Post-Traumatic Stress Symptoms among Lithuanian Parents Raising Children with Cancer
Abstract
:1. Introduction
2. Materials and Methods
2.1. Research Tools
2.2. Data Analysis
3. Results
3.1. Experimental-Setup Characteristics
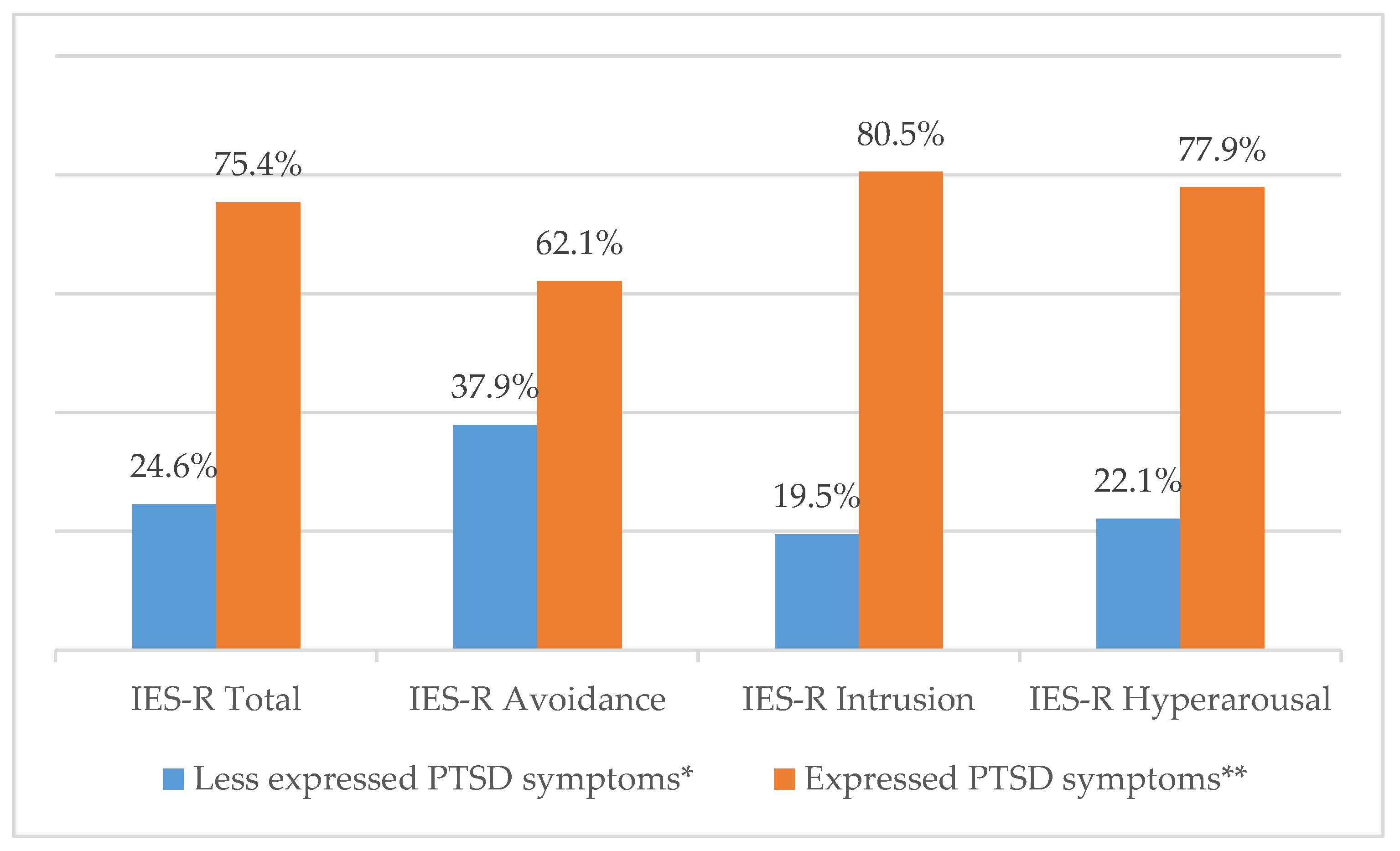
3.2. PTSS Expression among Parents of Children with Cancer
3.3. PTSS Expression in Parents of Children with Oncologic Disease by Sociodemographic Factor
3.4. Parental PTSS Expression by Medical Factors of Child’s Cancer
3.5. Sociodemographic and Medical Factors Predicting Parental PTSD Symptom Expression
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lindahl Norberg, A.; Pöder, U.; von Essen, L. Early avoidance of disease- and treatment-related distress predicts post-traumatic stress in parents of children with cancer. Eur. J. Oncol. Nurs. 2011. [Google Scholar] [CrossRef] [PubMed]
- Steliarova-Foucher, E.; Colombet, M.; Ries, L.A.G.; Moreno, F.; Dolya, A.; Bray, F.; Hesseling, P.; Shin, H.Y.; Stiller, C.A.; Bouzbid, S.; et al. International incidence of childhood cancer, 2001–10: A population-based registry study. Lancet Oncol. 2017. [Google Scholar] [CrossRef]
- Kazak, A.E.; Alderfer, M.; Rourke, M.T.; Simms, S.; Streisand, R.; Grossman, J.R. Posttraumatic Stress Disorder (PTSD) and Posttraumatic Stress Symptoms (PTSS) in families of adolescent childhood cancer survivors. J. Pediatr. Psychol. 2004. [Google Scholar] [CrossRef] [PubMed]
- Makari, J.; Zaborskis, A.; Labanauskas, L.; Rageliene, L. The quality of life of children suffering from oncologic diseases in Lithuania. Medicina 2007, 43, 726. [Google Scholar] [CrossRef] [Green Version]
