The Effectiveness of an Integrated Treatment for Functional Speech Sound Disorders—A Randomized Controlled Trial
Abstract
1. Introduction
1.1. Developmental Speech Sound Disorders
1.2. Evidence for Treatment Effects in SSD
1.3. New Treatment Concepts for SSD
1.4. Efficacy vs. Effectiveness Studies and the Need for Precise Description of Interventions
1.5. Aim of the Study
2. Materials and Methods
2.1. Treatment Procedure of PhonoSens
2.1.1. Steps of the PhonoSens Treatment
Phonological Encoding—Treatment Step 1: Categorical Phonological Perception
Motor Planning—Treatment Step 2: Phoneme Acquirement
Motor Programming—Treatment Step 3: Articulatory Fine-Tuning I
Motor Execution—Treatment Step 4: Articulatory Fine-Tuning II
Treatment Step 5: Enhanced Auditory Self-Monitoring
Treatment Step 6: Assisted Generalization
Sensorimotor Feedback—Thermal Tactile Oral Stimulation (TTOS)
Treatment Dose and Division
2.2. Participants
2.3. Data Collection
Time Course of Critical Target Testing
2.4. Therapists
2.5. Outcome Measures, Statistical Analyses
3. Results
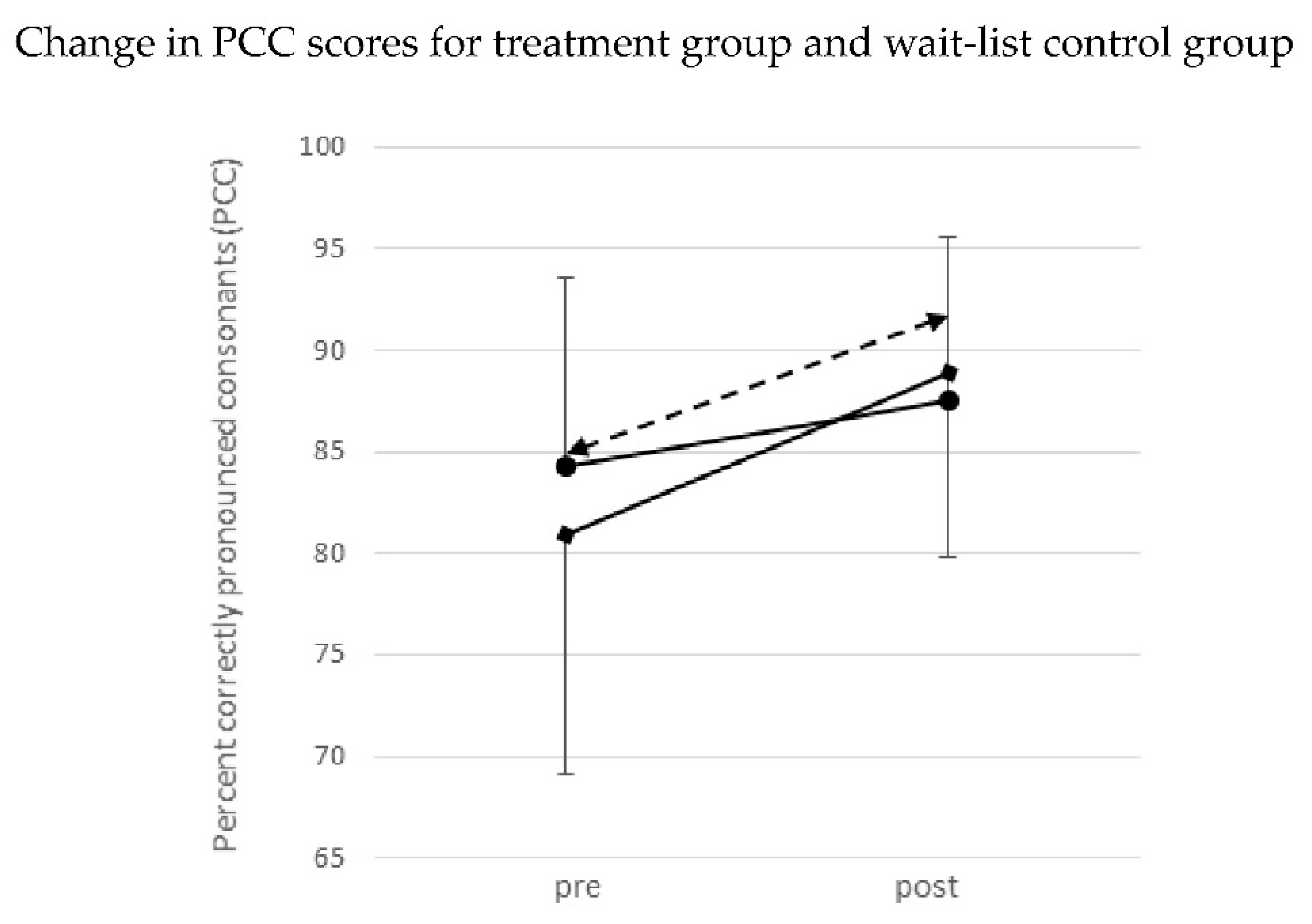
3.1. Scores for Percentage of Correct Consonants (PCC)
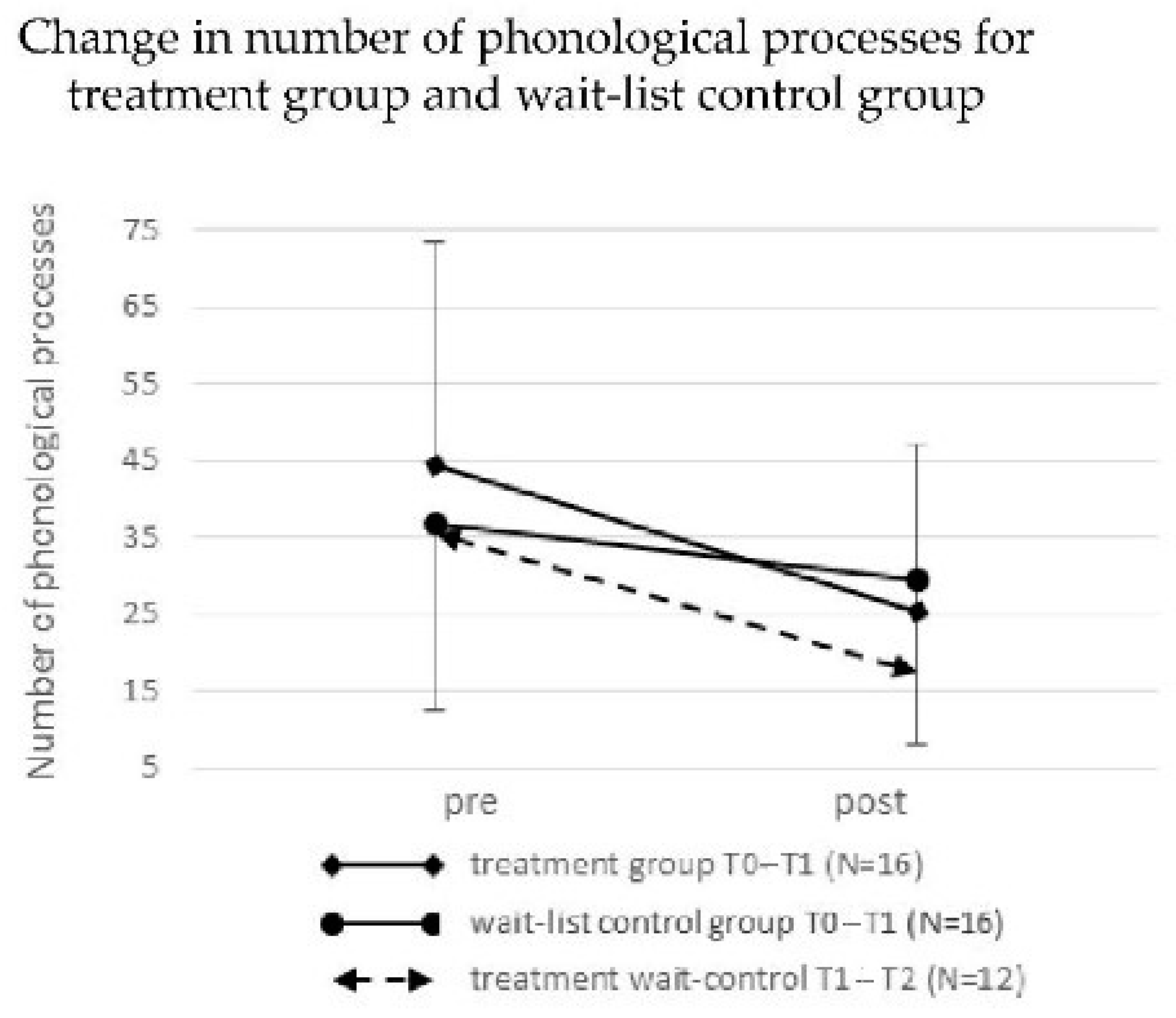
3.2. Number of Phonological Processes
3.3. Spontaneous Improvements of Misarticulated Phonemes
3.4. Reaching Success Criterion
3.5. Inter-Rater Agreement
3.6. Age, Gender, Parental Educational Level, and Treatment Success
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. ICD-11 International Classification of Diseases 11th Revision. Available online: https://icd.who.int/en/ (accessed on 19 June 2021).
