Surgical Treatment of Sprengel’s Deformity: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
- (1)
- Release of the medial muscle attachments, lowering the scapula and securing the inferior pole to the rib or the surrounding muscles. The main procedures belonging to this group are the Putti or Putti–Schrock procedure and Green’s procedure.
- a.
- Putti’s procedure, which is uncommon and obsolete, involves the lowering of the scapula and its fixing to the rib. Schrock’s modified procedure adds the osteotomy of the supraspinous scapular region and the acromial base to facilitate scapular descent [13].
- b.
- Green’s procedure, via a midline incision, consists of extraperiosteal detachment of the medial and superior scapular muscles, excision of the supraspinous portion, lowered positioning of the scapula and reattachment of the muscles. In the modified technique, the inferior angle of the scapula ias placed into a pocket created beneath the latissimus dorsi muscle, eliminating the need for a traction system, previously secured by a percutaneous wire [14,15]. Green’s procedure provides a good visualization of the supero-medial scapular angle, better access to the acromiothoracic vasculo-nervous pedicle and an intraoperative exposition of the scapula, which allows one to achieve a good scapular mobilization. It is considered a difficult technique, frequently associated with a wide scar-keloid.
- (2)
- Release of the trapezius, elevator scapulae and rhomboids at the origins from the spinous processes, placing the scapula in an inferiorly-located pocket and reattaching the muscles inferiorly. The most widespread technique was reported by Woodward [16,17] in an attempt to simplify surgery and decrease complications. Woodward’s procedure seems the most physiological and the best biomechanically adapted, since it displaces more distally the origin of muscle insertion. On the other hand, it does not modify the muscular insertion and the scapular rotation and its complexity is increased in cases of spinal deformity, such as scoliosis or vertebral abnormalities.
- (3)
- Mears’s procedure. Through a transverse incision centered on the scapular spine, this procedure consists of the muscular detachment at the scapular origin and the excision of the superomedial angle. It adds an oblique osteotomy through the body of the scapula to avoid the impingement of the residual portions of the bone during full abduction. The literature has reported the need for the resection of at least 50% of the body to obtain an adequate ROM. The technique includes a release of the long head of the triceps, which is considered by the author as a passive limitation of the abduction [18,19].
