Pediatric Cardio-Oncology Medicine: A New Approach in Cardiovascular Care
Abstract
:1. Introduction
2. Evolution of Pediatric Cardio-Oncology as a Discipline
3. Surveillance and Management
3.1. Screening
3.2. Diagnosis
3.3. Prevention
3.4. Treatment
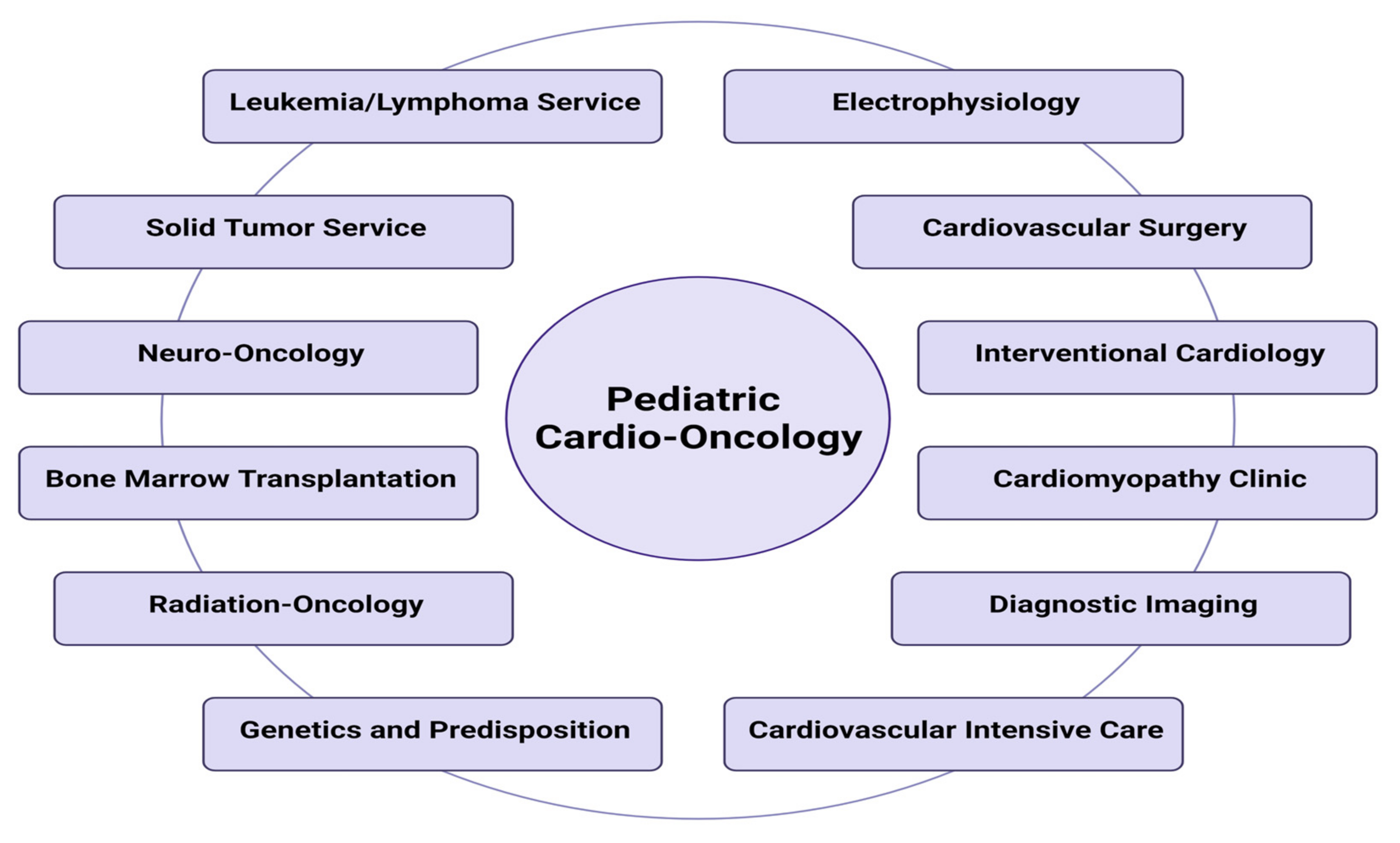
4. Pediatric Cardio-Oncology Healthcare Model
4.1. Inpatient PedCO
4.2. Outpatient PedCO
4.3. Pediatric Oncology-Critical Care
4.4. Congenital Heart Disease
4.5. Cardiac Electrophysiology
4.6. Sickle Cell Disease (SCD)
4.7. Cardiovascular Imaging
4.8. Long-Term Follow-Up
5. Academic Practices
6. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACC | American College of Cardiology |
| ACEi | angiotensin-converting enzyme inhibitor |
| ACT | after completion of therapy |
| ARBs | Angiotensin receptor blocker |
| AHA | American Heart Association |
| BB | beta blocker |
| BNP | B-type natriuretic peptide |
| CHD | congenital heart disease |
| DD | diastolic dysfunction |
| cMRI | cardiac magnetic resonance imaging |
| CV | cardiovascular |
| DCM | dilated cardiomyopathy |
| Echo | echocardiography |
| HF | heart failure |
| ILR | implantable loop recorder |
| LBCH | Le Bonheur Children’s Hospital |
| LVEF | left ventricular ejection fraction |
| LVSF | left ventricular shortening fraction |
| MCS | mechanical circulatory support |
| NT-proBNP | N-terminal pro B-type natriuretic peptide |
| PedCO | pediatric cardio-oncology |
| SCD | sickle cell disease |
| SJCRH | St. Jude Children’s Research Hospital |
References
- Howlader, N.; Noone, A.M.; Krapcho, M.; Miller, D.; Brest, A.; Yu, M.; Ruhl, J.; Tatalovich, Z.; Mariotto, A.; Lewis, D.R.; et al. SEER Cancer Statistics Review (CSR), 1975–2017; National Cancer Institute: Bethesda, MD, USA, 2020. Available online: https://seer.cancer.gov/csr/1975_2017/ (accessed on 8 September 2021).
