Skin Disease in Children: Effects on Quality of Life, Stigmatization, Bullying, and Suicide Risk in Pediatric Acne, Atopic Dermatitis, and Psoriasis Patients
Abstract
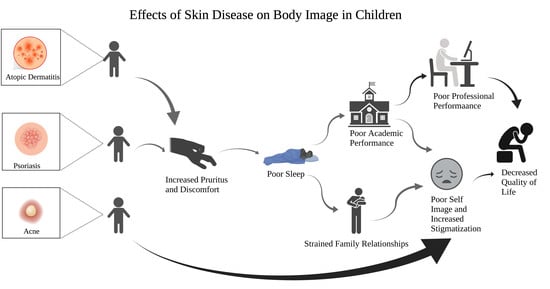
:1. Introduction
2. Materials and Methods
3. Results
3.1. Acne
3.1.1. Effect on Quality of Life
3.1.2. Impact of Bullying
3.1.3. Risk of Suicide
3.2. Atopic Dermatitis
3.2.1. Effect on Quality of Life
3.2.2. Impact of Bullying
3.2.3. Risk of Suicide
3.3. Psoriasis
3.3.1. Impact on Quality of Life
3.3.2. Impact of Bullying
3.3.3. Risk of Suicide
4. Discussion
4.1. Management Options
4.1.1. Resources for Families
4.1.2. Resources for Teachers
4.1.3. Physician-Mediated Interventions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Vilar, G.N.; Dos Santos, L.A.; Filho, J.F.S. Quality of life, self-esteem and psychosocial factors in adolescents with acne vulgaris. An. Bras. Dermatol. 2015, 90, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Silverberg, N.B.; Durán-McKinster, C. Special Considerations for Therapy of Pediatric Atopic Dermatitis. Dermatol. Clin. 2017, 35, 351–363. [Google Scholar] [CrossRef]
- Lin, V.W. Tough-Skinned Kids: Identifying Psychosocial Effects of Psoriasis and Helping Pediatric Patients and Families Cope. J. Pediatr. Nurs. 2012, 27, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Picardi, A.; Lega, I.; Tarolla, E. Suicide risk in skin disorders. Clin. Dermatol. 2013, 31, 47–56. [Google Scholar] [CrossRef]
- Patrick, N.L.; Topolski, T.D.; Edwards, T.C.; Aspinall, C.L.; Kapp-Simon, K.A.; Rumsey, N.J.; Strauss, R.P.; Thomas, C.R. Measuring the Quality of Life of Youth with Facial Differences. Cleft Palate-Craniofacial J. 2007, 44, 538–547. [Google Scholar] [CrossRef]
- Strauss, R.P.; Ramsey, B.L.; Edwards, T.C.; Topolski, T.D.; Kapp-Simon, K.A.; Thomas, C.R.; Fenson, C.; Patrick, D.L. Stigma experiences in youth with facial differences: A multi-site study of adolescents and their mothers. Orthod. Craniofacial Res. 2007, 10, 96–103. [Google Scholar] [CrossRef]
- Tasoula, E.; Gregoriou, S.; Chalikias, J.; Lazarou, D.; Danopoulou, I.; Katsambas, A.; Rigopoulos, D. The impact of acne vulgaris on quality of life and psychic health in young adolescents in Greece: Results of a population survey. An. Bras. Dermatol. 2012, 87, 862–869. [Google Scholar] [CrossRef] [PubMed]
- Gupta, A.K. Depression and suicidal ideation in dermatology patients with acne, alopecia areata, atopic dermatitis and psoriasis. Br. J. Dermatol. 1998, 139, 846–850. [Google Scholar] [CrossRef]
- Krowchuk, D.P.; Stancin, T.; Keskinen, R.; Walker, R.; Bass, J.; Anglin, T.M. The Psychosocial Effects of Acne on Adolescents. Pediatr. Dermatol. 1991, 8, 332–338. [Google Scholar] [CrossRef]
- Magin, P.; Adams, J.; Heading, G.; Pond, D.; Smith, W. Experiences of appearance-related teasing and bullying in skin diseases and their psychological sequelae: Results of a qualitative study. Scand. J. Caring Sci. 2008, 22, 430–436. [Google Scholar] [CrossRef]