- Muscara, F.; Burke, K.; Mccarthy, M.C.; Anderson, V.A.; Hearps, S.J.C.; Hearps, S.J.; Dimovski, A.; Nicholson, J.M. Parent distress reactions following a serious illness or injury in their child: A protocol paper for the take a breath cohort study. BMC Psychiatry 2015. [Google Scholar] [CrossRef] [Green Version]
- Compas, B.E.; Bemis, H.; Gerhardt, C.A.; Dunn, M.J.; Rodriguez, E.M.; Desjardins, L.; Preacher, C.J.; Manring, S.; Vannatta, K. Mothers and fathers coping with their children’s cancer: Individual and interpersonal processes. Heal. Psychol. 2015, 7, 405–411. [Google Scholar] [CrossRef]
- Davidson, J.E.; Jones, C.; Bienvenu, O.J. Family response to critical illness: Postintensive care syndrome-family. Crit. Care Med. 2012, 40, 618–624. [Google Scholar] [CrossRef]
- Pöder, U.; Ljungman, G.; von Essen, L. Posttraumatic stress disorder among parents of children on cancer treatment: A longitudinal study. Psychooncology 2008. [Google Scholar] [CrossRef]
- Jantien Vrijmoet-Wiersma, C.M.; Van Klink, J.M.M.; Kolk, A.M.; Koopman, H.M.; Ball, L.M.; Maarten Egeler, R. Assessment of parental psychological stress in pediatric cancer: A review. J. Pediatr. Psychol. 2008, 33, 694–706. [Google Scholar] [CrossRef] [Green Version]
- Kazak, A.E.; Boeving, C.A.; Alderfer, M.A.; Hwang, W.T.; Reilly, A. Posttraumatic stress symptoms during treatment in parents of children with cancer. J. Clin. Oncol. 2005. [Google Scholar] [CrossRef]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th Revision, Fifth Edition. 2016. Available online: https://apps.who.int/iris/handle/10665/246208 (accessed on 20 January 2020).
- Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013.