- Campia, U.; Moslehi, J.J.; Amiri-Kordestani, L.; Barac, A.; Beckman, J.A.; Chism, D.D.; Cohen, P.; Groarke, J.D.; Herrmann, J.; Reilly, C.M.; et al. Cardio-Oncology: Vascular and Metabolic Perspectives: A Scientific Statement from the American Heart Association. Circulation 2019, 139, e579–e602. [Google Scholar] [CrossRef]
- Lipshultz, S.E.; Adams, M.J.; Colan, S.D.; Constine, L.S.; Herman, E.H.; Hsu, D.T.; Hudson, M.M.; Kremer, L.C.; Landy, D.C.; Miller, T.L.; et al. Long-term cardiovascular toxicity in children, adolescents, and young adults who receive cancer therapy: Pathophysiology, course, monitoring, management, prevention, and research directions: A scientific statement from the American Heart Association. Circulation 2013, 128, 1927–1995. [Google Scholar] [CrossRef] [Green Version]
- Carver, J.R.; Szalda, D.; Ky, B. Asymptomatic cardiac toxicity in long-term cancer survivors: Defining the population and recommendations for surveillance. Semin. Oncol. 2013, 40, 229–238. [Google Scholar] [CrossRef] [Green Version]
- Cardinale, D.; Colombo, A.; Bacchiani, G.; Tedeschi, I.; Meroni, C.A.; Veglia, F.; Civelli, M.; Lamantia, G.; Colombo, N.; Curigliano, G.; et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy [A study that validates the concept that early detection and intervention on anthracycline toxicity improves outcomes]. Circulation 2015, 131, 1981–1988. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steinherz, L.J.; Graham, T.; Hurwitz, R.; Sondheimer, H.M.; Schwartz, R.G.; Shaffer, E.M.; Sandor, G.; Benson, L.; Williams, R. Guidelines for cardiac monitoring of children during and after anthracycline therapy: Report of the Cardiology Committee of the Childrens Cancer Study Group. Pediatrics 1992, 89, 942–949. [Google Scholar] [CrossRef] [PubMed]
- Getz, K.D.; Sung, L.; Ky, B.; Gerbing, R.B.; Leger, K.J.; Leahy, A.B.; Sack, L.; Woods, W.G.; Alonzo, T.; Gamis, A.; et al. Occurrence of Treatment-Related Cardiotoxicity and Its Impact on Outcomes Among Children Treated in the AAML0531 Clinical Trial: A Report from the Children’s Oncology Group. J. Clin. Oncol. 2019, 37, 12–21. [Google Scholar] [CrossRef]
- Hamo, C.E.; Bloom, M.W.; Cardinale, D.; Ky, B.; Nohria, A.; Baer, L.; Skopicki, H.; Lenihan, D.J.; Gheorghiade, M.; Lyon, A.R.; et al. Cancer Therapy-Related Cardiac Dysfunction and Heart Failure: Part 2: Prevention, Treatment, Guidelines, and Future Directions. Circ. Heart Fail. 2016, 9, e002843. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adao, R.; de Keulenaer, G.; Leite-Moreira, A.; Bras-Silva, C. Cardiotoxicity associated with cancer therapy: Pathophysiology and prevention strategies. Rev. Port. Cardiol. 2013, 32, 395–409. [Google Scholar] [CrossRef] [PubMed]
- Simbre, V.C.; Duffy, S.A.; Dadlani, G.H.; Miller, T.L.; Lipshultz, S.E. Cardiotoxicity of cancer chemotherapy: Implications for children. Paediatr. Drugs 2005, 7, 187–202. [Google Scholar] [CrossRef]
- Patane, S. Cardiotoxicity: Cisplatin and long-term cancer survivors. Int. J. Cardiol. 2014, 175, 201–202. [Google Scholar] [CrossRef]
- Chen, M.H.; Kerkela, R.; Force, T. Mechanisms of cardiac dysfunction associated with tyrosine kinase inhibitor cancer therapeutics. Circulation 2008, 118, 84–95. [Google Scholar] [CrossRef]
- Goldberg, J.F.; Peters, E.J.; Tolley, E.A.; Hagler, M.N.; Joshi, V.M.; Wallace, S.E.; Nouer, S.S.; Beasley, G.S.; Martinez, H.R.; Ryan, K.A.; et al. Association of persistent tachycardia with early myocardial dysfunction in children undergoing allogeneic hematopoietic cell transplantation. Bone Marrow Transplant. 2021, 56, 2544–2554. [Google Scholar] [CrossRef]
- Martinez, H.R.; Salloum, R.; Wright, E.; Bueche, L.; Khoury, P.R.; Tretter, J.T.; Ryan, T.D. Echocardiographic myocardial strain analysis describes subclinical cardiac dysfunction after craniospinal irradiation in pediatric and young adult patients with central nervous system tumors. Cardiooncology 2021, 7, 5. [Google Scholar] [CrossRef] [PubMed]
- Jefferies, J.L.; Mazur, W.M.; Howell, C.R.; Plana, J.C.; Ness, K.K.; Li, Z.; Joshi, V.M.; Green, D.M.; Mulrooney, D.A.; Towbin, J.A.; et al. Cardiac remodeling after anthracycline and radiotherapy exposure in adult survivors of childhood cancer: A report from the St Jude Lifetime Cohort Study. Cancer 2021. [Google Scholar] [CrossRef]
- Marwick, T.H. Ejection Fraction Pros and Cons: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2018, 72, 2360–2379. [Google Scholar] [CrossRef] [PubMed]
- Versmissen, J.; Mirabito Colafella, K.M.; Koolen, S.L.W.; Danser, A.H.J. Vascular Cardio-Oncology: Vascular Endothelial Growth Factor inhibitors and hypertension. Cardiovasc. Res. 2019, 115, 904–914. [Google Scholar] [CrossRef]
- Moslehi, J.; Pandey, A.K.; Bhatia, N. Cardio-Oncology: Vascular Endothelial Growth Factor Inhibitors, Salt, and Macrophages: A Complicated Interaction. Hypertension 2017, 69, 785–786. [Google Scholar] [CrossRef] [Green Version]
- Ueyama, H.; Miyashita, H.; Takagi, H.; Cruz, C.; Burger, A.; Briasoulis, A.; Kuno, T. Network meta-analysis of anticoagulation strategies for venous thromboembolism in patients with cancer. J. Thromb. Thrombolysis 2021, 51, 102–111. [Google Scholar] [CrossRef]
- Mosarla, R.C.; Vaduganathan, M.; Qamar, A.; Moslehi, J.; Piazza, G.; Giugliano, R.P. Anticoagulation Strategies in Patients with Cancer: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2019, 73, 1336–1349. [Google Scholar] [CrossRef] [PubMed]
- Curigliano, G.; Lenihan, D.; Fradley, M.; Ganatra, S.; Barac, A.; Blaes, A.; Herrmann, J.; Porter, C.; Lyon, A.R.; Lancellotti, P.; et al. Management of cardiac disease in cancer patients throughout oncological treatment: ESMO consensus recommendations. Ann. Oncol. 2020, 31, 171–190. [Google Scholar] [CrossRef] [Green Version]
- US Food and Drug Administration. Orphan Drug Designations and Approvals. Available online: https://www.accessdata.fda.gov/scripts/opdlisting/oopd/detailedIndex.cfm?cfgridkey=441314. (accessed on 1 April 2021).
