Compressive Garments in Individuals with Autism and Severe Proprioceptive Dysfunction: A Retrospective Exploratory Case Series
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
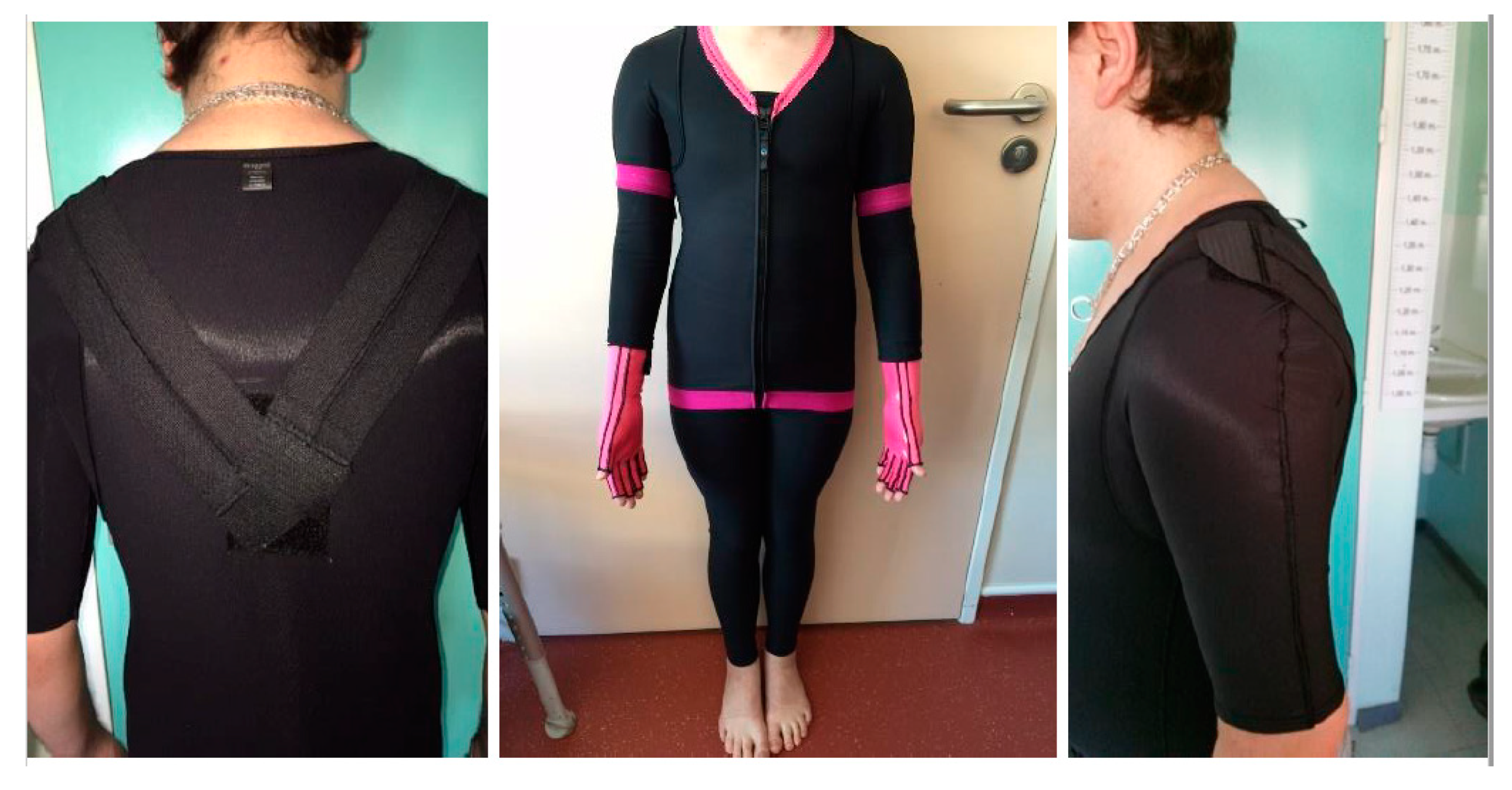
2.3. Intervention: The Compression Garments
2.4. Clinical Measures
2.5. Statistical Analysis
3. Results
3.1. Characteristics of the Participants and Adverse Events
3.2. Outcome Variables
4. Discussion
4.1. Summary of the Results
4.2. Problems Raised by the Use of CGs in Patients with Autism
4.3. Limitations
4.4. Implications for Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Guinchat, V.; Cravero, C.; Diaz, L.; Perisse, D.; Xavier, J.; Amiet, C.; Gourfinkel-An, I.; Bodeau, N.; Wachtel, L.; Cohen, D.; et al. Acute behavioral crises in psychiatric inpatients with autism spectrum disorder (ASD): Recognition of concomitant medical or Non-ASD psychiatric conditions predicts enhanced improvement. Res. Dev. Disabil. 2015, 38, 242–255. [Google Scholar] [CrossRef]
- Tordjman, S.; Anderson, G.M.; Botbol, M.; Brailly-Tabard, S.; Perez-Diaz, F.; Graignic, R.; Carlier, M.; Schmit, G.; Rolland, A.C.; Bonnot, O.; et al. Pain reactivity and plasma Beta-Endorphin in children and adolescents with autistic disorder. PLoS ONE 2009, 4, e5289. [Google Scholar] [CrossRef] [PubMed]
- Cohen, D.; Raffin, M.; Canitano, R.; Bodeau, N.; Bonnot, O.; Périsse, D.; Consoli, A.; Laurent, C. Risperidone or aripiprazole in children and adolescents with autism and/or intellectual disability: A Bayesian Meta-Analysis of efficacy and secondary effects. Res. Autism Spectr. Disord. 2013, 7, 167–175. [Google Scholar] [CrossRef]
- LeClerc, S.; Easley, D. Pharmacological therapies for autism spectrum disorder: A review. Pharm. Ther. 2015, 40, 389–397. [Google Scholar]
- Lambrey, S.; Falissard, B.; Martin-Barrero, M.; Bonnefoy, C.; Quilici, G.; Rosier, A.; Guillin, O. Effectiveness of clozapine for the treatment of aggression in an adolescent with autistic disorder. J. Child Adolesc. Psychopharmacol. 2010, 20, 79–80. [Google Scholar] [CrossRef] [PubMed]
- Frazier, T.W.; Youngstrom, E.A.; Haycook, T.; Sinoff, A.; Dimitriou, F.; Knapp, J.; Sinclair, L. Effectiveness of medication combined with intensive behavioral intervention for reducing aggression in youth with autism spectrum disorder. J. Child Adolesc. Psychopharmacol. 2010, 20, 167–177. [Google Scholar] [CrossRef] [PubMed]
- Wachtel, L.E.; Contrucci-Kuhn, S.A.; Griffin, M.; Thompson, A.; Dhossche, D.M.; Reti, I.M. ECT for Self-Injury in an autistic boy. Eur. Child Adolesc. Psychiatry 2009, 18, 458–463. [Google Scholar] [CrossRef]
- Consoli, A.; Cohen, J.; Bodeau, N.; Guinchat, V.; Wachtel, L.; Cohen, D. Electroconvulsive therapy in adolescents with intellectual disability and severe Self-Injurious behavior and aggression: A retrospective study. Eur. Child Adolesc. Psychiatry 2013, 22, 55–62. [Google Scholar] [CrossRef]
- Iarocci, G.; McDonald, J. Sensory integration and the perceptual experience of persons with autism. J. Autism Dev. Disord. 2006, 36, 77–90. [Google Scholar] [CrossRef] [Green Version]
- Hannant, P.; Tavassoli, T.; Cassidy, S. The Role of Sensorimotor Difficulties in Autism Spectrum Conditions. Front. Neurol. 2016, 7, 124. [Google Scholar] [CrossRef] [Green Version]
- Lane, A.E.; Young, R.L.; Baker, A.E.; Angley, M.T. Sensory processing subtypes in autism: Association with adaptive behavior. J. Autism Dev. Disord. 2010, 40, 112–122. [Google Scholar] [CrossRef] [PubMed]
- Dellapiazza, F.; Michelon, C.; Oreve, M.J.; Robel, L.; Schoenberger, M.; Chatel, C.; Vesperini, S.; Maffre, T.; Schmidt, R.; Blanc, N.; et al. The Impact of Atypical Sensory Processing on Adaptive Functioning and Maladaptive Behaviors in Autism Spectrum Disorder During Childhood: Results From the ELENA Cohort. J. Autism Dev. Disord. 2019, 50, 2142–2152. [Google Scholar] [CrossRef] [PubMed]
