Facilitators and Barriers to the Implementation of Preschool Oral Healthcare Programme in Malaysia from the Perspective of Dental Therapists: A Qualitative Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Setting
2.3. Sampling and Recruitment
2.4. Development of FGD Questions and Training of Facilitators
2.5. Conduct of FGDs, Data Analysis and Ethics
3. Results
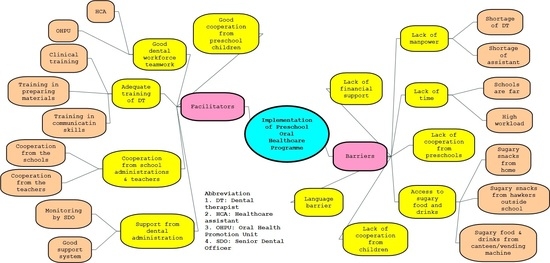
3.1. Themes
3.1.1. Facilitators to the Implementation of the POHP
Good Dental Workforce Teamwork
“…OHPU helps in reducing time, as OHPU can concentrate on giving OHE and TBD, and the dental mobile team (DT, HCA) for preschool children can work on the clinical aspect of the visit”(DT 6, Gombak 2nd group)
“Teachers would be delighted when OHPU came to schools because they are dentists in the unit. The teachers’ attention towards the DO was different compared to us (DT) who wear white uniform. They do not really give full attention to us”(DT 4, Klang 2nd group)
“Between DT, the cooperation is good, we are really close and very positive. We help each other if one has to go for a course or has to take emergency leave”(DT 7, Petaling)
Cooperation from School Administrations and Teachers
“Sometimes the headmaster would also come and monitor our programme. If he coincidently walks by our treatment room, he will look inside, at the children having the treatment and he would also like to know about the treatment”(DT 10, Hulu Selangor)
“Let say if we give them appointment date, they will reserve the date only for us”(DT 2, Hulu Langat 2nd group).
“The OHPU will encourage the preschool to prepare an oral health corner, and some preschools took up the advice and prepared a suitable oral health corner (as suggested by the dental team)”(DT 2, Klang 1st group)
“The teachers asked us nicely what we needed before we came for our visit. I informed the teachers (that) we would come the next day, please ask the preschool children to bring their toothbrush. The message will surely reach the children”(DT 6, Sepang).
“We informed the teachers about our visit and asked them to remind the parents, so that all the children will be there during our visit”(DT 9, Hulu Langat 2nd group)
“We can see that the children are ready, the teachers already arranged the children. They knew that we are coming, and the children are in orderly manner”(DT 3, Petaling)
“If the preschool children were uncooperative during the treatment, the teachers would wait by their side and hold the children’s hands until the treatment are completed”(DT 10, Kuala Selangor)
Adequate Training of DT
“At dental college, we learned how to handle preschool children. There were preschool children invited to the college. It helped a lot”(DT 3, Gombak 1st group)
“During our training at the college, we were given a lecture on how to prepare slides show suitable for preschool children”(DT 6, Sabak Bernam)
“We were also trained how to make dolls, puppets, and how to conduct tooth brushing drills. We sat for an examination in oral health promotion”(DT 8, Petaling)
“There are courses such as how to conduct OHE using puppets. It is a 3-day course. The last time such a course was held was when I first joined the service 5 years ago. It involved all districts in Selangor state with invited speakers came from outside the dental service”(DT 9, Gombak 1st group)
“The latest course was on how to handle children and communicate with children. The lecturer was not from dental (outsource). He is a specialist from Teachers Learning Institute (TLI). Many speakers were involved. A puppet specialist taught us how to do voice intonation”(DT 6, Hulu Langat 1st group)
Support from Dental Administration
“The SDO gives full support by asking a dental officer to be involved in the POHP through the OHPU. The dental officer will be in the same team with the dental therapist and helps in OHE”(DT 10, Gombak group 2)
“Our dental officer in-charge would ask a dentist who is free to replace the DT who could not go to the preschools”(DT6, Hulu Langat 2nd group)
“The SDO really put an emphasis on the fluoride varnish application to the children because it is one of our core duties. She would remind us to get it done quickly. She would also ask if we faced with any problem, or if we want to add more preschool centres in the schedule”(DT 6, Gombak 1st group)
Good Cooperation from Preschool Children
“Children received a lot of dental exposures nowadays. Most children are not afraid of dental treatment anymore and they are ready. From that angle it is obvious”(DT 1, Petaling)
“During our visit to the preschool centre, when we called the children for dental check-up, they did not cry. The teacher did not need to tell them to sit on the chair and open their mouth. They were doing it willingly”(DT 4, Hulu Langat 2nd group)
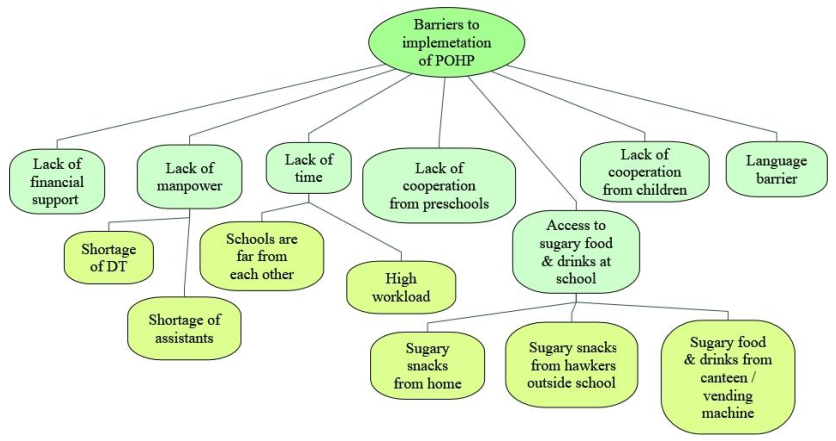
3.1.2. Barriers to the Implementation of the POHP
Lack of Financial Support