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey, D.E., Jr.; Colvin, M.M.; Drazner, M.H.; Filippatos, G.S.; Fonarow, G.C.; Givertz, M.M.; et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 2017, 136, e137–e161. [Google Scholar] [CrossRef] [PubMed]
- Menna, P.; Salvatorelli, E. Primary Prevention Strategies for Anthracycline Cardiotoxicity: A Brief Overview. Chemotherapy 2017, 62, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Cortes, J.; Di Cosimo, S.; Climent, M.A.; Cortes-Funes, H.; Lluch, A.; Gascon, P.; Mayordomo, J.I.; Gil, M.; Benavides, M.; Cirera, L.; et al. Nonpegylated liposomal doxorubicin (TLC-D99), paclitaxel, and trastuzumab in HER-2-overexpressing breast cancer: A multicenter phase I/II study. Clin. Cancer Res. 2009, 15, 307–314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lipshultz, S.E.; Miller, T.L.; Lipsitz, S.R.; Neuberg, D.S.; Dahlberg, S.E.; Colan, S.D.; Silverman, L.B.; Henkel, J.M.; Franco, V.I.; Cushman, L.L.; et al. Continuous Versus Bolus Infusion of Doxorubicin in Children with ALL: Long-term Cardiac Outcomes. Pediatrics 2012, 130, 1003–1011. [Google Scholar] [CrossRef] [Green Version]
- Yamada, S.; Wongwanakul, P. Randomized controlled trial of high dose bolus versus continuous intravenous infusion pantoprazole as an adjunct therapy to therapeutic endoscopy in massive bleeding peptic ulcer. J. Med. Assoc. Thai. 2012, 95, 349–357. [Google Scholar]
- Liesse, K.; Harris, J.; Chan, M.; Schmidt, M.L.; Chiu, B. Dexrazoxane Significantly Reduces Anthracycline-induced Cardiotoxicity in Pediatric Solid Tumor Patients: A Systematic Review. J. Pediatr. Hematol. Oncol. 2018, 40, 417–425. [Google Scholar] [CrossRef]
- Getz, K.D.; Sung, L.; Alonzo, T.A.; Leger, K.J.; Gerbing, R.B.; Pollard, J.A.; Cooper, T.; Kolb, E.A.; Gamis, A.S.; Ky, B.; et al. Effect of Dexrazoxane on Left Ventricular Systolic Function and Treatment Outcomes in Patients with Acute Myeloid Leukemia: A Report from the Children’s Oncology Group. J. Clin. Oncol. 2020, 38, 2398–2406. [Google Scholar] [CrossRef] [PubMed]
- Feijen, E.A.; Leisenring, W.M.; Stratton, K.L.; Ness, K.K.; van der Pal, H.J.; Caron, H.N.; Armstrong, G.T.; Green, D.M.; Hudson, M.M.; Oeffinger, K.C.; et al. Equivalence Ratio for Daunorubicin to Doxorubicin in Relation to Late Heart Failure in Survivors of Childhood Cancer. J. Clin. Oncol. 2015, 33, 3774–3780. [Google Scholar] [CrossRef] [Green Version]
- Feijen, E.A.M.; Leisenring, W.M.; Stratton, K.L.; Ness, K.K.; van der Pal, H.J.H.; van Dalen, E.C.; Armstrong, G.T.; Aune, G.J.; Green, D.M.; Hudson, M.M.; et al. Derivation of Anthracycline and Anthraquinone Equivalence Ratios to Doxorubicin for Late-Onset Cardiotoxicity. JAMA Oncol. 2019, 5, 864–871. [Google Scholar] [CrossRef]
- Mulrooney, D.A.; Armstrong, G.T.; Huang, S.; Ness, K.K.; Ehrhardt, M.J.; Joshi, V.M.; Plana, J.C.; Soliman, E.Z.; Green, D.M.; Srivastava, D.; et al. Cardiac Outcomes in Adult Survivors of Childhood Cancer Exposed to Cardiotoxic Therapy: A Cross-sectional Study. Ann. Intern. Med. 2016, 164, 93–101. [Google Scholar] [CrossRef] [Green Version]
- van der Pal, H.J.; van Dalen, E.C.; van Delden, E.; van Dijk, I.W.; Kok, W.E.; Geskus, R.B.; Sieswerda, E.; Oldenburger, F.; Koning, C.C.; van Leeuwen, F.E.; et al. High risk of symptomatic cardiac events in childhood cancer survivors. J. Clin. Oncol. 2012, 30, 1429–1437. [Google Scholar] [CrossRef] [Green Version]
- Haddy, N.; Diallo, S.; El-Fayech, C.; Schwartz, B.; Pein, F.; Hawkins, M.; Veres, C.; Oberlin, O.; Guibout, C.; Pacquement, H.; et al. Cardiac Diseases Following Childhood Cancer Treatment: Cohort Study. Circulation 2016, 133, 31–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mulrooney, D.A.; Hyun, G.; Ness, K.K.; Ehrhardt, M.J.; Yasui, Y.; Duprez, D.; Howell, R.M.; Leisenring, W.M.; Constine, L.S.; Tonorezos, E.; et al. Major cardiac events for adult survivors of childhood cancer diagnosed between 1970 and 1999: Report from the Childhood Cancer Survivor Study cohort. BMJ 2020, 368, l6794. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mulrooney, D.A.; Yeazel, M.W.; Kawashima, T.; Mertens, A.C.; Mitby, P.; Stovall, M.; Donaldson, S.S.; Green, D.M.; Sklar, C.A.; Robison, L.L.; et al. Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: Retrospective analysis of the Childhood Cancer Survivor Study cohort. BMJ 2009, 339, b4606. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parent, S.; Pituskin, E.; Paterson, D.I. The Cardio-oncology Program: A Multidisciplinary Approach to the Care of Cancer Patients with Cardiovascular Disease. Can. J. Cardiol. 2016, 32, 847–851. [Google Scholar] [CrossRef]
- Francis, S.A.; Asnani, A.; Neilan, T.; Scherrer-Crosbie, M. Optimizing cardio-oncology programs for cancer patients. Future Oncol. 2015, 11, 2011–2015. [Google Scholar] [CrossRef]
- Tajiri, K.; Aonuma, K.; Sekine, I. Cardio-oncology: A multidisciplinary approach for detection, prevention and management of cardiac dysfunction in cancer patients. Jpn. J. Clin. Oncol. 2017, 47, 678–682. [Google Scholar] [CrossRef] [Green Version]