- Hazen, E.P.; Stornelli Jl Fau-O’Rourke, J.A.; O’Rourke Ja Fau-Koesterer, K.; Koesterer, K. Fau-McDougle, C.J.; McDougle, C.J. Sensory symptoms in autism spectrum disorders. Harv. Rev. Psychiatry 2014, 22, 112–124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lang, R.; O’Reilly, M.; Healy, O.; Rispoli, M.; Lydon, H.; Streusand, W.; Davis, T.; Kang, S.; Sigafoos, J.; Lancioni, G.; et al. Sensory integration therapy for autism spectrum disorders: A systematic review. Res. Autism Spectr. Disord. 2012, 6, 1004–1018. [Google Scholar] [CrossRef]
- Case-Smith, J.; Weaver, L.L.; Fristad, M.A. A systematic review of sensory processing interventions for children with autism spectrum disorders. Autism 2015, 19, 133–148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wan Yunus, F.; Liu, K.P.; Bissett, M.; Penkala, S. Sensory-Based Intervention for Children with Behavioral Problems: A Systematic Review. J. Autism Dev. Disord. 2015, 45, 3565–3579. [Google Scholar] [CrossRef] [PubMed]
- Ayres, J. Sensory Integration and Learning Disorders; Western Psychological Services: Los Angeles, CA, USA, 1972. [Google Scholar]
- Weimer, A.K.; Schatz, A.M.; Lincoln, A.; Ballantyne, A.O.; Trauner, D.A. “Motor” impairment in Asperger syndrome: Evidence for a deficit in proprioception. J. Dev. Behav. Pediatr. 2001, 22, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Torres, E.B.; Brincker, M.; Isenhower, R.W.; Yanovich, P.; Stigler, K.A.; Nurnberger, J.I.; Metaxas, D.N.; Jose, J.V. Autism: The Micro-Movement perspective. Front. Integr. Neurosci. 2013, 7, 32. [Google Scholar] [CrossRef] [Green Version]
- Fuentes, C.T.; Mostofsky, S.H.; Bastian, A.J. No proprioceptive deficits in autism despite Movement-Related sensory and execution impairments. J. Autism Dev. Disord. 2011, 41, 1352–1361. [Google Scholar] [CrossRef]
- Haswell, C.C.; Izawa, J.; Dowell, L.R.; Mostofsky, S.H.; Shadmehr, R. Representation of internal models of action in the autistic brain. Nat. Neurosci. 2009, 12, 970–972. [Google Scholar] [CrossRef] [Green Version]
- Izawa, J.; Pekny, S.E.; Marko, M.K.; Haswell, C.C.; Shadmehr, R.; Mostofsky, S.H. Motor learning relies on integrated sensory inputs in ADHD, but Over-Selectively on proprioception in autism spectrum conditions. Autism Res. 2012, 5, 124–136. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paton, B.; Hohwy, J.; Enticott, P.G. The rubber hand illusion reveals proprioceptive and sensorimotor differences in autism spectrum disorders. J. Autism Dev. Disord. 2012, 42, 1870–1883. [Google Scholar] [CrossRef] [PubMed]
- Morris, S.L.; Foster, C.J.; Parsons, R.; Falkmer, M.; Falkmer, T.; Rosalie, S.M. Differences in the use of vision and proprioception for postural control in autism spectrum disorder. Neuroscience 2015, 307, 273–280. [Google Scholar] [CrossRef] [PubMed]
- Sharer, E.A.; Mostofsky, S.H.; Pascual-Leone, A.; Oberman, L.M. Isolating Visual and Proprioceptive Components of Motor Sequence Learning in ASD. Autism Res. 2016, 9, 563–569. [Google Scholar] [CrossRef] [Green Version]
- Voight, M.L.; Hardin, J.A.; Blackburn, T.A.; Tippett, S.; Canner, G.C. The effects of muscle fatigue on and the relationship of arm dominance to shoulder proprioception. J. Orthop. Sports Phys. Ther. 1996, 23, 348–352. [Google Scholar] [CrossRef] [Green Version]
- Yahalom, G.; Blatt, I.; Neufeld, M.Y.; Dvir, Z.; Gandelman-Marton, R. Epilepsy Syndrome-Associated balance dysfunction assessed by static posturography. Seizure 2011, 20, 214–217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwaller, F.; Fitzgerald, M. The consequences of pain in early life: Injury-Induced plasticity in developing pain pathways. Eur. J. Neurosci. 2014, 39, 344–352. [Google Scholar] [CrossRef] [Green Version]
- Miyahara, M. Meta review of systematic and meta analytic reviews on movement differences, effect of movement based interventions, and the underlying neural mechanisms in autism spectrum disorder. Front. Integr. Neurosci. 2013, 7, 16. [Google Scholar] [CrossRef] [Green Version]
- Lim, Y.H.; Partridge, K.; Girdler, S.; Morris, S.L. Standing Postural Control in Individuals with Autism Spectrum Disorder: Systematic Review and Meta-analysis. J. Autism Dev. Disord. 2017, 47, 2238–2253. [Google Scholar] [CrossRef]
