Evaluating the Use of Telepractice for Bottle-Feeding Assessments
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Evaluation Methodology
2.3. The Telepractice System
2.4. The Assessment Form
2.5. Telepractice Sessions
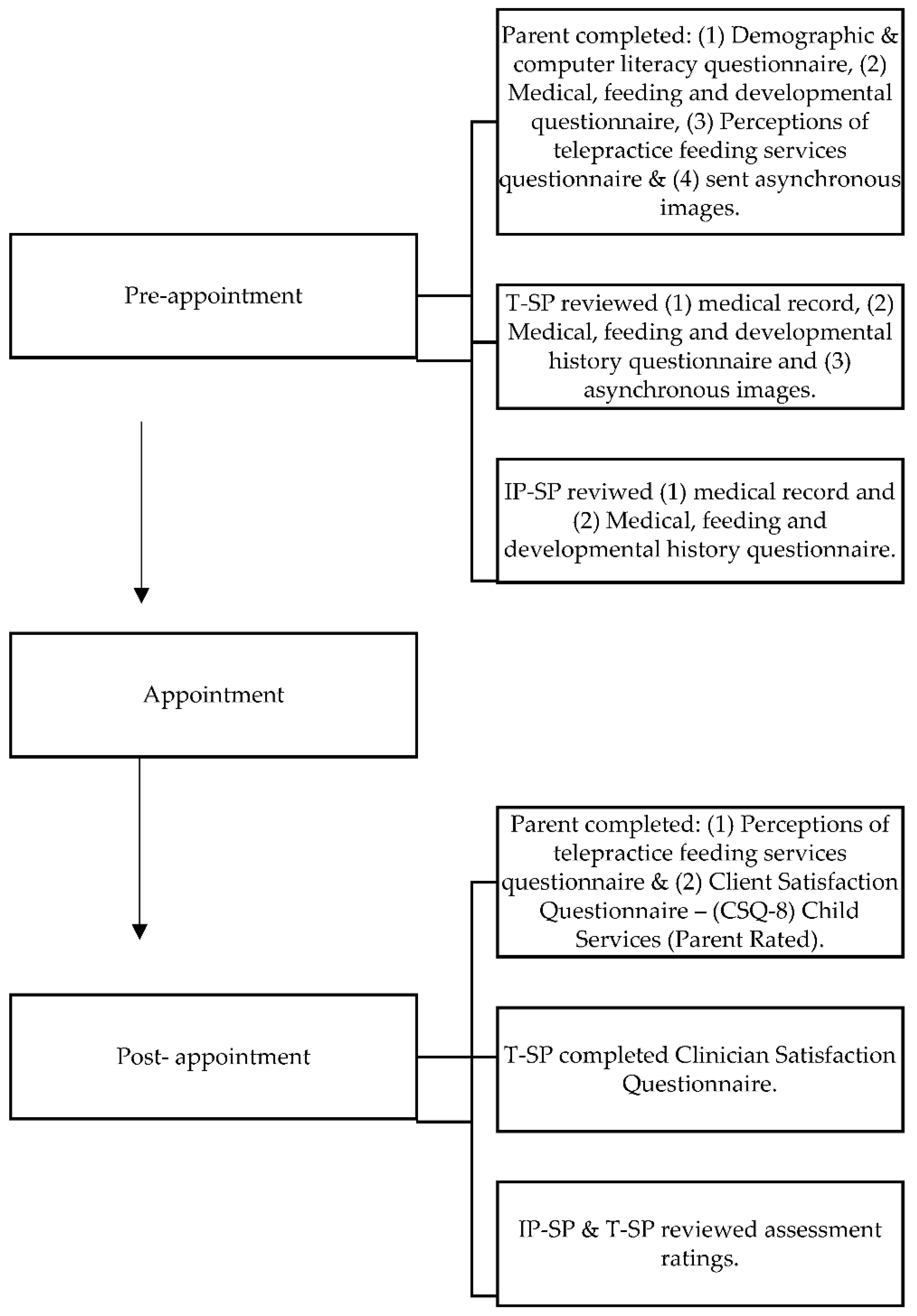
2.5.1. Pre-Appointment
2.5.2. Telepractice Appointment
2.5.3. Post-Session Feedback
2.6. Data Analysis
3. Results
3.1. Participants
3.1.1. Child Characteristics
3.1.2. Parent Demographic and Technology Information
3.2. Telepractice Sessions
3.2.1. Primary Aim: Inter-Rater Reliability
3.2.2. Secondary Aims: Clinician Satisfaction
3.2.3. Secondary Aims: Parent Perceptions (CSQ-8 and Perceptions of Telepractice Feeding Services)
3.2.4. Device Use and Technical Difficulties
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arvedson, J.C. Assessment of pediatric dysphagia and feeding disorders: Clinical and instrumental approaches. Dev. Disabil. Res. Rev. 2008, 14, 118–127. [Google Scholar] [CrossRef]
- Estrem, H.H.; Thoyre, S.M.; Knafl, K.A.; Pados, B.F.; van Riper, M. “It’s a long-term process”: Description of daily family life when a child has a feeding disorder. J. Pediatr. Health Care 2018, 32, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Goday, P.; Huh, S.Y.; Silverman, A.H.; Lukens, C.T.; Dorill, P.; Cohen, S.S.; Delaney, A.L.; Feuling, M.B.; Neol, R.J.; Gisel, E.; et al. Pediatric feeding disorder—Consensus definition and conceptual framework. J. Pediatr. Gastroenterol. Nutr. 2019, 68, 124–129. [Google Scholar] [CrossRef] [PubMed]
- Tohidast, S.A.; Mansuri, B.; Bagheri, R.; Azimi, H. Provision of speech-language pathology services for the treatment of speech and language disorders in children during the COVID-19 pandemic: Problems, concerns, and solutions. Int. J. Pediatr. Otorhinolaryngol. 2020, 138, 110262. [Google Scholar] [CrossRef]
- Ashton, L.; May, J.; Brook, T.; Clarke, K. Multidisciplinary therapy services for children with feeding disorders in country South Australia. In Proceedings of the 12th National Rural Health Conference, Adelaide, Australia, 7–10 April 2013; Available online: https://www.ruralhealth.org.au/12nrhc/wp-content/uploads/2013/06/Ashton-Larissa_May-Jodie_ppr.pdf (accessed on 5 June 2021).
- Fairweather, G.C.; Lincoln, M.A.; Ramsden, R. Speech-language pathology teletherapy in rural and remote educational settings: Decreasing service inequities. Int. J. Speech-Lang. Pathol. 2016, 18, 592–602. [Google Scholar] [CrossRef] [PubMed]