- Bozkurt, B.; Coats, A.J.S.; Tsutsui, H.; Abdelhamid, C.M.; Adamopoulos, S.; Albert, N.; Anker, S.D.; Atherton, J.; Bohm, M.; Butler, J.; et al. Universal definition and classification of heart failure: A report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure: Endorsed by the Canadian Heart Failure Society, Heart Failure Association of India, Cardiac Society of Australia and New Zealand, and Chinese Heart Failure Association. Eur. J. Heart. 2021, 23, 352–380. [Google Scholar] [CrossRef]
- Kantor, P.F.; Lougheed, J.; Dancea, A.; McGillion, M.; Barbosa, N.; Chan, C.; Dillenburg, R.; Atallah, J.; Buchholz, H.; Chant-Gambacort, C.; et al. Presentation, diagnosis, and medical management of heart failure in children: Canadian Cardiovascular Society guidelines. Can. J. Cardiol. 2013, 29, 1535–1552. [Google Scholar] [CrossRef]
- Yildirim, A.; Sedef Tunaoglu, F.; Pinarli, F.G.; Ilhan, M.; Oguz, A.; Karadeniz, C.; Olgunturk, R.; Oguz, D.; Kula, S. Early diagnosis of anthracycline toxicity in asymptomatic long-term survivors: Dobutamine stress echocardiography and tissue Doppler velocities in normal and abnormal myocardial wall motion. Eur. J. Echocardiogr. 2010, 11, 814–822. [Google Scholar] [CrossRef] [Green Version]
- Heidenreich, P.A.; Hancock, S.L.; Vagelos, R.H.; Lee, B.K.; Schnittger, I. Diastolic dysfunction after mediastinal irradiation. Am. Heart J. 2005, 150, 977–982. [Google Scholar] [CrossRef] [PubMed]
- Chow, E.J.; Leger, K.J.; Bhatt, N.S.; Mulrooney, D.A.; Ross, C.J.; Aggarwal, S.; Bansal, N.; Ehrhardt, M.J.; Armenian, S.H.; Scott, J.M.; et al. Paediatric cardio-oncology: Epidemiology, screening, prevention, and treatment. Cardiovasc. Res. 2019, 115, 922–934. [Google Scholar] [CrossRef] [PubMed]
- Menna, P.; Calabrese, V.; Armento, G.; Annibali, O.; Greco, C.; Salvatorelli, E.; Marchesi, F.; Reggiardo, G.; Minotti, G. Pharmacology of Cardio-Oncology: Chronotropic and Lusitropic Effects of B-Type Natriuretic Peptide in Cancer Patients with Early Diastolic Dysfunction Induced by Anthracycline or Nonanthracycline Chemotherapy. J. Pharmacol. Exp. Ther. 2018, 366, 158–168. [Google Scholar] [CrossRef] [Green Version]
- Shinke, T.; Takeuchi, M.; Takaoka, H.; Yokoyama, M. Beneficial effects of heart rate reduction on cardiac mechanics and energetics in patients with left ventricular dysfunction. Jpn. Circ. J. 1999, 63, 957–964. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Armenian, S.H.; Lacchetti, C.; Barac, A.; Carver, J.; Constine, L.S.; Denduluri, N.; Dent, S.; Douglas, P.S.; Durand, J.B.; Ewer, M.; et al. Prevention and Monitoring of Cardiac Dysfunction in Survivors of Adult Cancers: American Society of Clinical Oncology Clinical Practice Guideline. J. Clin. Oncol. 2017, 35, 893–911. [Google Scholar] [CrossRef] [PubMed]
- Pignatelli, R.H.; Ghazi, P.; Reddy, S.C.; Thompson, P.; Cui, Q.; Castro, J.; Okcu, M.F.; Jefferies, J.L. Abnormal Myocardial Strain Indices in Children Receiving Anthracycline Chemotherapy. Pediatr. Cardiol. 2015, 36, 1610–1616. [Google Scholar] [CrossRef]
- Pignatelli, R.; Law, M.A.; Martinez, H.; Altman, C.; Ayres, N.; Jefferies, J.L.; Ganame, J. Two-dimensional speckle strain imaging: In the management of paraganglioma, acute junctional tachycardia, and myocardial dysfunction in a child. Tex. Heart Inst. J. 2012, 39, 119–121. [Google Scholar]
- Nagata, Y.; Takeuchi, M.; Mizukoshi, K.; Wu, V.C.; Lin, F.C.; Negishi, K.; Nakatani, S.; Otsuji, Y. Intervendor variability of two-dimensional strain using vendor-specific and vendor-independent software. J. Am. Soc. Echocardiogr. 2015, 28, 630–641. [Google Scholar] [CrossRef]
- Bansal, N.; Adams, M.J.; Ganatra, S.; Colan, S.D.; Aggarwal, S.; Steiner, R.; Amdani, S.; Lipshultz, E.R.; Lipshultz, S.E. Strategies to prevent anthracycline-induced cardiotoxicity in cancer survivors. Cardiooncology 2019, 5, 18. [Google Scholar] [CrossRef] [Green Version]
- McMurray, J.J.; Packer, M.; Desai, A.S.; Gong, J.; Lefkowitz, M.P.; Rizkala, A.R.; Rouleau, J.L.; Shi, V.C.; Solomon, S.D.; Swedberg, K.; et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N. Engl. J. Med. 2014, 371, 993–1004. [Google Scholar] [CrossRef] [Green Version]
- Lipshultz, S.E.; Law, Y.M.; Asante-Korang, A.; Austin, E.D.; Dipchand, A.I.; Everitt, M.D.; Hsu, D.T.; Lin, K.Y.; Price, J.F.; Wilkinson, J.D.; et al. Cardiomyopathy in Children: Classification and Diagnosis: A Scientific Statement from the American Heart Association. Circulation 2019, 140, e9–e68. [Google Scholar] [CrossRef]
- Price, J.F. Congestive Heart Failure in Children. Pediatr. Rev. 2019, 40, 60–70. [Google Scholar] [CrossRef]
- Shaddy, R.; Canter, C.; Halnon, N.; Kochilas, L.; Rossano, J.; Bonnet, D.; Bush, C.; Zhao, Z.; Kantor, P.; Burch, M.; et al. Design for the sacubitril/valsartan (LCZ696) compared with enalapril study of pediatric patients with heart failure due to systemic left ventricle systolic dysfunction (PANORAMA-HF study). Am. Heart J. 2017, 193, 23–34. [Google Scholar] [CrossRef]