- Kloeckner, A.; Jutard, C.; Bullinger, A.; Nicoulaud, L.; Tordjman, S.; Cohen, D. Intérêt de l’abord sensorimoteur dans les pathologies autistiques sévères I: Introduction aux travaux d’André Bullinger. Neuropsychiatr. De L’enfance Et De L’adolescence 2009, 57, 154–159. [Google Scholar] [CrossRef]
- Anderson, P.G.; Nienhuis, B.; Mulder, T.; Hulstijn, W. Are older adults more dependent on visual information in regulating Self-Motion than younger adults? J. Mot. Behav. 1998, 30, 104–113. [Google Scholar] [CrossRef] [PubMed]
- Glazebrook, C.; Gonzalez, D.; Hansen, S.; Elliott, D. The role of vision for online control of manual aiming movements in persons with autism spectrum disorders. Autism 2009, 13, 411–433. [Google Scholar] [CrossRef] [PubMed]
- Blanche, E.I.; Reinoso, G.; Chang, M.C.; Bodison, S. Proprioceptive processing difficulties among children with autism spectrum disorders and developmental disabilities. Am. J. Occup. Ther. 2012, 66, 621–624. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olson, L.J.; Moulton, H.J. Occupational therapists’ reported experiences using weighted vests with children with specific developmental disorders. Occup. Ther. Int. 2004, 11, 52–66. [Google Scholar] [CrossRef]
- Hodgetts, S.; Magill-Evans, J. Fau-Misiaszek, J.E.; Misiaszek, J.E. Weighted vests, stereotyped behaviors and arousal in children with autism. J. Autism Dev. Disord. 2011, 41, 41–805. [Google Scholar] [CrossRef]
- Watkins, N.; Sparling, E. The Effectiveness of the Snug Vest on Stereotypic Behaviors in Children Diagnosed With an Autism Spectrum Disorder. Behav. Modif. 2014, 38, 412–427. [Google Scholar] [CrossRef]
- Champagne, T.; Mullen, B.; Dickson, D.; Krishnamurty, S. Evaluating the Safety and Effectiveness of the Weighted Blanket With Adults During an Inpatient Mental Health Hospitalization. Occup. Ther. Ment. Health 2015, 31, 211–233. [Google Scholar] [CrossRef]
- Losinski, M.; Sanders, S.A.; Wiseman, N.M. Examining the Use of Deep Touch Pressure to Improve the Educational Performance of Students With Disabilities: A Meta-Analysis. Res. Pract. Pers. Sev. Disabil. 2016, 41, 3–18. [Google Scholar] [CrossRef]
- Bestbier, L.; Williams, T.I. The Immediate Effects of Deep Pressure on Young People with Autism and Severe Intellectual Difficulties: Demonstrating Individual Differences. Occup. Ther. Int. 2017, 2017, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rombaut, L.; Malfait, F.; Cools, A.; De Paepe, A.; Calders, P. Musculoskeletal complaints, physical activity and Health-Related quality of life among patients with the Ehlers-Danlos syndrome hypermobility type. Disabil. Rehabil. 2010, 32, 1339–1345. [Google Scholar] [CrossRef]
- Clayton, H.A.; Jones, S.A.; Henriques, D.Y. Proprioceptive precision is impaired in Ehlers-Danlos syndrome. SpringerPlus 2015, 4, 323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malfait, F.; Francomano, C.; Byers, P.; Belmont, J.; Berglund, B.; Black, J.; Bloom, L.; Bowen, J.M.; Brady, A.F.; Burrows, N.P.; et al. The 2017 international classification of the Ehlers-Danlos syndromes. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 8–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baeza-Velasco, C.; Cohen, D.; Hamonet, C.; Vlamynck, E.; Diaz, L.; Cravero, C.; Cappe, E.; Guinchat, V. Autism, Joint Hypermobility-Related Disorders and Pain. Front. Psychiatry 2018, 9, 656. [Google Scholar] [CrossRef] [PubMed]
- Cederlof, M.; Larsson, H.; Lichtenstein, P.; Almqvist, C.; Serlachius, E.; Ludvigsson, J.F. Nationwide Population-Based cohort study of psychiatric disorders in individuals with Ehlers-Danlos syndrome or hypermobility syndrome and their siblings. BMC Psychiatry 2016, 16, 207. [Google Scholar] [CrossRef] [Green Version]