“If we keep bringing the same materials every year, the children will get bored, so we need to make or purchase new materials. But these require money, so we have little choice except to use our own money as there was no budget for it. Sometimes, the teachers ask for posters to put on the wall but there are no extra posters”(DT 7, Hulu Langat 2nd group)
“In the plan of action, we need to produce at least one OHE material per year, but there is no funding provided. So, we had little choice except to collect money among us, or we tried to construct something. We have to comply with the plan of action, and that means we need to have at least one OHE material for each clinic, every year”(DT 1, Gombak 2nd group)
Lack of Manpower
“…the number of preschools (need to be covered) is increasing. We have difficulties in visiting all of the preschool centres with the shortage of manpower. Also, the number of staff is small. There is no replacement staff for those who have retired or transferred out”(DT 3, Sepang)
“They (the OHPU) were not given any guidelines on what to do. They just continue the work like the previous year which was also conducted by DT”(DT 9, Klang 2nd group)
“The earlier agreement was to replace the DT in the OHPU with a DO to go to school. However, this has not happened as we are also short of DO for the POHP”(DT 8, Kuala Selangor)
“Sometimes, we were not given any assistant although we needed it. We need a dental assistant to assist us in the treatment of the preschool children. We had an appointment with the teacher to come to the school. But when we did not have an assistant, or if we were denied an assistant, we had to cancel our visit to the school”(DT 9, Kuala Selangor).
Lack of Time
“…sometimes the schedule was very pack, had to cover 2 or 3 preschool per day”(DT 7, Kuala Langat)
“Sometimes, we supposed to go to 2 preschools inside the school premise, and 2 kindergartens. However, we could cover only one preschool. There was no time to visit all. When this happened, it disturbed our schedule for the week”(DT 6, Sabak Bernam)
“The location between preschools are not near to each other. Moreover, on Friday they will be a lot of movement, some DT would go for courses, some would go to secondary schools”(DT 3, Kuala Selangor)
Lack of Cooperation from Preschools
“The schools did not cooperate with us. We must follow their request. We have a lot of preschools to visit. So, we informed them of our visiting date much earlier, but they refused to accept it, they wanted us to follow their schedule”(DT 5, Hulu Langat 1st group)
“They only want the first visit. They always refuse when we informed them about the second visit. Their excuse was, our schedule is very pack”(Dental therapist 7, Klang 1st group)
“…the staff was in the middle of giving OHE using a video presentation when the headmaster came and switch off the LCD, he said the children had enough with the talk and should do tooth brushing exercise. He dictated the programme, and we must follow the school’s regulations”(DT 5, Hulu Langat 1st group)
Lack of Cooperation from Children
“The children can be hard to handle, especially when there were many of them. Some of them would stand up and sit down repeatedly”(DT 3, Kuala Selangor)
“The children were bored, every year it is the same thing. Those who attended the preschool at 4 years old had similar activities when they were 5 and 6 years old”(DT 3, Sepang)
“…they were afraid of the white uniform”(DT 6, Gombak group)
“Some children cried because they were too afraid when they saw us and they refused treatment”(DT, Hulu Selangor)
Language Barrier
“In Chinese schools, the teachers would translate for us. It was a bit difficult if we want to communicate directly with the children”(DT 9, Gombak 1st group)
“In preschools where there were many children who speak Tamil, the teacher had to explain to the children the messages that we delivered to the children”(DT 5, Hulu Selangor)
“But when we went to the aborigine’s area, they appeared to be lost. I mean, do they understand what we are talking about? The teachers would translate and explain to the children in their language”(DT 7, Sepang)
Accessibility to Sugary Food and Drinks at School
“…some private preschools have their own menu, some cook at the centre (at the preschool), some allowed children to bring food from home. I’ve seen that children who brought food from home would bring junk food, packet drinks, and carbonated drinks that are not healthy”(DT 6, Sabak Bernam)
“The primary school has a canteen. The canteen sells sugary food such as doughnut and ice cream. The school also has a vending machine selling carbonated drinks”(DT 5, Klang 1st group)
“Most of the children bought junk food from outside the school premise. This contributed to caries”(DT 2, Kuala Selangor)
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ministry of Health. Guidelines on Oral Healthcare for Preschool Children; Oral Health Division: Federal Territory of Putrajaya, Malaysia, 2003.