- (4)
- Partial scapulectomy, consisting in the excision of the superomedial scapular angle. This procedure is performed, separately or in association with other techniques, when this portion is redundant [20,21]. This treatment does not improve scapular function, but it has a role in cases with mild disfigurement.
- (5)
- Vertical scapular osteotomy (VSO). Following a vertical paramedial incision, the scapula is osteotomized about 1 cm from its vertebral border, the supero-medial part of the scapula is freed of all muscle attachments and the major lateral portion is lowered and reattached. This category includes the König–Wittek procedure [22], which was rapidly abandoned, because of scar-keloids, difficulties in osteotomy and postoperative bone irregularities, as well as poor functional improvement [23].
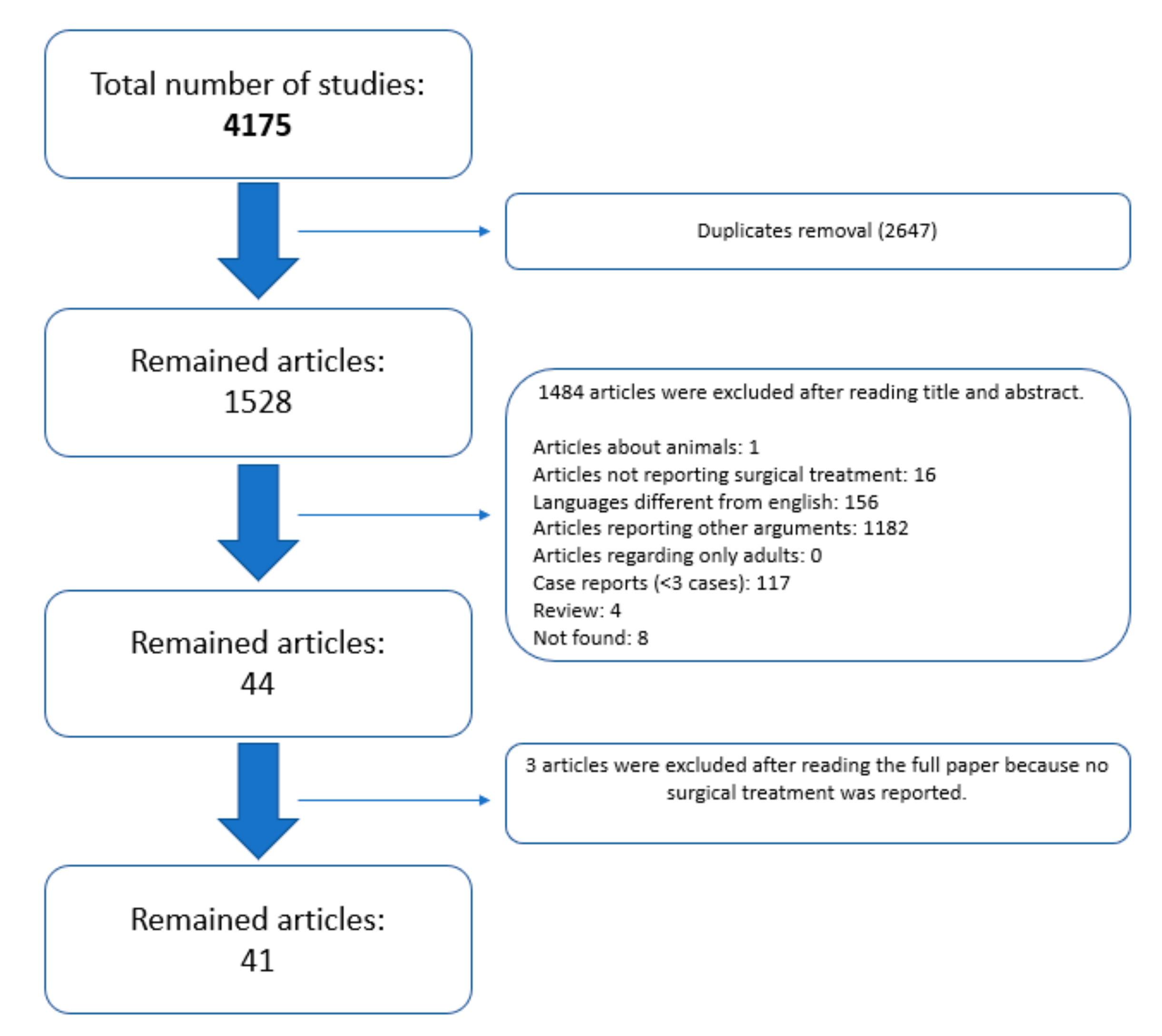
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Eligibility Criteria
2.4. Article Selection
2.5. Data Extraction, Analysis and Critical Appraisal
2.6. Statistical Analysis
3. Results
3.1. Studies Included and Quality Assessment
3.2. Demographic Data
3.3. Clinical and Radiological Presentation
3.4. Surgery
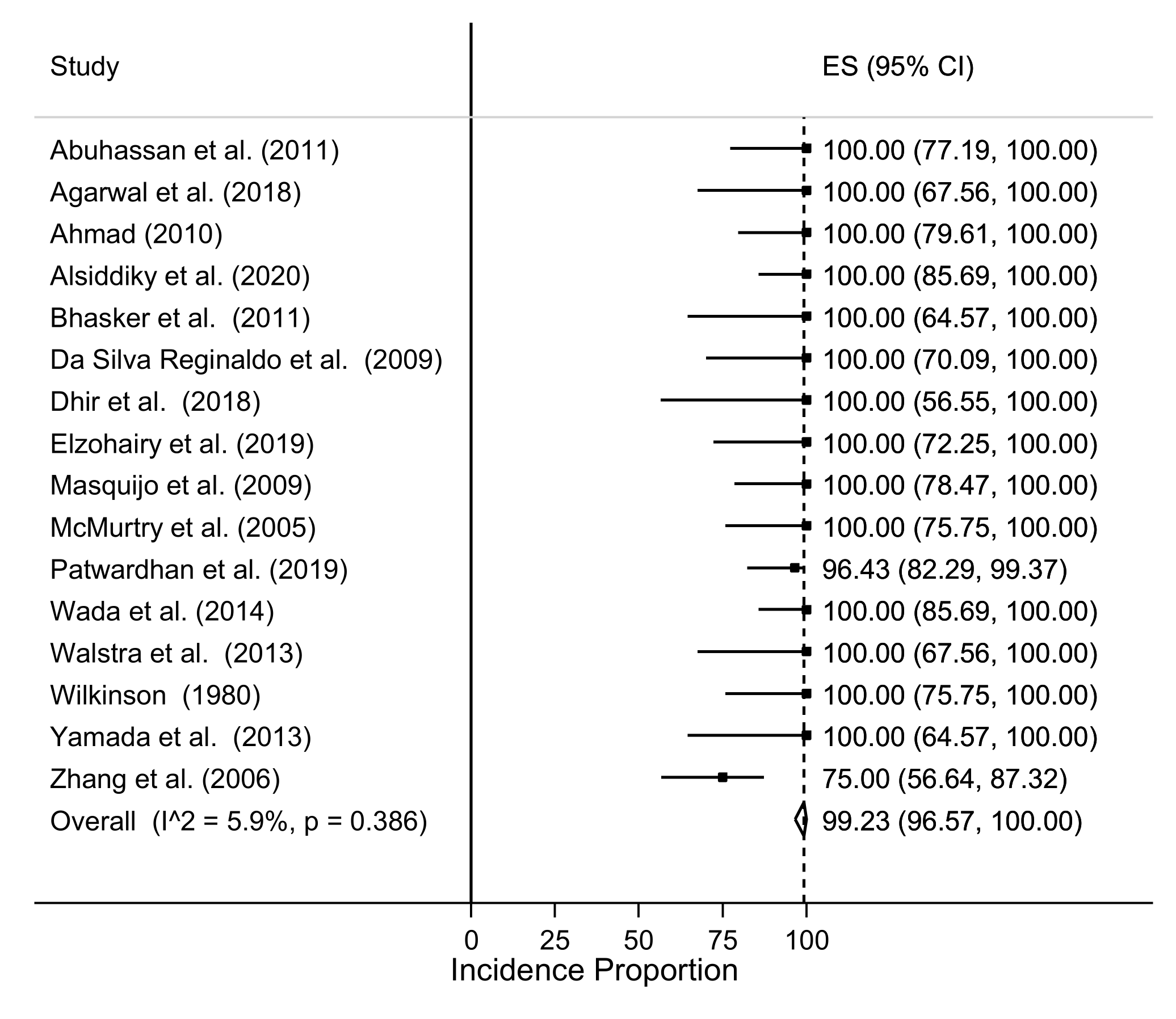
3.5. Postoperative Assessment
3.6. Complications
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Harvey, E.J.; Bernstein, M.; Desy, N.M.; Saran, N.; Ouellet, J.A. Sprengel deformity: Pathogenesis and management. J. Am. Acad. Orthop. Surg. 2012, 20, 177–186. [Google Scholar] [CrossRef]
- Grogan, D.P.; Stanley, E.A.; Bobechko, W.P. The congenital undescended scapula. Surgical correction by the Woodward procedure. J. Bone Jt. Surg. Ser. B 1983, 65, 598–605. [Google Scholar] [CrossRef] [Green Version]
- Cavendish, M.E. Congenital elevation of the scapula. J. Bone Jt. Surg. Br. Vol. 1972, 54, 395–408. [Google Scholar] [CrossRef]
- Eulenberg, M. Beitrag zue Dislocation der Scapula. Amtl. Ber. Uber Die Versamml. Dtsch. Nat. Und Aerzte Fur Die Jahre 1863, 37, 291–294. [Google Scholar]
- Willett, A.; Walsham, W.J. An Account of the Dissection of the Parts Removed after Death from the Body of a Woman the Subject of Congenital Malformation of the Spinal Column, Bony Thorax, and Left Scapular Arch; with Remarks on the Probable Nature of the Defects in Development Producing the Deformities. J. R. Soc. Med. 1880, MCT-63, 257–301. [Google Scholar] [CrossRef] [Green Version]
