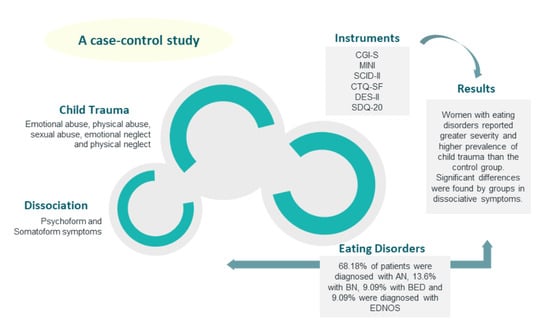
Child Trauma Experiences and Dissociative Symptoms in Women with Eating Disorders: Case-Control Study
Abstract
:1. Introduction
- We expected greater (somatoform and psychoform) dissociation in the group of participants with eating disorders than in the control group;
- We expected greater dissociation amongst the compulsive eating disorder subtypes than amongst the restrictive types;
- We expected a greater severity/prevalence of traumatic events in the group of participants with eating disorders than in the control group;
- We expected a greater severity/prevalence of traumatic events amongst the compulsive eating disorder subtypes than amongst the restrictive types.
2. Method
2.1. Participants
2.2. Procedure
2.3. Measuring Instruments
2.4. Statistical Analysis
3. Results
Socio-Demographic Data
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lanius, R.A.; Vermetten, E.; Pain, C. The Impact of Early Life Trauma on Health and Dissease. The Hidden Epdemic; Cambridge University Press: Cambridge, UK, 2010. [Google Scholar]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Koss, M.P.; Marks, J.S. Reprint of: Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 2019, 56, 774–786. [Google Scholar] [CrossRef] [PubMed]
- Hughes, K.; Bellis, M.A.; Hardcastle, K.A.; Sethi, D.; Butchart, A.; Mikton, C.; Jones, L.; Dunne, M.P. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health 2017, 2, e356–e366. [Google Scholar] [CrossRef] [Green Version]
- Felitti, V.J. Childhood sexual abuse, depression, and family dysfunction in adult obese patients: A case control study. South. Med. J. 1993, 86, 732–736. [Google Scholar] [CrossRef]
- Scheffers, M.; Hoek, M.; Bosscher, R.J.; Van Duijin, M.A.J.; Schoevers, R.A.; Van Busschbach, J.T. Negative body experience in women with early childhood trauma: Associations with trauma severity and dissociation. Eur. J. Psychotraumatol. 2017, 8, 1322892. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van der Kolk, B.A. Clinical implications of neuroscience research in PTSD. Ann. N. Y. Acad. Sci. 2006, 1071, 277–293. [Google Scholar] [CrossRef] [PubMed]
- Petzold, H.G. Integrative Movement and Living Body Based Therapy. A Holistic Path of Living Body Based Psychotherapy; Junfermann: Paderborn, Germany, 1996. [Google Scholar]
- Backhlom, K.; Isomaa, R.; Birgegard, A. The prevalence and impact of trauma history in eating disorders patients. Eur. J. Psychotraumatol. 2013, 4, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Caslini, M.; Bartoli, F.; Crocamo, C.; Dakanalis, A.; Clerici, M.; Carrà, G. Disentangling the association between child abuse and eating disorders: A systematic review and meta-analysis. Psychosom. Med. 2016, 78, 79–90. [Google Scholar] [CrossRef] [PubMed]
- Palmisano, G.L.; Innamorati, M.; Vanderlinden, J. Life adverse experiences in relation with obesity and binge eating disorder: A systematic review. J. Behav. Addict. 2016, 5, 11–31. [Google Scholar] [CrossRef] [Green Version]
- Palmisano, G.L.; Innamorati, M.; Susca, G.; Traetta, D.; Sarracino, D.; Vanderlinden, J. Childhood traumatic experiences and dissociative phenomena in eating disorders: Level and disociation with the severity of binge eating symptoms. J. Trauma Dissociation 2018, 10, 1–20. [Google Scholar] [CrossRef] [Green Version]
- Smolak, L.; Murnen, S. A meta- analytic examination of the relationship between child sexual abuse and eating disorders. Int. J. Eat. Disord. 2002, 31, 136–150. [Google Scholar] [CrossRef]