- Peng, D.M.; Rosenthal, D.N.; Zafar, F.; Smyth, L.; VanderPluym, C.J.; Lorts, A. Collaboration and new data in ACTION: A learning health care system to improve pediatric heart failure and ventricular assist device outcomes. Transl. Pediatr. 2019, 8, 349–355. [Google Scholar] [CrossRef]
- Essa, H.; Dobson, R.; Wright, D.; Lip, G.Y.H. Hypertension management in cardio-oncology. J. Hum. Hypertens. 2020, 34, 673–681. [Google Scholar] [CrossRef]
- Piccirillo, J.F.; Tierney, R.M.; Costas, I.; Grove, L.; Spitznagel, E.L., Jr. Prognostic importance of comorbidity in a hospital-based cancer registry. JAMA 2004, 291, 2441–2447. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Subcommittee on screening and management of high blood pressure in children; Flynn, J.T.; Kaelber, D.C.; Baker-Smith, C.M.; Blowey, D.; Carroll, A.E.; Daniels, S.R.; de Ferranti, S.D.; Dionne, J.M.; Falkner, B.; et al. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics 2017, 140, e20171904. [Google Scholar] [CrossRef] [Green Version]
- Kheshti, R.; Aalipour, M.; Namazi, S. A comparison of five common drug-drug interaction software programs regarding accuracy and comprehensiveness. J. Res. Pharm. Pract. 2016, 5, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Pizzo, P.; Poplack, D. Principles and Practice of Pediatric Oncology, 6th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2011; Available online: https://www.r2library.com/Resource/Title/160547682X (accessed on 1 October 2021).
- Collins, R.T., II; Von Behren, J.; Yang, W.; Carmichael, S.L.; Reynolds, P.; Fisher, P.G.; Shaw, G.M. Congenital heart disease complexity and childhood cancer risk. Birth Defects Res. 2018, 110, 1314–1321. [Google Scholar] [CrossRef] [PubMed]
- Bergstrom, S.; Carr, H.; Petersson, G.; Stephansson, O.; Bonamy, A.K.; Dahlstrom, A.; Halvorsen, C.P.; Johansson, S. Trends in Congenital Heart Defects in Infants with Down Syndrome. Pediatrics 2016, 138, e20160123. [Google Scholar] [CrossRef] [Green Version]
- Paladini, D.; Tartaglione, A.; Agangi, A.; Teodoro, A.; Forleo, F.; Borghese, A.; Martinelli, P. The association between congenital heart disease and Down syndrome in prenatal life. Ultrasound Obstet. Gynecol. 2000, 15, 104–108. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Gurvitz, M.Z.; Beausejour-Ladouceur, V.; Lawler, P.R.; Therrien, J.; Marelli, A.J. Cancer Risk in Congenital Heart Disease-What Is the Evidence? Can. J. Cardiol. 2019, 35, 1750–1761. [Google Scholar] [CrossRef] [PubMed]
- Stevens, T.; van der Werff Ten Bosch, J.; De Rademaeker, M.; Van Den Bogaert, A.; van den Akker, M. Risk of malignancy in 22q11.2 deletion syndrome. Clin. Case Rep. 2017, 5, 486–490. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hou, H.T.; Chen, H.X.; Wang, X.L.; Yuan, C.; Yang, Q.; Liu, Z.G.; He, G.W. Genetic characterisation of 22q11.2 variations and prevalence in patients with congenital heart disease. Arch. Dis. Child 2020, 105, 367–374. [Google Scholar] [CrossRef]
- Mulrooney, D.A.; Soliman, E.Z.; Ehrhardt, M.J.; Lu, L.; Duprez, D.A.; Luepker, R.V.; Armstrong, G.T.; Joshi, V.M.; Green, D.M.; Srivastava, D.; et al. Electrocardiographic abnormalities and mortality in aging survivors of childhood cancer: A report from the St Jude Lifetime Cohort Study. Am. Heart J. 2017, 189, 19–27. [Google Scholar] [CrossRef]
- Buza, V.; Rajagopalan, B.; Curtis, A.B. Cancer Treatment-Induced Arrhythmias: Focus on Chemotherapy and Targeted Therapies. Circ. Arrhythm Electrophysiol. 2017, 10, e005443. [Google Scholar] [CrossRef]
- Guglin, M.; Aljayeh, M.; Saiyad, S.; Ali, R.; Curtis, A.B. Introducing a new entity: Chemotherapy-induced arrhythmia. Europace 2009, 11, 1579–1586. [Google Scholar] [CrossRef]
- Tamargo, J.; Caballero, R.; Delpon, E. Cancer chemotherapy and cardiac arrhythmias: A review. Drug Saf. 2015, 38, 129–152. [Google Scholar] [CrossRef]
- Alexandre, J.; Moslehi, J.J.; Bersell, K.R.; Funck-Brentano, C.; Roden, D.M.; Salem, J.E. Anticancer drug-induced cardiac rhythm disorders: Current knowledge and basic underlying mechanisms. Pharmacol. Ther. 2018, 189, 89–103. [Google Scholar] [CrossRef]
- Fradley, M.G.; Moslehi, J. QT Prolongation and Oncology Drug Development. Card. Electrophysiol. Clin. 2015, 7, 341–355. [Google Scholar] [CrossRef] [PubMed]
- Woosley, R.L.; Black, K.; Heise, C.W.; Romero, K. CredibleMeds.org: What does it offer? Trends Cardiovasc. Med. 2018, 28, 94–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coen, M.; Jandus, P.; Rollason, V.; Seebach, J.; Serratrice, J. Cinderella side effect: Intravenous corticosteroid-induced bradycardia. Therapie 2020, 76, 480–481. [Google Scholar] [CrossRef] [PubMed]
- Shankar, S.M.; Marina, N.; Hudson, M.M.; Hodgson, D.C.; Adams, M.J.; Landier, W.; Bhatia, S.; Meeske, K.; Chen, M.H.; Kinahan, K.E.; et al. Monitoring for cardiovascular disease in survivors of childhood cancer: Report from the Cardiovascular Disease Task Force of the Children’s Oncology Group. Pediatrics 2008, 121, e387–396. [Google Scholar] [CrossRef]