- Nicholl, H. ‘Going between worlds’: Travelling with children with complex needs. J. Child Health Care 2015, 19, 293–303. [Google Scholar] [CrossRef]
- O’Donoghue, C.; Dean-Claytor, A. Training and self-reported confidence for dysphagia management among speech-language pathologists in the schools. Lang. Speech Hear. Serv. Sch. 2008, 39, 192–198. [Google Scholar] [CrossRef]
- Raatz, M.; Ward, E.C.; Marshall, J.; Afoakwah, C.; Byrnes, J. “It takes a whole day, even though it’s a one-hour appointment!” Factors impacting access to pediatric feeding services. Dysphagia 2021, 36, 419–429. [Google Scholar] [CrossRef]
- Simione, M.; Dartley, A.; Cooper-Vince, C.; Martin, V.; Hartnick, C.; Taveras, E.M.; Fiechtner, L. Family-centered outcomes that matter most to parents: A pediatric feeding disorders qualitative study. J. Pediatr. Gastroenterol. Nutr. 2020, 71, 270–275. [Google Scholar] [CrossRef]
- Zimmerman, E. Pediatric dysphagia: A rise in preterm infants and a need for more formal training for speech-language pathologists. Int. J. Gynecol. Obstet. Neonatal Care 2016, 3, 15–20. [Google Scholar] [CrossRef]
- Raatz, M.; Ward, E.C.; Marshall, J. Telepractice for the delivery of pediatric feeding services: A survey of practice investigating clinician perceptions and current service models in Australia. Dysphagia 2020, 35, 378–388. [Google Scholar] [CrossRef]
- Borders, J.C.; Sevitz, J.S.; Malandraki, J.B.; Malandraki, G.A.; Troche, M.S. Objective and subjective clinical swallowing outcomes via telehealth: Reliability in outpatient clinical practice. Am. J. Speech-Lang. Pathol. 2021, 30, 598–608. [Google Scholar] [CrossRef]
- Morrell, K.; Hyers, M.; Stuchiner, T.; Lucas, L.; Schwartz, K.; Mako, J.; Spinelli, K.J.; Yanase, L. Telehealth stroke dysphagia evaluation is safe and effective. Cerebrovasc. Dis. 2017, 44, 225–231. [Google Scholar] [CrossRef]
- Ward, E.C.; Sharma, S.; Burns, C.L.; Theodoros, D.G.; Russell, T. Validity of conducting clinical dysphagia assessments for patients with normal to mild cognitive impairment via telerehabilitation. Dysphagia 2012, 27, 460–472. [Google Scholar] [CrossRef] [PubMed]
- Ward, E.C.; Burns, C.L.; Theodoros, D.G.; Russell, T.G. Impact of dysphagia severity on clinical decision making via telerehabilitation. Telemed. e-Health 2014, 20, 296–303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kantarcigil, C.; Sheppard, J.J.; Gordon, A.M.; Friel, K.M.; Malandraki, G.A. A telehealth approach to conducting clinical swallowing evaluations in children with cerebral palsy. Res. Dev. Disabil. 2016, 55, 207–217. [Google Scholar] [CrossRef]