- Cravero, C.; Guinchat, V.; Barete, S.; Consoli, A. Cornelia de Lange and Ehlers-Danlos: Comorbidity of two rare syndromes. BMJ Case Rep. 2016, 2016, bcr2015210925. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hamonet, C.; Laouar, R.; Vienne, M.; Brissot, R.; Bernard, J.C.; Comberg, A. Vêtements compressifs et syndrome d’Ehlers-Danlos. Étude multicentrique et prospective sur 49 personnes du handicap avec le Handitest. J. Réadaptation Médicale Prat. Form. Médecine Phys. Réadaptation 2010, 30, 184–191. [Google Scholar] [CrossRef]
- Dupuy, E.G.; Leconte, P.; Vlamynck, E.; Sultan, A.; Chesneau, C.; Denise, P.; Besnard, S.; Bienvenu, B.; Decker, L.M. Ehlers-Danlos Syndrome, Hypermobility Type: Impact of Somatosensory Orthoses on Postural Control (A Pilot Study). Front. Hum. Neurosci. 2017, 11, 283. [Google Scholar] [CrossRef] [Green Version]
- Smith, T.O.; Jerman, E.; Easton, V.; Bacon, H.; Armon, K.; Poland, F.; Macgregor, A.J. Do people with benign joint hypermobility syndrome (BJHS) have reduced joint proprioception? A systematic review and Meta-Analysis. Rheumatol. Int. 2013, 33, 2709–2716. [Google Scholar] [CrossRef]
- Scheper, M.C.; Nicholson, L.L.; Adams, R.D.; Tofts, L.; Pacey, V. The natural history of children with joint hypermobility syndrome and Ehlers-Danlos hypermobility type: A longitudinal cohort study. Rheumatology 2017, 56, 2073–2083. [Google Scholar] [CrossRef] [Green Version]
- Zafeiriou, D.I.; Ververi, A.; Dafoulis, V.; Kalyva, E.; Vargiami, E. Autism spectrum disorders: The quest for genetic syndromes. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2013, 162b, 327–366. [Google Scholar] [CrossRef]
- Baeza-Velasco, C.; Grahame, R.; Bravo, J.F. A connective tissue disorder may underlie ESSENCE problems in childhood. Res. Dev. Disabil. 2017, 60, 232–242. [Google Scholar] [CrossRef] [PubMed]
- Law 2012–300. 5 March 2012. Available online: https://www.legifrance.gouv.fr/affichTexte.do?cidTexte=JORFTEXT000025441587&categorieLien=id (accessed on 21 January 2019).
- APA. Diagnostic and Statistical Manual of Mental Disorders Fifth Edition; American Psychiatric Press: Washington, DC, USA, 2013. [Google Scholar]
- Aman, M.G.; Singh, N.N.; Stewart, A.W.; Field, C.J. The aberrant behavior checklist: A behavior rating scale for the assessment of treatment effects. Am. J. Ment. Defic. 1985, 89, 485–491. [Google Scholar] [PubMed]
- Lord, C.; Rutter, M.; Le Couteur, A. Autism Diagnostic Interview-Revised: A revised version of a diagnostic interview for caregivers of individuals with possible pervasive developmental disorders. J. Autism Dev. Disord. 1994, 24, 659–685. [Google Scholar] [CrossRef] [PubMed]
- Dunn, W. Sensory Profile; Psychological Corporation: San Antonio, TX, USA, 1999. [Google Scholar]
- Bogdashina, O.; Lawson, W. Sensory Perceptual Issues in Autism and Asperger Syndrome: Different Sensory Experiences—Different Perceptual Worlds; Jessica Kingsley Publishers: London, UK, 2003; p. 224. [Google Scholar]
- Vallier, G. Traité de Posturologie Clinique et Thérapeutique—2ème Édition; Posturopole: Fontainebleau, France, 2016; p. 174. [Google Scholar]
- Brown, T.; Lalor, A. The Movement Assessment Battery for Children-Second Edition (MABC-2): A review and critique. Phys. Occup. Ther. Pediatr. 2009, 29, 86–103. [Google Scholar] [CrossRef] [PubMed]
- Sparrow, S.; Cicchetti, D.V.; Balla, D.A. qu’auteur, V.l.n.l.e.t. Vineland-II-Echelles de Comportement Adaptatif de Vineland, 2nd ed.; Pearson: Montreuil, France, 2015. [Google Scholar]
- Chamak, B.; Bonniau, B.; Jaunay, E.; Cohen, D. What can we learn about autism from autistic persons? Psychother. Psychosom. 2008, 77, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Grandin, T. Emergence, Labeled Autistic; Grand Central Publishing: New York, NY, USA, 1986; p. 183. [Google Scholar]
- Rogers, S.J.; Hepburn, S.; Fau-Wehner, E.; Wehner, E. Parent reports of sensory symptoms in toddlers with autism and those with other developmental disorders. J. Autism Dev. Disord. 2003, 33, 631–642. [Google Scholar] [CrossRef]
- Consoli, A.; Gheorghiev, C.; Jutard, C.; Bodeau, N.; Kloeckner, A.; Pitron, V.; Cohen, D.; Bonnot, O. Lorazepam, fluoxetine and packing therapy in an adolescent with pervasive developmental disorder and catatonia. J. Physiol. Paris 2010, 104, 309–314. [Google Scholar] [CrossRef]