- Ministry of Health. Guidelines Early Childhood Oral Healthcare; Oral Health Division: Federal Territory of Putrajaya, Malaysia, 2008.
- Ministry of Health. National Oral Health Survey of Preschool Children 2015; Oral Health Division: Federal Territory of Putrajaya, Malaysia, 2017.
- Ministry of Health. National Oral Health Plan for Malaysia 2011–2020; Oral Health Division: Federal Territory of Putrajaya, Malaysia, 2010.
- Ewles, L.; Simnett, I. Promoting Health: A Practical Guide; Baillière Tindall: London, UK, 1999. [Google Scholar]
- Petersen, P.E.; Kwan, S. Evaluation of community-based oral health promotion and oral disease prevention-WHO recommendations for improved evidence in public health practice. Community Dent. Health 2004, 21, 319–329. [Google Scholar] [PubMed]
- Hennink, M.M. Focus Group Discussions; Oxford University Press: Oxford, UK, 2013. [Google Scholar]
- Gill, P.; Chestnutt, I.G.; Channing, D. Opportunities and challenges to promoting oral health in primary schools. Community Dent. Health 2009, 26, 188. [Google Scholar] [PubMed]
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 2013, 13, 117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kanji, Z. Decoding qualitative research for Dental Hygiene. Can. J. Dent. Hyg. 2012, 46, 239–243. [Google Scholar]
- Fusch, P.I.; Ness, L.R. Are we there yet? Data saturation in qualitative research. Qual. Rep. 2015, 20, 1408. [Google Scholar]
- Archibald, M.M. Investigator Triangulation: A Collaborative Strategy With Potential for Mixed Methods Research. J. Mix. Methods Res. 2016, 10, 228–250. [Google Scholar] [CrossRef]
- Nowjack-Raymer, R.E. Teamwork in Prevention: Possibilities and Barriers to Integrating Oral Health Into General Health. Adv. Dent. Res. 1995, 9, 100–105. [Google Scholar] [CrossRef]
- Simpson, D.D. A framework for implementing sustainable oral health promotion interventions. J. Public Health Dent. 2011, 71, S84–S94. [Google Scholar] [CrossRef]
- Dyson, K.; Kruger, E.; Tennant, M. A decade of experience evolving visiting dental services in partnership with rural remote Aboriginal communities. Aust. Dent. J. 2014, 59, 187–192. [Google Scholar] [CrossRef]
- Wennhall, I.; Norlund, A.; Matsson, L.; Twetman, S. Cost-analysis of an oral health outreach program for preschool children in a low socioeconomic multicultural area in Sweden. Swed. Dent. J. 2010, 34, 1–7. [Google Scholar]
- Vichayanrat, T.; Steckler, A.; Tanasugarn, C. Barriers and facilitating factors among lay health workers and primary care providers to promote children’s oral health in Chon Buri Province, Thailand. Southeast Asian J. Trop. Med. Public Health 2013, 44, 332–343. [Google Scholar] [PubMed]
- Wolff, M.S.; Hill, R.; Wilson-Genderson, M.; Hirsch, S.; Dasanayake, A.P. Nationwide 2.5-year school-based public health intervention program designed to reduce the incidence of caries in children of Grenada. Caries Res. 2016, 50, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, H.; Wright, K.; Robertson, C. Evaluation of a pilot oral health promotion programme; Keep Smiling’: Perspectives from GDPs, health champions and school staff. Br. Dent. J. 2015, 218, 455. [Google Scholar] [CrossRef] [PubMed]
- Veale, M.; Ajwani, S.; Johnson, M.; Nash, L.; Patterson, T.; George, A. The early childhood oral health program: A qualitative study of the perceptions of child and family health nurses in South Western Sydney, Australia. BMC Oral Health 2016, 16, 56. [Google Scholar] [CrossRef] [Green Version]
- Markovic, D.; Soldatovic, I.; Vukovic, R.; Peric, T.; Campus, G.G.; Vukovic, A. How Much Country Economy Influences ECC Profile in Serbian Children—A Macro-Level Factor Analysis. Front. Public Health 2019, 7. [Google Scholar] [CrossRef]