- Raatz, M.; Ward, E.C.; Marshall, J.; Burns, C.L. Evaluating the use of telepractice to deliver pediatric feeding assessments. Am. J. Speech-Lang. Pathol. 2021, 30, 1686–1699. [Google Scholar] [CrossRef] [PubMed]
- Rojjanasrirat, W.; Nelson, E.L.; Wambach, K.A. A pilot study of home-based videoconferencing for breastfeeding support. J. Hum. Lact. 2012, 28, 464–467. [Google Scholar] [CrossRef] [PubMed]
- Jensen, D.D.; Wallace, S.; Kelsay, P. LATCH: A breastfeeding charting system and documentation tool. J. Obstet. Gynecol. Neonatal Nurs. 1994, 23, 27–32. [Google Scholar] [CrossRef]
- Sheppard, J.J. Dysphagia disorder survey and dysphagia management staging scale (adult and pediatric applications). In Users Manual, 1st ed.; Nutritional Management Associates: Lake Hopatcong, NJ, USA, 2002. [Google Scholar]
- Raatz, M.; Ward, E.C.; Marshall, J.; Burns, C.L. Developing the system architecture for conducting synchronous paediatric feeding assessments via telepractice. J. Telemed. Telecare 2019, 25, 522–558. [Google Scholar] [CrossRef] [PubMed]
- Raatz, M.; Ward, E.C.; Marshall, J.; Burns, C.L.; Afoakwah, C.; Byrnes, J. A time and cost analysis of speech pathology paediatric feeding services delivered in-person versus via telepractice. J. Telemed. Telecare 2021. [Google Scholar] [CrossRef]
- Ward, E.C.; Burns, C.L.; Theodoros, D.G.; Russell, T.G. Evaluation of a clinical service model for dysphagia assessment via telerehabilitation. Int. J. Telemed. Appl. 2013, 2013, 918526. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, S.; Ward, E.C.; Burns, C.L.; Theodoros, D.G.; Russell, T. Assessing swallowing disorders online: A pilot telerehabilitation study. Telemed. e-Health 2011, 17, 688–695. [Google Scholar] [CrossRef] [PubMed]
- Bickell, M.; Barton, C.; Dow, K.; Fucile, S. A systematic review of clinical and psychometric properties of infant oral motor feeding assessments. Dev. Neurorehabilit. 2018, 21, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Heckathorn, D.; Speyer, R.; Taylor, J.; Cordier, R. Systematic review: Non-instrumental swallowing and feeding assessments in pediatrics. Dysphagia 2016, 31, 1–23. [Google Scholar] [CrossRef]
