Reducing the Burden of Care: Multidisciplinary Management of Late-Manifested Crouzon Syndrome—A Case Report
Abstract
:1. Introduction
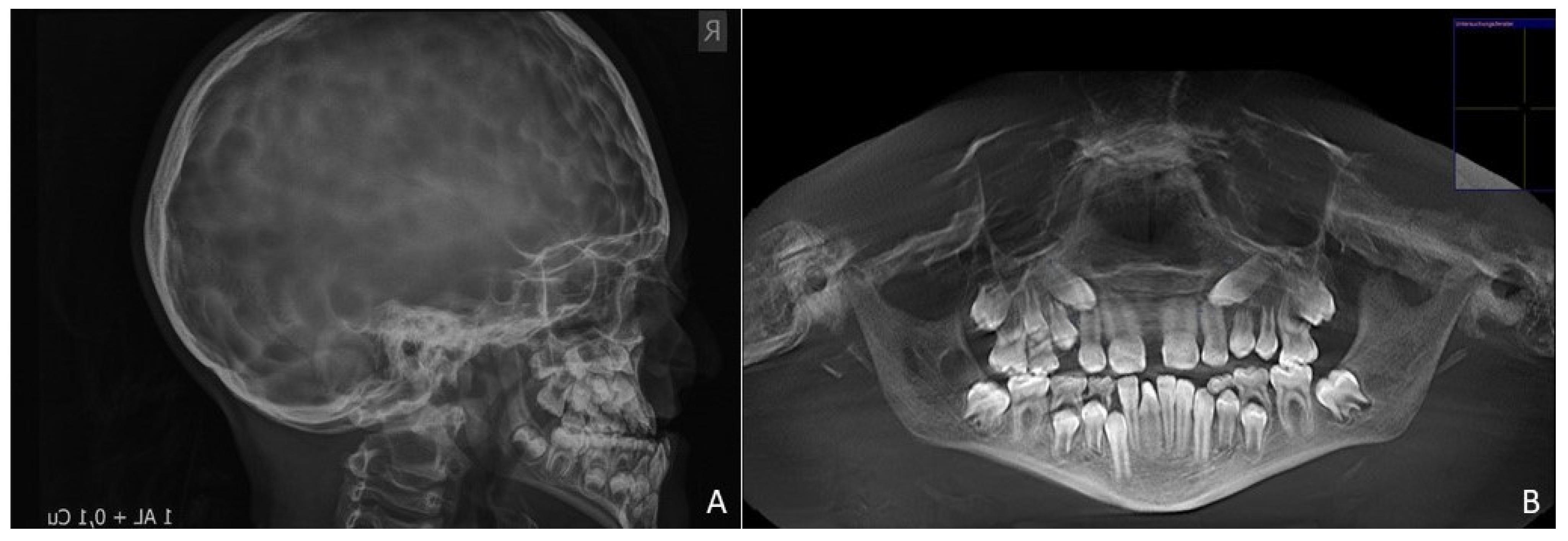
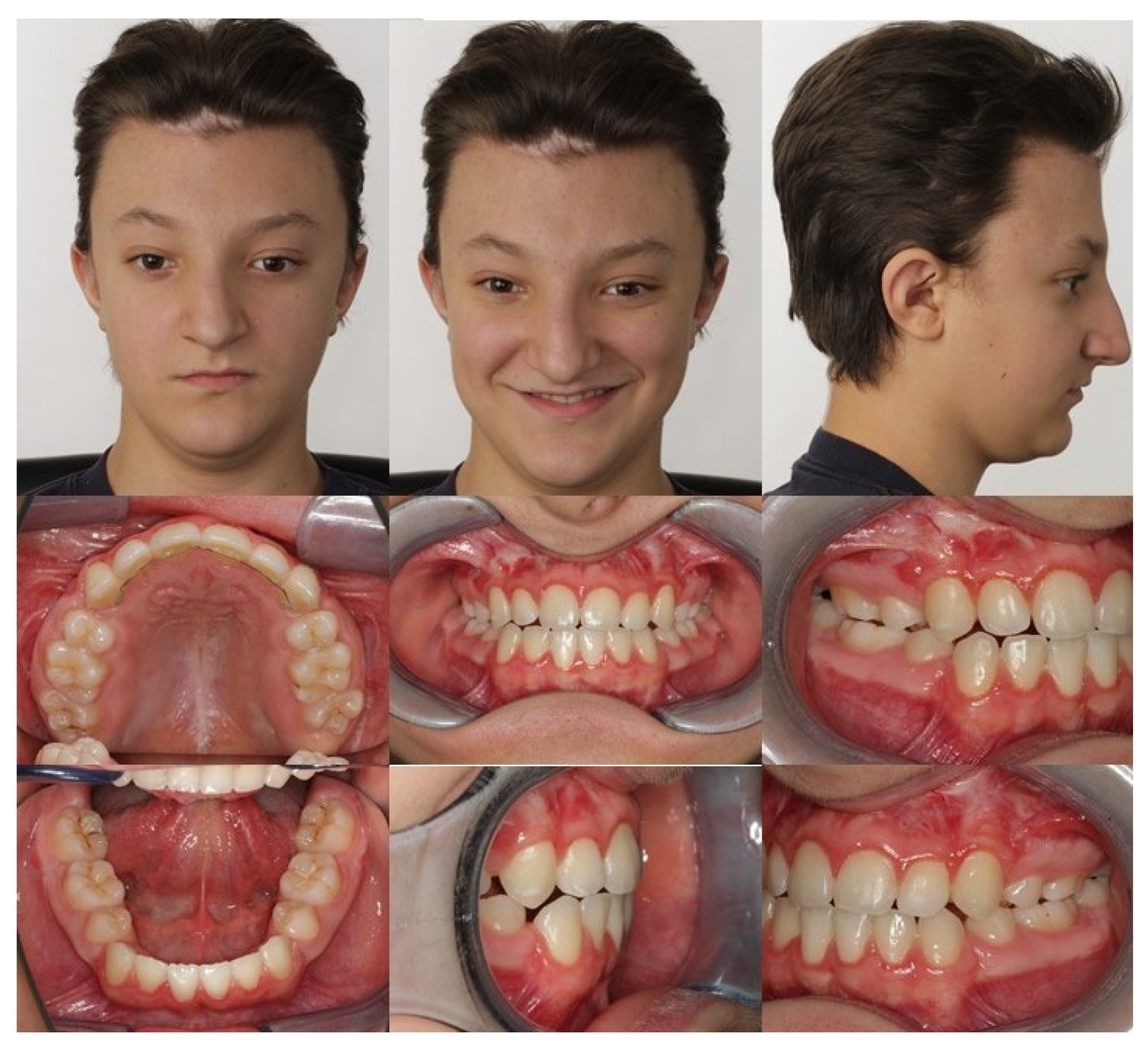
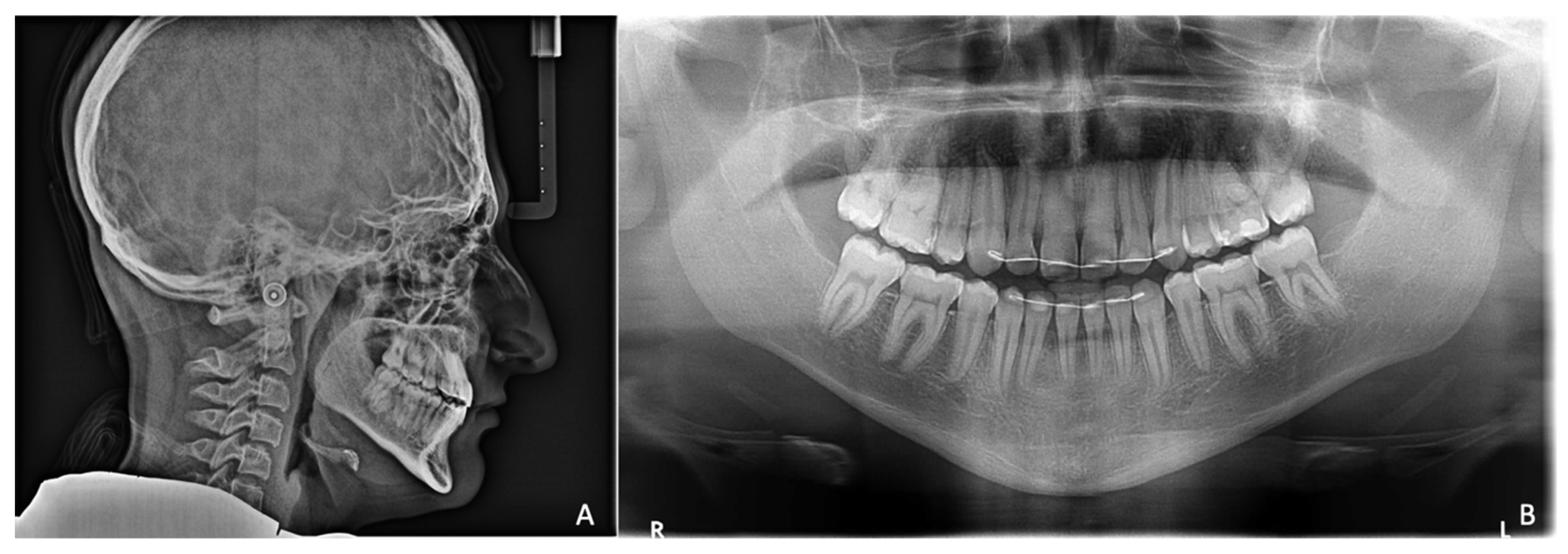
2. Case Report
Assessment of Patient’s Quality of Life
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cohen, M.M.; Kreiborg, S. Birth prevalence studies of the Crouzon syndrome: Comparison of direct and indirect methods. Clin. Genet. 1992, 41, 12–25. [Google Scholar] [CrossRef] [PubMed]
- Al-Namnam, N.M.; Hariri, F.; Thong, M.K.; Rahman, Z.A. Crouzon syndrome: Genetic and intervention review. J. Oral Biol. Craniofacial Res. 2019, 9, 37–39. [Google Scholar] [CrossRef]
- Reardon, W.; Winter, R.M.; Rutland, P.; Pulleyn, L.J.; Jones, B.M.; Malcolm, S. Mutations in the fibroblast growth factor receptor 2 gene cause Crouzon syndrome. Nat. Genet. 1994, 8, 98–103. [Google Scholar] [CrossRef] [PubMed]
- Zöller, J.E.; Kübler, A.C.; Lorber, W.D.; Mühling, J.F.H. Kraniofaziale Chirurgie; Springer: Berlin/Heidelberg, Germany, 2003. [Google Scholar]
- al-Qattan, M.M.; Phillips, J.H. Clinical features of Crouzon’s syndrome patients with and without a positive family history of Crouzon’s syndrome. J. Craniofacial Surg. 1997, 8, 11–13. [Google Scholar] [CrossRef] [PubMed]
- Virchow, R. Ueber den Cretinismus, namentlich in Franken, und über pathologische Schädelformen. Verh. Phys. Med. Gesellsch Würzburg 1851, 2, 230–256. [Google Scholar]
- Meazzini, M.C.; Corradi, F.; Mazzoleni, F.; De Ponti, E.; Maccagni, M.; Novelli, G.; Bozzetti, A. Circummaxillary Sutures in Patients with Apert, Crouzon, and Pfeiffer Syndromes Compared to Nonsyndromic Children: Growth, Orthodontic, and Surgical Implications. Cleft Palate-Craniofacial J. 2021, 58, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Crouzon, O. Dysostosis craniofaciale hereditaire. Bull. Mem. Soc. Med. Hosp. Paris 1912, 33, 545–555. [Google Scholar]