- Delion, P.; Labreuche, J.; Deplanque, D.; Cohen, D.; Duhamel, A.; Lallie, C.; Ravary, M.; Goeb, J.L.; Medjkane, F.; Xavier, J. Therapeutic body wraps (TBW) for treatment of severe injurious behaviour in children with autism spectrum disorder (ASD): A 3-Month randomized controlled feasibility study. PLoS ONE 2018, 13, e0198726. [Google Scholar] [CrossRef] [Green Version]
- Chamak, B. Lobbying by association: The case of autism and the controversy over packing therapy in France. Soc. Sci. Med. 2019, 230, 256–263. [Google Scholar] [CrossRef]
- Marko, M.K.; Crocetti, D.; Hulst, T.; Donchin, O.; Shadmehr, R.; Mostofsky, S.H. Behavioural and neural basis of anomalous motor learning in children with autism. Brain 2015, 138, 784–797. [Google Scholar] [CrossRef] [Green Version]
- Collins, D.F.; Prochazka, A. Movement illusions evoked by ensemble cutaneous input from the dorsum of the human hand. J. Physiol. 1996, 496 Pt 3, 857–871. [Google Scholar] [CrossRef] [PubMed]
- Iles, J.F. Evidence for cutaneous and corticospinal modulation of presynaptic inhibition of Ia afferents from the human lower limb. J. Physiol. 1996, 491 Pt 1, 197–207. [Google Scholar] [CrossRef]
- Wakeling, J.M.; Jackman, M.; Fau-Namburete, A.I.; Namburete, A.I. The effect of external compression on the mechanics of muscle contraction. J. Appl. Biomech. 2013, 29, 360–364. [Google Scholar] [CrossRef] [PubMed]
- Nigg, B.M.; Wakeling, J.M. Impact forces and muscle tuning: A new paradigm. Exerc. Sport Sci. Rev. 2001, 29, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Gandevia, S.C.; Smith, J.L.; Crawford, M.; Proske, U.; Taylor, J.L. Motor commands contribute to human position sense. J. Physiol. 2006, 571, 703–710. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, J.; Andreasson, G.O. The effect of external ankle support in chronic lateral ankle joint instability. An electromyographic study. Am. J. Sports Med. 1992, 20, 257–261. [Google Scholar] [CrossRef]
- Kaminski, T.W.; Perrin, D.H. Effect of prophylactic knee bracing on balance and joint position sense. J. Athl. Train 1996, 31, 131–136. [Google Scholar]
- Birmingham, T.B.; Kramer, J.F.; Inglis, J.T.; Mooney, C.A.; Murray, L.J.; Fowler, P.J.; Kirkley, S. Effect of a neoprene sleeve on knee joint position sense during sitting open kinetic chain and supine closed kinetic chain tests. Am. J. Sports Med. 1998, 26, 562–566. [Google Scholar] [CrossRef]
- Cholewicki, J.; Shah, K.R.; McGill, K.C. The effects of a 3-week use of lumbosacral orthoses on proprioception in the lumbar spine. J. Orthop. Sports Phys. Ther. 2006, 36, 225–231. [Google Scholar] [CrossRef]
- Miyamoto, N.; Hirata, K.; Mitsukawa, N.; Yanai, T.; Kawakami, Y. Effect of pressure intensity of graduated elastic compression stocking on muscle fatigue following Calf-Raise exercise. J. Electromyogr. Kinesiol. 2011, 21, 249–254. [Google Scholar] [CrossRef]
- Engel, F.A.; Holmberg, H.C.; Sperlich, B. Is There Evidence that Runners can Benefit from Wearing Compression Clothing? Sports Med. 2016, 46, 1939–1952. [Google Scholar] [CrossRef] [PubMed]
- Loturco, I.; Winckler, C.; Lourenco, T.F.; Verissimo, A.; Kobal, R.; Kitamura, K.; Pereira, L.A.; Nakamura, F.Y. Effects of compression clothing on speed-power performance of elite Paralympic sprinters: A pilot study. SpringerPlus 2016, 5, 1047. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marques-Jimenez, D.; Calleja-Gonzalez, J.; Arratibel, I.; Delextrat, A.; Terrados, N. Are compression garments effective for the recovery of exercise-induced muscle damage? A systematic review with Meta-Analysis. Physiol. Behav. 2016, 153, 133–148. [Google Scholar] [CrossRef]