- Felsenfeld, S.; Broen, P.A.; McGue, M. A 28-year follow-up of adults with a history of moderate phonological disorder: Educational and occupational results. J. Speech Hear. Res. 1994, 37, 1341–1353. [Google Scholar] [CrossRef] [PubMed]
- McCormack, J.; McLeod, S.; McAllister, L.; Harrison, L.J. A systematic review of the association between childhood speech impairment and participation across the lifespan. Int. J. Speech Lang. Pathol. 2009, 11, 155–170. [Google Scholar] [CrossRef]
- Von Suchodoletz, W. Wie wirksam ist Sprachtherapie? [How effective is speech therapy?]. Kindh. Und Entwickl. 2009, 18, 213–221. [Google Scholar] [CrossRef]
- Wren, Y.; Miller, L.L.; Peters, T.J.; Emond, A.; Roulstone, S. Prevalence and predictors of persistent speech sound disorder at eight years old: Findings from a population cohort study. J. Speech Lang. Hear. Res. 2016, 59, 647–673. [Google Scholar] [CrossRef]
- Broomfield, J.; Dodd, B. Children with speech and language disability: Caseload characteristics. Int. J. Lang. Commun. Disord. 2004, 39, 303–324. [Google Scholar] [CrossRef] [PubMed]
- Campbell, T.F.; Dollaghan, C.A.; Rockette, H.E.; Paradise, J.L.; Feldman, H.M.; Shriberg, L.D.; Sabo, D.L.; Kurs-Lasky, M. Risk factors for speech delay of unknown origin in 3-year-old children. Child Dev. 2003, 74, 346–357. [Google Scholar] [CrossRef]
- Fox-Boyer, A.V.; Glück, C.W.; Elsing, C.E.; Siegmüller, J. Erwerb von Phonologie, Lexikon und Grammatik bei Kindern im Alter von 3; 0–5; 0 Jahren [Acquisition of phonology, lexicon, and grammar in 3- to 5-year-old children]. In Handbuch Spracherwerb und Sprachentwicklungsstörungen. Kindergartenphase [Handbook of Language Acquisition and Language Development Disorders. Kindergarten Phase]; Fox-Boyer, A., Ed.; Elsevier: München, Germany, 2014; pp. 3–23. ISBN 9783437445262. [Google Scholar]
- Shriberg, L.D.; Kwiatkowski, J. Self-monitoring and generalization in preschool speech-delayed children. Lang. Speech Hear. Serv. Sch. 1990, 21, 157–170. [Google Scholar] [CrossRef][Green Version]
- Van Borsel, J. Basisbegrippen Logopedie, Deel 2: Communicatiestoornissen [Basic Concepts of Speech Therapy, Part 2: Communication Disorders], 3rd ed.; Acco Nederland: Den Haag, The Netherlands, 2019; ISBN 978-90-334-7645-7. [Google Scholar]
- Weggemans, M. Jaarverslag Logopedie 2004–2005 [Annual Report Speech Therapy 2004–2005]; GGD Groningen: Groningen, The Netherlands, 2005. [Google Scholar]
- Waltersbacher, A.; WIdO—Institut der AOK. Heilmittelbericht 2019 Ergotherapie, Sprachtherapie Physiotherapie, Podologie. [Cure Report: Occupational Therapy Speech Therapy Physiotherapy Podiatry]; Berlin, Germany, 2019. Available online: https://www.wido.de/fileadmin/Dateien/Dokumente/Publikationen_Produkte/Buchreihen/Heilmittelbericht/wido_hei_hmb_2019.pdf (accessed on 19 March 2020).
- American Speech-Language-Hearing Association (n.d.) Speech sound disorders: Articulation and phonology. (Practice Portal). Available online: www.asha.org/Practice-Portal/Clinical-Topics/Articulation-and-Phonology (accessed on 12 September 2020).