- Ritvo, E.; Del Rosso, J.Q.; Stillman, M.A.; La Riche, C. Psychosocial judgements and perceptions of adolescents with acne vulgaris: A blinded, controlled comparison of adult and peer evaluations. Biopsychosoc. Med. 2011, 5, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, M.Z.; Naeem, A.; Mufti, K.A. Prevalence of mental health problems in acne patients. J. Ayub Med. Coll. Abbottabad JAMC 2002, 13. [Google Scholar]
- Purvis, D.; Robinson, E.; Merry, S.; Watson, P. Acne, anxiety, depression and suicide in teenagers: A cross-sectional survey of New Zealand secondary school students. J. Paediatr. Child Health 2006, 42, 793–796. [Google Scholar] [CrossRef]
- Halvorsen, J.A.; Stern, R.S.; Dalgard, F.; Thoresen, M.; Bjertness, E.; Lien, L. Suicidal Ideation, Mental Health Problems, and Social Impairment Are Increased in Adolescents with Acne: A Population-Based Study. J. Investig. Dermatol. 2011, 131, 363–370. [Google Scholar] [CrossRef] [Green Version]
- Erdoğan, Y.; Erturan, I.; Aktepe, E.; Akyıldız, A. Comparison of Quality of Life, Depression, Anxiety, Suicide, Social Anxiety and Obsessive–Compulsive Symptoms Between Adolescents with Acne Receiving Isotretinoin and Antibiotics: A Prospective, Non-randomised, Open-Label Study. Pediatr. Drugs 2019, 21, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Chernyshov, P. Stigmatization and self-perception in children with atopic dermatitis. Clin. Cosmet. Investig. Dermatol. 2016, ume 9, 159–166. [Google Scholar] [CrossRef] [Green Version]
- Pauli-Pott, U.; Darui, A.; Beckmann, D. Infants with atopic dermatitis: Maternal hopelessness, child-rearing attitudes and perceived infant temperament. Psychother. Psychosom. 1999, 68, 39–45. [Google Scholar] [CrossRef]
- Lawson, V.; Lewis-Jones, M.S.; Finlay, A.Y.; Reid, P.; Owens, R.G. The family impact of childhood atopic dermatitis: The Dermatitis Family Impact questionnaire. Br. J. Dermatol. 1998, 138, 107–113. [Google Scholar] [CrossRef]
- Nguyen, C.M.; Koo, J.; Cordoro, K.M. Psychodermatologic Effects of Atopic Dermatitis and Acne: A Review on Self-Esteem and Identity. Pediatr. Dermatol. 2016, 33, 129–135. [Google Scholar] [CrossRef]
- Xie, Q.; Chan, C.; Chan, C.H. The wounded self—lonely in a crowd: A qualitative study of the voices of children living with atopic dermatitis in Hong Kong. Health Soc. Care Community 2019, 28, 862–873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Machado, A.C.C.D.P.; de Oliveria, S.U.; Magalhães, L.C.; de Miranda, D.M.; Bouzada, M.C.F. Sensory processing during childhood in preterm infants: A Systematic review. Rev. Paul. Pediatr. 2017, 35, 92–101. [Google Scholar] [CrossRef]
- Kim, J.P.; Chao, L.X.; Simpson, E.L.; Silverberg, J.I. Persistence of atopic dermatitis (AD): A systematic review and meta-analysis. J. Am. Acad. Dermatol. 2016, 75, 681–687.e11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brenninkmeijer, E.E.; Legierse, C.M.; Sillevis Smitt, J.H.; Last, B.F.; Grootenhuis, M.A.; Bos, J.D. The Course of Life of Patients with Childhood Atopic Dermatitis. Pediatr. Dermatol. 2009, 26, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Eckert, L.; Gupta, S.; Amand, C.; Gadkari, A.; Mahajan, P.; Gelfand, J. Impact of atopic dermatitis on health-related quality of life and productivity in adults in the United States: An analysis using the National Health and Wellness Survey. J. Am. Acad. Dermatol. 2017, 77, 274–279.e3. [Google Scholar] [CrossRef] [Green Version]