- Balyen, L.; Deniz Balyen, L.S.; Pasa, S. Clinical characteristics of Crouzon syndrome. Oman J. Ophthalmol. 2017, 10, 120–122. [Google Scholar] [CrossRef] [PubMed]
- David, D.J.; Poswillo, D.; Simpson, D. The Craniosynostosis: Causes, Natural History and Management; Springer: London, UK, 2012. [Google Scholar]
- Pal, U.S.; Gupta, C.; Chellappa, A.A.L. Crouzon syndrome with primary optic nerve atrophy and normal brain functions: A case report. J. Oral Biol. Craniofacial Res. 2012, 2, 116–118. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lu, X.; Sawh-Martinez, R.; Forte, A.J.; Wu, R.; Cabrejo, R.; Wilson, A.; Steinbacher, D.M.; Alperovich, M.; Alonso, N.; Persing, J.A. Classification of Subtypes of Crouzon Syndrome Based on the Type of Vault Suture Synostosis. J. Craniofacial Surg. 2020, 31, 678–684. [Google Scholar] [CrossRef] [PubMed]
- Wood, B.C.; Oh, A.K.; Keating, R.F.; Boyajian, M.J.; Myseros, J.S.; Magge, S.N.; Rogers, G.F. Progressive postnatal pansynostosis: An insidious and pernicious form of craniosynostosis. J. Neurosurg. Pediatrics 2015, 16, 309–316. [Google Scholar] [CrossRef] [Green Version]
- Rogers, G.F.; Greene, A.K.; Proctor, M.R.; Mulliken, J.B.; Goobie, S.M.; Stoler, J.M. Progressive Postnatal Pansynostosis. Cleft Palate-Craniofacial J. 2015, 52, 751–757. [Google Scholar] [CrossRef] [PubMed]
- Hoefkens, M.F.; Vermeij-Keers, C.; Vaandrager, J.M. Crouzon syndrome: Phenotypic signs and symptoms of the postnatally expressed subtype. J. Craniofacial Surg. 2004, 15, 233–240; discussion 241–232. [Google Scholar] [CrossRef] [PubMed]
