bermann, S.A. Conflict appraisals in a multiethnic sample of children exposed to intimate partner violence. J. Fam. Violence 2016, 31, 655–665. [Google Scholar] [CrossRef]
- Alhusen, J.L.; Bullock, L.; Sharps, P.; Schminkey, D.; Comstock, E.; Campbell, J. Intimate partner violence during pregnancy and adverse neonatal outcomes in low-income women. J. Women’s Health 2014, 23, 920–926. [Google Scholar] [CrossRef] [PubMed]
- Karakurt, G.; Patel, V.; Whiting, K.; Koyutürk, M. Mining electronic health records data: Domestic violence and adverse health effects. J. Fam. Violence 2017, 32, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Karakurt, G.; Smith, D.; Whiting, J. Impact of intimate partner violence on women’s mental health. J. Fam. Violence 2014, 29, 693–702. [Google Scholar] [CrossRef] [PubMed]
- Maddoux, J.; Symes, L.; McFarlane, J.; Koci, A.; Gilroy, H.; Fredland, N. Problem-solving and mental health outcomes of women and children in the wake of intimate partner violence. J. Environ. Public Health 2014, 2014, 708198. [Google Scholar] [CrossRef] [PubMed]
- Capaldi, D.; Knoble, N.; Shortt, J.; Kim, H. A systematic review of risk factors for intimate partner violence. Partn. Abus. 2012, 3, 231–280. [Google Scholar] [CrossRef] [PubMed]
- Arroyo, K.; Lundahl, B.; Butters, R.; Vanderloo, M.; Wood, D.S. Short-term interventions for survivors of intimate partner violence. Trauma Violence Abus. 2017, 18, 155–171. [Google Scholar] [CrossRef] [PubMed]
- Adams, A.E.; Tolman, R.M.; Bybee, D.; Sullivan, C.M.; Kennedy, A.C. The impact of intimate partner violence on low-income women’s economic well-being: The mediating role of job stability. Violence Women 2012, 18, 1345–1367. [Google Scholar] [CrossRef] [PubMed]
- Breiding, M.J.; Basile, K.C.; Klevens, J.; Smith, S.G. Economic Insecurity and Intimate Partner and Sexual Violence Victimization. Am. J. Prev. Med. 2017, 53, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Whitfield, C.L.; Anda, R.F.; Dube, S.R.; Felitti, V.J. Violent childhood experiences and the risk of intimate partner violence in adults: Assessment in a large health maintenance organization. J. Interpers. Violence 2003, 18, 166–185. [Google Scholar] [CrossRef]
- Porche, M.V.; Costello, D.M.; Rosen-Reynoso, M. Adverse Family Experiences, Child Mental Health, and Educational Outcomes for a National Sample of Students. School Ment. Health 2016, 8, 44–60. [Google Scholar] [CrossRef]
- Tonelli, L.; Pregulman, M.; Markman, H. The Prevention and Relationship Education Program (PREP) for individuals and couples. In Evidence-Based Approaches to Relationship and Marriage Education; Ponzetti, J.J.J., Ed.; Taylor & Francis: New York, NY, USA, 2016; pp. 180–196. [Google Scholar]
- Wadsworth, M.E.; Markman, H.J. Where’s the Action? Understanding What Works and Why in Relationship Education. Behav. Ther. 2012, 43, 99–112. [Google Scholar] [CrossRef] [PubMed]
- Pearson, M.; Stanley, S.; Rhoades, G. Within My Reach Instructor Manual; PREP: Denver, CO, USA, 2008. [Google Scholar]
- Stanley, S.M.; Pearson, M.; Kline, G.H. The Development of Relationship Education for Low Income Individuals: Lessons from Research and Experience. In Proceedings of the Association for Public Policy Analysis and Management Conference, Washington, DC, USA, 3–5 December 2005. [Google Scholar]
