Cementless Ceramic-on-Ceramic Total Hip Replacement in Children and Adolescents
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Patients Evaluation
2.3. Statistical Analysis
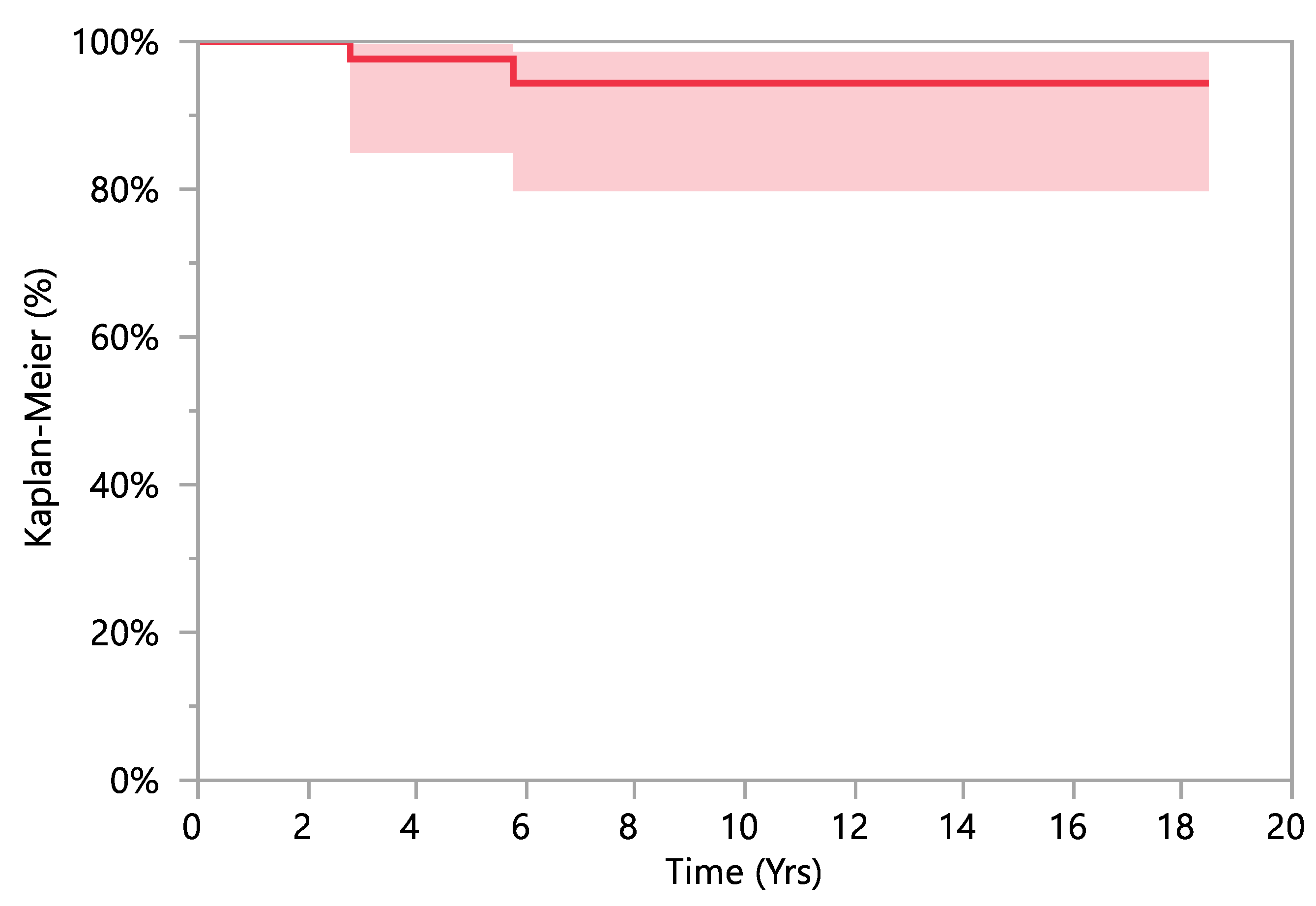
3. Results
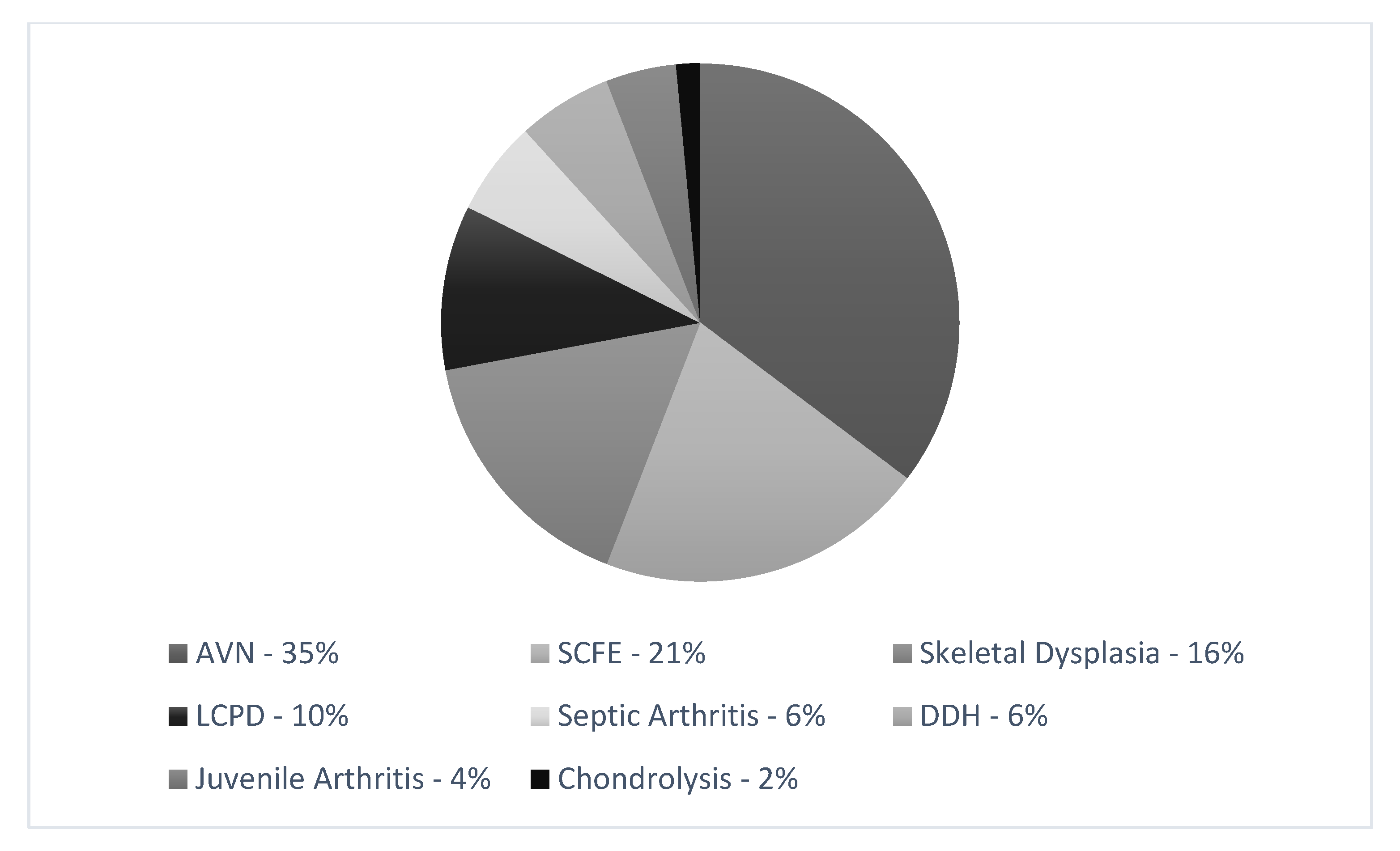
3.1. Patients’ Population
3.2. Surgical Data
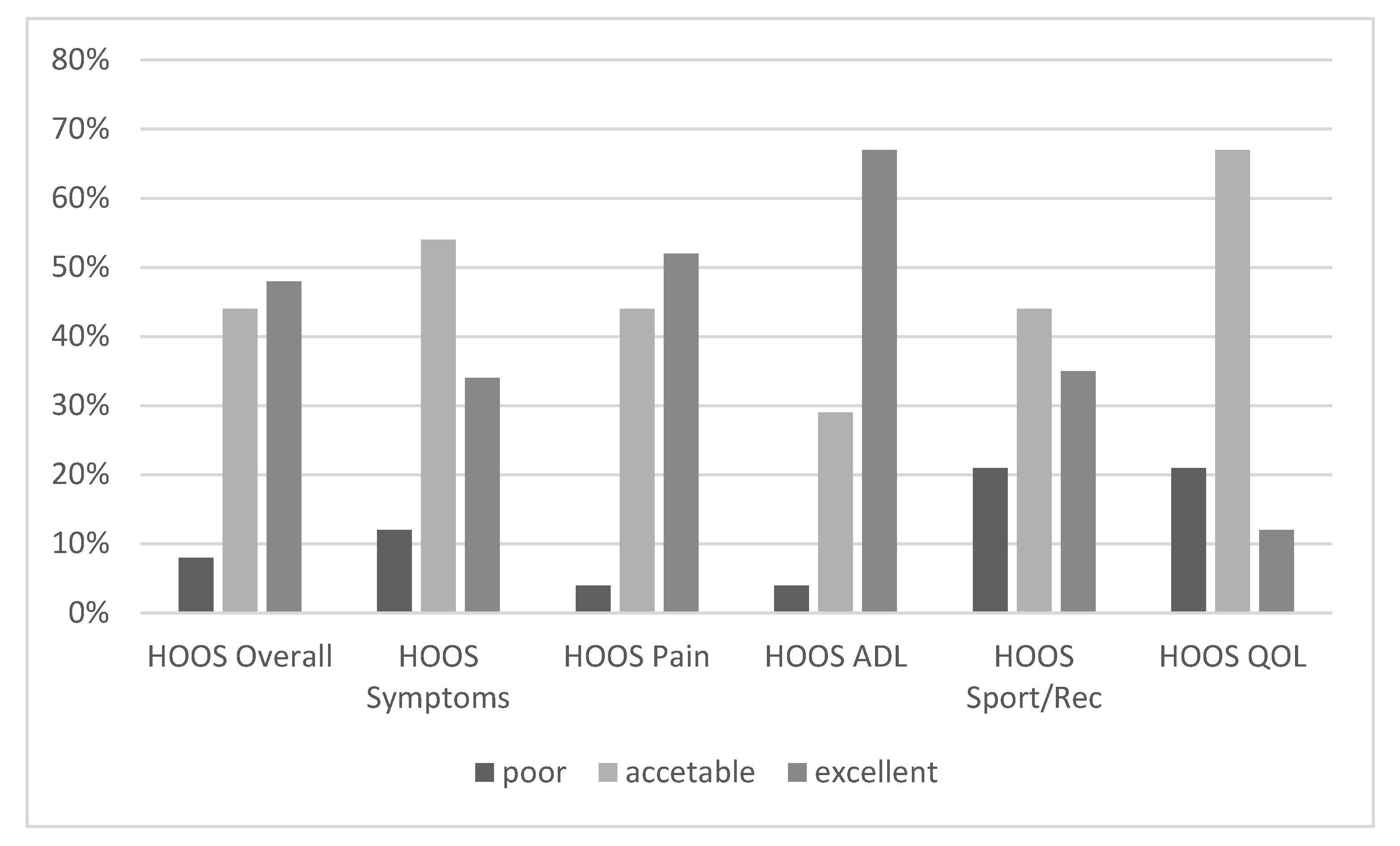
3.3. Clinical Evaluation
3.4. Radiographic Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zucker, E.J.; Lee, E.Y.; Restrepo, R.; Eisenberg, R.L. Hip disorders in children. Am. J. Roentgenol. 2013, 201, W776–W796. [Google Scholar] [CrossRef]
- Novais, E.N. Treatment options for end-stage hip disease in adolescents: To replace, fuse, or reconstruct? J. Pediatric Orthop. 2021, 41 (Suppl. 1), S47–S52. [Google Scholar] [CrossRef]
- Millis, M.B. Prearthritic hip disease: Important issues. JBJS 2020, 102 (Suppl. 2), 3–7. [Google Scholar] [CrossRef]
- Steppacher, S.D.; Huemmer, C.; Schwab, J.M.; Tannast, M.; Siebenrock, K.A. Surgical hip dislocation for treatment of femoroacetabular impingement: Factors predicting 5-year survivorship. Clin. Orthop. Relat. Res. 2014, 472, 337–348. [Google Scholar] [CrossRef] [Green Version]
- Lachiewicz, P.F.; McCaskill, B.; Inglis, A.; Ranawat, C.S.; Rosentein, B.D. Total hip arthroplasty in juvenile rheumatoid arthritis. Two to eleven-year results. J. Bone Jt. Surg. Am. 1986, 68, 502–508. [Google Scholar] [CrossRef]
- Witt, J.D.; Swann, M.; Ansell, B.M. Total hip replacement for juvenile chronic arthritis. J. Bone Jt. Surgery. Br. Vol. 1991, 73, 770–773. [Google Scholar] [CrossRef] [PubMed]
- Torchia, M.E.; Klassen, R.A.; Bianco, A.J. Total hip arthroplasty with cement in patients less than twenty years old: Long-term results. JBJS 1996, 78, 995–1003. [Google Scholar] [CrossRef] [PubMed]