- Willett, A.; Walsham, W.J. A Second Case of Malformation of the Left Shoulder-Girdle; removal of the abnormal portion of bone; with remarks on the probable nature of the deformity. Med. Chir. Trans. 1883, 66, 145–158. [Google Scholar] [CrossRef]
- Sprengel, R. Die angeborene Verschiebung der Schulterblattes nach oben. Arch. Fur Klin. Chir. 1891, 42, 545–549. [Google Scholar]
- Greenberg, L.M. Sprengel’s Deformity. Ann. Paediatr. 1962, 198, 89–119. [Google Scholar]
- Öner, A.; Köksal, A.; Çimen, O.; Kargin, D.; Albayrak, A.; Akman, Y.E. Modified Woodward Technique for Sprengel Deformity and a Modification of the Cavendish Classification. J. Pediatr. Orthop. 2020, 40, 401–407. [Google Scholar] [CrossRef]
- Rigault, P.; Pouliquen, J.; Guyonvarch, G.; Zujovic, J. Congenital elevation of the scapula in children: Anatomopathological and therapeutic study apropos of 27 cases [French]. Rev. Chir. Orthop. Reparatrice Appar. Mot. 1976, 62, 5–26. [Google Scholar] [PubMed]
- Bhatia, D.N.; Kadavkolan, A.S.; DasGupta, B.; Bhosale, P.B. Sprengel’s deformity of the shoulder: Current perspectives in management. Int. J. Shoulder Surg. 2011, 5, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Herring, J.A.; Tachdjian, M.O. Texas Scottish Rite Hospital for Children. In Tachdjian’s Pediatric Orthopaedics from the Texas Scottish Rite Hospital for Children, 4th ed.; Saunders/Elsevier: Philadelphia, PA, USA, 2008. [Google Scholar]
- Sulamaa, M.; Wallgren, G.R. Congenital high scapula (sprengels deformity). Acta Orthop. 1954, 24, 195–206. [Google Scholar] [CrossRef]
- Wada, A.; Nakamura, T.; Fujii, T.; Takamura, K.; Yanagida, H.; Yamaguchi, T.; Kubota, H.; Oketani, Y. Sprengel deformity: Morphometric assessment and surgical treatment by the modified green procedure. J. Pediatr. Orthop. 2014, 34, 55–62. [Google Scholar] [CrossRef] [Green Version]
- Andrault, G.; Salmeron, F.; Laville, J.M. Green’s surgical procedure in Sprengel’s deformity: Cosmetic and functional results. Orthop. Traumatol. Surg. Res. 2009, 95, 330–335. [Google Scholar] [CrossRef] [Green Version]
- Ashok, A.; James, D.; Gahukamble, A.; Palocaren, T.; Madhuri, V. Modified Woodward’s procedure confers functional improvement in Sprengel’s deformity. J. Pediatr. Orthop. B 2020, 30, 585–592. [Google Scholar] [CrossRef]