- Visvanathan, P.D.; Richmond, M.; Winder, C.; Koenck, C.H. Individual-Oriented Relationship Education: An Evaluation Study in Community-Based Settings. Fam. Process 2014, 54, 686–702. [Google Scholar] [CrossRef] [PubMed]
- Antle, B.; Sar, B.; Christensen, D.; Karam, E.; Ellers, F.; Barbee, A.; Zyl, M.V. The Impact of the within My Reach Relationship Training on Relationship Skills and Out comes for Low-Income Individuals. J. Marital Fam. Ther. 2013, 39, 346–357. [Google Scholar] [CrossRef] [PubMed]
- Carlson, R.G.; Rappleyea, D.L.; Daire, A.P.; Harris, S.M.; Liu, X. The Effectiveness of Couple and Individual Relationship Education: Distress as a Moderator. Fam. Process 2015, 56, 91–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McTavish, J.R.; MacGregor, J.C.D.; Wathen, C.N.; MacMillan, H.L. Children’s exposure to intimate partner violence: An overview. Int. Rev. Psychiatry 2016, 28, 504–518. [Google Scholar] [CrossRef] [PubMed]
- Goldberg, J.S.; Carlson, M.J. Parents Relationship Quality and Childrens Behavior in Stable Married and Cohabiting Families. J. Marriage Fam. 2014, 76, 762–777. [Google Scholar] [CrossRef] [PubMed]
- Keller, P.S.; Cummings, E.M.; Peterson, K.M.; Davies, P.T. Marital conflict in the context of parental depressive symptoms: Implications for the development of children’s adjustment problems. Soc. Dev. 2009, 18, 536–555. [Google Scholar] [CrossRef] [PubMed]
- El-Sheikh, M.; Hinnant, J.B.; Erath, S. Developmental trajectories of delinquency symptoms in childhood: The role of marital conflict and autonomic nervous system activity. J. Abnorm. Psychol. 2011, 120, 16–32. [Google Scholar] [CrossRef] [PubMed]
- Fusco, R.A. Socioemotional Problems in Children Exposed to Intimate Partner Violence: Mediating Effects of Attachment and Family Supports. J. Interpers. Violence 2017, 32, 2515–2532. [Google Scholar] [CrossRef] [PubMed]
- Holmes, M.; Voith, L.; Gromoske, A. Lasting effect of intimate partner violence exposure during preschool on aggressive behavior and prosocial skills. J. Interpers. Violence 2015, 30, 1651–1670. [Google Scholar] [CrossRef] [PubMed]
- Madigan, S.; Plamondon, A.; Jenkins, J.M. Marital Conflict Trajectories and Associations with Childrens Disruptive Behavior. J. Marriage Fam. 2016, 79, 437–450. [Google Scholar] [CrossRef]
- Zemp, M.; Milek, A.; Cummings, E.M.; Cina, A.; Bodenmann, G. How couple- and parenting-focused programs affect child behavioral problems: A randomized controlled trial. J. Child Fam. Stud. 2016, 25, 798–810. [Google Scholar] [CrossRef]
- Bandura, A. Aggression: A Social Learning Analysis; Prentice Hall: Englewood Cliffs, NY, USA, 1973. [Google Scholar]
- Levendosky, A.; Lannert, B.; Yalch, M. The effects of intimate partner violence on women and children survivors: An attachment perspective. Psychodyn. Psychiatry 2012, 40, 397–434. [Google Scholar] [CrossRef] [PubMed]
- Fosco, G.; DeBoard, R.L.; Rych, J.H. Making sense of family violence: Implications of children’s appraisals of interparental aggression for their short- and long-term functioning. Eur. Psychol. 2007, 12, 6–16. [Google Scholar] [CrossRef]