- Nizard, R.; Pourreyron, D.; Raould, A.; Hannouche, D.; Sedel, L. Alumina-on-alumina hip arthroplasty in patients younger than 30 years old. Clin. Orthop. Relat. Res. 2008, 466, 317–323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sedrakyan, A.; Romero, L.; Graves, S.; Davidson, D.; De Steiger, R.; Lewis, P.; Solomon, M.; Vial, R.; Lorimer, M. Survivorship of hip and knee implants in pediatric and young adult populations: Analysis of registry and published data. JBJS 2014, 96 (Suppl. 1), 73–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Halvorsen, V.; Fenstad, A.M.; Engesæter, L.B.; Nordsletten, L.; Overgaard, S.; Pedersen, A.B.; Kärrholm, J.; Mohaddes, M.; Eskelinen, A.; Mäkelä, K.T.; et al. Outcome of 881 total hip arthroplasties in 747 patients 21 years or younger: Data from the Nordic Arthroplasty Register Association (NARA) 1995–2016. Acta Orthop. 2019, 90, 331–337. [Google Scholar] [CrossRef] [Green Version]
- Finkbone, P.R.; Severson, E.P.; Cabanela, M.E.; Trousdale, R.T. Ceramic-on-ceramic total hip arthroplasty in patients younger than 20 years. J. Arthroplast. 2012, 27, 213–219. [Google Scholar] [CrossRef]
- Van De Velde, S.K.; Loh, B.; Donnan, L. Total hip arthroplasty in patients 16 years of age or younger. J. Child. Orthop. 2017, 11, 428–433. [Google Scholar] [CrossRef]
- Clohisy, J.C.; Oryhon, J.M.; Seyler, T.M.; Wells, C.W.; Liu, S.S.; Callaghan, J.J.; Mont, M.A. Function and fixation of total hip arthroplasty in patients 25 years of age or younger. Clin. Orthop. Relat. Res. 2010, 468, 3207–3213. [Google Scholar] [CrossRef] [Green Version]
- Hsu, J.E.; Kinsella, S.D.; Garino, J.P.; Lee, G.C. Ten-year follow-up of patients younger than 50 years with modern ceramic-on-ceramic total hip arthroplasty. Semin. Arthroplast. JSES 2011, 22, 229–233. [Google Scholar] [CrossRef]
- Castagnini, F.; Bordini, B.; Stea, S.; Calderoni, P.P.; Masetti, C.; Busanelli, L. Highly porous titanium cup in cementless total hip arthroplasty: Registry results at eight years. Int. Orthop. 2019, 43, 1815–1821. [Google Scholar] [CrossRef]
- Varnum, C. Outcomes of different bearings in total hip arthroplasty—Implant survival, revision causes, and patient-reported outcome. Dan Med. J. 2017, 64, B5350. [Google Scholar] [PubMed]
- Pallante, G.D.; Statz, J.M.; Milbrandt, T.A.; Trousdale, R.T. Primary total hip arthroplasty in patients 20 years old and younger. JBJS 2020, 102, 519–525. [Google Scholar] [CrossRef] [PubMed]