- Roberts, R.M.; Gierasch, A. The effect of visible facial difference on personal space during encounters with the general public. Plastic Surgical Nurs. 2013, 33, 71–80. [Google Scholar] [CrossRef] [Green Version]
- Sandhu, J.K.; Wu, K.K.; Bui, T.-L.; Armstrong, A.W. Association Between Atopic Dermatitis and Suicidality. JAMA Dermatol. 2019, 155, 178–187. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Shin, A. Association of atopic dermatitis with depressive symptoms and suicidal behaviors among adolescents in Korea: The 2013 Korean Youth Risk Behavior Survey. BMC Psychiatry 2017, 17, 3. [Google Scholar] [CrossRef] [Green Version]
- Kyung, Y.; Choi, M.H.; Jeon, Y.J.; Lee, J.S.; Lee, J.H.; Jo, S.H.; Kim, S.H. Association of atopic dermatitis with suicide risk among 788,411 adolescents. Ann. Allergy Asthma Immunol. 2020, 125, 55–64. [Google Scholar] [CrossRef]
- Noh, H.-M.; Cho, J.J.; Park, Y.S.; Kim, J.-H. The relationship between suicidal behaviors and atopic dermatitis in Korean adolescents. J. Heal. Psychol. 2015, 21, 2183–2194. [Google Scholar] [CrossRef]
- Leung, D.Y.; Berdyshev, E.; Goleva, E. Association of atopic dermatitis and suicide: More than a coincidence? Ann. Allergy, Asthma Immunol. 2020, 125, 4–5. [Google Scholar] [CrossRef] [PubMed]
- Lindqvist, D.; Janelidze, S.; Hagell, P.; Erhardt, S.; Samuelsson, M.; Minthon, L.; Hansson, O.; Bjorkqvist, M.; Träskman-Bendz, L.; Brundin, L. Interleukin-6 Is Elevated in the Cerebrospinal Fluid of Suicide Attempters and Related to Symptom Severity. Biol. Psychiatry 2009, 66, 287–292. [Google Scholar] [CrossRef]
- Simpson, E.L.; Bieber, T.; Guttman-Yassky, E.; Beck, L.A.; Blauvelt, A.; Cork, M.; Silverberg, J.I.; Deleuran, M.; Kataoka, Y.; Lacour, J.-P.; et al. Two Phase 3 Trials of Dupilumab versus Placebo in Atopic Dermatitis. N. Engl. J. Med. 2016, 375, 2335–2348. [Google Scholar] [CrossRef]
- Buske-Kirschbaum, A.; Geiben, A.; Hoöllig, H.; Morschhaäuser, E.; Hellhammer, D. Altered Responsiveness of the Hypothalamus-Pituitary-Adrenal Axis and the Sympathetic Adrenomedullary System to Stress in Patients with Atopic Dermatitis. J. Clin. Endocrinol. Metab. 2002, 87, 4245–4251. [Google Scholar] [CrossRef]
- Turnbull, A.V.; Rivier, C.L. Regulation of the Hypothalamic-Pituitary-Adrenal Axis by Cytokines: Actions and Mechanisms of Action. Physiol. Rev. 1999, 79, 1–71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonzalez, J.; Cunningham, K.; Perlmutter, J.; Gottlieb, A. Systematic Review of Health-Related Quality of Life in Adolescents with Psoriasis. Dermatology 2016, 232, 541–549. [Google Scholar] [CrossRef] [PubMed]
- Golics, C.; Basra, M.; Finlay, A.Y.; Salek, M. Adolescents with Skin Disease Have Specific Quality of Life Issues. Dermatology 2009, 218, 357–366. [Google Scholar] [CrossRef] [PubMed]
- Tekin, B.; Gurel, M.S.; Topkarci, Z.; Demir, F.T.; Aytekin, S.; Kahraman, F.C.; Singer, R.; Erdemir, V.A.; Uzuncakmak, T.K.; Yasar, S.; et al. Assessment of quality of life in Turkish children with psoriasis and their caregivers. Pediatr. Dermatol. 2018, 35, 651–659. [Google Scholar] [CrossRef]