- Norberg, A.L.; Boman, K.K. Mothers and fathers of children with cancer: Loss of control during treatment and posttraumatic stress at later follow-up. Psychooncology. 2013. [Google Scholar] [CrossRef] [PubMed]
- Dunn, M.J.; Rodriguez, E.M.; Barnwell, A.S.; Grossenbacher, J.C.; Vannatta, K.; Gerhardt, C.A.; Compas, B.E. Posttraumatic stress symptoms in parents of children with cancer within six months of diagnosis. Heal. Psychol. 2012. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greening, L.; Stoppelbein, L.; Cheek, K. Racial/ethnic disparities in the risk of posttraumatic stress disorder symptoms among mothers of children diagnosed with cancer and Type-1 diabetes mellitus. Psychol. Trauma Theory Res. Pr. Policy 2017. [Google Scholar] [CrossRef] [PubMed]
- Stoppelbein, L.; Greening, L.; Fite, P. The role of cortisol in PTSD among women exposed to a trauma-related stressor. J. Anxiety Disord. 2012. [Google Scholar] [CrossRef] [Green Version]
- Jurbergs, N.; Long, A.; Ticona, L.; Phipps, S. Symptoms of posttraumatic stress in parents of children with cancer: Are they elevated relative to parents of healthy children? J. Pediatr. Psychol. 2009. [Google Scholar] [CrossRef] [Green Version]
- Norberg, A.L.; Pöder, U.; Ljungman, G.; von Essen, L. Objective and subjective factors as predictors of post-traumatic stress symptoms in parents of children with cancer—A longitudinal study. PLoS ONE 2012, 7, 036218. [Google Scholar] [CrossRef]
- Naderi, M.; Moghadam, M.F.; Hamzenejad, M.; Emamdadi, A.; Karami, H. Post-Traumatic stress disorder and related factors in parents of children with cancer in south-east of Iran. Iran. Red Crescent Med. J. 2012. [Google Scholar] [CrossRef] [Green Version]
- Landolt, M.A.; Ystrom, E.; Sennhauser, F.H.; Gnehm, H.E.; Vollrath, M.E. The mutual prospective influence of child and parental post-traumatic stress symptoms in pediatric patients. J. Child. Psychol. Psychiatry Allied Discip. 2012. [Google Scholar] [CrossRef]
- Mccarthy, M.C.; Ashley, D.M.; Lee, K.J.; Anderson, V.A. Predictors of acute and posttraumatic stress symptoms in parents following their child’s cancer diagnosis. J. Trauma. Stress 2012. [Google Scholar] [CrossRef]
- Boman, K.K.; Kjällander, Y.; Eksborg, S.; Becker, J. Impact of prior traumatic life events on parental early stage reactions following a child’s cancer. PLoS ONE 2013, 8, 057556. [Google Scholar] [CrossRef] [Green Version]
- Kazlauskas, E.; Gailiene, D.; Domanskaite-Gota, V.; Trofimova, J. Psychometric properties of the Lithuanian version of the Impact of Event Scale-Revised (IES-R). Psichology 2006, 22–30. [Google Scholar]
- Weiss, D.S.; Marmar, C.R. The Impact of Event Scale—Revised. In Assessing Psychological Trauma and PTSD; American Psychological Association: Washington, DC, USA, 1997; ISBN 1-57230-162-7. [Google Scholar]
- Creamer, M.; Bell, R.; Failla, S. Psychometric properties of the Impact of Event Scale—Revised. Behav. Res. 2003. [Google Scholar] [CrossRef] [PubMed]
- Weiss, D.S. The impact of event scale: Revised. In Cross-Cultural Assessment of Psychological Trauma and PTSD; American Psychological Association: Washington, DC, USA, 2007; ISBN 9788578110796. [Google Scholar]
- Björk, M.; Wiebe, T.; Hallström, I. Striving to survive: Families’ lived experiences when a child is diagnosed with cancer. J. Pediatr. Oncol. Nurs. 2005. [Google Scholar] [CrossRef] [PubMed]