- Erel, O.; Burman, B. Interrelatedness of marital relations and parent-child relations: A meta-analytic review. Psychol. Bull. 1995, 118, 108–132. [Google Scholar] [CrossRef] [PubMed]
- Katz, L.F.; Low, S.M. Marital Violence, Co-Parenting, and Family-Level Processes in Relation to Children’s Adjustment. J. Fam. Psychol. 2004, 18, 372–382. [Google Scholar] [CrossRef] [PubMed]
- Sellers, C.S.; Cochran, J.K.; Branch, K.A. Social Learning Theory and Partner Violence: A Research Note. Deviant Behav. 2005, 26, 379–395. [Google Scholar] [CrossRef]
- Martin, M.J.; Sturge-apple, M.L.; Davies, P.T.; Romero, C.V. A process model of the implications of spillover from coparenting conflicts into the parent-child attachment relationship in adolescence. Dev. Psychopathol. 2017, 29, 417–431. [Google Scholar] [CrossRef] [PubMed]
- Rhoades, K.A. Children’s Responses to Interparental Conflict: A Meta-Analysis of Their Associations with Child Adjustment. Child Dev. 2008, 79, 1942–1956. [Google Scholar] [CrossRef] [PubMed]
- Jouriles, E.N.; Rosenfield, D.; Mcdonald, R.; Mueller, V. Child Involvement in Interparental Conflict and Child Adjustment Problems: A Longitudinal Study of Violent Families. J. Abnorm. Child Psychol. 2014, 42, 693–704. [Google Scholar] [CrossRef] [PubMed]
- Washington, T.; Rose, T.; Colombo, G.; Hong, J.S.; Coard, S.I. Family-Level Factors and African American Children’s Behavioral Health Outcomes: A Systematic Review. Child Youth Care Forum 2015, 44, 819–834. [Google Scholar] [CrossRef]
- Antle, B.F.; Karam, E.; Christensen, D.N.; Barbee, A.P.; Sar, B.K. An evaluation of healthy relationship education to reduce intimate partner violence. J. Fam. Soc. Work 2011, 14, 387–406. [Google Scholar] [CrossRef]
- McGill, J.; Adler-Baeder, F.; Bradford, A.B.; Kerpelman, J.; Ketring, S.A.; Sollie, D. The Role of Relational Instability on Individual and Partner Outcomes Following Couple Relationship Education Participation. Fam. Relat. 2016, 65, 407–423. [Google Scholar] [CrossRef]
- Barton, A.W.; Futris, T.G.; Bradley, R.C. Changes following Premarital Education for Couples with Differing Degrees of Future Marital Risk. J. Marital Fam. Ther. 2014, 40, 165–177. [Google Scholar] [CrossRef] [PubMed]
- Adler-Baeder, F.; Calligas, A.; Skuban, E.; Keiley, M.; Ketring, S.; Smith, T. Linking Changes in Couple Functioning and Parenting Among Couple Relationship Education Participants. Fam. Relat. 2013, 62, 284–297. [Google Scholar] [CrossRef]
- Job, A.K.; Baucom, D.H.; Hahlweg, K. Who Benefits from Couple Relationship Education? Findings from the Largest German CRE Study. J. Couple Relatsh. Ther. 2017, 16, 79–101. [Google Scholar] [CrossRef]
- Owen, J.; Antle, B.; Barbee, A. Does adherence to relationship education curriculum relate to participants’ outcomes? Couple Fam. Psychol. Res. Pract. 2014, 3, 99–109. [Google Scholar] [CrossRef]
- Kurdek, L. Predicting change in marital satisfaction from husbands and wives conflict resolution styles. J. Marriage Fam. 1995, 57, 153–164. [Google Scholar] [CrossRef]
- Kurdek, L.A. Change in relationship quality for partners from lesbian, gay male, and heterosexual couples. J. Fam. Psychol. 2008, 22, 701–711. [Google Scholar] [CrossRef] [PubMed]