- Basra, M.K.A.; Finlay, A.Y. The family impact of skin diseases: The Greater Patient concept. Br. J. Dermatol. 2007, 156, 929–937. [Google Scholar] [CrossRef]
- Nazik, H.; Nazik, S.; Gul, F.C. Body Image, Self-esteem, and Quality of Life in Patients with Psoriasis. Indian Dermatol. Online J. 2017, 8, 343–346. [Google Scholar] [CrossRef]
- Wojtyna, E.; Łakuta, P.; Marcinkiewicz, K.; Bergler-Czop, B.; Brzezińska-Wcisło, L. Gender, Body Image and Social Support: Biopsychosocial Determinants of Depression Among Patients with Psoriasis. Acta Derm. Venereol. 2017, 97, 91–97. [Google Scholar] [CrossRef] [Green Version]
- Jankowiak, B.; Kowalewska, B.; Krajewska-Kułak, E.; Khvorik, D.F.; Niczyporuk, W. Relationship between self-esteem and stigmatization in psoriasis patients. Adv. Dermatol. Allergol. 2020, 37, 597–602. [Google Scholar] [CrossRef]
- Lu, Y.; Duller, P.; Van Der Valk, P.; Evers, A. Helplessness as Predictor of Perceived Stigmatization in Patients with Psoriasis and Atopic Dermatitis. Dermatol. Psychosom./Dermatol. und Psychosom. 2003, 4, 146–150. [Google Scholar] [CrossRef]
- Alpsoy, E.; Polat, M.; Yavuz, I.H.; Kartal, P.; Balci, D.D.; Karadag, A.S.; Bilgic, A.; Arca, E.; Karaman, B.F.; Emre, S.; et al. Internalized Stigma in Pediatric Psoriasis: A Comparative Multicenter Study. Ann. Dermatol. 2020, 32, 181–188. [Google Scholar] [CrossRef]
- Koo, J.; Marangell, L.; Nakamura, M.; Armstrong, A.; Jeon, C.; Bhutani, T.; Wu, J. Depression and suicidality in psoriasis: Review of the literature including the cytokine theory of depression. J. Eur. Acad. Dermatol. Venereol. 2017, 31, 1999–2009. [Google Scholar] [CrossRef]
- Nicholas, M.N.; Gooderham, M. Psoriasis, Depression, and Suicidality. Skin Ther. Lett. 2017, 22, 1–4. [Google Scholar]
- Tohid, H.; Aleem, D.; Jackson, C. Major Depression and Psoriasis: A Psychodermatological Phenomenon. Ski. Pharmacol. Physiol. 2016, 29, 220–230. [Google Scholar] [CrossRef]
- Dixon, L.J.; Snorrason, Í. Prevalence and clinical characteristics of skin picking among adults with skin disease symptoms. J. Obsessive-Compulsive Relat. Disord. 2019, 22. [Google Scholar] [CrossRef]
- Odlaug, B.L.; Grant, J.E. Clinical characteristics and medical complications of pathologic skin picking. Gen. Hosp. Psychiatry 2008, 30, 61–66. [Google Scholar] [CrossRef] [PubMed]
- Oostveen, A.M.; Koulil, S.S.-V.; Otero, M.E.; Klompmaker, W.; Evers, A.W.; Seyger, M.M. Development and design of a multidisciplinary training program for outpatient children and adolescents with psoriasis and their parents. J. Dermatol. Treat. 2012, 24, 60–63. [Google Scholar] [CrossRef]
- Patel, N.U.; D’Ambra, V.; Feldman, S.R. Increasing Adherence with Topical Agents for Atopic Dermatitis. Am. J. Clin. Dermatol. 2017, 18, 323–332. [Google Scholar] [CrossRef]
- Bashyam, A.M.; Cuellar-Barboza, A.; Ghamrawi, R.I.; Feldman, S.R. Placebo tailoring improves patient satisfaction of treatment plans in atopic dermatitis. J. Am. Acad. Dermatol. 2020, 83, 944–946. [Google Scholar] [CrossRef]
- Olsen, J.; Gallacher, J.; Finlay, A.; Piguet, V.; Francis, N. Quality of life impact of childhood skin conditions measured using the Children’s Dermatology Life Quality Index (CDLQI): A meta-analysis. Br. J. Dermatol. 2016, 174, 853–861. [Google Scholar] [CrossRef] [Green Version]