- Gironda, F.; Fabus, R. Assessment of articulation and phonological disorders. In A Guide to Clinical Assessment and Professional Report Writing in Speech-Language Pathology; Stein, C., Fabus, R., Eds.; Delmar Publications: New York, NY, USA, 2011; pp. 140–176. ISBN 978-1-4354-8532-7. [Google Scholar]
- Fox-Boyer, A.V. Kindliche Aussprachestörungen [Speech Sound Disorders in Children], 7th ed.; Schulz-Kirchner: Idstein, Germany, 2016; ISBN 978-3-8248-1160-1. [Google Scholar]
- Wertzner, H.; Amaro, L.; Teramoto, S.S. Severity of phonological disorders: Perceptual judgement and percentage of correct consonants. Pró Fono Rev. De Atualizaçã Científica 2005, 17, 185–194. [Google Scholar] [CrossRef]
- Law, J.; Garrett, Z.; Nye, C. The efficacy of treatment for children with developmental speech and language delay disorder: A meta-analysis. J. Speech Lang. Hear. Res. 2004, 47, 924–943. [Google Scholar] [CrossRef]
- Nelson, H.D.; Nygren, P.; Walker, M.; and Panoscha, R. Screening for speech and language delay in preschool children: Systematic evidence review for the US Preventive Services Task Force. Pediatrics 2006, 117, e298–e319. [Google Scholar] [CrossRef]
- Glogowska, M.; Roulstone, S.; Enderby, P.; Peters, T.J. Randomized controlled trial of community based speech and language therapy in preschool children. Br. Med. J. 2000, 321, 923. [Google Scholar] [CrossRef]
- Almost, D.; Rosenbaum, P. Effectiveness of speech intervention for phonological disorders: A randomized controlled trial. Dev. Med. Child Neurol. 1998, 40, 319–325. [Google Scholar] [CrossRef]
- Wren, Y.; Harding, S.; Goldbart, J.; Roulstone, S. A systematic review and classification of interventions for speech-sound disorder in preschool children. Int. J. Commun. Disord. 2018, 53, 446–467. [Google Scholar] [CrossRef]
- Rvachew, S.; Nowak, M.; Cloutier, G. Effect of phonemic perception training on the speech production and phonological awareness skill of children with expressive phonological delay. Am. J. Speech Lang. Pathol. 2004, 13, 250–263. [Google Scholar] [CrossRef]
- Weiner, F.F. Treatment of phonological disability using the method of meaningful minimal contrast: Two case studies. J. Speech Hear. Disord. 1981, 46, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Baker, E.; McLeod, S. Evidence-Based practice for children with speech sound disorders: Part 1 Narrative Review. Lang. Speech Hear. Serv. Sch. 2011, 42, 102–139. [Google Scholar] [CrossRef]
- Yoder, P.; Camarata, S.; Gardner, E. Treatment effects on speech intelligibility and length of utterance in children with specific language and intelligibility impairments. J. Early Interv. 2005, 28, 34–49. [Google Scholar] [CrossRef]
- Howell, J.; Dean, E.C. Treating Phonological Disorders in Children: Metaphon Theory to Practice, 2nd ed.; Whurr: London, UK, 2004. [Google Scholar]
- Dodd, B.; Holm, A.; Crosbie, S.; McIntosh, B. Core vocabulary intervention. In Interventions for Speech Sound Disorders in Children; Williams, A.-L., McLeod, S., McCauly, R., Eds.; P. H. Brookes: Baltimore, MD, USA, 2010; pp. 117–118. ISBN -978-1-5985-7018-2. [Google Scholar]
- Crosbie, S.; Holm, A.; Dodd, B. Intervention for children with severe speech disorder: A comparison of two approaches. Int. J. Lang. Comm. Dis. 2005, 40, 467–491. [Google Scholar] [CrossRef]
- Pamplona, M.C.; Ysunza, A.; Espinosa, J. A comparative trial of two modalities of speech intervention for compensatory articulation in cleft palate children, phonological approach versus articulatory approach. Int. J. Pediatric Otorhinolaryngol. 1999, 49, 21–26. [Google Scholar] [CrossRef]
- Lousada, M.; Jesus, L.; Capelas, S.; Margaça, C.; Tomé, D.; Valente, R.; Hall, A.; Joffe, V. Phonological and articulation treatment approaches in Portuguese children with speech and language impairments: A randomized controlled intervention study. Int. J. Lang. Commun. Disord. R. Coll. Speech Lang. Ther. 2013, 48, 172–187. [Google Scholar] [CrossRef]