- Alsiddiky, A.M.; Rafiq, Z.; Bakarman, K.A.; Alhuzaimi, F.S.; Asif, M. A Novel Modification of Woodward Procedure for Correction of Sprengel Deformity by Application of Anchoring Sutures. Indian J. Orthop. 2021, 55, 189–198. [Google Scholar] [CrossRef] [PubMed]
- Mears, D.C. Partial resection of the scapula and a release of the long head of triceps for the management of Sprengel’s deformity. J. Pediatr. Orthop. 2001, 21, 242–245. [Google Scholar] [CrossRef]
- Masquijo, J.J.; Bassini, O.; Paganini, F.; Goyeneche, R.; Miscione, H. Congenital elevation of the scapula: Surgical treatment with mears technique. J. Pediatr. Orthop. 2009, 29, 269–274. [Google Scholar] [CrossRef]
- Zhang, Z.M.; Zhang, J.; Lu, M.L.; Cao, G.L.; Dai, L.Y. Partial scapulectomy for congenital elevation of the scapula. Clin. Orthop. Relat. Res. 2007, 457, 171–175. [Google Scholar] [CrossRef]
- Dhir, R.; Chin, K.; Lambert, S. The congenital undescended scapula syndrome: Sprengel and the cleithrum: A case series and hypothesis. J. Shoulder Elb. Surg. 2018, 27, 252–259. [Google Scholar] [CrossRef]
- Konig, F. Operationsverfahren bei angeborenem Schulterblatthochstand. Zbl. Chir. 1913, 40, 1186–1187. [Google Scholar]
- Greitemann, B.; Rondhuis, J.J.; Karbowski, A. Treatment of congenital elevation of the scapula: 10 (2–18) year follow-up of 37 cases of sprengel’s deformity. Acta Orthop. 1993, 64, 365–368. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Prisma Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [Green Version]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Dodwell, E.R.; Pathy, R.; Widmann, R.F.; Green, D.W.; Scher, D.M.; Blanco, J.S.; Doyle, S.M.; Daluiski, A.; Sink, E.L. Reliability of the Modified Clavien-Dindo-Sink Complication Classification System in Pediatric Orthopaedic Surgery. JBJS Open Access 2018, 3, e0020. [Google Scholar] [CrossRef]
- Gummesson, C.; Atroshi, I.; Ekdahl, C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: Longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet. Disord. 2003, 4, 11. [Google Scholar] [CrossRef] [Green Version]
- Beaton, D.; Richards, R.R. Assessing the reliability and responsiveness of 5 shoulder questionnaires. J. Shoulder Elb. Surg. 1998, 7, 565–572. [Google Scholar] [CrossRef]
- Gates, P.; Campbell, S. Effects of age, sex, and comorbidities on the pediatric outcomes data collection instrument (PODCI) in the general population. J. Pediatr. Orthop. 2015, 35, 203–209. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2000. Available online: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 25 November 2021).