- Cacciari, E.; Milani, S.; Balsamo, A.; Spada, E.; Bona, G.; Cavallo, L.; Cerutti, F.; Gargantini, L.; Greggio, N.; Tonini, G.; et al. Italian cross-sectional growth charts for height, weight and BMI (2 to 20 Yr). J. Endocrinol. Investig. 2006, 29, 581–593. [Google Scholar] [CrossRef]
- Torre, M.; Luzi, I.; Mirabella, F.; Del Manso, M.; Zanoli, G.; Tucci, G.; Romanini, E. Cross-cultural adaptation and validation of the italian version of the Hip disability and Osteoarthritis Outcome Score (HOOS). Health Qual. Life Outcomes 2018, 16, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Calistri, A.; Di Martino, L.; Gurzì, M.D.; Bove, M.; De Smet, K.; Villani, C. Italian version of University of California at Los Angeles (UCLA) Activity Score: Cross-cultural adaptation. J. Arthroplast. 2014, 29, 1733–1735. [Google Scholar] [CrossRef]
- Scalone, L.; Cortesi, P.A.; Ciampichini, R.; Belisari, A.; D’Angiolella, L.S.; Cesana, G.; Mantovani, L.G. Italian population-based values of EQ-5D health states. Value Health 2013, 16, 814–822. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sundén, A.; Lidengren, K.; Roos, E.M.; Lohmander, L.S.; Ekvall Hansson, E. Hip complaints differ across age and sex: A population-based reference data for the Hip disability and Osteoarthritis Outcome Score (HOOS). Health Qual. Life Outcomes 2018, 16, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Tannast, M.; Siebenrock, K.A.; Anderson, S.E. Femoroacetabular impingement: Radiographic diagnosis—What the radiologist should know. Am. J. Roentgenol. 2007, 188, 1540–1552. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lucchini, S.; Castagnini, F.; Giardina, F.; Tentoni, F.; Masetti, C.; Tassinari, E.; Bordini, B.; Traina, F. Cementless ceramic-on-ceramic total hip arthroplasty in post-traumatic osteoarthritis after acetabular fracture: Long-term results. Arch. Orthop. Trauma Surg. 2021, 141, 683–691. [Google Scholar] [CrossRef]