- van Warmerdam, J.; Zabih, V.; Kurdyak, P.; Sutradhar, R.; Nathan, P.C.; Gupta, S. Prevalence of anxiety, depression, and posttraumatic stress disorder in parents of children with cancer: A meta-analysis. Pediatr. Blood Cancer 2019. [Google Scholar] [CrossRef] [PubMed]
- Malinauskienė, V.; Bernotaitė, L. The impact of event scale–revised: Psychometric properties of the Lithuanian version in a sample of employees exposed to workplace bullying. Acta Med. Litu. 2016. [Google Scholar] [CrossRef] [Green Version]
- Deng, L.X.; Khan, A.M.; Drajpuch, D.; Fuller, S.; Ludmir, J.; Mascio, C.E.; Partington, S.L.; Qadeer, A.; Tobin, L.; Kovacs, A.H.; et al. Prevalence and correlates of post-traumatic stress disorder in adults with congenital heart disease. Am. J. Cardiol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Rash, C.J.; Coffey, S.F.; Baschnagel, J.S.; Drobes, D.J.; Saladin, M.E. Psychometric properties of the IES-R in traumatized substance dependent individuals with and without PTSD. Addict. Behav. 2008. [Google Scholar] [CrossRef] [Green Version]
- Rabineau, K.M.; Mabe, P.A.; Vega, R.A. Parenting stress in pediatric oncology populations. J. Pediatr. Hematol. Oncol. 2008. [Google Scholar] [CrossRef]
- Karadeniz Cerit, K.; Cerit, C.; Nart, Ö.; Eker, N.; Kıyan, G.; Dağlı, T.; Ekingen, G.; Tokuç, G.; Karaca, Ö.; Çorapçıoğlu, F. Post-traumatic stress disorder in mothers of children who have undergone cancer surgery. Pediatr. Int. 2017. [Google Scholar] [CrossRef]
- Conrad, D.; Wilker, S.; Pfeiffer, A.; Lingenfelder, B.; Ebalu, T.; Lanzinger, H.; Elbert, T.; Kolassa, I.T.; Kolassa, S. Does trauma event type matter in the assessment of traumatic load? Eur. J. Psychotraumatol. 2017. [Google Scholar] [CrossRef] [Green Version]
- Karunakara, U.K.; Neuner, F.; Schauer, M.; Singh, K.; Hill, K.; Elbert, T.; Burnha, G. Traumatic events and symptoms of post-traumatic stress disorder amongst Sudanese nationals, refugees and Ugandans in the West Nile. Afr. Health Sci. 2004, 4, 83–93. [Google Scholar] [PubMed]
- Bruce, M.; Gumley, D.; Isham, L.; Fearon, P.; Phipps, K. Post-traumatic stress symptoms in childhood brain tumour survivors and their parents. Child. Care. Health Dev. 2011. [Google Scholar] [CrossRef] [PubMed]
- Irish, L.A.; Fischer, B.; Fallon, W.; Spoonster, E.; Sledjeski, E.M.; Delahanty, D.L. Gender differences in PTSD symptoms: An exploration of peritraumatic mechanisms. J. Anxiety Disord. 2011, 25, 209–216. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duncan, L.E.; Ratanatharathorn, A.; Aiello, A.E.; Almli, L.M.; Amstadter, A.B.; Ashley-Koch, A.E.; Baker, D.G.; Beckham, J.C.; Bierut, L.J.; Bisson, J.; et al. Largest GWAS of PTSD (N=20 070) yields genetic overlap with schizophrenia and sex differences in heritability. Mol. Psychiatry 2018. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Sonnega, A.; Bromet, E.; Hughes, M.; Nelson, C.B. Posttraumatic Stress Disorder in the National Comorbidity Survey. Arch. Gen. Psychiatry 1995. [Google Scholar] [CrossRef]
- McQueen, C.; Henwood, K. Young men in “crisis”: Attending to the language of teenage boys’ distress. Soc. Sci. Med. 2002. [Google Scholar] [CrossRef]
- Cadell, S.; Hemsworth, D.; Quosai, T.S.; Steele, R.; Davies, E.; Liben, S.; Straatman, L.; Siden, H. Posttraumatic growth in parents caring for a child with a life-limiting illness: A structural equation model. Am. J. Orthopsychiatry 2014. [Google Scholar] [CrossRef]
