Relapse of Neonatal Escherichia coli Meningitis: Did We Miss Something at First?
Abstract
:1. Introduction
2. Cases
3. Discussion
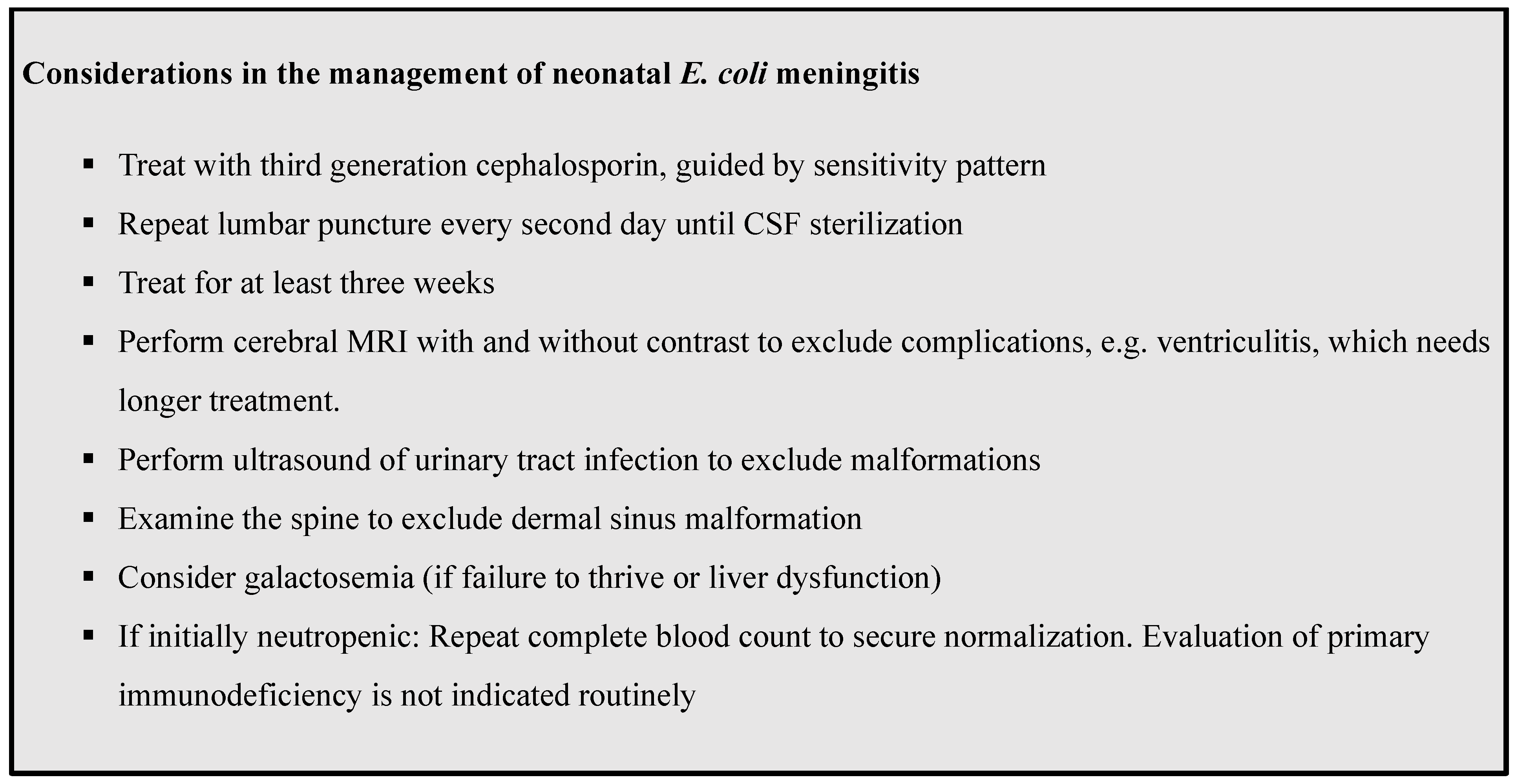
Treatment
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Case 1 |
| A female born prematurely at gestational age (GA) 36 weeks + 3 days, birth weight (BW) 2130 g, admitted to the neonatal department. Presented at age 3 days with fever and drowsiness with elevated inflammatory parameters (CRP 123 mg/L) and was treated with cefuroxime and gentamicin in suspicion of sepsis. After 24 h, she was irritable and shivering and therapy was changed to meningitis treatment (cefotaxime, ampicillin, and gentamicin). Lumbar puncture was performed after 58 h of treatment and cerebrospinal fluid (CSF) grew E. coli sensitive to cefotaxime. Cefotaxime was continued as monotherapy for 21 days. Cerebral magnetic resonance imaging (MRI) at completion of therapy was normal except for two very minor bleedings. The girl was thriving. Four days after completion of antibiotic treatment, the girl was readmitted with fever, respiratory distress, and cardiac failure, and referred to intensive care unit for mechanical ventilation, inotropes, and empirically treated for meningitis with cefotaxime and gentamicin. Blood culture was positive for E. coli sensitive to cefotaxime. CSF examination was postponed to day 3 of relapse due to clinical instability. It was culture negative, but with elevated CSF white blood cells (722 mill/L) and marked hypoglycorrhachia (0.0), a high percentage of neutrophiles (375 mill/L= 49%), and elevated CSF protein 2.29 g/L, all suggestive of acute infection in the CNS. Antibiotic therapy was changed to ceftriaxone monotherapy for 9 weeks. At follow-up, the girl had normal neurological development and no apparent sequelae to the infection. |
| Case 2 |
| A male born prematurely at GA 34 + 0, BW 1980 g, admitted to the neonatal department. Presented at age 5 days with drowsiness and elevated inflammatory parameters (CRP 145 mg/L) and was treated with ampicillin and gentamicin in suspicion of sepsis. After 24 h, therapy was changed to cefotaxime and ampicillin due to clinical worsening, and lumbar puncture was performed. CSF culture was positive for E. coli, sensitive to third generation cephalosporins. Transfontanellar ultrasound showed thickened meninges. Cefotaxime was continued for 3 weeks. Urinary tract ultrasound was normal. MRI of cerebrum and repeat TFU was normal. A lumbar puncture was performed at the end of treatment showed elevated WBC 111 mill/L and protein 1,67 g/L with negative culture. At discharge, the boy was thriving. Eleven days after completion of antibiotic therapy, the boy was readmitted due to severe vomiting and irritability. He was treated with cefotaxime and gentamicin in suspicion of relapsing meningitis. Blood and CSF cultures were positive E. coli, sensitive to third generation cephalosporins. The E. coli strain was typed as K1. Repeated lumbar puncture after 36 h was without bacterial growth. MRI of cerebrum and spine and ultrasound of urinary tract and abdomen were normal. Ceftriaxone was continued for 12 weeks. At follow-up, the boy had normal neurological development and no sequelae to the infection. |