- Kurdek, L. Relationship outcomes and their predictors: Longitudinal evidence from heterosexual married, gay cohabiting, and lesbian cohabiting couples. J. Marriage Fam. 1998, 60, 553–568. [Google Scholar] [CrossRef]
- Spanier, G.B. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. J. Marriage Fam. 1976, 38, 15–28. [Google Scholar] [CrossRef]
- Gerard, A.B. Parent-Child Relationship Inventory (PCRI); Western Psychological Services: Los Angeles, CA, USA, 1994. [Google Scholar]
- Coffman, J.; Guerin, D.; Gottfried, A. Reliability and validity of the parent-Child relationship inventory (PCRI): Evidence from a longitudinal cross-informant investigation. Psychol. Assess. 2006, 18, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Gardner, W.; Murphy, M.; Childs, G.; Kelleher, K.; Pagano, M.; Jellinek, M.; Chiappetta, L. The pSC-17: A brief pediatric symptom checklist with psychosocial problem sub scales: A report from pROS and aSPN. Ambul. Child Health 1999, 5, 225–236. [Google Scholar]
- Jellinek, M.S.; Murphy, J.M.; Little, M.; Pagano, M.E.; Comer, D.M.; Kelleher, K.J. Use of the Pediatric Symptom Checklist to Screen for Psychosocial Problems in Pediatric Primary Care. Arch. Pediatr. Adolesc. Med. 1999, 153, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.M.; Bergmann, P.; Chiang, C.; Sturner, R.; Howard, B.; Abel, M.R.; Jellinek, M. The PSC-17: Subscale Scores, Reliability, and Factor Structure in a New National Sample. Pediatrics 2016, 138, e20160038. [Google Scholar] [CrossRef] [PubMed]
- Hayes, A. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 2nd ed.; The Guilford Press: New York, NY, USA, 2018. [Google Scholar]
- Jacobson, N.; Truax, P. Clinical significance: A statistical approach to defining meaninful change in psychotherapy research. J. Consult. Clin. Psychol. 1991, 59, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.; Altman, D. Multiple significance tests: The Bonferroni method. Br. Med. J. 1995, 310, 170. [Google Scholar] [CrossRef]
- Rucker, D.D.; Preacher, K.J.; Tormala, Z.L.; Petty, R.E. Mediation Analysis in Social Psychology: Current Practices and New Recommendations. Soc. Personal. Psychol. Compass 2011, 5, 359–371. [Google Scholar] [CrossRef]
- Bandura, A. Social Learning Theory; Prentice-Hall: Englewood Cliffs, NJ, USA, 2002. [Google Scholar]
- Ditzen, B.; Hahlweg, K.; Fehm-Wolfsdorf, G.; Baucom, D. Assisting couples to develop healthy relationships: Effects of couples relationship education on cortisol. Psychoneuroendocrinology 2011, 36, 597–607. [Google Scholar] [CrossRef] [PubMed]
- Gunlicks-Stoessel, M.L.; Powers, S.I. Romantic partners’ coping strategies and partners of cortisol reactivity and recovery in response to relationship conflict. J. Soc. Clin. Psychol. 2009, 28, 630–649. [Google Scholar] [CrossRef] [PubMed]
- Sanner, C.M.; Neece, C.L. Parental Distress and Child Behavior Problems: Parenting Behaviors as Mediators. J. Child Fam. Stud. 2018, 27, 591–601. [Google Scholar] [CrossRef]
- Lavigne, J.V.; Gouze, K.R.; Hopkins, J.; Bryant, F.B.; LeBailly, S.A. A multi-domain model of risk factors for odd symptoms in a community sample of 4-year-olds. J. Abnorm. Child Psychol. 2012, 40, 741–757. [Google Scholar] [CrossRef] [PubMed]
- Baumrind, D. Differentiating between confrontive and coercive kinds of parental power-assertive disciplinary practices. Hum. Dev. 2012, 55, 35–51. [Google Scholar] [CrossRef]