- Coghlan, N.; Copley, J.; Aplin, T.; Strong, J. Patient Experience of Wearing Compression Garments Post Burn Injury: A Review of the Literature. J. Burn Care Res. 2017, 38, 260–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Tiggelen, D.; Coorevits, P.; Witvrouw, E. The use of a neoprene knee sleeve to compensate the deficit in knee joint position sense caused by muscle fatigue. Scand. J. Med. Sci. Sports 2008, 18, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Southard, V.; DiFrancisco-Donoghue, J.; Mackay, J.; Idjadi, S.; Wright, N. The Effects of Below Knee Compression Garments on Functional Performance in Individuals with Parkinson Disease. Int. J. Health Sci. 2016, 10, 373–380. [Google Scholar] [CrossRef]
- Chopra, P.; Tinkle, B.; Hamonet, C.; Brock, I.; Gompel, A.; Bulbena, A.; Francomano, C. Pain management in the Ehlers-Danlos syndromes. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 212–219. [Google Scholar] [CrossRef] [Green Version]
- Hillier, S.; Immink, M.; Thewlis, D. Assessing Proprioception: A Systematic Review of Possibilities. Neurorehabilit. Neural Repair 2015, 29, 933–949. [Google Scholar] [CrossRef]
- Le Menn-Tripi, C.; Vachaud, A.; Defas, N.; Malvy, J.; Roux, S.; Bonnet-Brilhault, F. Sensory-Psychomotor evaluation in Autism: A new tool for functional diagnosis. Encephale 2019, 45, 312–319. [Google Scholar] [CrossRef]
- Sibley, K.M.; Beauchamp, M.K.; Van Ooteghem, K.; Straus, S.E.; Jaglal, S.B. Using the systems framework for postural control to analyze the components of balance evaluated in standardized balance measures: A scoping review. Arch. Phys. Med. Rehabil. 2015, 96, 122–132.e29. [Google Scholar] [CrossRef] [Green Version]
- Sim, T.; Yoo, H.; Lee, D.; Suh, S.W.; Yang, J.H.; Kim, H.; Mun, J.H. Analysis of sensory system aspects of postural stability during quiet standing in adolescent idiopathic scoliosis patients. J. Neuroeng. Rehabil. 2018, 15, 54. [Google Scholar] [CrossRef]
- Smith, S.A.; Press, B.; Koenig, K.P.; Kinnealey, M. Effects of sensory integration intervention on Self-Stimulating and Self- Injurious behaviors. Am. J. Occup. Ther. 2005, 59, 418–425. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jasmin, E.; Couture, M.; McKinley, P.; Reid, G.; Fombonne, E.; Gisel, E. Sensori-Motor and daily living skills of preschool children with autism spectrum disorders. J. Autism Dev. Disord. 2009, 39, 231–241. [Google Scholar] [CrossRef] [PubMed]
- Eriksson, M.A.; Westerlund, J.; Hedvall, A.; Amark, P.; Gillberg, C.; Fernell, E. Medical conditions affect the outcome of early intervention in preschool children with autism spectrum disorders. Eur. Child Adolesc. Psychiatry 2013, 22, 23–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Clark, D.J.; Christou, E.A.; Ring, S.A.; Williamson, J.B.; Doty, L. Enhanced somatosensory feedback reduces prefrontal cortical activity during walking in older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2014, 69, 1422–1428. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dankerl, P.; Keller, A.K.; Haberle, L.; Stumptner, T.; Pfaff, G.; Uder, M.; Forst, R. Effects on posture by different neuromuscular afferent stimulations and proprioceptive insoles: Rasterstereographic evaluation. Prosthet. Orthot. Int. 2016, 40, 369–376. [Google Scholar] [CrossRef] [Green Version]
- Travers, B.G.; Powell, P.S.; Klinger, L.G.; Klinger, M.R. Motor difficulties in autism spectrum disorder: Linking symptom severity and postural stability. J. Autism Dev. Disord. 2013, 43, 1568–1583. [Google Scholar] [CrossRef] [PubMed]


| Tone (max = 3) (Hypotonia, Hypertonia, and Tonic Fluctuation) | Postural Control (max = 6) (Tiptoeing, Pushing Others or Objects, Leaning on the Ground or Others, Searching for Pressure or Enjoy Being Pulled, Head Down, and Balance Difficulties) | Motor Control (max = 5) (Crashing and Falling, Movement Overactivity, Poor Joint Alignment, Stiff Movements, and Movement Avoidance) | Stereotypies (max = 5) (Spinning and Running, Seeking Body Vibrations, Swinging Movements, Turning One’s Head, Breath-Hold, and Shouts) | |
|---|---|---|---|---|
| P1 | 1 | 4 | 4 | 3 |
| P2 | 2 | 3 | 3 | 3 |
| P3 | 2 | 4 | 1 | 3 |
| P4 | 2 | 2 | 4 | 2 |
| P5 | 1 | 2 | 2 | 0 |
| P6 | 1 | 3 | 1 | 4 |
| P7 | 3 | 5 | 3 | 3 |
| P8 | 1 | 3 | 1 | 1 |
| P9 | 0 | 4 | 1 | 5 |
| P10 | 2 | 3 | 2 | 2 |
| P11 | 2 | 1 | 2 | 0 |
| P12 | 1 | 2 | 2 | 3 |
| P13 | 2 | 2 | 3 | 2 |