- Bezzerides, V.J.; Walsh, A.; Martuscello, M.; Escudero, C.A.; Gauvreau, K.; Lam, G.; Abrams, D.J.; Triedman, J.K.; Alexander, M.E.; Bevilacqua, L.; et al. The Real-World Utility of the LINQ Implantable Loop Recorder in Pediatric and Adult Congenital Heart Patients. JACC Clin. Electrophysiol. 2019, 5, 245–251. [Google Scholar] [CrossRef]
- DeBaun, M.R.; Ghafuri, D.L.; Rodeghier, M.; Maitra, P.; Chaturvedi, S.; Kassim, A.; Ataga, K.I. Decreased median survival of adults with sickle cell disease after adjusting for left truncation bias: A pooled analysis. Blood 2019, 133, 615–617. [Google Scholar] [CrossRef] [Green Version]
- Kassim, A.A.; Payne, A.B.; Rodeghier, M.; Macklin, E.A.; Strunk, R.C.; DeBaun, M.R. Low forced expiratory volume is associated with earlier death in sickle cell anemia. Blood 2015, 126, 1544–1550. [Google Scholar] [CrossRef] [Green Version]
- Platt, O.S.; Brambilla, D.J.; Rosse, W.F.; Milner, P.F.; Castro, O.; Steinberg, M.H.; Klug, P.P. Mortality in sickle cell disease. Life expectancy and risk factors for early death. N. Engl. J. Med. 1994, 330, 1639–1644. [Google Scholar] [CrossRef] [PubMed]
- Piel, F.B.; Steinberg, M.H.; Rees, D.C. Sickle Cell Disease. N. Engl. J. Med. 2017, 376, 1561–1573. [Google Scholar] [CrossRef] [Green Version]
- Voskaridou, E.; Christoulas, D.; Terpos, E. Sickle-cell disease and the heart: Review of the current literature. Br. J. Haematol. 2012, 157, 664–673. [Google Scholar] [CrossRef] [PubMed]
- Niss, O.; Quinn, C.T.; Lane, A.; Daily, J.; Khoury, P.R.; Bakeer, N.; Kimball, T.R.; Towbin, J.A.; Malik, P.; Taylor, M.D. Cardiomyopathy with Restrictive Physiology in Sickle Cell Disease. JACC Cardiovasc. Imaging. 2016, 9, 243–252. [Google Scholar] [CrossRef]
- Rai, P.; Niss, O.; Malik, P. A reappraisal of the mechanisms underlying the cardiac complications of sickle cell anemia. Pediatr. Blood Cancer 2017, 64, e26607. [Google Scholar] [CrossRef]
- Habibian, M.; Lyon, A.R. Monitoring the heart during cancer therapy. Eur. Heart J. Suppl. 2019, 21, M44–M49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Frommelt, P.C.; Minich, L.L.; Trachtenberg, F.L.; Altmann, K.; Camarda, J.; Cohen, M.S.; Colan, S.D.; Dragulescu, A.; Frommelt, M.A.; Johnson, T.R.; et al. Challenges with Left Ventricular Functional Parameters: The Pediatric Heart Network Normal Echocardiogram Database. J. Am. Soc. Echocardiogr. 2019, 32, 1331–1338. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.E.; Barac, A.; Thavendiranathan, P.; Scherrer-Crosbie, M. Strain Imaging in Cardio-Oncology. JACC Cardiol. Oncol. 2020, 2, 677–689. [Google Scholar] [CrossRef]
- Avelar, E.; Strickland, C.R.; Rosito, G. Role of Imaging in Cardio-Oncology. Curr. Treat. Opt. Cardiovasc. Med. 2017, 19, 46. [Google Scholar] [CrossRef] [PubMed]
- Nagueh, S.F.; Smiseth, O.A.; Appleton, C.P.; Byrd, B.F., III; Dokainish, H.; Edvardsen, T.; Flachskampf, F.A.; Gillebert, T.C.; Klein, A.L.; Lancellotti, P.; et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2016, 17, 1321–1360. [Google Scholar] [CrossRef] [PubMed]
- Bhatla, P.; Nielsen, J.C.; Ko, H.H.; Doucette, J.; Lytrivi, I.D.; Srivastava, S. Normal values of left atrial volume in pediatric age group using a validated allometric model. Circ. Cardiovasc. Imaging 2012, 5, 791–796. [Google Scholar] [CrossRef] [Green Version]
- Eidem, B.W.; McMahon, C.J.; Cohen, R.R.; Wu, J.; Finkelshteyn, I.; Kovalchin, J.P.; Ayres, N.A.; Bezold, L.I.; O’Brian Smith, E.; Pignatelli, R.H. Impact of cardiac growth on Doppler tissue imaging velocities: A study in healthy children. J. Am. Soc. Echocardiogr. 2004, 17, 212–221. [Google Scholar] [CrossRef]
- Armstrong, G.T.; Plana, J.C.; Zhang, N.; Srivastava, D.; Green, D.M.; Ness, K.K.; Daniel Donovan, F.; Metzger, M.L.; Arevalo, A.; Durand, J.B.; et al. Screening adult survivors of childhood cancer for cardiomyopathy: Comparison of echocardiography and cardiac magnetic resonance imaging. J. Clin. Oncol. 2012, 30, 2876–2884. [Google Scholar] [CrossRef] [PubMed]
- Bottinor, W.; Trankle, C.R.; Hundley, W.G. The Role of Cardiovascular MRI in Cardio-Oncology. Heart. Fail. Clin. 2021, 17, 121–133. [Google Scholar] [CrossRef] [PubMed]
- Winther, J.F.; Kenborg, L.; Byrne, J.; Hjorth, L.; Kaatsch, P.; Kremer, L.C.; Kuehni, C.E.; Auquier, P.; Michel, G.; de Vathaire, F.; et al. Childhood cancer survivor cohorts in Europe. Acta Oncol. 2015, 54, 655–668. [Google Scholar] [CrossRef]
- Howell, C.R.; Bjornard, K.L.; Ness, K.K.; Alberts, N.; Armstrong, G.T.; Bhakta, N.; Brinkman, T.; Caron, E.; Chemaitilly, W.; Green, D.M.; et al. Cohort Profile: The St. Jude Lifetime Cohort Study (SJLIFE) for paediatric cancer survivors. Int. J. Epidemiol. 2021, 50, 39–49. [Google Scholar] [CrossRef] [PubMed]
