Comparison of Heart Rate Feedback from Dry-Electrode ECG, 3-Lead ECG, and Pulse Oximetry during Newborn Resuscitation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Equipment and Data Collection
2.3. Inclusion and Exclusion Criteria
2.4. Calculations and Definitions
2.5. Statistical Analysis
2.6. Ethical Considerations
3. Results
3.1. General Characteristics of Participants
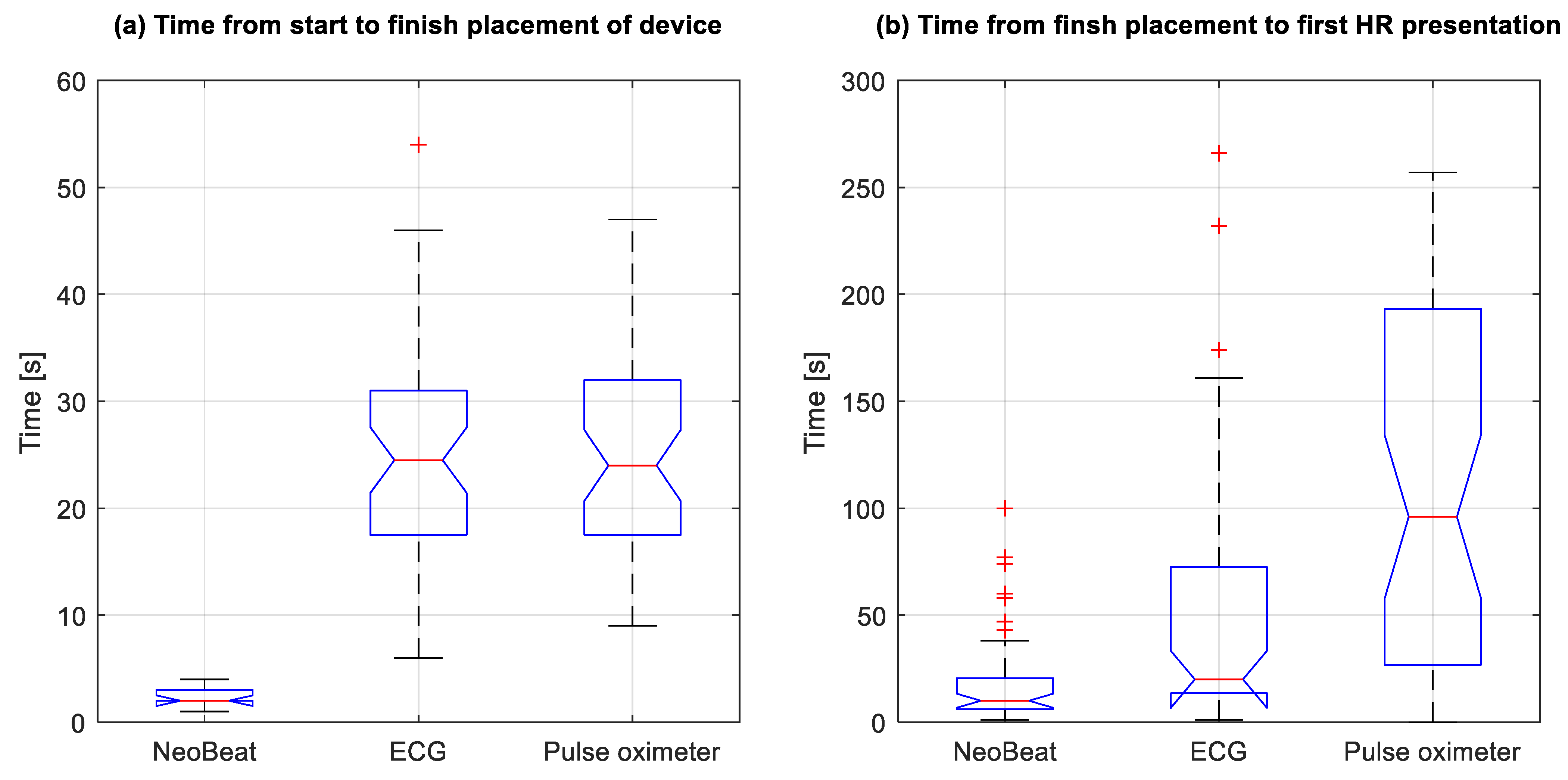
3.2. Time from Birth to Placement of the Devices and Device Placement Time
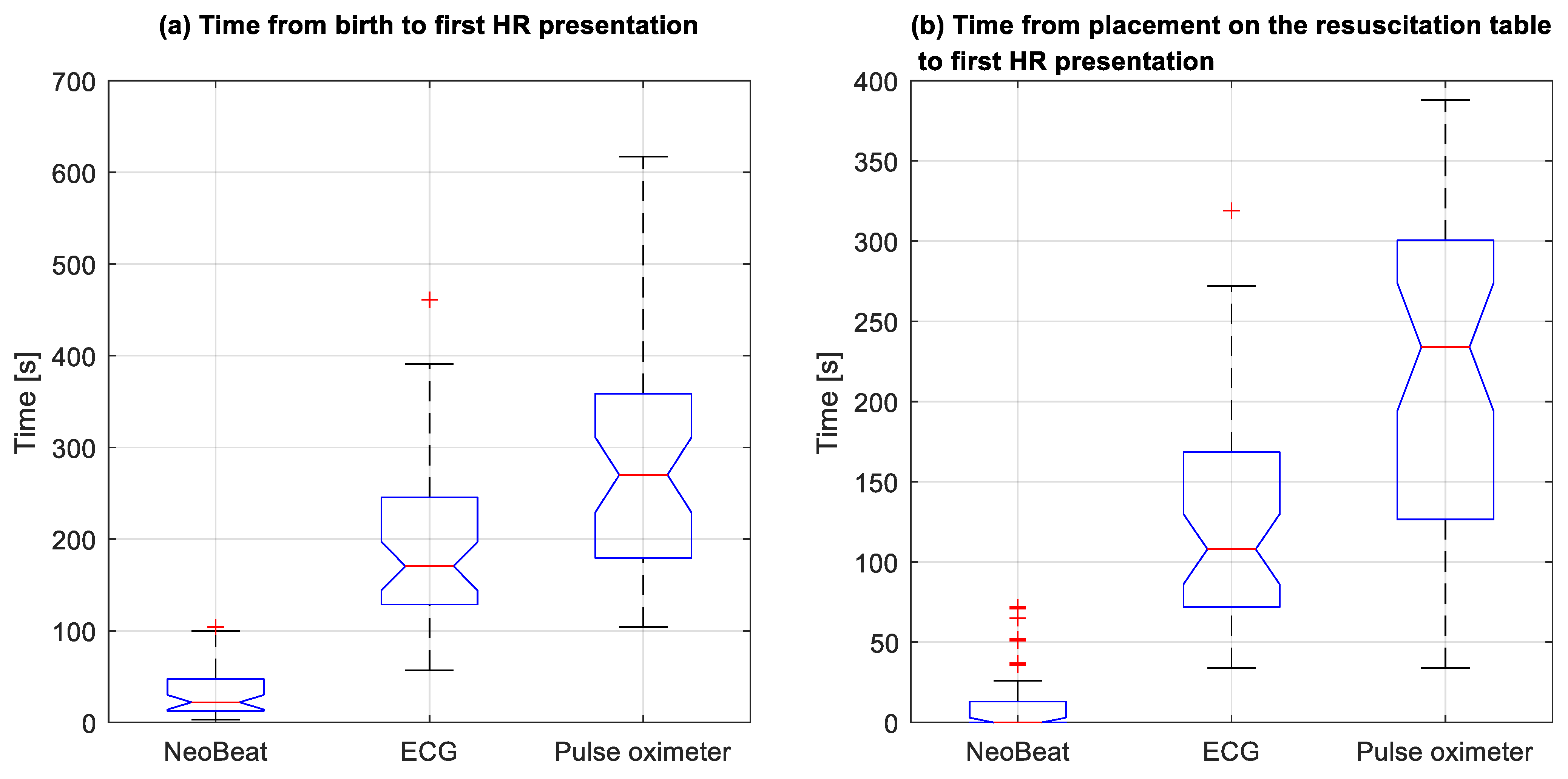
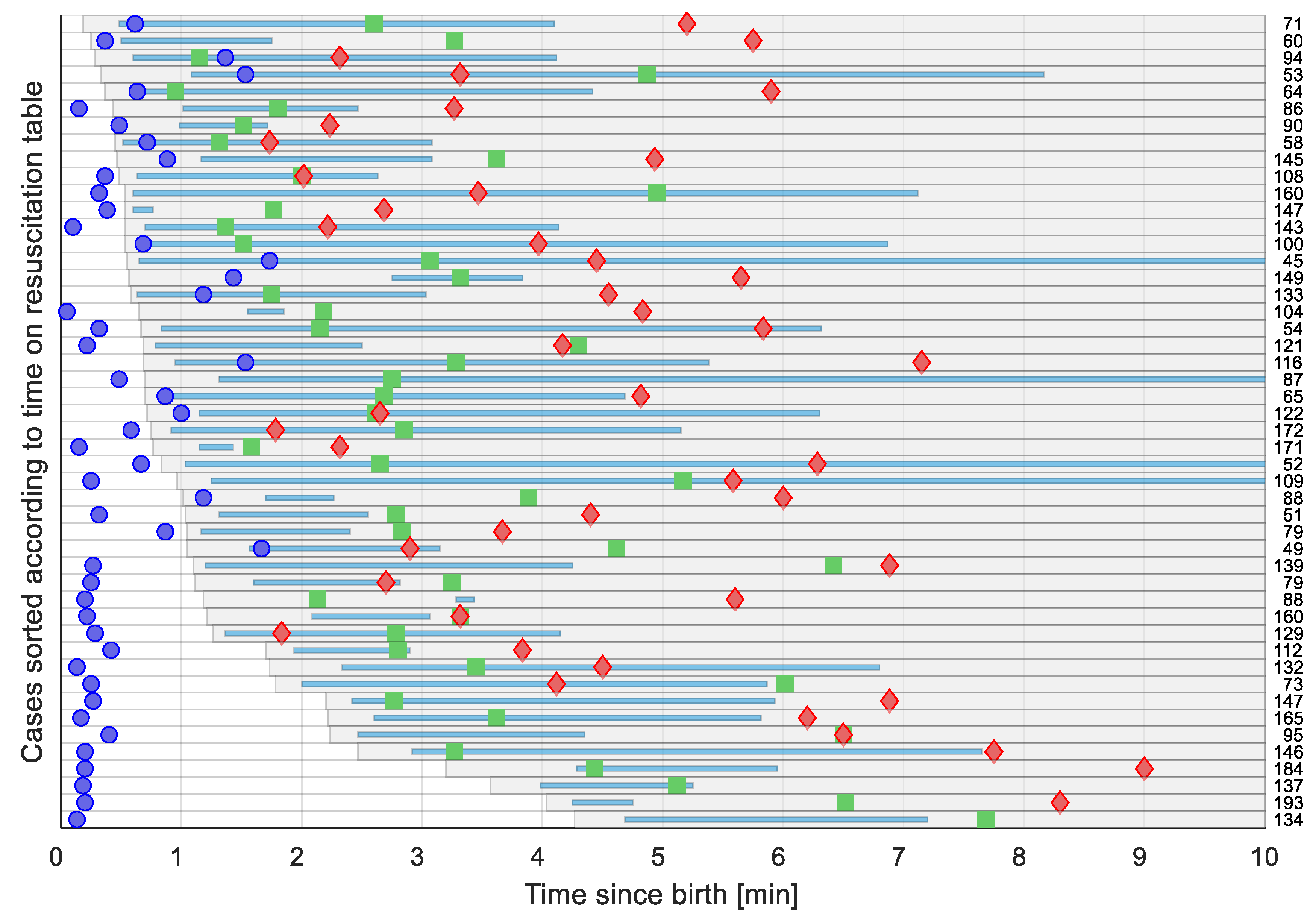
3.3. Time to First HR Presentation
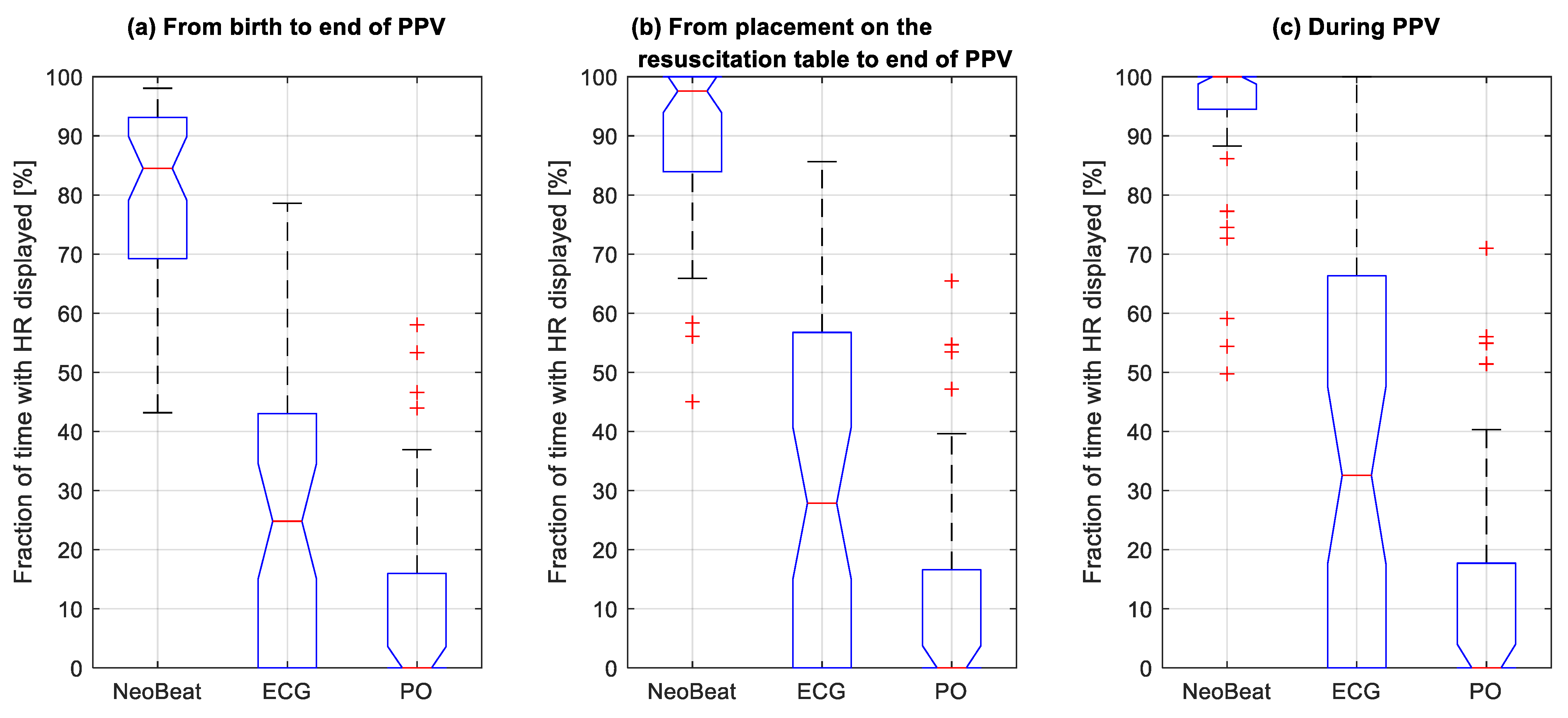
3.4. Proportion of Time with HR Feedback during Resuscitation
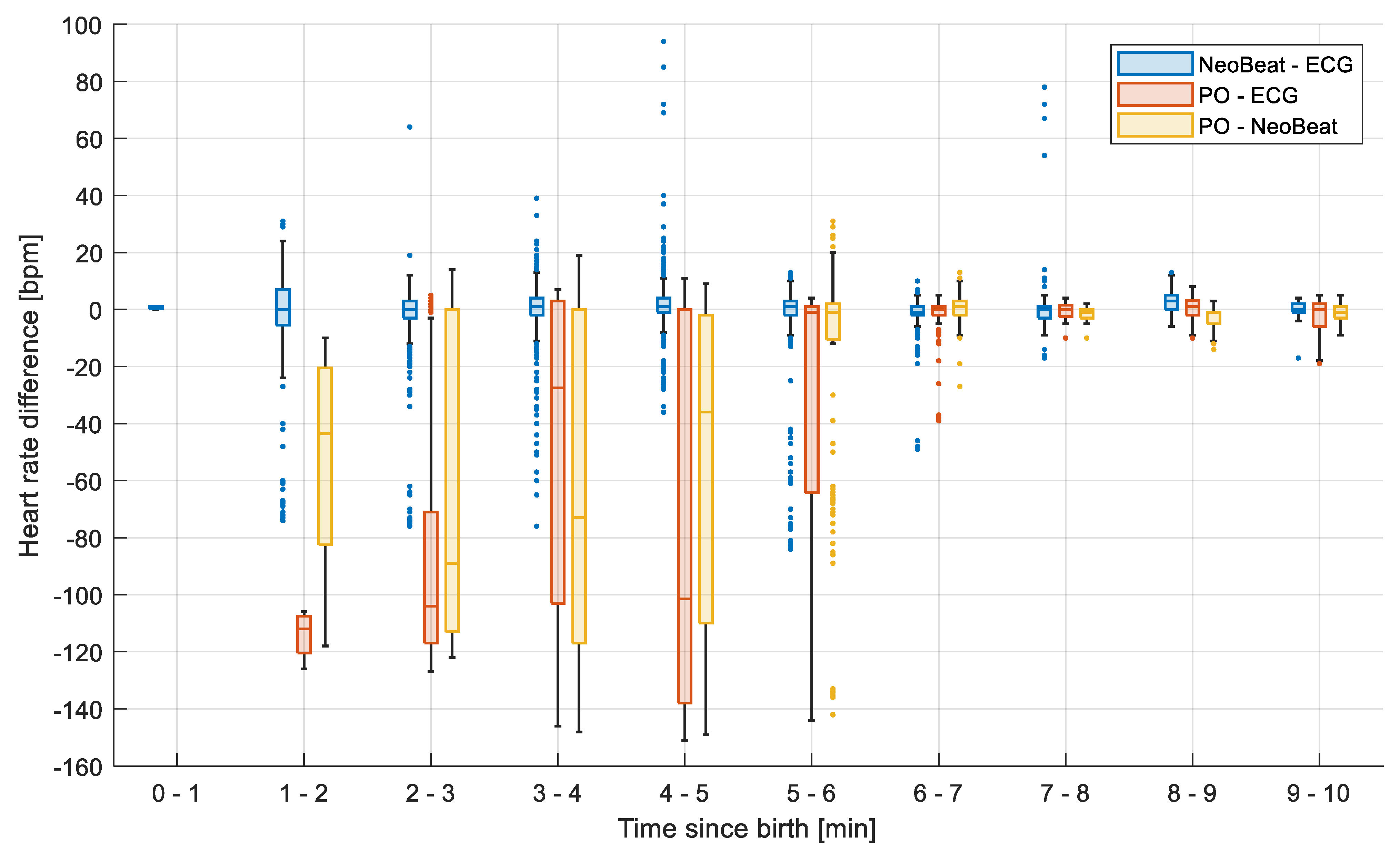
3.5. Heart Rate Correlation between Devices
4. Discussion
4.1. NeoBeat Was Placed More Rapidly
4.2. Dry-Electrode Technology Provided HR Feedback More Rapidly and More Continuously during Resuscitation