- Hon, K.; Kam, W.; Lam, M.; Leung, T.; Ng, P. CDLQI, Scorad and Ness: Are they Correlated? Qual. Life Res. 2006, 15, 1551–1558. [Google Scholar] [CrossRef]
- Djurović, M.R.; Jankovic, J.; Cirkovic, A.; Spiric, V.T.; Maksimovic, N.; Timotijevic, Z.S.; Vukićević, D.; Mirkovic, Z.; Vitkovic, L.; Janković, S. Quality of life in infants with atopic dermatitis and their families. Adv. Dermatol. Allergol. 2020, 37, 66–72. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Infants’ Dermatitis Quality of Life Index-School of Medicine-Cardiff University. Available online: https://www.cardiff.ac.uk/medicine/resources/quality-of-life-questionnaires/infants-dermatitis-quality-of-life-index (accessed on 25 August 2021).
- Beattie, P.; Lewis-Jones, M. An audit of the impact of a consultation with a paediatric dermatology team on quality of life in infants with atopic eczema and their families: Further validation of the Infants’ Dermatitis Quality of Life Index and Dermatitis Family Impact score. Br. J. Dermatol. 2006, 155, 1249–1255. [Google Scholar] [CrossRef] [PubMed]
- Chamlin, S.L.; Lai, J.-S.; Cella, D.; Frieden, I.J.; Williams, M.L.; Mancini, A.J.; Chren, M.-M. Childhood Atopic Dermatitis Impact Scale. Arch. Dermatol. 2007, 143, 768–772. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chamlin, S.L.; Cella, D.; Frieden, I.J.; Williams, M.L.; Mancini, A.J.; Lai, J.-S.; Chren, M.-M. Development of the Childhood Atopic Dermatitis Impact Scale: Initial Validation of a Quality-of-Life Measure for Young Children with Atopic Dermatitis and their Families. J. Investig. Dermatol. 2005, 125, 1106–1111. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Name | Participants | Description | Scoring Algorithm | Severity Scoring | Advantages | Limitations |
|---|---|---|---|---|---|---|
| Children’s Dermatology Life Quality Index | Children aged 4–16 [52] | 10 questions in a 1-week recall period [53] Includes questions about symptoms, embarrassment, friendships, clothes, playing, sports, school, bullying, and impact of treatment [52] | 0–3 for each question 0: Not at all 1: Only a little 2: Quite a lot 3: Very Much [52] | 0–1: no effect 2–6: small effect 7–12: moderate effect 13–18: Very large effect 19–30: extremely large effect [52] | Measures QoL in children with other comorbid nonskin diseases Allows comparison between children with many different skin diseases [52] | Does not correlate well with acute and chronic AD severity scores, including SCORAD and total CDLQI [53] |
| Infant Dermatitis Quality of Life Index | Infants with AD less than 4 years of age [54] | 10 questions in a 1-week recall period [55] Includes questions about itching, mood, sleep, play, family, activities, mealtime, dressing, bathing, and problems from treatment of disease [54] Question for parents to assess disease severity [54] | Q1/5–10: 0: None 1: A little 2: A lot 3: All the time [55] Q2: 0: Happy 1: Slightly fretful 2: Very fretful 3: Always crying Q3: 0: 1–15 min 1: 15 min–1 h 2: 1–2 h 3: >2 h Q4: 0: < 1 h 1: 1–2 h 2: 3–4 h 3: >5 h | 0–30 The higher the score, the greater the impact on QoL Severity scored separately 4: Extremely severe 3: Severe 2: Average 1: Fairly good 0: None [55] | Easy and quick to administer in an outpatient setting 50 parents of infants with AD completed IDQoLIs before the 1st and 2nd dermatology consultations and demonstrated a decrease in median IDqoLI score from 8 to 5.5 [56] | Only assesses effects on QoL in patients with AD Only used as a short-term measurement |