- Howe, T.; Lin, K.; Fu, C.; Su, C.; Hsieh, C. A review of psychometric properties of feeding assessment tools used in neonates. JOGNN J. Obstet. Gynecol. Neonatal Nurs. 2008, 37, 338–349. [Google Scholar] [CrossRef] [PubMed]
- Pados, B.F.; Park, J.; Estrem, H.; Awotwi, A. Assessment tools for evaluation of oral feeding in infants younger than 6 months. Adv. Neonatal Care 2016, 16, 143–150. [Google Scholar] [CrossRef] [Green Version]
- Dodrill, P. Functional oral intake scale—Suckle feeds and transitional feeds. In Dysphagia: Clinical Management in Adults and Children, 2nd ed.; Groher, M.E., Crary, M.A., Eds.; Mosby: Maryland Heights, MO, USA, 2016; p. 320. [Google Scholar]
- American Speech-Language-Hearing Association. Pediatric Dysphagia. Available online: https://www.asha.org/practice-portal/clinical-topics/pediatric-dysphagia/ (accessed on 30 March 2019).
- Ballard, J.L.; Auer, C.E.; Khoury, J.C. Ankyloglossia: Assessment, incidence and effect of freunuloplasty on the breastfeeding dyad. Pediatrics 2002, 101, e63. [Google Scholar] [CrossRef] [Green Version]
- Dodrill, P. Evaluating feeding and swallowing in infants and children. In Dysphagia: Clinical Management in Adults and Children, 2nd ed.; Groher, M.E., Crary, M.A., Eds.; Mosby: Maryland Heights, MO, USA, 2016; pp. 205–323. [Google Scholar]
- Hall, K. Pediatric Dysphagia Resource Guide, 1st ed.; Cengage Learning: Boston, MA, USA, 2000. [Google Scholar]
- Martinelli, R.L.C.; Marchesan, I.Q.; Berretin-Felix, G. Lingual frenulum protocol with scores for infants. Int. J. Orofac. Myol. 2012, 38, 104–112. [Google Scholar] [CrossRef]
- Wolf, L.S.; Glass, R.P. Feeding and Swallowing Disorders in Infancy: Assessment and Management; Hammill Institute on Disabilities: Austin, TX, USA, 1992. [Google Scholar]
- Sellers, D.; Mandy, A.; Pennington, L.; Hankins, M.; Morris, C. Development and reliability of a system to classify the eating and drinking ability of people with cerebral palsy. Dev. Med. Child Neurol. 2014, 56, 245–251. [Google Scholar] [CrossRef]
- Cartmill, B.; Wall, L.R.; Ward, E.C.; Hill, A.J.; Porceddu, S. Computer literacy and health locus of control as determinants for readiness and acceptability of telepractice in a head and neck cancer population. Int. J. Telerehabilit. 2016, 8, 49–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Attkisson, C. Client Satisfaction Questionnaire—8 Child Services (Parent Rated). 2014. Available online: https://csqscales.com (accessed on 22 August 2018).