- Pignatelli, A.M.; Wampers, M.; Loriedo, C.; Biondi, M.; Vanderlinden, J. Childhood neglect in eating disorders: A systematic review and meta- analysis. J. Trauma Dissociation 2017, 18, 100–115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Behar, R.; Arancibia, M.; Sepúlveda, E.; Muga, A. Child sexual abuse as risk factor in eating disorders. In Eating Disorders; Morton, N., Ed.; Nova Science Publishers: Hauppauge, NY, USA, 2016; pp. 149–172. [Google Scholar]
- Moulton, S.J.; Newman, E.; Power, K.; Swanson, V.; Day, K. Chilhood trauma and eating psychopatology: A mediating role for dissociation and emotion dysregulation. Child. Abuse Negl. 2015, 39, 167–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Racine, S.E.; Wildes, J.E. Emotion dysregulation and anorexia nervosa: An exploration of the role of childhood abuse. Int. J. Eat. Disord. 2015, 48, 55–58. [Google Scholar] [CrossRef] [PubMed]
- Vanderlinden, J.; Claes, L.; De Cuyper, K.; Vrieze, E. Dissociation and dissociative disorders. In Encyclopedia of Feeding and Eating Disorders; Wade, T., Ed.; Springer: Singapore, 2015. [Google Scholar]
- Beato, L.; Rodríguez; T. ; Belmonte, A. Relationship of dissociative experiences to body shape concerns in eating disorders. Eur. Eat. Disord. Rev. 2003, 11, 38–45. [Google Scholar] [CrossRef]
- Vanderlinden, J.; Vanderreycken, W.; Van Dyck, R.; Vertommen, H. Dissociative experiences and trauma in eating disorders. Int. J. Eat. Disord. 1993, 13, 187–193. [Google Scholar] [CrossRef]
- La Mela, C.; Maglietta, M.; Castellini, G.; Amoroso, L.; Lucarelli, S. Dissociation in eating disorders: Relationship between dissociative experiences and binge-eating episodes. Compr. Psychiatry 2010, 51, 339–400. [Google Scholar] [CrossRef]
- Lyubomirsky, S.; Casper, R.C.; Sousa, L. What triggers abnormal eating in bulimic and non-bulimic women? The role of dissociative experiences, negative affect, and psychopathology. Psychol. Women Q. 2001, 25, 223–232. [Google Scholar] [CrossRef] [Green Version]
- Rodriguez-Srednicki, O. Childhood sexual abuse, dissociation and adult self-destructive behavior. J. Child Sex Abuse 2001, 10, 75–90. [Google Scholar] [CrossRef]
- Nijenhuis, E.R.S.; Spinhoven, P.; Van Dyck, R.; Van der Hart, O.; Vanderlinden, J. Degree of somatoform and psychological dissociation in dissociative disorder is correlated with reported trauma. J. Trauma Stress 1998, 11, 711–730. [Google Scholar] [CrossRef]
- Nijenhuis, E. Somatoform dissociation: Major symptoms of dissociative disorders. J. Trauma Dissociation 2000, 1, 7–32. [Google Scholar] [CrossRef]
- González-Vázquez, A.; Río-Casanova, L.; Seijo-Almendros, N.; Cabaleiro-Fernández, P.; Seoane-Pillado, T.; Justo-Alonso, A.; Santed-Germán, M.A. Validity and reliability of the Spanish version of the Somatoform Dissociation Questionnaire (SDQ-20). Psicothema 2017, 29, 275–280. [Google Scholar] [PubMed]
- Fuller-Tyszkiewicz, M.; Mussap, A. Examining the dissociative basis for body image disturbances. Int. J. Psychol. Stud. 2011, 3, 3–13. [Google Scholar] [CrossRef]
- Fuller-Tyszkiewicz, M.; Mussap, A. The relationship between dissociation and binge eating. J. Trauma Dissociation 2008, 9, 445–462. [Google Scholar] [CrossRef] [PubMed]
- Brown, L.; Russell, J.; Thornton, C.; Dunn, S. Dissociation, abuse and the eating disorders: Evidence from an Australian population. Aust. N. Z. J. Psychiatry 1999, 33, 521–528. [Google Scholar] [CrossRef]