- Mueller, M.; Schilling, T.; Minne, H.W.; Ziegler, R. A systemic acceleratory phenomenon (SAP) accompanies the regional acceleratory phenomenon (RAP) during healing of a bone defect in the rat. J. Bone Miner. Res. 1991, 6, 401–410. [Google Scholar] [CrossRef]
- Frost, H.M. The Regional Acceleratory Phenomenon: A Review. Henry Hosp. Med. J. 1983, 31, 3–9. [Google Scholar]
- Liou, E.J.; Chen, P.H.; Wang, Y.C.; Yu, C.C.; Huang, C.S.; Chen, Y.R. Surgery-first accelerated orthognathic surgery: Postoperative rapid orthodontic tooth movement. J. Oral Maxillofac. Surg. 2011, 69, 781–785. [Google Scholar] [CrossRef]
- Shaw, W. Global Strategies to Reduce the Health Care Burden of Craniofacial Anomalies: Report of WHO Meetings on International Collaborative Research on Craniofacial Anomalies. Cleft Palate-Craniofacial J. 2004, 41, 238–243. [Google Scholar] [CrossRef]
- Kubler, A.; Zoller, J. Trans-facial distraction of the facial skull at the LeFort III level. Mund- Kiefer-Gesichtschirurgie MKG 2002, 6, 153–157. [Google Scholar] [CrossRef]
- Stavropoulos, D.; Hallberg, U.; Mohlin, B.; Hagberg, C. Living with Crouzon syndrome: How do young adults with Crouzon syndrome handle their life situation? Int. J. Paediatric Dent. 2011, 21, 35–42. [Google Scholar] [CrossRef]
- Sakamoto, Y.; Takenouchi, T.; Miwa, T.; Kishi, K. Assessment of long-term quality of life in patients with syndromic craniosynostosis. J. Plast. Reconstr. Aesthetic Surg. 2020, 74, 336–340. [Google Scholar] [CrossRef]
- Prahl, C.; Prahl-Andersen, B. Craniofacial Anomalies and Quality of Life. Semin. Orthod. 2007, 13, 116–121. [Google Scholar] [CrossRef]