- Attkisson, C.; Greenfield, T. The client satisfaction questionnaire (CSQ) scales and the service satisfaction scales-30 (SSS-30). In Outcomes Assessment in Clinical Practice; Sederer, L.L., Dickey, B., Eds.; Williams & Wilkins: Philadelphia, PA, USA, 1996; pp. 120–127. [Google Scholar]
- Burns, C.L.; Ward, E.C.; Hill, A.J.; Malcolm, K.; Bassett, L.; Kenny, L.M.; Greenup, P. A pilot trial of a speech pathology telehealth service for head and neck cancer patients. J. Telemed. Telecare 2012, 18, 443–446. [Google Scholar] [CrossRef] [PubMed]
- Collins, A.; Burns, C.L.; Ward, E.C.; Comans, T.; Blake, C.; Kenny, L.; Greenup, P.; Best, D. Home-based telehealth service for swallowing and nutritional management following head and neck cancer treatment. J. Telemed. Telecare 2017, 23, 866–872. [Google Scholar] [CrossRef] [PubMed]
- Kummervold, P.E.; Johnsen, J.A.; Skrøvseth, S.O.; Wynn, R. Using noninferiority tests to evaluate telemedicine and e-health services: Systematic review. J. Med. Internet Res. 2012, 14, e132. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Russell, T.G.; Martin-Khan, M.; Khan, A.; Wade, V. Method-comparison studies in telehealth: Study design and analysis considerations. J. Telemed. Telecare 2017, 23, 797–802. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martin, P.; Lizarondo, L.; Kumar, S. A systematic review of the factors that influence the quality and effectiveness of telesupervision for health professionals. J. Telemed. Telecare 2018, 24, 271–281. [Google Scholar] [CrossRef]
- Garand, K.L.; McCullough, G.; Crary, M.; Arvedson, J.C.; Dodrill, P. Assessment across the life span: The clinical swallow evaluation. Am. J. Speech-Lang. Pathol. 2020, 29, 919–933. [Google Scholar] [CrossRef] [PubMed]
- Clark, R.R.; Fischer, A.J.; Lehman, E.L.; Bloomfield, B.S. Developing and implementing a telehealth enhanced interdisciplinary pediatric feeding disorders clinic: A program description and evaluation. J. Dev. Phys. Disabil. 2019, 31, 171–188. [Google Scholar] [CrossRef]
- Garne Holm, K.; Brødsgaard, A.; Zachariassen, G.; Smith, A.C.; Clemensen, J. Parent perspectives of neonatal tele-homecare: A qualitative study. J. Telemed. Telecare 2019, 25, 221–229. [Google Scholar] [CrossRef]
- Rasmussen, M.K.; Clemensen, J.; Zachariassen, G.; Kidholm, K.; Brødsgaard, A.; Smith, A.C.; Holm, K.G. Cost analysis of neonatal tele-homecare for preterm infants compared to hospital-based care. J. Telemed. Telecare 2020, 26, 474–481. [Google Scholar] [CrossRef]
- Hines, M.; Lincoln, M.; Ramsden, R.; Martinovich, J.; Fairweather, C. Speech pathologists’ perspectives on transitioning to telepractice: What factors promote acceptance? J. Telemed. Telecare 2015, 21, 469–473. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | n (%) |
|---|---|
| Age (Corrected) | |
| 1–3 months | 9 (30) |
| 4–6 months | 9 (30) |
| 7–11 months | 5 (17) |
| 1–2 years | 7 (23) |
| Medical diagnose/s | |
| History of prematurity | 17 (57) |
| Neurological | 5 (17) |
| Respiratory | 19 (63) |
| Gastroenterology | 7 (23) |
| Allergy/Immunology | 5 (17) |
| Cardiac | 4 (13) |
| Developmental | 2 (7) |
| Musculoskeletal | 3 (10) |
| Genetic | 4 (13) |
| Renal | 3 (10) |
| Cleft/Craniofacial | 1 (3) |