- Dodd, B.; Bradford, A. A comparison of three therapy methods for children with different types of developmental phonological disorder. Int. J. Lang. Commun. Disord. 2000, 35, 189–209. [Google Scholar] [CrossRef] [PubMed]
- Terband, H.; Maassen, B.; Maas, E.A. Psycholinguistic framework for diagnosis and treatment planning of developmental speech disorders. Folia Phoniatr. Logop. 2019, 71, 216–227. [Google Scholar] [CrossRef] [PubMed]
- Dodd, B. Differential diagnosis of pediatric speech sound disorder. Curr. Dev. Disord. Rep. 2014, 1, 189–196. [Google Scholar] [CrossRef]
- Dworkin, J.P.; Marunick, M.T.; Krouse, J.H. Velopharyngeal dysfunction: Speech characteristics, variable etiologies, evaluation techniques, and differential treatments. Lang. Speech Hear. Serv. Sch. 2004, 35, 333–352. [Google Scholar] [CrossRef] [PubMed]
- Kummer, A.W.; Marty-Grames, L.; Jones, D.L.; Kurnell, M.P.; Ruscello, D. Response to “velopharyngeal dysfunction: Speech characteristics, variable etiologies, evaluation techniques, and differential treatments” by Dworkin, Marunick, and Krouse, October 2004. Lang. Speech Hear. Serv. Sch. 2006, 37, 236–238, author reply 239–243. [Google Scholar] [CrossRef]
- Namasivayam, A.K.; Coleman, D.; O’Dwyer, A.; van Lieshout, P. Speech sound disorders in children: An articulatory phonology perspective. Front. Psychol. 2020, 10, 2998. [Google Scholar] [CrossRef]
- Van Lieshout, P. Dynamical systems theory and its application in speech. In Speech Motor Control in Normal and Disordered Speech; Maassen, B., Kent, R., Herman, P., van Lieshout, P., Woulter, H., Eds.; Oxford University Press: Oxford, UK, 2004; pp. 51–82. ISBN 978-2889639281. [Google Scholar]
- Namasivayam, A.K.; van Lieshout, P. Speech motor skill and stuttering. J. Motor. Behav. 2011, 43, 477–489. [Google Scholar] [CrossRef]
- Furlong, L.M.; Morris, M.E.; Serry, T.A.; Erickson, S. Treating childhood speech sound disorders: Current approaches to management by Australian speech-language pathologists. Lang. Speech Hear. Serv. Sch. 2021, 52, 581–596. [Google Scholar] [CrossRef]
- Guenther, F.H. A neural network model of speech acquisition and motor equivalent speech production. Biol. Cybern. 1994, 72, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Guenther, F.; Perkell, J. A new model of speech production and its application to studies of the role of auditory feedback in speech. In Speech Motor Control in Normal and Disordered Speech; Maassen, B., Kent, R., Peters, H.F.M., van Lieshout, P., Hulstijn, W., Eds.; Oxford University Press: Oxford, UK, 2004; pp. 29–50. ISBN 978-0198526261. [Google Scholar]
- Tourville, J.A.; Guenther, F.H. The DIVA model: A neural theory of speech acquisition and production. Lang. Cogn. Process. 2011, 26, 952–981. [Google Scholar] [CrossRef]
- Levelt, W.J.; Roelofs, A.; Meyer, A.S. A theory of lexical access in speech production. Behav. Brain Sci. 1999, 22, 1–38. [Google Scholar] [CrossRef]
- Kühnert, B.; Nolan, F. The origin of coarticulation. In Coarticulation. Theory, Data and Techniques; Hardcastle, W.J., Hewlett, N., Eds.; Cambridge University Press: New York, NY, USA, 1999; pp. 7–30. ISBN 9780521029858. [Google Scholar]
- Özdemir, R.; Roelofs, A.; Levelt, W.J. Perceptual uniqueness point effects in monitoring internal speech. Cognition 2007, 105, 457–465. [Google Scholar] [CrossRef][Green Version]
- Koegel, L.K.; Koegel, R.L.; Costello Ingham, J. Programming rapid generalization of correct articulation through self-monitoring procedures. J. Speech Hear. Disord. 1986, 51, 24–32. [Google Scholar] [CrossRef]
- Wolfe, V.; Presley, C.; Mesaris, J. The importance of sound identification training in phonological intervention. Am. J. Speech-Lang. Pathol. 2003, 12, 282–288. [Google Scholar] [CrossRef]
- Gierut, J.A.; Champion, A.H. Syllable onsets II: Three-element clusters in phonological treatment. J. Speech Lang. Hear. Res. 2001, 44, 886–904. [Google Scholar] [CrossRef]
- Storkel, H.L. The complexity approach to phonological treatment: How to select target phonemes. Lang. Speech Hear. Serv. Sch. 2018, 49, 463–481. [Google Scholar] [CrossRef]