- Engesæter, I.Ø.; Laborie, L.B.; Lehmann, T.G.; Sera, F.; Fevang, J.; Pedersen, D.; Morcuende, J.; Lie, S.A.; Engesæter, L.B.; Rosendahl, K. Radiological findings for hip dysplasia at skeletal maturity. Validation of digital and manual measurement techniques. Skeletal Radiol. 2012, 41, 775–785. [Google Scholar] [CrossRef] [PubMed]
- Troy, M.J.; Miller, P.E.; Price, N.; Talwalkar, V.; Zaina, F.; Donzelli, S.; Negrini, S.; Hresko, M.T. The “Risser+” grade: A new grading system to classify skeletal maturity in idiopathic scoliosis. Eur. Spine J. 2019, 28, 559–566. [Google Scholar] [CrossRef]
- Lewinnek, G.E.; Lewis, J.L.; Tarr, R.; Compere, C.L.; Zimmerman, J.R. Dislocations after total hip-replacement arthroplasties. J. Bone Jt. Surg. 1978, 60, 217–220. [Google Scholar] [CrossRef]
- Min, B.W.; Song, K.S.; Bae, K.C.; Cho, C.H.; Kang, C.H.; Kim, S.Y. The effect of stem alignment on results of total hip arthroplasty with a cementless tapered-wedge femoral component. J. Arthroplast. 2008, 23, 418–423. [Google Scholar] [CrossRef]
- O’Brien, S.; Kernohan, G.; Fitzpatrick, C.; Hill, J.; Beverland, D. Perception of imposed leg length inequality in normal subjects. Hip Int. 2010, 20, 505–511. [Google Scholar] [CrossRef]
- Matsuda, K.; Nakamura, S.; Matsushita, T. A simple method to minimize limb-length discrepancy after hip arthroplasty. Acta Orthop. 2006, 77, 375–379. [Google Scholar] [CrossRef]
- D’Ambrosio, A.; Peduzzi, L.; Roche, O.; Bothorel, H.; Saffarini, M.; Bonnomet, F. Influence of femoral morphology and canal fill ratio on early radiological and clinical outcomes of uncemented total hip arthroplasty using a fully coated stem. Bone Jt. Res. 2020, 9, 182–191. [Google Scholar] [CrossRef] [PubMed]
- Engh, C.A.; Massin, P.; Suthers, K.E. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin. Orthop. Relat. Res. 1990, 257, 107–128. [Google Scholar] [CrossRef]
- Moore, M.S.; McAuley, J.P.; Young, A.M.; Engh, C.A. Radiographic signs of osseointegration in porous-coated acetabular components. Clin. Orthop. Relat. Res. 2006, 444, 176–183. [Google Scholar] [CrossRef]