| Structural/ENT (e.g., laryngeal cleft) | 6 (20) |
| Number of body systems impaired | |
| 0 | 1 (3) |
| 1 | 11 (37) |
| 2 | 10 (33) |
| 3 | 7 (23) |
| 7 | 1 (3) |
| FOIS-SFTF Rating (1 = most severe impairment) n = 29 | |
| 1 (No oral intake) | 0 (0) |
| 2 (Tube dependent with minimal oral intake) | 1 (3) |
| 3 (Tube dependent with consistent oral intake) | 10 (34) |
| 4 (Total oral diet requiring special preparation) | 2 (7) |
| 5 (Total oral diet requiring compensations) | 9 (31) |
| 6 (Total oral intake with no restriction relative to peers) | 7 (24) |
| EDACS Rating (5 = most severe impairment) n = 29 | |
| 1 (Eats/drinks safely and efficiently) | 7 (24) |
| 2 (Eats/drinks safely, but with limitations to efficiency) | 14 (48) |
| 3 (Eats/drinks with some limitations to safety) | 6 (21) |
| 4 (Eats and drinks with significant limitations to safety) | 2 (7) |
| 5 (Unable to eat or drink safely) | 0 (0) |
| Characteristics | n (%) |
|---|---|
| Age | |
| 18–25 years | 4 (14) |
| 26–34 years | 15 (52) |
| 35–44 years | 7 (24) |
| Not specified | 3 (10) |
| Highest level of education | |
| Grade 10 or below | 4 (14) |
| Grade 12 | 3 (10) |
| Certificate or Diploma | 13 (45) |
| Bachelor’s Degree | 9 (31) |
| Usual device/s | |
| Desktop computer | 11 (38) |
| Laptop computer | 20 (69) |
| Tablet | 15 (52) |
| Smart phone | 29 (100) |
| Confidence using device/s for everyday activities | |
| Very confident | 17 (59) |
| Somewhat confident | 11 (38) |
| Not confident | 0 (0) |
| No response | 1 (3) |
| Previously used device/s for online health related activities | |
| Yes | 12 (41) |
| No | 17 (59) |
| Confidence using device/s for online health related activities | |
| Very confident | 8 (28) |
| Somewhat confident | 14 (48) |
| Unsure | 5 (17) |
| Somewhat not confident | 1 (3) |
| No response | 1 (3) |
| Assessment Component | Percentage Exact Agreement (PEA) | Kappa Coefficient |
|---|---|---|
| Developmental screen | 98 | 0.84 |
| State | ||
| Before feed | 96 | 0.77 |
| During feed | 93 | – |
| After feed | 96 | 0.82 |
| Color | ||
| Before feed | 100 | 1.00 |
| During feed | 100 | – |
| After feed | 100 | 1.00 |
| Pre-feeding respiration | 99 | – |
| Oral sensorimotor assessment | ||
| Total agreement | 89 | – |
| Face | 99 | – |
| Lips | 99 | 0.65 |
| Tongue | 93 | – |
| Fat pads | 93 | – |
| Jaw | 99 | 0.84 |
| Saliva control | 90 | – |
| Palate | 67 a | 0.31 b |
| Cry | 83 | 0.62 |
| Infant Oral Reflex Exam (n = 17) | ||
| Rooting reflex | 94 | 0.85 |
| Tongue protrusion reflex | 82 | 0.69 |
| Transverse tongue reflex | 100 | 1.00 |
| Phasic bit | 94 | 0.77 |
| Gag | 76 a | 0.53 b |
| Tongue Tie Screen (n = 13) | ||
| Overall rating (within normal limits vs. concerns) | 92 | 0.63 |
| Tongue posture during crying | 54 a | 0.03 b |
| Shape of elevated tongue | 100 | 1.00 |
| Tongue lateralization | 62 a | 0.24 b |
| Lingual frenulum | 54 a | 0.23 b |
| Frenulum thickness | 61 a | 0.27 b |
| Frenulum attachment to tongue | 54 a | 0.32 b |
| Extension of tongue | 69 a | 0.29 b |
| Non-nutritive Suck assessment (n = 17) | ||
| Total agreement | 90 | – |
| Response to stimulus | 94 | 0.77 |
| Positive pressure generation | 100 | – |
| Negative pressure generation | 94 | 0.88 |