- Cochrane, A.L. Effectiveness and Efficiency: Random Reflection on Health Services; Nuffield Provincial Hospitals Trust: London, UK, 1972. [Google Scholar]
- Haynes, B. Can it work? Does it work? Is it worth it? Br. Med. J. 1999, 319, 653–654. [Google Scholar] [CrossRef]
- Baker, E.; Williams, A.L.; McLeod, S.; McCauley, R. Elements of phonological interventions for children with speech sound disorders: The development of a taxonomy. Am. J. Speech Lang. Pathol. 2018, 27, 906–935. [Google Scholar] [CrossRef]
- Hesketh, A.; Adams, C.; Nightingale, C.; Hall, R. Phonological awareness therapy and articulatory training approaches for children with phonological disorders: A comparative outcome study. Int. J. Lang. Commun. Disord. 2000, 35, 337–354. [Google Scholar] [CrossRef]
- Fox, A.V. PLAKSS—Psycholinguistische Analyse Kindlicher Sprechstörungen [Psycholinguistic Analysis of Speech Sound Disorders in Childhood], 4th ed.; Pearson Assessment & Information GmbH: Frankfurt/Main, Germany, 2009. [Google Scholar]
- Möttönen, R.; Watkins, K.E. Motor representations of articulators contribute to categorical perception of speech sounds. J. Neurosci. 2009, 5, 9819–9825. [Google Scholar] [CrossRef]
- Rvachew, S.; Jamieson, D.G. Perception of voiceless fricatives by children with a functional articulation disorder. J. Speech Hear. Disord. 1989, 54, 193–208. [Google Scholar] [CrossRef]
- Teismann, I.K.; Steinsträter, O.; Warnecke, T.; Suntrup, S.; Ringelstein, E.B.; Pantev, C.; Dziewas, R. Tactile thermal oral stimulation increases the cortical representation of swallowing. BMC Neurosci. 2009, 10, 71. [Google Scholar] [CrossRef] [PubMed]
- Ito, T.; Tiede, M.; Ostry, D.J. Somatosensory function in speech perception. Proc. Natl. Acad. Sci. USA 2009, 106, 1245–1248. [Google Scholar] [CrossRef] [PubMed]
- Nasir, S.M.; Ostry, D.J. Auditory plasticity and speech motor learning. Proc. Natl. Acad. Sci. USA 2009, 106, 20470–20475. [Google Scholar] [CrossRef] [PubMed]
- Sugden, E.; Baker, E.; Munro, N.; Williams, A.L.; Trivette, C.M. Service delivery and intervention intensity for phonological-based speech sound disorders. Int. J. Lang. Commun. Disord. 2018, 53, 718–734. [Google Scholar] [CrossRef]
- Williams, A.L. Intensity in phonological intervention: Is there a prescribed amount? Int. J. Speech Lang. Pathol. 2012, 14, 456–461. [Google Scholar] [CrossRef]
- Neumann, K.; Holler-Zittlau, I.; van Minnen, S.; Sick, U.; Zaretsky, Y.; Euler, H.A. Katzengoldstandards in der Sprachstandserfassung: Sensitivität und Spezifität des Kindersprachscreenings (KiSS). [Fool’s gold standards in language screening. Sensitivity and specificity of the Hessian child language screening test (Kindersprachscreening, KiSS)]. HNO 2011, 59, 97–109. [Google Scholar] [CrossRef]
- Ritterfeld, U.; Rindermann, H. Mütterliche Einstellung zur sprachtherapeutischen Behandlung ihrer Kinder [Maternal attitudes toward speech therapy treatment of their children]. Z. Für Klin. Psychol. Und Psychother. 2004, 33, 172–182. [Google Scholar] [CrossRef]
- Goorhuis-Brouwer, S.M.; Knijff, W.A. Language disorders in children: When is speech therapy recommend? Int. J. Pediatric Otorhinolaryngol. 2003, 67, 525–529. [Google Scholar] [CrossRef]
- Hickok, G. The functional neuroanatomy of language. Phys. Life Rev. 2009, 6, 121–143. [Google Scholar] [CrossRef] [PubMed]
- Hickok, G.; Poeppel, D. Dorsal and ventral streams: A framework for understanding aspects of the functional anatomy of language. Cognition 2004, 92, 67–99. [Google Scholar] [CrossRef] [PubMed]
- Kotz, S.A.; Schwartze, M. Cortical speech processing unplugged: A timely subcortico-cortical framework. Trends Cogn. Sci. 2010, 14, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Hodson, B.; Paden, E. Targeting Intelligible Speech: A Phonological Approach to Remediation, 2nd ed.; Pro-Ed/College Hill: Austin, TX, USA, 1991. [Google Scholar]
- Wiefferink, K.; van Beugen, C.; Wegener Sleeswijk, C.; Gerrits, E. Children with language delay referred to Dutch speech and hearing centres: Caseload characteristics. Int. J. Lang. Commun. Disord. 2020, 55, 573–582. [Google Scholar] [CrossRef]