- Sierwald, I.; John, M.T.; Sagheri, D.; Neuschulz, J.; Schuler, E.; Splieth, C.; Jost-Brinkmann, P.G.; Reissmann, D.R. The German 19-item version of the Child Oral Health Impact Profile: Translation and psychometric properties. Clin. Oral Investig. 2016, 20, 301–313. [Google Scholar] [CrossRef]
- Aarabi, G.; Reissmann, D.R.; Sagheri, D.; Neuschulz, J.; Heydecke, G.; Kofahl, C.; Sierwald, I. Oral health-related quality of life of children and adolescents with and without migration background in Germany. Qual. Life Res. 2018, 27, 2619–2627. [Google Scholar] [CrossRef]
- Nada, R.M.; Sugar, A.W.; Wijdeveld, M.G.; Borstlap, W.A.; Clauser, L.; Hoffmeister, B.; Kuijpers-Jagtman, A.M. Current practice of distraction osteogenesis for craniofacial anomalies in Europe: A web based survey. J. Craniomaxillofac. Surg. 2010, 38, 83–89. [Google Scholar] [CrossRef]
- Bredero-Boelhouwer, H.; Joosten, K.F.; van Veen-van der Hoek, M.; Mathijssen, I.M. Family-centred care during midface advancement with a rigid external device: What do families need? J. Plast. Reconstr. Aesthetic Surg. 2013, 66, 1103–1108. [Google Scholar] [CrossRef]
- Engel, M.; Berger, M.; Hoffmann, J.; Kuhle, R.; Ruckschloss, T.; Ristow, O.; Freudlsperger, C.; Kansy, K. Midface correction in patients with Crouzon syndrome is Le Fort III distraction osteogenesis with a rigid external distraction device the gold standard? J. Cranio-Maxillofac. Surg. 2019, 47, 420–430. [Google Scholar] [CrossRef]
- Kubler, A.C.; Speder, B.; Zoller, J.E. Fronto-orbital advancement with simultaneous LeFort III-distraction. J. Cranio-Maxillofac. Surg. 2004, 32, 291–295. [Google Scholar] [CrossRef]
- Arriola-Guillen, L.E.; Aliaga-Del Castillo, A.; Ruiz-Mora, G.A.; Rodriguez-Cardenas, Y.A.; Dias-Da Silveira, H.L. Influence of maxillary canine impaction characteristics and factors associated with orthodontic treatment on the duration of active orthodontic traction. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 391–400. [Google Scholar] [CrossRef]