| Rhythmicity | 88 | 0.43 b |
| Jaw excursion | 94 | 0.64 |
| Tongue cupping (n = 8) | 88 | 0.75 |
| Bottle feeding (n = 42) | ||
| Oral phase | 92 | 0.52 b |
| Suck-swallow | 98 | 0.93 |
| Physiological stability | 98 | 0.78 |
| Disengagement cues | 91 | 1.00 |
| Feeder response to infant cues | 100 | 1.00 |
| Respiratory changes | 95 | 0.83 |
| Indicators of penetration +/- aspiration | 97 | 0.68 |
| Nasal congestion/regurgitation | 98 | 0.48 b |
| Overall assessment | ||
| Within normal limits vs impaired | 100 | 1.00 |
| FOIS-SFTF rating | 100 | 1.00 |
| EDACS rating | 100 | 1.00 |
| Recommendations | ||
| Fluid level | 100 | 1.00 |
| Equipment change | 100 | 1.00 |
| Positioning change | 97 | 0.93 |
| Implementation of feeding strategies | 90 | 0.53 b |
| Session outcome (discharge vs. urgent review vs. non-urgent review) | 100 | 1.00 |
| Parameter | 1 Strongly Disagree | 2 | 3 Neutral | 4 | 5 Strongly Agree | Median |
|---|---|---|---|---|---|---|
| Effective service delivery method for appointment reason | 0 | 1 (3%) | 2 (7%) | 15 (52%) | 11 (38%) | 4 |
| Established rapport with child | 0 | 1 (3%) | 14 (48%) | 12 (41%) | 2 (7%) | 3 |
| Established rapport with parent/carer | 0 | 1 (3%) | 1 (3%) | 16 (55%) | 11 (38%) | 4 |
| Managed child’s behavior | 0 | 0 | 12 (41%) | 15 (52%) | 2 (7%) | 4 |
| Able to assess feeding skills | 0 | 1 (3%) | 3 (10%) | 14 (48%) | 11 (38%) | 4 |
| Able to assess swallow safety | 0 | 1 (3%) | 3 (10%) | 20 (69%) | 5 (17%) | 4 |
| Able to assess oral sensorimotor skills | 0 | 2 (7%) | 4 (14%) | 16 (55%) | 7 (24%) | 4 |
| Assessing child in the home environment improved clinical decision-making | 0 | 0 | 4 (14%) | 11 (38%) | 14 (48%) | 4 |
| Information gathered via in-home telepractice that would not have been gathered during in-clinic appointment | 0 | 2 (7%) | 3 (10%) | 12 (41%) | 12 (41%) | 4 |
| Video quality adequate for general session | 0 | 2 (7%) | 2 (7%) | 15 (52%) | 10 (34%) | 4 |
| Video quality adequate for diagnostic purposes | 0 | 3 (10%) | 7 (24%) | 15 (52%) | 4 (14%) | 4 |
| Audio quality adequate for general session | 1 (3%) | 1 (3%) | 0 | 15 (52%) | 12 (41%) | 4 |
| Audio quality adequate for diagnostic purposes | 1 (3%) | 2 (7%) | 7 (24%) | 16 (55%) | 3 (10%) | 4 |
| Would use telepractice to provide feeding services again for this child | 0 | 2 (7%) | 0 | 17 (59%) | 10 (34%) | 4 |
| Parameter | 1 = Low | 2 | 3 | 4 = High | Mean |
|---|---|---|---|---|---|
| Quality of services provided to child | 0 | 0 | 3 | 20 | 3.9 |
| Received the kind of service wanted | 0 | 0 | 7 | 16 | 3.7 |
| The service met child’s needs | 0 | 1 | 8 | 14 | 3.6 |
| Would recommend service to friend’s child in need of similar help | 0 | 0 | 8 | 15 | 3.7 |
| Satisfaction with amount of help child received | 0 | 0 | 7 | 16 | 3.7 |
| Services have helped child to deal more effectively with problems | 0 | 0 | 10 | 13 | 3.6 |
| Satisfaction with services child received | 0 | 0 | 4 | 19 | 3.8 |
| Would come back | 0 | 0 | 5 | 18 | 3.8 |
| Item | Pre-Assessment | Post-Assessment | Chi-Square/ Fisher’s Exact | |||||
|---|---|---|---|---|---|---|---|---|
| Disagree | Unsure | Agree | Disagree | Unsure | Agree | No Response (post) | ||