- Brooker, A.F.; Bowerman, J.W.; Robinson, R.A.; Riley, L.H., Jr. Ectopic ossification following total hip replacement. incidence and a method of classification. J. Bone Jt. Surg. Am. 1973, 55, 1629–1632. [Google Scholar] [CrossRef]
- Boyer, B.; Bordini, B.; Caputo, D.; Neri, T.; Stea, S.; Toni, A. What are the influencing factors on hip and knee arthroplasty survival? Prospective cohort study on 63,619 arthroplasties. Orthop. Traumatol. Surg. Res. 2019, 105, 1251–1256. [Google Scholar] [CrossRef] [PubMed]
- Metcalfe, D.; Peterson, N.; Wilkinson, J.M.; Perry, D.C. Temporal trends and survivorship of total hip arthroplasty in very young patients: A study using the National Joint Registry data set. Bone Jt. J. 2018, 100, 1320–1329. [Google Scholar] [CrossRef] [PubMed]
- Buddhdev, P.K.; Vanhegan, I.S.; Khan, T.; Hashemi-Nejad, A. Early to medium-term outcomes of uncemented ceramic-bearing total hip arthroplasty in teenagers for paediatric hip conditions. Bone Jt. J. 2020, 102, 1491–1496. [Google Scholar] [CrossRef]
- Vendittoli, P.A.; Shahin, M.; Rivière, C.; Barry, J.; Lavoie, P.; Duval, N. Ceramic-on-ceramic total hip arthroplasty is superior to metal-on-conventional polyethylene at 20-year follow-up: A randomised clinical trial. Orthop. Traumatol. Surg. Res. 2021, 107, 102744. [Google Scholar] [CrossRef]
- Castagnini, F.; Bordini, B.; Biondi, F.; Cosentino, M.; Stea, S.; Traina, F. Mixed ceramic combinations in primary total hip arthroplasty achieved reassuring mid-to-longterm outcomes. J. Mater. Sci. Mater. Med. 2020, 31, 1–6. [Google Scholar] [CrossRef]
- Viceconti, M.; Lattanzi, R.; Antonietti, B.; Paderni, S.; Olmi, R.; Sudanese, A.; Toni, A. CT-based surgical planning software improves the accuracy of total hip replacement preoperative planning. Med. Eng. Phys. 2003, 25, 371–377. [Google Scholar] [CrossRef]
- Noble, P.C.; Sugano, N.; Johnston, J.D.; Thompson, M.T.; Conditt, M.A.; Engh, C.A.; Mathis, K.B. Computer simulation: How can it help the surgeon optimize implant position? Clin. Orthop. Relat. Res. 2003, 417, 242–252. [Google Scholar] [CrossRef]