- Stoppelbein, L.A.; Greening, L.; Elkin, T.D. Risk of posttraumatic stress symptoms: A comparison of child survivors of pediatric cancer and parental bereavement. J. Pediatr. Psychol. 2006. [Google Scholar] [CrossRef]
- Chaves, C.; Lopez-Gomez, I.; Hervas, G.; Vazquez, C. A Comparative Study on the Efficacy of a Positive Psychology Intervention and a Cognitive Behavioral Therapy for Clinical Depression. Cogn. Res. 2017. [Google Scholar] [CrossRef]
| Factors | n (%) | |
|---|---|---|
| Gender | Male | 44 (22.6) |
| Female | 151 (77.4) | |
| Age (years) | 19–39 | 121 (62.1) |
| 40–64 | 74 (37.9) | |
| Education | Higher education | 112 (57.4) |
| Below higher education | 83 (42.6) | |
| Place of residence | Urban | 128 (65.6) |
| Rural | 67 (34.4) | |
| Employment | Professionally active | 118 (60.5) |
| Professionally inactive | 77 (39.5) | |
| Financial situation | Good | 44 (22.6) |
| Worse than good | 150 (76.9) | |
| Marital status | In couple | 168 (86.2) |
| Single | 27 (13.8) | |
| Number of children in the family | 1 | 58 (29.7) |
| 2 | 88 (45.1) | |
| 3 and more | 48 (24.6) | |
| Involvement in childcare | Direct (permanent) | 157 (80.5) |
| Indirect (periodic) | 38 (19.5) | |
| Gender of child with cancer | Male | 98 (50.3) |
| Female | 97 (49.7) | |
| Age of child with cancer (years) | 1–10 | 128 (65.5) |
| 11–17 | 65 (33.3) | |
| Cancer type | Blood and lymph | 82 (42.1) |
| Central nervous system | 47 (24.1) | |
| Solid tumor | 66 (33.8) | |
| Disease duration | Shorter than one year | 106 (54.4) |
| Longer than one year | 89 (45.6) | |
| Cancer stage | I | 9 (4.6) |
| II | 29 (14.9) | |
| III | 29 (14.9) | |
| IV | 31 (15.9) | |
| Not specified | 78 (40.0) | |
| Treatment method | Surgery | 5 (2.6) |
| Chemotherapy | 79 (40.5) | |
| Radiotherapy | 12 (6.2) | |
| Bone-marrow transplantation | 8 (4.1) | |
| Follow-up after treatment | 87 (44.6) | |
| Chemotherapy and radiotherapy together | 4 (2.1) | |
| Relapse | Occurred | 46 (23.6) |
| Did not occur | 128 (65.6) | |
| Subjectively perceived treatment prognosis | Good | 55 (28.2) |
| Bad | 111 (56.9) | |
| IES-R | N | Minimum | Maximum | Mean | Standard Deviation (SD) |
|---|---|---|---|---|---|
| IES-R Total | 195 | 0 | 3.86 | 2.01 | 0.76 |
| IES-R Avoidance | 195 | 0 | 3.75 | 1.70 | 0.77 |
| IES-R Intrusion | 195 | 0 | 4.00 | 2.24 | 0.88 |
| IES-R Hyperarousal | 195 | 0 | 4.00 | 2.13 | 0.96 |
| Sociodemographic Factor | IES-R Total | p | ||
|---|---|---|---|---|
| Mean (SD) | ||||
| Gender | Male | 2.19 (0.68) | <0.001 | |
| Female | 1.40 (0.72) | |||
| Age (years) | 19–39 | 1.91 (0.74) | 0.018 | |
| 40–64 | 2.17 (0.77) | |||
| Education | Higher education | 1.94 (0.81) | 0.127 | |
| Below higher education | 2.10 (0.69) | |||
| Place of residence | Urban | 2.02 (0.73) | 0.842 | |
| Rural | 1.99 (0.81) | |||
| Employment | Professionally active | 1.91 (0.78) | 0.029 | |
| Professionally inactive | 2.16 (0.70) | |||
| Financial situation | Good | 1.91 (0.72) | 0.337 | |
| Worse than good | 2.04 (0.77) | |||
| Number of children in the family | 1–2 | 1.96 (0.73) | 0.172 | |
| 3 and more | 2.13 (0.84) | |||
| Gender of child with cancer | Male | 1.96 (0.72) | 0.339 | |
| Female | 2.06 (0.79) | |||
| Age of child with cancer (years) | 1–10 | 1.91 (0.80) | 0.005 | |