| I feel (felt) comfortable having my child’s feeding and/or swallowing skills assessed via telehealth | 0 | 1 (4%) | 22 (96%) | 0 | 1 (4%) | 22 (96%) | 0 | 0.758 |
| I am (was) comfortable using technology for my child’s appointment | 0 | 2 (9%) | 21 (91%) | 0 | 0 | 23 (100%) | 0 | – |
| The telepractice feeding assessment will save (saved) me time (e.g., time spent travelling to appointment) | 1 (4%) | 1 (4%) | 21 (91%) | 0 | 0 | 23 (100%) | 0 | – |
| The telepractice feeding assessment will save (saved) me money (e.g., bus fare, parking) | 0 | 0 | 23 (100%) | 0 | 0 | 23 (100%) | 0 | – |
| It will be (was) easy to set up for the telepractice appointment | 0 | 7 (30%) | 16 (70%) | 1 (4%) | 1 (4%) | 21 (91%) | 0 | 0.283 |
| I feel that the online feeding assessment will be (was) equal to having a face to face feeding assessment | 1 (4%) | 10 (43%) | 12 (52%) | 1 (4%) | 3 (13%) | 19 (83%) | 0 | 0.129 |
| I will have (had) opportunities to clarify any questions I had during the online assessment | 0 | 3 (13%) | 20 (87%) | 0 | 1 (4%) | 22 (96%) | 0 | 0.875 |
| I will be (was) able to manage my child’s behavior during the telepractice assessment | 1 (4%) | 6 (26%) | 16 (70%) | 0 | 2 (9%) | 21 (91%) | 0 | 0.776 |
| I feel (felt) the telepractice feeding assessment will accurately represent(ed) my child’s usual feeding and swallowing skills | 0 | 8 (35%) | 15 (65%) | 1 (4%) | 0 | 22 (96%) | 0 | 0.130 |
| Having the telepractice appointment in our home will improve (improved) the speech pathologist’s understanding of my child’s feeding skills and behavior | 0 | 3 (13%) | 20 (87%) | 1 (4%) | 2 (9%) | 20 (87%) | 0 | 0.236 |
| I will be (was) able to establish rapport with the telepractice speech pathologist | 0 | 1 (4%) | 22 (96%) | 0 | 1 (4%) | 22 (96%) | 0 | 0.958 |
| My child will be (was) able to establish rapport with the telepractice speech pathologist | 0 | 8 (35%) | 15 (65%) | 2 (9%) | 3 (13%) | 14 (61%) | 4 (17%) | 0.016 * |
| I feel that a telepractice feeding assessment can replace a face-to-face feeding assessment | 1 (4%) | 9 (39%) | 13 (57%) | 1 (4%) | 5 (22%) | 15 (65%) | 2 (9%) | 0.07 |
| I feel telepractice will improve easy access to healthcare | 0 | 2 (9%) | 21 (91%) | 0 | 2 (9%) | 19 (83%) | 2 (9%) | 0.004 * |
| I feel telepractice will be beneficial for other children with feeding difficulties | 0 | 5 (22%) | 18 (78%) | 1 (4%) | 2 (9%) | 18 (78%) | 2 (9%) | 0.557 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raatz, M.; Ward, E.C.; Marshall, J.; Burns, C.L. Evaluating the Use of Telepractice for Bottle-Feeding Assessments. Children 2021, 8, 989. https://doi.org/10.3390/children8110989
Raatz M, Ward EC, Marshall J, Burns CL. Evaluating the Use of Telepractice for Bottle-Feeding Assessments. Children. 2021; 8(11):989. https://doi.org/10.3390/children8110989
Chicago/Turabian StyleRaatz, Madeline, Elizabeth C. Ward, Jeanne Marshall, and Clare L. Burns. 2021. "Evaluating the Use of Telepractice for Bottle-Feeding Assessments" Children 8, no. 11: 989. https://doi.org/10.3390/children8110989
APA StyleRaatz, M., Ward, E. C., Marshall, J., & Burns, C. L. (2021). Evaluating the Use of Telepractice for Bottle-Feeding Assessments. Children, 8(11), 989. https://doi.org/10.3390/children8110989