| P14 | 1 | 3 | 4 | 3 |
| Socio-Demographics | |
|---|---|
| Males: N (%) | 13 (93) |
| Age (years): mean (±SD) [range] | 18.2 (±5.5) [8.2–30.0] |
| SES: N (%), low/middle/high | 4 (29)/3 (21)/7 (50) |
| Hospitalization | |
| Duration (months): mean (±SD) [range] | 10.8 (±5.5) [0.1–21.5] |
| Comorbidities: N (%) | |
| Syndromic ASD | 7 (50) |
| Epilepsy | 6 (43) |
| Catatonia | 6 (43) |
| Obesity | 3 (21) |
| OSA | 1 (7) |
| Osteoporosis | 1 (7) |
| GERD | 3 (21) |
| Esophagitis, duodenitis, gastritis | 11 (79) |
| Chronic constipation | 12 (86) |
| ENT and maxillofacial infections | 4 (29) |
| Parasitic infection | 3 (21) |
| Cardiopathy | 2 (14) |
| Anemia | 3 (21) |
| Pruritic skin diseases | 2 (14) |
| Iatrogeny | 3 (21) |
| At baseline | |
| Patients receiving medication: N (%) | 13 (93) |
| Poly-medication: N (%) | 10 (71) |
| Equivalent of chlorpromazine (mg) per patient receiving medication: mean (±SD) [range] | 664 (±665) [67–1750] |
| History of exception treatment: N (%) | |
| ECT | 2 (14) |
| TBW | 3 (21) |
| During the CG trial | |
| Change in medication: N (%) | 2 (14) |
| Change in equivalent chlorpromazine | −105 mg in one patient, +150 mg in another patient |
| List of compounds: N (%) | 10 |
| Antipsychotic | 6 |
| Anticonvulsant | 5 |
| Antidepressant | 3 |
| Mood stabilizer | 1 |
| Psychostimulant | 12 |
| Melatonin | 5 |
| Antiparkinsonian | 7 |
| Benzodiazepine | |
| Gastrointestinal comfort treatment (laxative, gastric protector, anti-reflux drug) | 26 |
| Oxygen therapy | 1 |
| Analgesic (level 2 or 3) | 3 |
| Other drugs | 3 |
| Physiotherapy: N (%) | 4 |
| Autism History | |
| ADI-R: 4–5 years, mean (±SD) * | |
| Social impairment score | 26.1 (±2.8) |
| Communication score | 9.6 (±2.1) |
| Repetitive interests score | 7.7 (±2.4) |
| Developmental score | 4.7 (±1.8) |
| Clinical Characteristics | |
| Main reason for referral | Self-injurious behavior (N = 7) Catatonia (N = 2) Agitation (N = 2) Destructive behavior (N = 2) Hetero-aggression (N = 1) |
| Language | Fluent (N = 0) Few words (N = 7) Non-verbal (N = 7) |
| ABC, mean (±SD) [range] | 61 (±23) [21–109] |
| CARS, mean (±SD) [range] | 38 (±5) [30–51] |
| Vineland Adaptive Behavior Scales-II ** | |
| Developmental age: years | 2.7 (±1.1) [1.8–5] |
| Variable | Baseline | T-1 (after CG) | Delta | Effect Size | p * |
|---|---|---|---|---|---|
| ABC Scores | |||||
| ABC-irritability | 21.64 (9.52) | 16.46 (9.03) | −5.18 (7.78) | −0.65 | 0.028 |
| ABC-lethargy | 12.79 (8.14) | 7.57(6.89) | −5.21 (4.25) | −1.19 | 0.002 |
| ABC-stereotypies | 7.64 (3.77) | 6.71 (3.09) | −0.93 (2.5) | −0.36 | NS |
| ABC-hyperactivity | 17.36 (12.59) | 11.61 (8.85) | −5.75 (7.97) | −0.7 | 0.003 |
| ABC-inappropriate speech | 1.79 (3.38) | 1.68 (3.21) | −0.11 (1.76) | −0.06 | NS |
| ABC-total | 61.21 (23.44) | 44.04 (20.19) | −17.18 (20.19) | −0.83 | 0.008 |
| DUNN Questionnaire | |||||
| Auditory processing | 2.2 (0.92) | 2.4 (0.7) | 0.2 (0.79) | 0.24 | 0.586 |
| Visual processing | 2.6 (0.7) | 2.7 (0.48) | 0.1 (0.57) | 0.17 | 0.773 |
| Vestibular processing | 2.5 (0.85) | 2.6 (0.7) | 0.1 (0.74) | 0.13 | 1 |
| Touch processing | 2 (0.82) | 2.3 (0.82) | 0.3 (0.82) | 0.35 | 0.345 |
| Multisensory processing | 1.9 (0.74) | 2.1 (0.88) | 0.2 (0.92) | 0.21 | 0.572 |
| Oral sensory processing | 2.2 (0.92) | 2.4 (0.84) | 0.2 (0.79) | 0.24 | 0.586 |
| Sensory processing related to endurance/tone | 2 (0.82) | 2 (0.82) | 0 (0.47) | 0 | 1 |
| Modulation related to body position and movement | 2.1 (0.88) | 2.3 (0.82) | 0.2 (0.63) | 0.3 | 1 |
| Modulation of movement affecting activity level | 2.9 (0.32) | 3 (0) | 0.1 (0.32) | 0.3 | 1 |
| Modulation of sensory input affecting emotional responses and activity level | 2.5 (0.71) | 2.5 (0.71) | 0 (0.82) | 0 | 1 |
| Modulation of visual input affecting emotional responses and activity level | 2 (0.47) | 2.4 (0.7) | 0.4 (0.52) | 0.74 | 0.072 |
| Emotional/social responses | 1.7 (0.95) | 1.7 (0.67) | 0 (0.94) | 0 | 1 |
| Behavioral outcomes of sensory processing | 2 (0.82) | 1.8 (0.63) | −0.2 (0.42) | −0.45 | 0.346 |