- Coleman, B.D.; Khan, K.M.; Maffulli, N.; Cook, J.L.; Wark, J.D. Studies of surgical outcome after patellar tendinopathy: Clinical significance of methodological deficiencies and guidelines for future studies. Scand. J. Med. Sci. Sports 2000, 10, 2–11. [Google Scholar] [CrossRef]
- Farsetti, P.; Weinstein, S.L.; Caterini, R.; de Maio, F.; Ippolito, E. Sprengel’s deformity: Long-term follow-up study of 22 cases. J. Pediatric Orthop. B 2003, 12, 202–210. [Google Scholar] [CrossRef]
- Carson, W.G. Congenital Elevation of the Scapula. J. Bone Jt. Surg. 1981, 63, 1199–1207. [Google Scholar] [CrossRef]
- Leibovic, S.J.L. Sprengel Deformity. J. Bone Jt. Surg. 1990, 72, 192–197. [Google Scholar] [CrossRef]
- Abuhassan, F.O. Subperiosteal resection of mid-clavicle in Sprengel’s deformity correction. Strateg. Trauma Limb Reconstr. 2011, 6, 59–67. [Google Scholar] [CrossRef] [Green Version]
- Agarwal, A.; Arkesh, M.; Jandial, G. Sprengel’s deformity correction by vertical scapular osteotomy in a paediatric age group: Influence of rib cage abnormalities. Int. Orthop. 2018, 42, 2191–2197. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, A.A. Surgical correction of severe sprengel deformity to allow greater postoperative range of shoulder abduction. J. Pediatr. Orthop. 2010, 30, 575–581. [Google Scholar] [CrossRef]
- Aslani, M.A.; Mirzaee, F.; Baradaran, A.F.; Ziaei, M.E.; Zafarani, Z.; Aslani, H. Results of surgical treatment for Sprengle’s deformity with vertical corrective scapular osteotomy. Ann. Med. Surg. 2020, 54, 32–36. [Google Scholar] [CrossRef] [PubMed]
- Aydinli, U.; Ozturk, C.; Akesen, B.; Ozer, O. Surgical treatment of Sprengel’s deformity: A modified Green procedure. Acta Orthop. Belg. 2005, 71, 264–268. [Google Scholar]
- Bellemans, M.; Lamoireux, J. Results of surgical treatment of Sprengel deformity by a modified Green’s procedure. J. Pediatr. Orthop. B 1999, 8, 194–196. [Google Scholar] [CrossRef] [PubMed]
- Bhasker, A.R.; Khullar, S.; Habeeb, M. Outcome of Mears procedure for Sprengel’s deformity. Indian J. Orthop. 2011, 45, 132–135. [Google Scholar] [CrossRef]
- Borges, J.L.P.; Shah, A.; Torres, B.C.; Bowen, J.R. Modified Woodward procedure for sprengel deformity of the shoulder: Long-term results. J. Pediatr. Orthop. 1996, 16, 508–513. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.; Farahvar, H. Surgery of the clavicle in Sprengle’s deformity. Clin. Orthop. Relat. Res. 1976, 116, 138–141. [Google Scholar]
- da Reginaldo, S.; de Macedo, R.R.; da Amaral, R.; Cardoso, A.L.P.; Araújo, H.R.S.; Daher, S. Sprengel’S Deformity: Surgical Correction By a Modified Green Procedure. Rev. Bras. Ortop. 2009, 44, 208–213. [Google Scholar] [CrossRef] [Green Version]
- di Gennaro, G.L.; Fosco, M.; Spina, M.; Donzelli, O. Surgical treatment of Sprengel’s shoulder. J. Bone Jt. Surg. Ser. B 2012, 94, 709–712. [Google Scholar] [CrossRef] [PubMed]
- Elzohairy, M.M.; Salama, A.M. Sprengel’s deformity of the shoulder joint treated by Woodward operation. Eur. J. Orthop. Surg. Traumatol. 2019, 29, 37–45. [Google Scholar] [CrossRef]