- Alsumait, A. Evaluation of a Long Standing School-based Oral Health Program: A Sequential-explanatory Mixed-Method Approach. Ph.D Thesis, University of Alberta, Edmonton, AB, Canada, 2016. [Google Scholar]
- Andersen, A. Dental Therapists: The Missing Link to Better Oral Health Care for Children in New Mexico. Ph.D Thesis, University of North Carolina, Chapel Hill, NC, USA, 2015. [Google Scholar]
- Stephen, C.; Stevenson, O.; Adey, C. Young children engaging with technologies at home: The influence of family context. J. Early Child. Res. 2013, 11, 149–164. [Google Scholar] [CrossRef]
- Can-Yasar, M.; Inal, G.; Uyanik, O.; Kandir, A. Using Technology in Pre-School Education. UCER-A 2012, 4, 375–383. [Google Scholar]
- Shim, Y.-S.; Kim, A.-H.; Jeon, E.-Y.; An, S.-Y. Dental fear & anxiety and dental pain in children and adolescents; a systemic review. J. Dent. Anesth. Pain Med. 2015, 15, 53–61. [Google Scholar]
- Yassin, R.M.; Baharom, E.; Low, L.L. Challenges in Implementation of “Toddlers’ Adoption Programme” Dental Nurses Perspectives. IJOH 2010, 13, 17. [Google Scholar]
- Salem, K.; Kousha, M.; Anissian, A.; Shahabi, A. Dental fear and concomitant factors in 3-6 year-old children. J. Dent. Res. Dent. Clin. Dent. Prospects 2012, 6, 70. [Google Scholar]
- Torriani, D.; Ferro, R.; Bonow, M.; Santos, I.; Matijasevich, A.; Barros, A.; Demarco, F.; Peres, K. Dental caries is associated with dental fear in childhood: Findings from a birth cohort study. Caries Res. 2014, 48, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Education. Early Childhood Care and Education Policy Implementation Review; Curriculum Development Centre: Federal Territory of Putrajaya, Malaysia, 2007.
- Simmer-Beck, M.; Gadbury-Amyot, C.C.; Ferris, H.; Voelker, M.A.; Keselyak, N.T.; Eplee, H.; Parkinson, J.; Marse, B.; Galemore, C. Extending oral health care services to underserved children through a school–based collaboration: Part 1–A descriptive overview. J. Am. Dent. Hyg. Assoc. 2011, 85, 181–192. [Google Scholar]
- Flores, G.; Lin, H. Trends in racial/ethnic disparities in medical and oral health, access to care, and use of services in US children: Has anything changed over the years? Int. J. Equity Health 2013, 12, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nh, N.R.; Muda, W.M.W.; Jamil, N.I.N.; Hanafi, N.N.N.; Rahman, R.A. How healthy is competitive food served at primary school canteen in Malaysia. Int. Med J. 2017, 24, 44–47. [Google Scholar]
- Turner, L.; Chriqui, J.F.; Chaloupka, F.J. Classroom parties in US elementary schools: The potential for policies to reduce student exposure to sugary foods and beverages. J. Nutr. Educ. Behav. 2013, 45, 611–619. [Google Scholar] [CrossRef] [PubMed]
- Skafida, V.; Chambers, S. Positive association between sugar consumption and dental decay prevalence independent of oral hygiene in pre-school children: A longitudinal prospective study. J. Public Health 2018, 40, e275–e283. [Google Scholar] [CrossRef] [Green Version]
- Bourgeois, D.; Saliasi, I.; Dussart, C.; Llodra, J.C.; Tardivo, D.; Laforest, L.; Bravo, M.; Viennot, S.; Foti, B.; Carrouel, F. Educational outcomes of a new curriculum on interproximal oral prophylaxis for dental students. PloS ONE 2018, 13, e0204564. [Google Scholar] [CrossRef]
- Tarvonen, P.L.; Sipilä, K.; Yang, G.S.; Kim, J.K.; Lamidi, M.L.; Suominen, A.L. Comparison of two preventive interventions on dental caries among children in Democratic People’s Republic of Korea. Int. J. Dent. Hyg. 2016, 14, 301–306. [Google Scholar] [CrossRef]
- Ministry of Health. Kursus pra Perkhidmatan Anggota Sains Kesihatan Bersekutu (Separa Perubatan) Kementerian Kesihatan Malaysia: Diploma Jururawat Pergigian. Available online: https://www.moh.gov.my/moh/resources/kerjaya/DIPLOMA_JURURAWAT_PERGIGIAN.pdf (accessed on 21 November 2020).