- McLeod, S.; Crowe, K. Children’s consonant acquisition in 27 languages: A cross-linguistic Review. Am. J. Speech Lang. Pathol. 2018, 27, 1546–1571. [Google Scholar] [CrossRef] [PubMed]
- Gartlehner, G.; Hansen, R.A.; Nissman, D.; Lohr, K.N.; Carey, T.S. A simple and valid tool distinguished efficacy from effectiveness studies. J. Clin. Epidemiol. 2006, 59, 1040–1048. [Google Scholar] [CrossRef] [PubMed]
- Singal, A.G.; Higgins, P.D.R.; Waljee, A.K. A Primer on Effectiveness and Efficacy Trials. Clin. Transl. Gastroenterol. 2014, 5, e45. [Google Scholar] [CrossRef]
- Ottow-Henning, E.; Keij, B. Does group intervention make a difference for the speech sound development of Dutch pre-school children with Developmental Language Disorder? Int. J. Speech Lang. Pathol. 2020, 22, 696–707. [Google Scholar] [CrossRef]
- Jesus, L.M.T.; Martinez, J.; Santos, J.; Hall, A.; Joffe, V. Comparing traditional and tablet-based intervention for children with speech sound disorders: A randomized controlled trial. J. Speech Lang. Hear. Res. 2019, 62, 4045–4061. [Google Scholar] [CrossRef]


| Realization of the IPMSP Model in PhonoSens | |
|---|---|
| Processing/Monitoring Levels of IPMSP Model | Realization in the PhonoSens Concept |
| Processes | PhonoSens steps |
| Phonological encoding: | Step 1: Categorical phonological perception |
| Selection and sequencing of linguistic units that target the formation of phonological units | Training of categorical phonological perception for target phonemes, error phonemes, and acoustically similar phonemes |
| Motor planning: | Step 2: Phoneme acquirement |
| Articulatory movement targets are selected | Stepwise initiation of the target phoneme in an increasingly complex coarticulatory context up to the sentence level |
| Motor programming: | Step 3: Articulatory fine-tuning I |
| Muscle-specific motor planning | Phoneme production training in additional words and sentences |
| Motor execution: | Step 4: Articulatory fine-tuning II |
| Neural signals are transmitted to peripheral systems and converted into coordinated muscle activity | Phoneme production training for words that are repeated three times quickly in one breath |
| Monitoring | PhonoSens steps |
| Internal self-monitoring: | Step 5: Enhanced auditory self-monitoring |
| Incorrectly planned phonemes are detected | This step focuses on the planned decision for the correct use (selection and localization) of the target phoneme in words |
| External auditory self-monitoring: | Step 6: Assisted generalization |
| Error correction and instant articulatory adaptation | This step focuses on improvement of the child’s self-correction during spontaneous speech. Steps 5 and 6 both address internal, external auditory, and somatosensory self-monitoring processes |
| External somatosensory self-monitoring: | TTOS: Thermal Tactile Oral Stimulation |
| Information regarding the current state of the articulators and necessary error correction | Each treatment begins with a short thermal tactile oral stimulation (TTOS) using an ice-stick. The TTOS is believed to facilitate speech motor learning by temporarily increasing cortical somatosensory activity. |
| Mispronounced Consonants per Participant | ||||||
|---|---|---|---|---|---|---|
| Age at T0 | Assessment T0 | Assessment T1 | ||||
| Child | (y;m) | Gender | Incorrect Consonants | Conson | Incorrect Consonants | Conson |
| Treatment group | ||||||
| 1 | 5;06 | f | m p f l n t j x g k s ʃ | 38 | m n t k s | 18 |
| 5 | 4;10 | f | m b p v l n t ç g ŋ k ʃ | 40 | m b l n g ʃ | 11 |
| 7 | 3;07 | f | m b f v l n t j ç ʁ g ŋ k z s ʃ | 100 | m b f v l n d t ç ʁ g k s ʃ | 52 |
| 8 | 4;09 | m | f l n t ç ʁ g k ʃ | 13 | k ʃ | 2 |
| 10 | 4;04 | f | m b p n t g k s ʃ | 39 | m b n t ʁ g k z s ʃ | 31 |
| 13 | 5;05 | m | f l t ç g ŋ k ʃ | 47 | f v l t j ç k z s ʃ | 41 |
| 14 | 4;05 | m | m l n t ç g k ʃ | 32 | l n t ç x g k s ʃ | 18 |
| 16 | 5;02 | f | m n t ç g ŋ k s ʃ | 59 | n t ç | 4 |
| 18 | 3;07 | f | f v l n d t ç g ŋ k s ʃ | 64 | l n d t ç g k ʃ | 42 |