- Gonen, E.; Simsek, U.; Solak, S.; Bektaser, B.; Ates, Y.; Aydin, E. Long-term results of modified Green method in Sprengel’s deformity. J. Child. Orthop. 2010, 4, 309–314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jiang, Y.; Guo, Y.; Zhu, Z.; Wang, Y. Surgical management of Sprengel’s deformity by a modification of Green’s procedure: A single center experience. Orthopade 2020, 49, 255–259. [Google Scholar] [CrossRef] [PubMed]
- Jindal, N.; Gupta, P. Sprengel’s shoulder treated by the Woodward procedure: Analysis of factors affecting functional and cosmetic outcome. J. Child. Orthop. 2012, 6, 291–296. [Google Scholar] [CrossRef] [Green Version]
- Khairouni, A. Congenital high scapula. Acta Orthop. Scand. 1955, 24, 195–206. [Google Scholar] [CrossRef]
- Klisić, P.; Filipović, M.; Uzelac, O.; Milinković, Z. Relocation of congenitally elevated scapula. J. Pediatr. Orthop. 1981, 1, 43–45. [Google Scholar] [CrossRef]
- McMurtry, I.; Bennet, G.C.; Bradish, C. Osteotomy for congenital elevation of the scapula (Sprengel’s deformity). J. Bone Jt. Surg. Ser. B 2005, 87, 986–989. [Google Scholar] [CrossRef]
- Naik, P.; Chauhan, H. Functional improvement in patients with Sprengel’s deformity following Modified Green’s procedure and simplified clavicle osteotomy—A study of forty cases. Int. Orthop. 2020, 44, 2653–2663. [Google Scholar] [CrossRef]
- Nakamura, N.; Inaba, Y.; Machida, J.; Saito, T. Use of glenoid inclination angle for the assessment of unilateral congenital high scapula. J. Pediatr. Orthop. Part B 2016, 25, 54–61. [Google Scholar] [CrossRef] [PubMed]
- Patwardhan, S.; Sodhai, V.; Gugale, S.; Sancheti, P.; Shyam, A. Surgical correction of Sprengel’s deformity by modified Woodward procedure: Outcomes in twenty eight patients. Int. Orthop. 2020, 44, 1143–1151. [Google Scholar] [CrossRef]
- Siu, K.K.; Ko, J.Y.; Huang, C.C.; Wang, F.S.; Chen, J.M.; Wong, T. Woodward procedure improves shoulder function in sprengel deformity. Chang. Gung Med. J. 2011, 34, 403–409. [Google Scholar]
- Vuillermin, C.; Wang, K.K.; Williams, K.A.; Hresko, M.T.; Waters, P.M. Sprengel’s deformity: An analysis of surgically and nonsurgically treated patients. J. Shoulder Elb. Surg. 2021, 30, e1–e9. [Google Scholar] [CrossRef]
- Walstra, F.E.; Alta, T.D.; van der Eijken, J.W.; Willems, W.J.; Ham, S.J. Long-term follow-up of Sprengel’s deformity treated with the Woodward procedure. J. Shoulder Elb. Surg. 2013, 22, 752–759. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, J.A. Scapular osteotomy for sprengel’s shoulder. J. Bone Jt. Surg. 1980, 62, 486–490. [Google Scholar] [CrossRef]
- Yamada, K.; Suenaga, N.; Iwasaki, N.; Oizumi, N.; Minami, A.; Funakoshi, T. Correction in malrotation of the scapula and muscle transfer for the management of severe sprengel deformity: Static and dynamic evaluation using 3-dimensional computed tomography. J. Pediatr. Orthop. 2013, 33, 205–211. [Google Scholar] [CrossRef] [PubMed]
- Hwang, J.H.; Kim, H.W.; Lee, D.H.; Chung, J.H.; Park, H. One-stage rotational osteotomy for congenital radioulnar synostosis. J. Hand Surg. Eur. Vol. 2015, 40, 855–861. [Google Scholar] [CrossRef]
- Kim, J.K.; Cho, T.J.; Lee, K.; Moon, H.J.; Park, M.S.; Yoo, W.J.; Chung, C.Y.; Choi, I.H. Atlantoaxial rotatory subluxation after surgical relocation of Sprengel deformity: A case report. J. Pediatr. Orthop. Part B 2012, 21, 276–279. [Google Scholar] [CrossRef]