| 11–17 | 2.21 (0.65) | |||
| Median (min; max) | Mean Rank | p | ||
| Marital status | In couple | 2.00 (0.00; 3.86) | 95.79 | 0.173 |
| Single | 2.00 (1.36; 3.48) | 111.74 | ||
| Involvement in childcare | Direct (permanent) | 2.05 (0.05; 3.86) | 106.25 | <0.001 |
| Indirect (periodic) | 1.50 (0.00; 3.45) | 63.93 | ||
| Medical Factors | Mean (SD) of Total IES-R | p | ||
| Cancer type | Blood and lymph | 2.00 (0.76) | 0.988 | |
| Central nervous system | 2.00 (0.78) | |||
| Solid tumor in different organs | 2.02 (0.75) | |||
| Disease duration | Shorter than one year | 1.97 (0.76) | 0.495 | |
| Longer than one year | 2.05 (0.76) | |||
| Relapse | Occurred | 2.39 (0.59) | <0.001 | |
| Did not occur | 1.85 (0.78) | |||
| Subjectively perceived treatment prognosis | Good | 1.87 (0.77) | 0.106 | |
| Bad | 2.08 (0.79) | |||
| Medical Factors | Median (min; max) | Mean Rank | p | |
| Treatment method | Surgery | 2.27 (1.73; 3.27) | 127.4 | 0.162 |
| Chemotherapy | 1.90 (0.00; 3.36) | 87.31 | ||
| Radiotherapy | 1.90 (1.36; 2.36) | 79.46 | ||
| Bone-marrow transplantation | 2.18 (1.50; 2.68) | 109.06 | ||
| Follow-up after treatment | 2.05 (0.68; 3.86) | 103.17 | ||
| Cancer stage | I | 2.00 (0.68; 2.91) | 85.78 | 0.026 |
| II | 2.14 (1.23; 3.36) | 104.55 | ||
| III | 1.68 (1.05; 3.48) | 76.78 | ||
| IV | 2.36 (0.05; 3.27) | 107.37 | ||
| Not specified | 1.98 (0.00; 3.86) | 79.71 | ||
| Factors | Simple Linear Regression | Multiple Linear Regression | |||||
|---|---|---|---|---|---|---|---|
| β | 95% CI | p | β | 95% CI | βs | p | |
| Gender (female vs. male) | 0.79 | 0.56; 1.00 | <0.001 | 0.83 | 0.60; 1.00 | 0.45 | <0.001 |
| Age (years; 40−64 vs. 19−39) | 0.27 | 0.05; 0.49 | 0.018 | - | - | - | - |
| Education (higher education vs. below higher education) | −0.17 | −0.38; 0.52 | 0.135 | −0.21 | −0.41; −0.17 | −0.14 | 0.034 |
| Place of residence (rural vs. urban) | −0.02 | −0.25; 0.21 | 0.842 | - | - | - | - |
| Employment (professionally active vs. professionally inactive) | 0.24 | 0.03; 0.46 | 0.029 | - | - | - | - |
| Financial situation (worse than good vs. good) | 0.13 | −0.13; 0.39 | 0.337 | - | - | - | - |
| Number of children in the family (3 or more vs. 1−2) | 0.17 | −0.08; 0.43 | 0.172 | - | - | - | - |
| Gender of child with cancer (female vs. male) | 0.11 | −0.11; 0.32 | 0.339 | - | - | - | - |
| Age of child with cancer (years; 11−17 vs. 1−10) | 0.31 | 0.08; 0.53 | 0.008 | - | - | - | - |
| Disease duration (longer vs. shorter than one year) | 0.08 | −0.14; 0.29 | 0.495 | - | - | - | - |
| Relapse (did not occur vs. occurred) | −0.54 | −0.78; 0.29 | <0.001 | −0.48 | −0.69; −0.26 | −0.27 | <0.001 |
| Subjectively perceived treatment prognosis (good vs. bad) | −0.21 | −0.47; 0.05 | 0.106 | - | - | - | - |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Banienė, I.; Žemaitienė, N. Post-Traumatic Stress Symptoms among Lithuanian Parents Raising Children with Cancer. Children 2020, 7, 116. https://doi.org/10.3390/children7090116
Banienė I, Žemaitienė N. Post-Traumatic Stress Symptoms among Lithuanian Parents Raising Children with Cancer. Children. 2020; 7(9):116. https://doi.org/10.3390/children7090116
Chicago/Turabian StyleBanienė, Irina, and Nida Žemaitienė. 2020. "Post-Traumatic Stress Symptoms among Lithuanian Parents Raising Children with Cancer" Children 7, no. 9: 116. https://doi.org/10.3390/children7090116