| 19 | 5;01 | m | n t g k ʃ | 10 | f l n ç g k ʃ | 8 |
| 20 | 4;10 | f | l t ç ʁ g s ʃ | 18 | v n ç g ʃ | 7 |
| 23 | 4;05 | m | p l n t ʁ g ŋ k ʃ | 56 | f v n t ʁ g ŋ k s ʃ | 54 |
| 26 | 5;00 | f | b l n t ç ʁ g ŋ k s ʃ | 25 | m b l n t h ç g k ʃ | 17 |
| 27 | 5;00 | f | l n d t ç g ŋ k s ʃ | 32 | m p v n t ç g k s ʃ | 16 |
| 28 | 4;02 | m | p l n t ç g k ʃ | 16 | n t g k | 8 |
| 29 | 4;02 | m | p f v l n t j ç ʁ g ŋ k s ʃ | 91 | m b v n d t ç ʁ g ŋ k s ʃ | 64 |
| Wait-list control group | ||||||
| 2 | 4;07 | f | b p f v n t ç ʁ g k z ʃ | 41 | m b p f v l n t j ç g z s ʃ | 44 |
| 3 | 4;05 | f | b l n d t j ç g k ʃ | 40 | m f n d t ç x ʁ g z ʃ | 24 |
| 4 | 4;01 | f | m p f v l n t j ç x ʁ g k s ʃ | 77 | v l t ç ʁ g ŋ k s ʃ | 58 |
| 6 | 4;06 | f | f l n t ç g ŋ k ʃ | 24 | m b p f l n t g ŋ k s ʃ | 20 |
| 9 | 4;09 | f | v t g k ʃ | 8 | m t ŋ s ʃ | 6 |
| 11 | 5;01 | f | f l d t ç g k s ʃ | 16 | n d t k | 9 |
| 12 | 4;01 | f | m v l n d t ç ʁ g k ʃ | 44 | m p v l n t j ç g k s ʃ | 44 |
| 15 | 4;06 | m | m b p v l n t ç g k s ʃ | 27 | m f l n d t ʁ g k s ʃ | 19 |
| 17 | 4;10 | f | t ç k ʃ | 7 | n t ç g ʃ | 7 |
| 21 | 4;11 | f | f n t g s ʃ | 15 | m l n t ʁ g k ʃ | 16 |
| 22 | 3;09 | m | m l n t ç ʁ g k s ʃ | 45 | b v l n t ç ʁ z ʃ | 31 |
| 24 | 3;09 | m | b p v l n t ç g k s ʃ | 76 | p v l n t ç g ŋ k ʃ | 56 |
| 25 | 4;02 | m | l n d t ʁ g ŋ k s ʃ | 46 | m b p n d t j g ŋ k s ʃ | 45 |
| 30 | 4;06 | m | l t ʃ | 31 | n ʃ | 2 |
| 31 | 5;00 | m | b g ʃ | 22 | n t ŋ k ʃ | 26 |
| 32 | 4;07 | m | f l t g ŋ k | 43 | m t g ŋ k s ʃ | 42 |
| Number of Phonological Processes per Participant | |||||
|---|---|---|---|---|---|
| Age at T0 | Assessment T0 | Assessment T1 | |||
| Child | (y;m) | Gender | # Phonological Processes | # Phonological Processes | # pp diff. T0-T1 |
| Treatment group | |||||
| 1 | 5;06 | f | 34 | 18 | −16 |
| 5 | 4;10 | f | 42 | 10 | −32 |
| 7 | 3;07 | f | 112 | 59 | −53 |
| 8 | 4;09 | m | 15 | 2 | −13 |
| 10 | 4;04 | f | 39 | 31 | −8 |
| 13 | 5;05 | m | 50 | 37 | −13 |
| 14 | 4;05 | m | 29 | 19 | −10 |
| 16 | 5;02 | f | 57 | 3 | −54 |
| 18 | 3;07 | f | 70 | 43 | −27 |
| 19 | 5;01 | m | 10 | 9 | −1 |
| 20 | 4;10 | f | 16 | 6 | −10 |
| 23 | 4;05 | m | 67 | 59 | −8 |
| 26 | 5;00 | f | 27 | 17 | −10 |
| 27 | 5;00 | f | 35 | 17 | −18 |
| 28 | 4;02 | m | 16 | 7 | −9 |
| 29 | 4;02 | m | 92 | 69 | −23 |
| Wait-list control group | |||||
| 2 | 4;07 | f | 41 | 43 | 2 |
| 3 | 4;05 | f | 40 | 21 | −19 |
| 4 | 4;01 | f | 88 | 72 | −16 |
| 6 | 4;06 | f | 25 | 21 | −4 |
| 9 | 4;09 | f | 7 | 6 | −1 |
| 11 | 5;01 | f | 15 | 8 | −7 |
| 12 | 4;01 | f | 51 | 39 | −12 |
| 15 | 4;06 | m | 23 | 17 | -6 |
| 17 | 4;10 | f | 7 | 7 | 0 |
| 21 | 4;11 | f | 15 | 17 | 2 |
| 22 | 3;09 | m | 49 | 34 | −15 |
| 24 | 3;09 | m | 86 | 70 | −16 |
| 25 | 4;02 | m | 49 | 44 | −5 |
| 30 | 4;06 | m | 32 | 2 | −30 |
| 31 | 5;00 | m | 21 | 26 | 5 |
| 32 | 4;07 | m | 43 | 46 | 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Siemons-Lühring, D.I.; Euler, H.A.; Mathmann, P.; Suchan, B.; Neumann, K. The Effectiveness of an Integrated Treatment for Functional Speech Sound Disorders—A Randomized Controlled Trial. Children 2021, 8, 1190. https://doi.org/10.3390/children8121190
Siemons-Lühring DI, Euler HA, Mathmann P, Suchan B, Neumann K. The Effectiveness of an Integrated Treatment for Functional Speech Sound Disorders—A Randomized Controlled Trial. Children. 2021; 8(12):1190. https://doi.org/10.3390/children8121190
Chicago/Turabian StyleSiemons-Lühring, Denise I., Harald A. Euler, Philipp Mathmann, Boris Suchan, and Katrin Neumann. 2021. "The Effectiveness of an Integrated Treatment for Functional Speech Sound Disorders—A Randomized Controlled Trial" Children 8, no. 12: 1190. https://doi.org/10.3390/children8121190
APA StyleSiemons-Lühring, D. I., Euler, H. A., Mathmann, P., Suchan, B., & Neumann, K. (2021). The Effectiveness of an Integrated Treatment for Functional Speech Sound Disorders—A Randomized Controlled Trial. Children, 8(12), 1190. https://doi.org/10.3390/children8121190