- Lee, Y.; Park, J.H.; Chang, N.Y.; Lee, M.Y.; Kim, B.C.; Seo, H.Y.; Mangal, U.; Chae, J.M. Assessment of bone density changes following two-jaw surgery using multidetector computed tomography: A pilot study. Korean J. Orthod. 2020, 50, 157–169. [Google Scholar] [CrossRef]
- Mathijssen, I.M. Guideline for Care of Patients with the Diagnoses of Craniosynostosis: Working Group on Craniosynostosis. J. Craniofacial Surg. 2015, 26, 1735–1807. [Google Scholar] [CrossRef] [Green Version]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Achterrath, S.; Kruse, T.; Neuschulz, J.; Graf, I.; Zöller, J.; Braumann, B. Reducing the Burden of Care: Multidisciplinary Management of Late-Manifested Crouzon Syndrome—A Case Report. Children 2021, 8, 1122. https://doi.org/10.3390/children8121122
Achterrath S, Kruse T, Neuschulz J, Graf I, Zöller J, Braumann B. Reducing the Burden of Care: Multidisciplinary Management of Late-Manifested Crouzon Syndrome—A Case Report. Children. 2021; 8(12):1122. https://doi.org/10.3390/children8121122
Chicago/Turabian StyleAchterrath, Sarah, Teresa Kruse, Julia Neuschulz, Isabelle Graf, Joachim Zöller, and Bert Braumann. 2021. "Reducing the Burden of Care: Multidisciplinary Management of Late-Manifested Crouzon Syndrome—A Case Report" Children 8, no. 12: 1122. https://doi.org/10.3390/children8121122
APA StyleAchterrath, S., Kruse, T., Neuschulz, J., Graf, I., Zöller, J., & Braumann, B. (2021). Reducing the Burden of Care: Multidisciplinary Management of Late-Manifested Crouzon Syndrome—A Case Report. Children, 8(12), 1122. https://doi.org/10.3390/children8121122