- Robison, L.L.; Armstrong, G.T.; Boice, J.D.; Chow, E.J.; Davies, S.M.; Donaldson, S.S.; Green, D.M.; Hammond, S.; Meadows, A.T.; Mertens, A.C.; et al. The Childhood Cancer Survivor Study: A National Cancer Institute-supported resource for outcome and intervention research. J. Clin. Oncol. 2009, 27, 2308–2318. [Google Scholar] [CrossRef] [Green Version]
- Armstrong, G.T.; Liu, Q.; Yasui, Y.; Neglia, J.P.; Leisenring, W.; Robison, L.L.; Mertens, A.C. Late mortality among 5-year survivors of childhood cancer: A summary from the Childhood Cancer Survivor Study. J. Clin. Oncol. 2009, 27, 2328–2338. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blanco, J.G.; Sun, C.L.; Landier, W.; Chen, L.; Esparza-Duran, D.; Leisenring, W.; Mays, A.; Friedman, D.L.; Ginsberg, J.P.; Hudson, M.M.; et al. Anthracycline-related cardiomyopathy after childhood cancer: Role of polymorphisms in carbonyl reductase genes—A report from the Children’s Oncology Group. J. Clin. Oncol. 2012, 30, 1415–1421. [Google Scholar] [CrossRef] [Green Version]
- Medicine, I.o.; Council, N.R. From Cancer Patient to Cancer Survivor: Lost in Transition; The National Academies Press: Washington, DC, USA, 2006; p. 534. [Google Scholar] [CrossRef]
- Armenian, S.H.; Hudson, M.M.; Mulder, R.L.; Chen, M.H.; Constine, L.S.; Dwyer, M.; Nathan, P.C.; Tissing, W.J.; Shankar, S.; Sieswerda, E.; et al. Recommendations for cardiomyopathy surveillance for survivors of childhood cancer: A report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol. 2015, 16, e123–136. [Google Scholar] [CrossRef] [Green Version]
- Kremer, L.C.; Mulder, R.L.; Oeffinger, K.C.; Bhatia, S.; Landier, W.; Levitt, G.; Constine, L.S.; Wallace, W.H.; Caron, H.N.; Armenian, S.H.; et al. A worldwide collaboration to harmonize guidelines for the long-term follow-up of childhood and young adult cancer survivors: A report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Pediatr. Blood Cancer 2013, 60, 543–549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Landier, W.; Bhatia, S.; Eshelman, D.A.; Forte, K.J.; Sweeney, T.; Hester, A.L.; Darling, J.; Armstrong, F.D.; Blatt, J.; Constine, L.S.; et al. Development of risk-based guidelines for pediatric cancer survivors: The Children’s Oncology Group Long-Term Follow-Up Guidelines from the Children’s Oncology Group Late Effects Committee and Nursing Discipline. J. Clin. Oncol. 2004, 22, 4979–4990. [Google Scholar] [CrossRef] [PubMed]
- Dutch Childhood Oncology Group. Richtlijn Follow-Up na Kinderkanker Meer dan 5 Jaar na Diagnose. Available online: https://www.dcog-ectc.nl (accessed on 1 October 2021).
- Improving Patient Care through Evidence-Based Guidelines. Available online: http://www.sign.ac.uk/ (accessed on 1 October 2021).
- CCLG. Available online: http://www.cclg.org.uk/ (accessed on 1 October 2021).
- Children’s Oncology Group. Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent and Young Adult Cancers: Version 5.0; Children’s Oncology Group: Monrovia, CA, USA, 2018; Available online: www.survivorshipguidelines.org (accessed on 1 October 2018).
- Ehrhardt, M.J.; Ward, Z.J.; Liu, Q.; Chaudhry, A.; Nohria, A.; Border, W.; Fulbright, J.M.; Mulrooney, D.A.; Oeffinger, K.C.; Nathan, P.C.; et al. Cost-Effectiveness of the International Late Effects of Childhood Cancer Guideline Harmonization Group Screening Guidelines to Prevent Heart Failure in Survivors of Childhood Cancer. J. Clin. Oncol. 2020, 38, 3851–3862. [Google Scholar] [CrossRef]
- Yeh, J.M.; Nohria, A.; Diller, L. Routine echocardiography screening for asymptomatic left ventricular dysfunction in childhood cancer survivors: A model-based estimation of the clinical and economic effects. Ann. Intern. Med. 2014, 160, 661–671. [Google Scholar] [CrossRef] [Green Version]
- Barac, A.; Murtagh, G.; Carver, J.R.; Chen, M.H.; Freeman, A.M.; Herrmann, J.; Iliescu, C.; Ky, B.; Mayer, E.L.; Okwuosa, T.M.; et al. Cardiovascular Health of Patients with Cancer and Cancer Survivors: A Roadmap to the Next Level. J. Am. Coll. Cardiol. 2015, 65, 2739–2746. [Google Scholar] [CrossRef] [Green Version]
- Rodriguez-Galindo, C.; Friedrich, P.; Alcasabas, P.; Antillon, F.; Banavali, S.; Castillo, L.; Israels, T.; Jeha, S.; Harif, M.; Sullivan, M.J.; et al. Toward the Cure of All Children with Cancer Through Collaborative Efforts: Pediatric Oncology as a Global Challenge. J. Clin. Oncol. 2015, 33, 3065–3073. [Google Scholar] [CrossRef] [PubMed]
- Bakeer, N.; James, J.; Roy, S.; Wansapura, J.; Shanmukhappa, S.K.; Lorenz, J.N.; Osinska, H.; Backer, K.; Huby, A.C.; Shrestha, A.; et al. Sickle cell anemia mice develop a unique cardiomyopathy with restrictive physiology. Proc. Natl. Acad. Sci. USA 2016, 113, E5182–E5191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Musa, B.M.; Galadanci, N.A.; Coker, M.; Bussell, S.; Aliyu, M.H. The global burden of pulmonary hypertension in sickle cell disease: A systematic review and meta-analysis. Ann. Hematol. 2016, 95, 1757–1764. [Google Scholar] [CrossRef]
- Ristow, B.; Schiller, N.B. Pulmonary hypertension in sickle cell disease. N. Engl. J. Med. 2011, 365, 1645–1646. [Google Scholar] [CrossRef] [Green Version]