- Dalle Grave, R.; Oliosi, M.; Todisco, P.; Bartocci, C. Trauma and dissociative experiences in eating disorders. Dissociation Prog. Dissociative Disord. 1996, 9, 274–281. [Google Scholar]
- Oberst, U.; Baltà, M.; Sánchez, L.; Rangil, T. Trastornos disociativos en mujeres con trastornos alimentarios. Rev. Psiqu. Facult. Med. Barc. 2001, 28, 284–290. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Association: Washington, DC, USA, 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5TM); American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Guy, W. Clinical Global Impression; Department of Health, Education and Welfare: Rockville, MD, USA, 1976. [Google Scholar]
- Sheehan, D.V.; Lecrubier, Y.; Harnett-Sheehan, K.; Janavs, J.; Weiller, E.; Bonora, L.I.; Keskiner, A.; Schinka, J.; Knapp, E.; Sheehan, M.F.; et al. Reliability and Validity of the MINI International Neuropsychiatric Interview (mini): According to the SCID-P. Eur. Psychiatry 1997, 12, 232–241. [Google Scholar] [CrossRef]
- Ferrando, L.; Bobes, J.; Gibert, M.; Soto, M.; Soto, O. Mini International Neuropsychiatric Interview. Versión en Español 5.0.0.DSM-IV; Instituto IAP: Madrid, Spain, 1998. [Google Scholar]
- First, M.B.; Gibbon, M.; Spitzer, R.L.; Williams, J.B.W.; Benjamin, L.S. User’s Guide for the Structured Clinical Interview for DSM-IV Axis II Personality Disorders; American Psychiatric Press, Inc.: Washington, DC, USA, 1997. [Google Scholar]
- First, M.B.; Gibbon, M.; Spitzer, R.L.; Williams, J.B.W.; Benjamin, L.S. Entrevista Clínica Estructurada para los Trastornos de Personalidad del Eje II del DSM-IV; Masson: Barcelona, Spain, 1999. [Google Scholar]
- Bernstein, E.M.; Putnam, F.W. Development, reliability, and validity of a dissociation scale. J. Nerv. Mental Dis. 1986, 174, 121–130. [Google Scholar] [CrossRef]
- Carlson, E.B.; Putnam, M.D. An update on the Dissociative Experiences Scale. Dissociation Prog. Dissociative Disord. 1993, 6, 16–25. [Google Scholar]
- Icarán, E.; Colom, R.; Orengo, F. Experiencias disociativas: Una escala de medida. Annu. Psicol. 1996, 70, 69–84. [Google Scholar]
- Icarán, E.; Colom, R.; Orengo, F. Estudio de validación de la escala de experiencias disociativas con muestra de población española. Actas Luso Esp. Neurol. Psiquiatr. Cienc. Afines 1996, 24, 7–10. [Google Scholar]
- Nijenhuis, E.R.S.; Spinhoven, P.; Van Dyck, R.; Van der Hart, O.; Vanderlinden, J. The development and psychometric characteristics os the somatoform dissociation questionnaire (SDQ-20). J. Nerv. Mental Dis. 1996, 184, 688–694. [Google Scholar] [CrossRef]
- Nijenhuis, E.R.R.; Spinhoven, P.; Vanderlinden, J.; Van Dyck, R.; Van der Hart, O. Somatoform dissociative symptoms as related to animal defensive reactions to predatory imminence and injury. J. Abnor. Psychol. 1998, 107, 63–73. [Google Scholar] [CrossRef]
- Bernstein, D.P.; Fink, L. Childhood Trauma Questionnaire: A Retrospective Self-Report Manual; The Psychological Corporation: San Antonio, TX, USA, 1998. [Google Scholar]
- Hernández, A.; Gallardo-Pujol, D.; Pereda, N.; Arntz, A.; Bernstein, D.P.; Gaviria, A.M.; Labal, A.; Valero, J.; Gutiérrez-Zotes, A. Initial validation of Spanish childhood trauma questionnaire-short form: Factor structure, reliability and association with parenting. J. Interpers. Violence 2013, 20, 1–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brewerton, T.D. Eating disorders, trauma and comorbidity: Focus on PTSD. Eat. Disord. 2007, 15, 285–304. [Google Scholar] [CrossRef] [PubMed]