- Frizziero, L.; Santi, G.M.; Liverani, A.; Napolitano, F.; Papaleo, P.; Maredi, E.; Di Gennaro, G.L.; Zarantonello, P.; Stallone, S.; Stilli, S.; et al. Computer-aided surgical simulation for correcting complex limb deformities in children. Appl. Sci. 2020, 10, 5181. [Google Scholar] [CrossRef]

| Radiographic Value | Description | Normal Value | Image |
|---|---|---|---|
| PREOPERATIVE | |||
| Lateral center-edge angle (lcea) | The angle measured between two lines drawn from the center of the best fit circle for the inferior and medial margins femoral head, one running vertically along the longitudinal axis of the pelvis and the other to the lateral acetabular rim [23,24] | 25–39° |  |
| Acetabular index | The angle described between the line running through the medial edge of the sclerotic acetabular zone and through the lateral sourcil, and its horizontal line | 3–13° |  |
| Acetabular depth/width ratio | The width is a line connecting the superolateral edge and the inferomedial edge of the acetabulum. The perpendicular line from the latter to the deepest part of acetabulum is the depth. The ADWR is the percentage of depth to the width [25] | >38% |  |
| Sharp angle | the angle between a line passing from the superior to the inferior acetabular rim and the horizontal plane | <42° |  |
| Neck-shaft angle | The angle between the longitudinal axes of the femoral neck and shaft | 130 ± 5° |  |
| Risser | Measured according to “Risser +” grade [26] | 0 to 5 | |
| POSTOPERATIVE | |||
| Cup abduction | The angle described between the interteardrop line and the tangent to the opening of the cup | 35–45° |  |
| Cup anteversion | measured according to the Lewinnek’s [27] method | 5–25° |  |
| Center of rotation high | the perpendicular distance between the center or rotation and the interteradrop line |  | |
| Center of rotation medialization | the perpendicular distance between the center of rotation and a line perpendicular to the interteardrop line and tangent to the medial border of the teardrop | 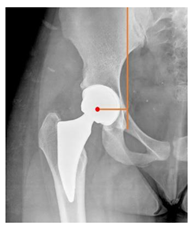 | |
| Stem varus-valgus | the angle between the axis of the femur and the main axis of the stem [28] +/−: the stem is valgus/varus | −5–+5° |  |