| Case 3 |
| A male born prematurely at GA 34 + 5, BW 2280 g without neonatal complications. Admitted from home at age 6 weeks (corrected GA 41 + 4) with fever and septic appearance and was treated with ampicillin, gentamicin, and cefotaxime in suspicion of meningitis and transferred to intensive care unit. Blood culture was drawn at admission and was positive for E. coli. Lumbar puncture was performed 21 h after initiation of antibiotics and was also positive for E. coli, sensitive to third generation cephalosporins. Cerebral MRI showed ischemic changes of cortical parenchyma, but no signs of abscess or ventriculitis. Cefotaxime was continued for 21 days. A lumbar puncture was performed at the end of treatment, showing elevated WBC (110 mill/L) and protein (1.72 g/L) with negative culture and PCR. Four weeks after completion of antibiotic therapy, the boy was readmitted with fever and irritability. He was treated with ampicillin and ceftriaxone in suspicion of relapsing meningitis. Blood culture was positive for E. coli, sensitive to third generation cephalosporins. CSF culture was negative, but PCR positive for E. coli. The whole genome sequenced of the strain was found to be identical to the previous episode of E. coli meningitis. Treatment was changed to ceftriaxone monotherapy for a total of 8 weeks as out-patient therapy after stabilization. Repeated CSF cultures at day 38 and 47 were negative. MRI of cerebrum and spine showed signs of ventriculitis and cortical changes from the former episode of meningitis. MRI of abdomen was normal. At follow-up, the boy had moderately delayed neurological development, but no signs of hydrocephalus or cerebral palsy. |
| Case 4 |
| A female born at term at GA 37 + 1, BW 2940 g without neonatal complications. Admitted from home at age 13 days with drowsiness, irritability, poor feeding, and elevated inflammatory parameters (CRP 57 g/L), and treated with gentamicin, ampicillin, and cefotaxime in suspicion for meningitis. Blood culture was positive for E. coli, sensitive to third generation cephalosporins. CSF obtained 48 h after initiated therapy was positive for E coli. Cefotaxime was continued as monotherapy for 21 days. An MRI at completion of therapy was normal except for signs of very minor bleedings. Two days after completion of antibiotic treatment, the patient was readmitted with irritability and rising CRP (53 mg/L). She was treated with gentamicin, ampicillin, and cefotaxime in suspicion of relapsing meningitis. CSF culture was positive for E. coli, sensitive to third generation cephalosporins. The treatment was changed to meropenem and ciprofloxacin. Cerebral MRI showed bilateral