- Sanders, M.R. Triple P-Positive Parenting Program as a Public Health Approach to Strengthening Parenting. J. Fam. Psychol. 2008, 22, 506–517. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- David, O.A.; David, D.; Dobrean, A. The Rational Positive Parenting Program for Child Externalizing Behavior: Mechanisms of chance analysis. J. Evid.-Based Psychother. 2014, 14, 21–38. [Google Scholar]
- Nichols, M.; Davis, S. Family Therapy: Concepts and Methods, 11th ed.; Pearson: New York, NY, USA, 2016. [Google Scholar]
- Langhinrichsen-Rohling, J.; Capaldi, D.M. Clearly We’ve only Just Begun: Developing Effective Prevention Programs for Intimate Partner Violence. Prev. Sci. 2012, 13, 410–414. [Google Scholar] [CrossRef] [PubMed]
- Langhinrichsen-Rohling, J.; Turner, L.A. The Efficacy of an Intimate Partner Violence Prevention Program with High-Risk Adolescent Girls: A Preliminary Test. Prev. Sci. 2012, 13, 384–394. [Google Scholar] [CrossRef] [PubMed]
| m or n (%) | SD | Possible Range | Pre-Post Diff. t-Test Score | Reliable Change Score t | |
|---|---|---|---|---|---|
| Race | |||||
| African-American | 234 (67%) | ||||
| White | 90 (26%) | ||||
| Multiracial | 8 (2.3%) | ||||
| Native American | 5 (1.4%) | ||||
| Hispanic | 2 (0.6%) | ||||
| Other | 6 (1.7%) | ||||
| Did not respond | 4 (1%) | ||||
| Age | 34 | 10.46 | |||
| Sex | |||||
| Female | 305 (87%) | ||||
| Male | 42 (12%) | ||||
| Did not respond | 2 (1%) | ||||
| Annual Family Income | |||||
| <$10,000 | 184 (53%) | ||||
| $10,000–$20,000 | 75 (21%) | ||||
| $20,000–$30,000 | 36 (10%) | ||||
| >$30,000 | 21 (6%) | ||||
| Didn’t respond | 33 (10%) | ||||
| Employment Status | |||||
| Full-time | 56 (16%) | ||||
| Part-time | 36 (10%) | ||||
| Unemployed | 209 (60%) | ||||
| Other | 40 (11%) | ||||
| Did not respond | 8 (2%) | ||||
| Education | |||||
| ≤8th grade | 14 (4%) | ||||
| Some high school | 46 (13%) | ||||
| 12th grade or General Education Diploma | 129 (37%) | ||||
| Some college or Technical School | 146 (42%) | ||||
| Bachelors or Graduate degree | 9 (3%) | ||||
| Pre-test in Conflict Engagement | 10.16 | 3.82 | 1–20 | ||
| Pre-test in Withdrawal | 11.13 | 3.64 | 1–20 | ||
| Pre-test in Positive Conflict | 12.26 | 3.48 | 1–20 | ||
| Pre-test in Compliance | 9.04 | 3.34 | 1–20 | ||
| Pre-test in Dyadic Adjustment Scale | 19.95 | 7.38 | 0–36 | ||
| Pre-test in Parent–Child Relationship | 45.15 | 6.64 | 1–60 | ||
| Pre-test in Child Problem Behaviors | 27.84 | 7.24 | 1–51 | ||
| Pre-Post Δ in Conflict Engagement | −0.48 | 3.4 | 2.61 ** | −0.24 | |
| Pre-Post Δ in Withdrawal | −0.84 | 3.6 | 4.23 ** | −0.36 | |
| Pre-Post Δ in Positive Conflict Resolution | 0.34 | 3.1 | −2.21 * | 0.12 | |
| Pre-Post Δ in Compliance | −0.26 | 3.4 | 1.30 | −0.08 | |
| Pre-Post Δ in DAS | 0.75 | 6.12 | −1.88 a | 0.13 | |
| Pre-Post Δ in Parent–Child Relationship | 1.2 | 5.2 | −4.11 ** | 0.26 | |
| Pre-Post Δ in Child Problem Behaviors | −0.73 | 4.9 | 2.60 ** | −0.28 | |
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | |
|---|---|---|---|---|---|---|---|---|---|
| 1. Ethnicity | — | ||||||||
| 2. Age | −0.02 | — | |||||||
| 3. Family Income | −0.09 | 0.11 * | — | ||||||