| Leg length discrepancy | Trochanteric method: the difference between the distances from the tip of the lesser trochanter to the interteardrop line, measured in both the hips [29] +/−: the treated hip was longer/shorter | 0 ± 10 mm | 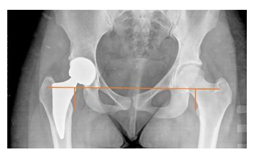 |
| Femoral offset | the perpendicular distance between the center of rotation and the axis of femoral shaft [30] | 41–44 mm | 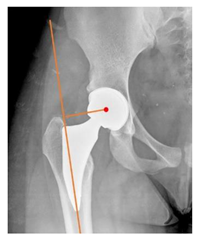 |
| Canal fill ratio | The ratio between the width of the femoral component by the width of the intramedullary bone canal at 1 cm below the lesser trochanter [31] | ||
| Stem osteointegration | Measured according to Engh [32] grading scale | ||
| Acetabular osteointegration | Measured according to Moore [33] scale | ||
| Heterotopic ossification | Classified according to Brooker [34] classification |
| PATIENTS BASELINE VARIABLES | |
|---|---|
| Patients (Male/Female) | 68 (33/35) |
| Hips (Left/Right) | 74 (44/30) |
| Mean Age at THR (years) | 15.7 ± 1.7 (11–18) |
| Weight (Kg) | 62.3 ± 14.9 (33–116) |
| Weight (z-score) | 0.52 ± 0.34 (0–1) |
| Height (cm) | 164.8 ± 10.8 (145–195) |
| Height (z-score) | 0.44 ± 0.34 (0–1) |
| BMI (cm2/Kg) | 22.8 ± 4.1 (14.7–33.3) |
| BMI (z-score) | 0.63 ± 0.32 (0–1) |
| Follow-up (years) | 6.6 ± 4.4 (2–20) |
| N | % | |
|---|---|---|
| Acetabular cup’s size | ||
| 42 | 12 | 16.2 |
| 44 | 6 | 8.1 |
| 46 | 16 | 21.6 |
| 48 | 13 | 17.6 |
| 50 | 11 | 14.9 |
| 52 | 6 | 8.1 |
| 54 | 5 | 6.8 |
| 56 | 1 | 1.4 |
| 58 | 4 | 5.4 |
| Cup’s commercial name | ||
| Fixa Ti-por® (Adler) | 44 | 59.5 |
| EP-FIT PLUS™ (Smih & Nephew) | 7 | 9.5 |
| ALLOFIT®-S IT (Zimmer) | 6 | 8.1 |
| Other (less than 5 implanted) | 17 | 23.0 |
| Stem’s commercial name | ||
| APTA (Adler-Ortho) | 13 | 17.6 |
| NANOS™ (Endoplant GmbH) | 11 | 14.9 |
| A-ACUTA S (Adler-Ortho) | 7 | 9.5 |
| Other (less than 5 implanted) | 43 | 58.1 |
| Head material | ||
| Biolox® or Biolox®Forte | 14 | 18.9 |
| BIOLOX®delta | 60 | 81.1 |
| Head size | ||
| 28 | 6 | 8.1 |
| 32 | 48 | 64.9 |
| 36 | 14 | 18.9 |
| 40 | 6 | 8.1 |