minor empyema and early stage of communicating hydrocephalus. MRI was repeated 4 weeks later with regression of both empyema and hydrocephalus. Urinary tracts ultrasound was normal. Repeated CSF culture at day 12 was negative. Ciprofloxacin and meropenem were discontinued after 6 weeks of treatment and changed to ceftriaxone for an additional 3 weeks as out-patient therapy. CSF culture 3 days after the end of treatment was negative. At follow-up, the girl had normal neurological development and no sequelae to the infection. |
References
- Anderson, S.G.; Gilbert, G.L. Neonatal Gram Negative Meningitis: A 10-Year Review, with Reference to Outcome and Relapse of Infection. J. Paediatr. Child Health 1990, 26, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Unhanand, M.; Mustafa, M.M.; McCracken, G.H.; Nelson, J.D. Gram-Negative Enteric Bacillary Meningitis: A Twenty-One-Year Experience. J. Pediatr. 1993, 122, 15–21. [Google Scholar] [CrossRef]
- Heath, P.T.; Yusoff, N.K.N.; Baker, C.J. Neonatal Meningitis. Arch. Dis. Child.-Fetal Neonatal Ed. 2003, 88, F173–F178. [Google Scholar] [CrossRef] [PubMed]
- Sarah, S. Long Principles and Practice of Pediatric Infectious Diseases, 3rd ed.; Churchill Livingstone: London, UK, 2012. [Google Scholar]
- National Collaborating Centre for Women’s and Children’s Health (UK). Bacterial Meningitis and Meningococcal Septicaemia: Management of Bacterial Meningitis and Meningococcal Septicaemia in Children and Young People Younger than 16 Years in Primary and Secondary Care; National Institute for Health and Clinical Excellence: Guidance; RCOG Press: London, UK, 2010. [Google Scholar]
- Agarwal, R.; Emmerson, A.J. Should Repeat Lumbar Punctures Be Routinely Done in Neonates with Bacterial Meningitis? Results of a Survey into Clinical Practice. Arch. Dis. Child. 2001, 84, 451–452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greenberg, R.G.; Benjamin, D.K., Jr.; Cohen-Wolkowiez, M.; Clark, R.H.; Cotten, C.M.; Laughon, M.; Smith, P.B. Repeat Lumbar Punctures in Infants with Meningitis in the Neonatal Intensive Care Unit. J. Perinatol. 2011, 31, 425–429. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Basmaci, R.; Bonacorsi, S.; Bidet, P.; Biran, V.; Aujard, Y.; Bingen, E.; Béchet, S.; Cohen, R.; Levy, C. Escherichia Coli Meningitis Features in 325 Children From 2001 to 2013 in France. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2015, 61, 779–786. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ouchenir, L.; Renaud, C.; Khan, S.; Bitnun, A.; Boisvert, A.-A.; McDonald, J.; Bowes, J.; Brophy, J.; Barton, M.; Ting, J.; et al. The Epidemiology, Management, and Outcomes of Bacterial Meningitis in Infants. Pediatrics 2017, 140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tauzin, M.; Ouldali, N.; Lévy, C.; Béchet, S.; Cohen, R.; Caeymaex, L. Combination Therapy with Ciprofloxacin and Third-Generation Cephalosporin versus Third-Generation Cephalosporin Monotherapy in Escherichia Coli Meningitis in Infants: A Multicentre Propensity Score-Matched Observational Study. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2018. [Google Scholar] [CrossRef] [PubMed]