4.3. Current Guideline Recommendations and HR Thresholds
4.4. PO Underestimates HR until Six Minutes from Birth
4.5. Prediction Value of HR for Outcome
4.6. Future Studies and Knowledge Gaps
4.7. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Wyckoff, M.H.; Wyllie, J.; Aziz, K.; de Almeida, M.F.; Fabres, J.; Fawke, J.; Guinsburg, R.; Hosona, S.; Isayama, T.; Kapadia, V.S.; et al. Neonatal Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2020, 142, S185–S221. [Google Scholar] [CrossRef] [PubMed]
- Madar, J.; Roehr, C.C.; Ainsworth, S.; Ersdal, H.; Morley, C.; Rüdiger, M.; Skåre, C.; Szczapa, T.; te Pas, A.; Trevisanuto, D.; et al. European Resuscitation Council Guidelines 2021: Newborn resuscitation and support of transition of infants at birth. Resuscitation 2021, 161, 291–326. [Google Scholar] [CrossRef]
- van Vonderen, J.J.; Hooper, S.B.; Kroese, J.K.; Roest, A.A.; Narayen, I.C.; van Zwet, E.W.; Te Pas, A.B. Pulse Oximetry measures a lower heart rate at birth compared with electrocardiography. J. Pediatric 2015, 166, 49–53. [Google Scholar] [CrossRef]
- Linde, J.E.; Schulz, J.; Perlman, J.M.; Øymar, K.; Francis, F.; Eilevstjønn, J.; Ersdal, H.L. Normal Newborn Heart Rate in the First Five Minutes of Life Assessed by Dry-Electrode Electrocardiography. Neonatology 2016, 110, 231–237. [Google Scholar] [CrossRef]
- Bjorland, P.A.; Ersdal, H.L.; Eilevstjønn, J.; Øymar, K.; Davis, P.G.; Rettedal, S.I. Changes in heart rate from 5 s to 5 min after birth in vaginally delivered term newborns with delayed cord clamping. Arch. Dis. Child. Fetal Neonatal Ed. 2020, 106, 311–315. [Google Scholar] [CrossRef]
- Pike, H.; Eilevstjønn, J.; Bjorland, P.; Linde, J.; Ersdal, H.; Rettedal, S. Heart rate detection properties of dry-electrode ECG compared to conventional 3-lead gel-electrode ECG in newborns. BMC Res. Notes 2021, 14, 166. [Google Scholar] [CrossRef] [PubMed]