| Neck | ||
| Modular | 27 | 36.5 |
| Nonmodular | 47 | 63.5 |
| PREOPERATIVE Radiographic Parameters | |
|---|---|
| LCEA | 41.6 ± 1.1 (3–110.4) |
| Acetabular Index | 9.1 ± 21.5 (−23.8–41) |
| Acetabular depth/width ratio | 29.5 ± 10 (3.9–63.7) |
| Sharp Angle | 39.2 ± 5.5 (20.1–51.2) |
| Neck-Shaft angle | 135 ± 9.5 (103–157) |
| Risser+ (0–0+–1–2–3–4–5) | 0%–0%–8%–2%–12%–46%–23% |
| POSTOPERATIVE Radiographic Parameters | |
| Cup Abduction | 37.3 ± 8.8 (18.5–62.7) |
| Cup Anteversion | 11.9 ± 5.7 (0–26) |
| Center of Rotation high | 20.8 ± 5 (7.7–35.4) |
| Center of Rotation medialization | 29.7 ± 4 (19.5–40.4) |
| Stem varus-valgus * | −1.2 ± 3.1 (−11–7.7) |
| Leg length discrepancy | −1.6 ± 7.9 (−27.9–16.3) |
| Femoral offset | 39.2 ± 7.1 (27.6–53.2) |
| Canal Fill Ratio | 75 ± 9.8% (50–95%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trisolino, G.; Stallone, S.; Castagnini, F.; Bordini, B.; Cosentino, M.; Lucchini, S.; Zarantonello, P.; Ferrari, D.; Dallari, D.; Traina, F. Cementless Ceramic-on-Ceramic Total Hip Replacement in Children and Adolescents. Children 2021, 8, 858. https://doi.org/10.3390/children8100858
Trisolino G, Stallone S, Castagnini F, Bordini B, Cosentino M, Lucchini S, Zarantonello P, Ferrari D, Dallari D, Traina F. Cementless Ceramic-on-Ceramic Total Hip Replacement in Children and Adolescents. Children. 2021; 8(10):858. https://doi.org/10.3390/children8100858
Chicago/Turabian StyleTrisolino, Giovanni, Stefano Stallone, Francesco Castagnini, Barbara Bordini, Monica Cosentino, Stefano Lucchini, Paola Zarantonello, Daniele Ferrari, Dante Dallari, and Francesco Traina. 2021. "Cementless Ceramic-on-Ceramic Total Hip Replacement in Children and Adolescents" Children 8, no. 10: 858. https://doi.org/10.3390/children8100858
APA StyleTrisolino, G., Stallone, S., Castagnini, F., Bordini, B., Cosentino, M., Lucchini, S., Zarantonello, P., Ferrari, D., Dallari, D., & Traina, F. (2021). Cementless Ceramic-on-Ceramic Total Hip Replacement in Children and Adolescents. Children, 8(10), 858. https://doi.org/10.3390/children8100858