- Lak, R.; Yazdizadeh, B.; Davari, M.; Nouhi, M.; Kelishadi, R. Newborn Screening for Galactosaemia. Cochrane Database Syst. Rev. 2020, 6, CD012272. [Google Scholar] [CrossRef] [PubMed]
- Schaad, U.B.; Nelson, J.D.; McCracken, G.H. Recrudescence and Relapse in Bacterial Meningitis of Childhood. Pediatrics 1981, 67, 188–195. [Google Scholar] [PubMed]
- Tebruegge, M.; Curtis, N. Epidemiology, Etiology, Pathogenesis, and Diagnosis of Recurrent Bacterial Meningitis. Clin. Microbiol. Rev. 2008, 21, 519–537. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Case | First E. coli Meningitis | Relapse E. coli Meningitis | Follow-Up | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sex | GA at birth (weeks) | BW (gram) | Age (days) | Treatment | Cerebral MRI | Urinary ultra-sound | Time from completion (days) | Treatment | Age (years) | Under-lying disease | Sequelae * | |
| 1 | F | 36 + 3 | 2130 | 3 | Cefotaxime 21 days + gentamicin day 1–5 | Minor hemorrhagic parenchymal infarctions. No signs of infection. (without contrast) | Normal | 4 | Meropenem 1 week followed by ceftriaxone 9 weeks | 4.0 | No | No |
| 2 | M | 34 + 0 | 1980 | 5 | Cefotaxime 21 days + gentamicin day 1–3 | Normal (with contrast) | Normal | 11 | Cefotaxime 1 week, meropenem 1 week followed by ceftriaxone 12 weeks | 3.5 | No | No |
| 3 | M | 34 + 5 | 2280 | 45 | Cefotaxime 20 days + gentamicin day 1–7 | Ischemic changes of cortical parenchyma. No signs of infection. (without contrast) | Normal | 28 | Ceftriaxone 8 weeks | 3.5 | No | Moderate sensory disabilities, visual impairment, delayed development. No signs of hydrocephalus or cerebral palsy. Persistent changes on MRI. |
| 4 | F | 37 + 1 | 2940 | 13 | Cefotaxime 22 days + gentamicin day 1–3 | Minor hemorrhagic parenchymal infarctions. No signs of infection. (without contrast) | Normal | 2 | Meropenem + ciprofloxacin 6 weeks followed by ceftriaxone 3 weeks | 4.0 | No | No |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vissing, N.H.; Mønster, M.B.; Nordly, S.; Dayani, G.K.; Heedegaard, S.S.; Knudsen, J.D.; Nygaard, U. Relapse of Neonatal Escherichia coli Meningitis: Did We Miss Something at First? Children 2021, 8, 126. https://doi.org/10.3390/children8020126
Vissing NH, Mønster MB, Nordly S, Dayani GK, Heedegaard SS, Knudsen JD, Nygaard U. Relapse of Neonatal Escherichia coli Meningitis: Did We Miss Something at First? Children. 2021; 8(2):126. https://doi.org/10.3390/children8020126
Chicago/Turabian StyleVissing, Nadja H., Mette B. Mønster, Sannie Nordly, Gholamreza K. Dayani, Sofie S. Heedegaard, Jenny D. Knudsen, and Ulrikka Nygaard. 2021. "Relapse of Neonatal Escherichia coli Meningitis: Did We Miss Something at First?" Children 8, no. 2: 126. https://doi.org/10.3390/children8020126