- Carretero-García, A.; Sánchez, L.; Doval, E.; Rusiñol, J.; Raich, R.; Vanderlinden, J. Repeated traumatic experiences in eating disorders and their association with eating symptoms. Eat. Weight Disord. 2012, 17, e267–e273. [Google Scholar] [CrossRef]
- Gleaves, D.H.; Eberenz, K.P. Assessing dissociative symptoms in eating disordered patients: Construct validation of two self-report measures. Int. J. Eat. Disord. 1995, 18, 99–102. [Google Scholar] [CrossRef]
- Vanderlinden, J.; Vandereycken, W. Trauma, Disociación y Descontrol de los Impulsos en los Trastornos Alimentarios; Granica: Barcelona, Spain, 1999. [Google Scholar]
| Variables | AN | BN | BED | EDNOS | p |
|---|---|---|---|---|---|
| Average (SD) | Average (SD) | Average (SD) | Average (SD) | ||
| DES—amnesia | 5.75 (5.96) | 22.5 (20.11) | 26.25 (24.75) | 0.62 (0.88) | 0.082 |
| DES—absorption | 21.68 (13.03) | 38.33 (26.16) | 12 (8.48) | 23 (8.48) | 0.459 |
| DES—depersonalization/derealization | 12 (14.47) | 15 (7.26) | 2.5 (3.53) | 3.33 (4.72) | 0.474 |
| DES—total | 14.43 (11.85) | 28.02 (17.67) | 13.57 (11.11) | 9.29 (3.52) | 0.442 |
| SDQ-20—total | 26.6 (7.92) | 39 (19) | 21 (1.41) | 25.5 (7.77) | 0.255 |
| CTQ—emotional abuse | 11.4 (5.3) | 14.33 (8.14) | 6 (0) | 13 (2.82) | 0.556 |
| CTQ—physical abuse | 6.6 (2.13) | 12.33 (6.35) | 6.5 (2.12) | 7 (2.82) | 0.563 |
| CTQ—sexual abuse | 8.4 (3.56) | 8.67 (4.72) | 5 (0) | 7.5 (2.12) | 0.385 |
| CTQ—emotional neglect | 11.57 (4.65) | 18 (2.64) | 7 (0) | 17.5 (6.36) | 0.059 |
| CTQ—physical neglect | 7.64 (3.67) | 11.33 (5.86) | 6 (1.41) | 9.5 (2.12) | 0.180 |
| CTQ—total | 54.71 (17.14) | 69 (24.74) | 50 (14.14) | 66.5 (12.02) | 0.530 |
| Variables | Group with Eating Disorders | Control Group | p |
|---|---|---|---|
| Average (SD) | Average (SD) | ||
| DES—amnesia | 9.43 (12.64) | 2.32 (4.85) | 0.007 |
| DES—absorption | 23.19 (15.21) | 14.04 (8.65) | 0.015 |
| DES—depersonalization/derealization | 10.75 (12.72) | 1.98 (7.33) | 0.001 |
| DES—total | 15.74 (12.53) | 8.59 (7.65) | 0.026 |
| SDQ-20—total | 27.68 (10.15) | 21.73 (2.16) | 0.024 |
| CTQ—emotional abuse | 11.45 (5.44) | 6.09 (1.17) | 0.001 |
| CTQ—physical abuse | 7.4 (3.39) | 5.42 (0.87) | 0.016 |
| CTQ—sexual abuse | 8.04 (3.44) | 6.33 (2.43) | 0.063 |
| CTQ—emotional neglect | 12.61 (5.23) | 8.88 (2.99) | 0.012 |
| CTQ—physical neglect | 8.19 (3,85) | 5.38 (0,66) | 0.001 |
| CTQ—total | 57.42 (17.09) | 38.42 (6.73) | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rabito-Alcón, M.F.; Baile, J.I.; Vanderlinden, J. Child Trauma Experiences and Dissociative Symptoms in Women with Eating Disorders: Case-Control Study. Children 2020, 7, 274. https://doi.org/10.3390/children7120274
Rabito-Alcón MF, Baile JI, Vanderlinden J. Child Trauma Experiences and Dissociative Symptoms in Women with Eating Disorders: Case-Control Study. Children. 2020; 7(12):274. https://doi.org/10.3390/children7120274
Chicago/Turabian StyleRabito-Alcón, María F., José I. Baile, and Johan Vanderlinden. 2020. "Child Trauma Experiences and Dissociative Symptoms in Women with Eating Disorders: Case-Control Study" Children 7, no. 12: 274. https://doi.org/10.3390/children7120274
APA StyleRabito-Alcón, M. F., Baile, J. I., & Vanderlinden, J. (2020). Child Trauma Experiences and Dissociative Symptoms in Women with Eating Disorders: Case-Control Study. Children, 7(12), 274. https://doi.org/10.3390/children7120274