- Bush, J.B.; Cooley, V.; Perlman, J.; Chang, C. NeoBeat offers rapid newborn heart rate assessment. Arch. Dis. Child. Fetal Neonatal Ed. 2021, 106, 550–552. [Google Scholar] [CrossRef] [PubMed]
- Bjorland, P.A.; Øymar, K.; Ersdal, H.L.; Rettedal, S.I. Incidence of newborn resuscitative interventions at birth and short-term outcomes: A regional population-based study. BMJ Paediatr. Open 2019, 3, e000592. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, P.A.; Cheung, P.Y.; Lee, T.F.; O’Reilly, M.; Schmölzer, G.M. Novel technologies for heart rate assessment during neonatal resuscitation at birth—A systematic review. Resuscitation 2019, 143, 196–207. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A.P.; Schmolzer, G.M. Heart Rate Assessment during Neonatal Resuscitation. Healthcare 2020, 8, 43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eilevstjonn, J.; Linde, J.E.; Blacy, L.; Kidanto, H.; Ersdal, H.L. Distribution of heart rate and responses to resuscitation among 1237 apnoeic newborns at birth. Resuscitation 2020, 152, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Ersdal, H.L.; Mduma, E.; Svensen, E.; Perlman, J.M. Early initiation of basic resuscitation interventions including face mask ventilation may reduce birth asphyxia related mortality in low-income countries: A prospective descriptive observational study. Resuscitation 2012, 83, 869–873. [Google Scholar] [CrossRef] [PubMed]
- Linde, J.E.; Schulz, J.; Perlman, J.M.; Øymar, K.; Blacy, L.; Kidanto, H.; Ersdal, H.L. The relation between given volume and heart rate during newborn resuscitation. Resuscitation 2017, 117, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Linde, J.E.; Perlman, J.M.; Øymar, K.; Schulz, J.; Eilevstjønn, J.; Thallinger, M.; Kusulla, S.; Kidanto, H.L.; Ersdal, H.L. Predictors of 24-h outcome in newborns in need of positive pressure ventilation at birth. Resuscitation 2018, 129, 1–5. [Google Scholar] [CrossRef] [PubMed]