| Dermatitis Family Impact | Caretakers of pediatric patients with AD [54] | 10 questions in a 1-week recall period Includes questions about housework, feeding, sleep, family activities, time spent on shopping, expenses related to treatment, fatigue, emotional distress, and family relationships [52] | 0–3 for each question. 0: Not at all [52] 1: Only a little 2: Quite a lot 3: Very Much | 0–30 The higher the score, the greater the impact on QoL [52] | Easy and quick to administer in an outpatient setting 50 parents of infants with AD completed DFIs before the 1st and 2nd dermatology consultations and demonstrated a decrease in the median DFI score from 9 to 3 [54] | Only assesses effects on QoL among family members of patients with AD Only used as a short-term measurement |
| Childhood Atopic Dermatitis Impact Scale | Children with AD younger than 6 years of age and their parents [57] | 45-item questionnaire in a 4-week recall period Includes 5 domains: child symptoms, child activity limitations and behavior, family and social function, parent sleep, and parent emotions [57] | 0–4 for each question Related to frequency from never to all the time [57] | Score of 0–180 The higher the score, the greater the impact on QoL [58] | Positive test–retest reliability, concurrent validity, discriminative validity, responsiveness evaluation Assesses QoL of both patients and caretakers [57] | Only pertains to patients and caregivers of those with AD Lack of a gold standard to use in comparison with global health questions [58] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kelly, K.A.; Balogh, E.A.; Kaplan, S.G.; Feldman, S.R. Skin Disease in Children: Effects on Quality of Life, Stigmatization, Bullying, and Suicide Risk in Pediatric Acne, Atopic Dermatitis, and Psoriasis Patients. Children 2021, 8, 1057. https://doi.org/10.3390/children8111057
Kelly KA, Balogh EA, Kaplan SG, Feldman SR. Skin Disease in Children: Effects on Quality of Life, Stigmatization, Bullying, and Suicide Risk in Pediatric Acne, Atopic Dermatitis, and Psoriasis Patients. Children. 2021; 8(11):1057. https://doi.org/10.3390/children8111057
Chicago/Turabian StyleKelly, Katherine A., Esther A. Balogh, Sebastian G. Kaplan, and Steven R. Feldman. 2021. "Skin Disease in Children: Effects on Quality of Life, Stigmatization, Bullying, and Suicide Risk in Pediatric Acne, Atopic Dermatitis, and Psoriasis Patients" Children 8, no. 11: 1057. https://doi.org/10.3390/children8111057
APA StyleKelly, K. A., Balogh, E. A., Kaplan, S. G., & Feldman, S. R. (2021). Skin Disease in Children: Effects on Quality of Life, Stigmatization, Bullying, and Suicide Risk in Pediatric Acne, Atopic Dermatitis, and Psoriasis Patients. Children, 8(11), 1057. https://doi.org/10.3390/children8111057