- Satsuma, S.; Yamamoto, T.; Kobayashi, D.; Yoshiya, S.; Marui, T.; Akisue, T.; Hitora, T.; Nagira, K.; Ohta, R.; Kurosaka, M. Extraabdominal desmoid tumor in a surgical scar of a patient with Sprengel’s deformity. J. Pediatr. Surg. 2003, 38, 1540–1542. [Google Scholar] [CrossRef]
- Senes, F.M.; Calevo, M.G.; Adani, R.; Baldrighi, C.; Bassetto, F.; Corain, M.; Landi, A.; Lando, M.; Monticelli, A.; Novelli, C.; et al. Hand and Upper Limb Malformations in Italy: A Multicentric Study. J. Hand Surg. Asian Pac. 2021, 26, 345–350. Available online: https://med.papers.bar/paper/34380395 (accessed on 21 October 2021). [CrossRef] [PubMed]
- Ekblom, A.G.; Laurell, T.; Arner, M. Epidemiology of congenital upper limb anomalies in Stockholm, Sweden, 1997 to 2007: Application of the Oberg, Manske, and Tonkin classification. J. Hand Surg. Am. 2014, 39, 237–248. [Google Scholar] [CrossRef] [PubMed]



| No. of Cases | Newcastle–Ottawa Scale | Modified Coleman Methodology Score | |
|---|---|---|---|
| Alsiddiky et al. (2020) [17] | 23 | 6 | 57 |
| Abuhassan et al. (2011) [35] | 13 | 6 | 52 |
| Agarwal et al. (2018) [36] | 8 | 6 | 54 |
| Ahmad (2010) [37] | 11 | 6 | 57 |
| Andrault et al. (2009) [15] | 6 | 6 | 49 |
| Ashok et al. (2020) [16] | 14 | 8 | 47 |
| Aslani et al. (2020) [38] | 31 | 6 | 61 |
| Aydinli et al. (2005) [39] | 12 | 6 | 51 |
| Bellemans (1999) [40] | 7 | 6 | 57 |
| Bhasker et al. (2011) [41] | 7 | 8 | 51 |
| Borges et al. (1996) [42] | 16 | 6 | 52 |
| Carson (1981) [33] | 11 | 6 | 43 |
| Chung et al. (1976) [43] | 5 | 6 | 42 |
| Da Silva Reginaldo et al. (2009) [44] | 9 | 6 | 46 |
| Dhir et al. (2018) [21] | 5 | 6 | 50 |
| Di Gennaro et al. (2012) [45] | 56 | 6 | 61 |
| Elzohairy et al. (2019) [46] | 10 | 6 | 54 |
| Farsetti et al. (2003) [32] | 8 | 6 | 44 |
| Gonen et al. (2010) [47] | 23 | 6 | 57 |
| Greitemann et al. (1993) [23] | 37 | 6 | 48 |
| Grogan et al. (1983) [2] | 13 | 6 | 58 |
| Jiang et al. (2019) [48] | 34 | 6 | 61 |
| Jindal et al. (2012) [49] | 12 | 6 | 54 |
| Khairouni (2002) [50] | 17 | 2 | 25 |
| Klisić et al. (1981) [51] | 28 | 2 | 45 |
| Leibovic (1990) [34] | 15 | 6 | 60 |
| Masquijo et al. (2009) [19] | 14 | 8 | 71 |
| McMurtry et al. (2005) [52] | 12 | 6 | 57 |
| Mears (2001) [18] | 8 | 6 | 57 |
| Naik et al. (2020) [53] | 40 | 6 | 61 |
| Nakamura et al. (2016) [54] | 14 | 6 | 57 |
| Öner et al. (2020) [9] | 17 | 6 | 55 |
| Patwardhan et al. (2019) [55] | 28 | 6 | 51 |
| Siu et al. (2011) [56] | 8 | 6 | 57 |
| Sulamaa et al. (1954) [13] | 4 | 6 | 44 |
| Vuillermin et al. (2020) [57] | 24 | 6 | 46 |
| Wada et al. (2014) [14] | 22 | 6 | 54 |
| Walstra et al. (2013) [58] | 7 | 8 | 60 |
| Wilkinson (1980) [59] | 12 | 6 | 54 |
| Yamada et al. (2013) [60] | 7 | 6 | 54 |
| Zhang et al. (2006) [20] | 26 | 6 | 58 |
| Factor | Level | Value |
|---|---|---|
| No. of patients | 236 | |
| Study | Abuhassan et al. (2011) [35] | 13 (5.5%) |
| Agarwal et al. (2018) [36] | 8 (3.4%) | |
| Ahmad (2010) [37] | 15 (6.4%) | |
| Alsiddiky et al. (2020) [17] | 23 (9.7%) | |
| Andrault et al. (2009) [15] | 6 (2.5%) | |