| Patient Demographic | |
|---|---|
| Gestational age (weeks) | |
| Mean (SD) | 39.5 (1.8) |
| Median (range) | 40 (32–41) |
| Term | 45 |
| Late preterm (34 0/7–36 6/7 weeks) | 2 |
| Preterm < 34 weeks | 1 |
| Birth weight (grams) | |
| Mean (SD) | 3538 (609) |
| Median (range) | 3583 (1730–5015) |
| Female sex | 20 (40%) |
| Mode of delivery | |
| Spontaneous vaginal | 13 (26%) |
| Instrumental vaginal | 26 (52%) |
| Forceps | 4 (8%) |
| Vacuum | 22 (44%) |
| Emergency Caesarean section | 11 (22%) |
| Apgar score | |
| Median (range) | |
| 1 min | 4 (0–9) |
| 5 min | 7 (1–10) |
| 10 min | 9 (4–10) |
| Umbilical arterial pH | |
| Mean (SD) | 7.2 (0.09) |
| Intubation | 2 (4%) |
| Chest compressions | 4 (8%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rettedal, S.; Eilevstjønn, J.; Kibsgaard, A.; Kvaløy, J.T.; Ersdal, H. Comparison of Heart Rate Feedback from Dry-Electrode ECG, 3-Lead ECG, and Pulse Oximetry during Newborn Resuscitation. Children 2021, 8, 1092. https://doi.org/10.3390/children8121092
Rettedal S, Eilevstjønn J, Kibsgaard A, Kvaløy JT, Ersdal H. Comparison of Heart Rate Feedback from Dry-Electrode ECG, 3-Lead ECG, and Pulse Oximetry during Newborn Resuscitation. Children. 2021; 8(12):1092. https://doi.org/10.3390/children8121092
Chicago/Turabian StyleRettedal, Siren, Joar Eilevstjønn, Amalie Kibsgaard, Jan Terje Kvaløy, and Hege Ersdal. 2021. "Comparison of Heart Rate Feedback from Dry-Electrode ECG, 3-Lead ECG, and Pulse Oximetry during Newborn Resuscitation" Children 8, no. 12: 1092. https://doi.org/10.3390/children8121092
APA StyleRettedal, S., Eilevstjønn, J., Kibsgaard, A., Kvaløy, J. T., & Ersdal, H. (2021). Comparison of Heart Rate Feedback from Dry-Electrode ECG, 3-Lead ECG, and Pulse Oximetry during Newborn Resuscitation. Children, 8(12), 1092. https://doi.org/10.3390/children8121092