| 4. Δ Conflict Engagement | −0.09 | 0.02 | 0.01 | — | |||||
| 5. Δ Positive Resolution | −0.03 | 0.03 | −0.06 | −0.29 **,t | — | ||||
| 6. Δ Withdrawal | −0.02 | 0.08 | −0.06 | 0.36 **,t | −0.09 | — | |||
| 7. Δ Compliance | 0.02 | −0.04 | −0.02 | 0.24 **,t | 0.01 | 0.29 **,t | — | ||
| 8. Δ Dyadic Adjustment | 0.00 | 0.05 | 0.11 * | −0.24 **,t | 0.22 **,t | −0.24 **,t | −0.17 ** | — | |
| 9. Δ Parent–Child Relationship | −0.02 | −0.02 | 0.01 | −0.14 * | 0.05 | −0.08 | −0.13 * | 0.14 * | — |
| 10. Δ Child Symptoms | −0.10 a | 0.05 | 0.01 | 0.22 * | −0.05 | 0.19 **,t | 0.11 * | −0.08 | −0.23 **,t |
| Predictors: | β | t | p |
|---|---|---|---|
| ∆ Parent–Child Relationship Quality | −0.20 | −3.51 | 0.00 **,t |
| ∆ Conflict Engagement | 0.16 | 2.56 | 0.01 * |
| ∆ Withdrawal | 0.12 | 1.92 | 0.06 a |
| ∆ Positive Resolution | 0.02 | 0.36 | 0.72 |
| ∆ Compliance | −0.01 | −0.17 | 0.86 |
| ∆ Dyadic Adjustment | 0.04 | −0.10 | 0.91 |
| Mediator as Outcome: ∆ Parent–Child Relationship Quality | Outcome: ∆ Child Mental Health Symptoms | Indirect Effect | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictors: | Coeff. | SE | p | Coeff. | SE | p | Effect | Lower Limit Confidence Interval | Upper Limit Confidence Level |
| ∆ Conflict Engagement | −0.18 | 0.08 | 0.02 | 0.28 | 0.04 | <0.001 t | 0.03 | 0.00 | 0.07 |
| ∆ Parent–Child RQ | — | — | — | −0.18 | 0.07 | <0.001 t | |||
| ∆ Withdrawal | −0.18 | 0.07 | 0.02 | 0.25 | 0.06 | <0.001 t | 0.03 | 0.00 | 0.07 |
| ∆ Parent–Child RQ | — | — | — | −0.18 | 0.04 | <0.001 t | |||
| ∆ Positive Resolution | 0.20 | 0.08 | 0.01 | −0.09 | 0.04 | 0.21 | −0.04 | −0.08 | 0.00 |
| ∆ Parent–Child RQ | — | — | — | −0.19 | 0.07 | <0.001 t | |||
| ∆ Compliance | −0.22 | 0.07 | 0.01 | 0.11 | 0.07 | 0.11 | 0.04 | 0.01 | 0.08 |
| ∆ Parent–Child RQ | — | — | — | −0.19 | 0.04 | <0.001 t | |||
| ∆ Dyadic Adjustment | 0.14 | 0.04 | <0.01 | −0.05 | 0.04 | 0.21 | −0.02 | −0.05 | −0.01 |
| ∆ Parent–Child RQ | — | — | — | −0.19 | 0.04 | <0.001 t | |||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sterrett-Hong, E.; Antle, B.; Nalley, B.; Adams, M. Changes in Couple Relationship Dynamics among Low-Income Parents in a Relationship Education Program Are Associated with Decreases in Their Children’s Mental Health Symptoms. Children 2018, 5, 90. https://doi.org/10.3390/children5070090
Sterrett-Hong E, Antle B, Nalley B, Adams M. Changes in Couple Relationship Dynamics among Low-Income Parents in a Relationship Education Program Are Associated with Decreases in Their Children’s Mental Health Symptoms. Children. 2018; 5(7):90. https://doi.org/10.3390/children5070090
Chicago/Turabian StyleSterrett-Hong, Emma, Becky Antle, Brianna Nalley, and Monica Adams. 2018. "Changes in Couple Relationship Dynamics among Low-Income Parents in a Relationship Education Program Are Associated with Decreases in Their Children’s Mental Health Symptoms" Children 5, no. 7: 90. https://doi.org/10.3390/children5070090
APA StyleSterrett-Hong, E., Antle, B., Nalley, B., & Adams, M. (2018). Changes in Couple Relationship Dynamics among Low-Income Parents in a Relationship Education Program Are Associated with Decreases in Their Children’s Mental Health Symptoms. Children, 5(7), 90. https://doi.org/10.3390/children5070090