- Oswald, D.; Sherratt, F.; Smith, S. Handling the Hawthorne effect: The challenges surrounding a participant observer. Rev. Soc. Stud. 2014, 1, 53–73. [Google Scholar] [CrossRef] [Green Version]

| No | Leading Question | Probing Question |
|---|---|---|
| 1. | Introduction Can you briefly explain your roles in the POHP in Selangor? | Not applicable |
| 2. | Feasibility A. Facilitating factors i.In your opinion, what are the factors that help or facilitate you in carrying out your duties in the POHP? | (a) Children’s reactions |
| (b) Dental administration’s factors | ||
| (c) Workforce | ||
| (d) Dental material/financial aid/transportation | ||
| (e) Preschool centre administration/teachers’ factors | ||
| (f) Training | ||
| (g) Time factors | ||
| B. Barriers ii.In your opinion, what are the barriers that you face in carrying out your duties in the POHP? | (h) Children’s reactions | |
| (i) Dental administration’s factors | ||
| (j) Workforce | ||
| (k) Dental material/financial aid/transportation | ||
| (l) Preschool centre administration/teachers’ factors | ||
| (m) Training | ||
| (n) Time factors |
| Variable | n(%) |
|---|---|
| District | |
| Gombak | 21(18.4) |
| Hulu Selangor | 11(9.6) |
| Hulu Langat | 21(18.4) |
| Klang | 17(14.9) |
| Kuala Langat | 8(7.0) |
| Kuala Selangor | 13(11.4) |
| Petaling | 8(7.0) |
| Sabak Bernam | 8(7.0) |
| Sepang | 7(6.1) |
| Area | |
| Urban | 68(59.6) |
| Rural | 46(40.4) |
| Race | |
| Malay | 99(86.8) |
| Chinese | 1(0.9) |
| Indian | 4(3.5) |
| Other | 10(8.8) |
| Age/year 1 | |
| 20–24 | 14(12.3) |
| 25–29 | 32(28.1) |
| 30–34 | 10(8.8) |
| 35–39 | 34(29.8) |
| 40–44 | 12(10.5) |
| 45–49 | 7(6.1) |
| 50–54 | 1(0.9) |
| Working experience/year 1 | |
| 1–4 | 34(29.8) |
| 5–9 | 21(18.4) |
| 10–14 | 21(18.4) |
| 15–19 | 24(21.1) |
| 20–24 | 7(6.10 |
| 24–29 | 2(1.8) |
| ≥ 30 | 4(3.5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nurdin, M.F.; Yusof, Z.Y.M. Facilitators and Barriers to the Implementation of Preschool Oral Healthcare Programme in Malaysia from the Perspective of Dental Therapists: A Qualitative Study. Children 2020, 7, 266. https://doi.org/10.3390/children7120266
Nurdin MF, Yusof ZYM. Facilitators and Barriers to the Implementation of Preschool Oral Healthcare Programme in Malaysia from the Perspective of Dental Therapists: A Qualitative Study. Children. 2020; 7(12):266. https://doi.org/10.3390/children7120266
Chicago/Turabian StyleNurdin, Muhammad Farid, and Zamros Yuzadi Mohd Yusof. 2020. "Facilitators and Barriers to the Implementation of Preschool Oral Healthcare Programme in Malaysia from the Perspective of Dental Therapists: A Qualitative Study" Children 7, no. 12: 266. https://doi.org/10.3390/children7120266
APA StyleNurdin, M. F., & Yusof, Z. Y. M. (2020). Facilitators and Barriers to the Implementation of Preschool Oral Healthcare Programme in Malaysia from the Perspective of Dental Therapists: A Qualitative Study. Children, 7(12), 266. https://doi.org/10.3390/children7120266