| Items indicating thresholds for responses | 2.1 (0.88) | 2.3 (0.95) | 0.2 (0.42) | 0.45 | 0.346 |
| DUNN Factors | |||||
| Sensory seeking | 2.7 (0.67) | 2.8 (0.63) | 0.1 (0.32) | 0.3 | 1 |
| Emotionally reactive | 2.1 (0.88) | 2.1 (0.88) | 0 (0.67) | 0 | 1 |
| Low endurance/tone | 2 (0.82) | 2.1 (0.88) | 0.1 (0.57) | 0.17 | 0.773 |
| Oral sensory sensitivity | 2.5 (0.71) | 2.5 (0.85) | 0 (0.82) | 0 | 1 |
| Inattention/distractibility | 2.5 (0.71) | 2.6 (0.52) | 0.1 (0.74) | 0.13 | 1 |
| Poor registration | 1.6 (0.7) | 2.1 (0.88) | 0.5 (0.53) | 0.91 | 0.037 |
| Sensory sensitivity | 2.3 (0.95) | 2.5 (0.85) | 0.2 (0.42) | 0.45 | 0.346 |
| Sedentary | 2.8 (0.42) | 2.7 (0.48) | −0.1 (0.32) | −0.3 | 1 |
| Fine motor/perceptual | 1.9 (0.99) | 1.5 (0.85) | −0.4 (0.7) | −0.55 | 0.174 |
| Motricity Path | |||||
| Successful items | 23.73 (18.45) | 29.91 (20.43) | 6.18 (7.31) | 0.81 | 0.025 |
| Emerging items | 12.91 (9.88) | 11.82 (9.9) | −1.09 (6.5) | −0.16 | 0.442 |
| Failed items | 13.27 (12.19) | 8.18 (8.87) | −5.09 (9.16) | −0.53 | 0.074 |
| Postural Control | |||||
| Frontal (mediolateral) | NA | NA | 0.92 (0.67) | 1.37 ** | 0.006 |
| Profile (anteroposterior) | NA | NA | 1.36 (0.81) | 1.69 ** | 0.007 |
| hEDS/ HSD * | Residual Symptoms before CG | Profile View | Dorsal View | CGI after CG | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Post Scapular Plan dev | Ant Scapular Plan dev | Changes Observed with CG | Global Lateral Deviation | Cervico-Dorsal Deviation | Lateral Rotation Deviation | Changes Observed with CG | ||||
| P1 | yes | SIB | 1 | 0 | no change | 1 | 0 | 0 | improved | improved |
| P2 | yes | SIB | 0 | 1 | no change | 0 | normalized | improved | ||
| P3 | yes | SIB | 0 | 1 | improved | 0 | 0 | 1 | improved | improved |
| P4 | yes | SIB | 0 | 1 | improved | 1 | 1 | 0 | improved | improved |
| P5 | yes | catatonia | 0 | 1 | normalized | 0 | 1 | 0 | improved | improved |
| P6 | yes | SIB | 0 | 0 | no change | 1 | 0 | 0 | improved | improved |
| P7 | yes | SIB | NE | NE | NE | NE | NE | NE | NE | improved |
| P8 | no | SIB | NE | NE | NE | NE | NE | NE | NE | worsen |
| P9 | no | instability | 0 | 0 | no change | 1 | 0 | 0 | normalized | improved |
| P10 | no | SIB | NE | NE | NE | 1 | 0 | 0 | normalized | improved |
| P11 | no | catatonia | 1 | 0 | normalized | 0 | no change | improved | ||
| P12 | no | SIB | 0 | 1 | normalized | 1 | 0 | no change | improved | |
| P13 | no | instability | 0 | 1 | normalized | 1 | 0 | 0 | no change | improved |
| P14 | no | hyperpnea | 0 | 1 | normalized | 1 | 0 | 0 | no change | improved |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guinchat, V.; Vlamynck, E.; Diaz, L.; Chambon, C.; Pouzenc, J.; Cravero, C.; Baeza-Velasco, C.; Hamonet, C.; Xavier, J.; Cohen, D. Compressive Garments in Individuals with Autism and Severe Proprioceptive Dysfunction: A Retrospective Exploratory Case Series. Children 2020, 7, 77. https://doi.org/10.3390/children7070077
Guinchat V, Vlamynck E, Diaz L, Chambon C, Pouzenc J, Cravero C, Baeza-Velasco C, Hamonet C, Xavier J, Cohen D. Compressive Garments in Individuals with Autism and Severe Proprioceptive Dysfunction: A Retrospective Exploratory Case Series. Children. 2020; 7(7):77. https://doi.org/10.3390/children7070077
Chicago/Turabian StyleGuinchat, Vincent, Elodie Vlamynck, Lautaro Diaz, Coralie Chambon, Justine Pouzenc, Cora Cravero, Carolina Baeza-Velasco, Claude Hamonet, Jean Xavier, and David Cohen. 2020. "Compressive Garments in Individuals with Autism and Severe Proprioceptive Dysfunction: A Retrospective Exploratory Case Series" Children 7, no. 7: 77. https://doi.org/10.3390/children7070077
APA StyleGuinchat, V., Vlamynck, E., Diaz, L., Chambon, C., Pouzenc, J., Cravero, C., Baeza-Velasco, C., Hamonet, C., Xavier, J., & Cohen, D. (2020). Compressive Garments in Individuals with Autism and Severe Proprioceptive Dysfunction: A Retrospective Exploratory Case Series. Children, 7(7), 77. https://doi.org/10.3390/children7070077