- Sachdev, V.; Machado, R.F.; Shizukuda, Y.; Rao, Y.N.; Sidenko, S.; Ernst, I.; St Peter, M.; Coles, W.A.; Rosing, D.R.; Blackwelder, W.C.; et al. Diastolic dysfunction is an independent risk factor for death in patients with sickle cell disease. J. Am. Coll. Cardiol. 2007, 49, 472–479. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Types of Anticancer Therapy | Examples Used for Pediatric Cancers | Cardiovascular Toxicities |
|---|---|---|
| Alkylating agents | Cyclophosphamide | Arrhythmias Endothelial dysfunction Pericardial effusions Thrombosis |
| Anthracyclines | Doxorubicin Daunorubicin | Dysrhythmias Endothelial dysfunction Cardiomyopathy (acute, usually reversible) Cardiomyopathy (chronic, usually non-reversible) Oxidative stress |
| Antimetabolites | Cisplatin 5-Fluorouracil | Dysrhythmias Myocardial ischemia |
| Immune-based therapies | Immune checkpoint inhibitors Chimeric antigen receptor T-cell therapy | Arterial hypertension Cardiomyopathy (acute, usually reversible) Cardiomyopathy (chronic, usually non-reversible) Cytokine release syndrome Dysrhythmias Endothelial dysfunction Pericardial effusions QTc prolongation Thrombosis |
| Radiation therapies | Proton radiation Photon radiation | Arterial hypertension Increase pulmonary vasoreactivity Cardiomyopathy (acute, usually reversible) Cardiomyopathy (chronic, usually non-reversible) Pericarditis |
| Tyrosine kinase inhibitors | Pazopanib Trametinib Sorafenib | Arterial hypertension Cardiomyopathy (acute, usually reversible) Dysrhythmias Endothelial dysfunction Pericardial effusions QTc prolongation Thrombosis |
| Vinca alkaloids | Vincristine Vinblastine | Myocardial ischemia |
| Primary Reason for Consultation | Percentage Representation |
|---|---|
| Diastolic dysfunction | 31.8% |
| Dysrhythmias | 15.6% |
| Systolic dysfunction | 12.4% |
| Systemic arterial hypertension | 10.1% |
| Pericardial disease | 9.6% |
| Thromboembolic phenomena | 8.9% |
| Pulmonary arterial hypertension | 5.6% |
| PedCO Stage | Description | PedCO Characteristics | Therapeutic Options |
|---|---|---|---|
| A | Patients at high risk to develop cardiovascular (CV) toxicity | -Anticancer therapy exposure without signs of pathologic cardiac remodeling or vascular toxicity -Patients scheduled to receive anticancer modalities associated with CV injury -Personal history of CV disease (e.g., diabetes, dyslipidemia, carriers of pathogenic gene variants associated with CV disease) | Primary prevention includes: -Encouraging regular exercise -Management of dyslipidemia, diabetes, and physical deconditioning -Avoidance of alcohol, illicit drugs, and smoking |
| B | Patients manifesting CV toxicity with no symptoms of heart failure | -Patients with subclinical systolic dysfunction (by ejection fraction or strain analysis), diastolic dysfunction, systemic or pulmonary hypertension, or abnormally elevated cardiac biomarkers | -Include primary prevention recommendations under stage A -Secondary prevention, includes the institution of medical therapy for CTRCD |
| C | Patients manifesting symptoms of CV toxicity | -Patients with symptoms associated with cancer therapy-related cardiovascular dysfunction | -Include recommendations under stage A and B in addition to managing symptoms of CTRCD (inpatient or outpatient) |
| D | Advanced CV disease requiring hospital-based support | -Patients with cancer therapy-related CV dysfunction requiring hospital-based support | -Include recommendations under stages A, B, and C -Escalation of care to hospital/intensive care |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martinez, H.R.; Beasley, G.S.; Goldberg, J.F.; Absi, M.; Ryan, K.A.; Guerrier, K.; Joshi, V.M.; Johnson, J.N.; Morin, C.E.; Hurley, C.; et al. Pediatric Cardio-Oncology Medicine: A New Approach in Cardiovascular Care. Children 2021, 8, 1200. https://doi.org/10.3390/children8121200
Martinez HR, Beasley GS, Goldberg JF, Absi M, Ryan KA, Guerrier K, Joshi VM, Johnson JN, Morin CE, Hurley C, et al. Pediatric Cardio-Oncology Medicine: A New Approach in Cardiovascular Care. Children. 2021; 8(12):1200. https://doi.org/10.3390/children8121200
Chicago/Turabian StyleMartinez, Hugo R., Gary S. Beasley, Jason F. Goldberg, Mohammed Absi, Kaitlin A. Ryan, Karine Guerrier, Vijaya M. Joshi, Jason N. Johnson, Cara E. Morin, Caitlin Hurley, and et al. 2021. "Pediatric Cardio-Oncology Medicine: A New Approach in Cardiovascular Care" Children 8, no. 12: 1200. https://doi.org/10.3390/children8121200
APA StyleMartinez, H. R., Beasley, G. S., Goldberg, J. F., Absi, M., Ryan, K. A., Guerrier, K., Joshi, V. M., Johnson, J. N., Morin, C. E., Hurley, C., Morrison, R. R., Rai, P., Hankins, J. S., Bishop, M. W., Triplett, B. M., Ehrhardt, M. J., Pui, C.-H., Inaba, H., & Towbin, J. A. (2021). Pediatric Cardio-Oncology Medicine: A New Approach in Cardiovascular Care. Children, 8(12), 1200. https://doi.org/10.3390/children8121200