| Bhasker et al. (2011) [41] | 7 (3.0%) | |
| Da Silva Reginaldo et al. (2009) [44] | 9 (3.8%) | |
| Dhir et al. (2018) [21] | 5 (2.1%) | |
| Elzohairy et al. (2019) [46] | 10 (4.2%) | |
| Farsetti et al. (2003) [32] | 8 (3.4%) | |
| Masquijo et al. (2009) [19] | 14 (5.9%) | |
| McMurtry et al. (2005) [52] | 12 (5.1%) | |
| Patwardhan et al. (2019) [55] | 28 (11.9%) | |
| Wada et al. (2014) [14] | 23 (9.7%) | |
| Walstra et al. (2013) [58] | 8 (3.4%) | |
| Wilkinson (1980) [59] | 12 (5.1%) | |
| Yamada et al. (2013) [60] | 7 (3.0%) | |
| Zhang et al. (2006) [20] | 28 (11.9%) | |
| Period of treatment | <1990 | 12 (5.1%) |
| 2000–2009 | 77 (32.6%) | |
| ≥2010 | 147 (62.3%) | |
| Age at treatment (mean in years), median (IQR) | 6 (4.7) | |
| Surgical technique | Green/Schrock | 71 (30.1%) |
| Mears | 21 (8.9%) | |
| Osteotomy | 32 (13.6%) | |
| Resection | 35 (14.8%) | |
| Woodward | 77 (32.6%) | |
| Cavendish classification | 2 | 31 (14.0%) |
| 3 | 137 (62.0%) | |
| 4 | 53 (24.0%) | |
| Rigault classification | 2 | 41 (43%) |
| 3 | 54 (57%) |
| Grade | Green/Schrock | Woodward | Osteotomy | Resection | Mears | |
|---|---|---|---|---|---|---|
| Preoperative Cavendish’s score | 2 | 0 (0%) | 14 (18%) | 4 (13%) | 11 (33%) | 2 (10%) |
| 3 | 38 (63%) | 42 (55%) | 27 (84%) | 16 (48%) | 15 (71%) | |
| 4 | 22 (37%) | 20 (26%) | 1 (3%) | 6 (18%) | 4 (19%) | |
| Postoperative Cavendish’s score | 1 | 31 (52%) | 41 (54%) | 19 (59%) | 14 (42%) | 17 (81%) |
| 2 | 24 (40%) | 33 (43%) | 12 (38%) | 15 (45%) | 4 (19%) | |
| 3 | 5 (8%) | 2 (3%) | 1 (3%) | 4 (12%) | 0 (0%) | |
| Preoperative Rigault’s score | 2 | 6 (18%) | 18 (46%) | 7 (88%) | 5 (71%) | 5 (71%) |
| 3 | 28 (82%) | 21 (54%) | 1 (13%) | 2 (29%) | 2 (29%) | |
| Postoperative Rigault’s score | 1 | 26 (76%) | 28 (72%) | 1 (13%) | 4 (57%) | |
| 2 | 8 (24%) | 11 (28%) | 7 (88%) | 2 (29%) | ||
| 3 | 0 (0%) | 0 (0%) | 0 (0%) | 1 (14%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zarantonello, P.; Di Gennaro, G.L.; Todisco, M.; Cataldi, P.; Stallone, S.; Evangelista, A.; Ferrari, D.; Antonioli, D.; Trisolino, G. Surgical Treatment of Sprengel’s Deformity: A Systematic Review and Meta-Analysis. Children 2021, 8, 1142. https://doi.org/10.3390/children8121142
Zarantonello P, Di Gennaro GL, Todisco M, Cataldi P, Stallone S, Evangelista A, Ferrari D, Antonioli D, Trisolino G. Surgical Treatment of Sprengel’s Deformity: A Systematic Review and Meta-Analysis. Children. 2021; 8(12):1142. https://doi.org/10.3390/children8121142
Chicago/Turabian StyleZarantonello, Paola, Giovanni Luigi Di Gennaro, Marco Todisco, Piergiorgio Cataldi, Stefano Stallone, Andrea Evangelista, Daniele Ferrari, Diego Antonioli, and Giovanni Trisolino. 2021. "Surgical Treatment of Sprengel’s Deformity: A Systematic Review and Meta-Analysis" Children 8, no. 12: 1142. https://doi.org/10.3390/children8121142
APA StyleZarantonello, P., Di Gennaro, G. L., Todisco, M., Cataldi, P., Stallone, S., Evangelista, A., Ferrari, D., Antonioli, D., & Trisolino, G. (2021). Surgical Treatment of Sprengel’s Deformity: A Systematic Review and Meta-Analysis. Children, 8(12), 1142. https://doi.org/10.3390/children8121142







