Pulmonary Vein Stenosis: A Rare Disease with a Global Reach
Abstract
:1. Introduction
2. Materials and Methods
3. Results
Case Descriptions
“The patient was a 1 month old, ex-33 week gestation, child with failure to thrive. She was diagnosed with supracardiac TAPVR which was obstructed at the entry into the vertical vein. She underwent urgent repair of at 1 month of age at another tertiary care hospital. 3 months following surgery, an echocardiogram revealed mild to moderate pulmonary vein stenosis at the pulmonary anastomotic site for which she was transferred to the National Heart Institute. A CT revealed all pulmonary veins draining into the left atrium with severe stenosis at the pulmonary vein confluence to left atrium anastomosis. A re-operation was performed to relieve the pulmonary vein stenosis 9 months following the initial surgery using the sutureless technique. On discharge the echocardiogram showed a wide open pulmonary venous confluence with no gradient across the anastomotic site (Figure 2).”—Sivakumar Sivalingam, FRCS(C.Th), Clinical Director Congenital Heart Surgery, Kuala Lumpur, Malaysia
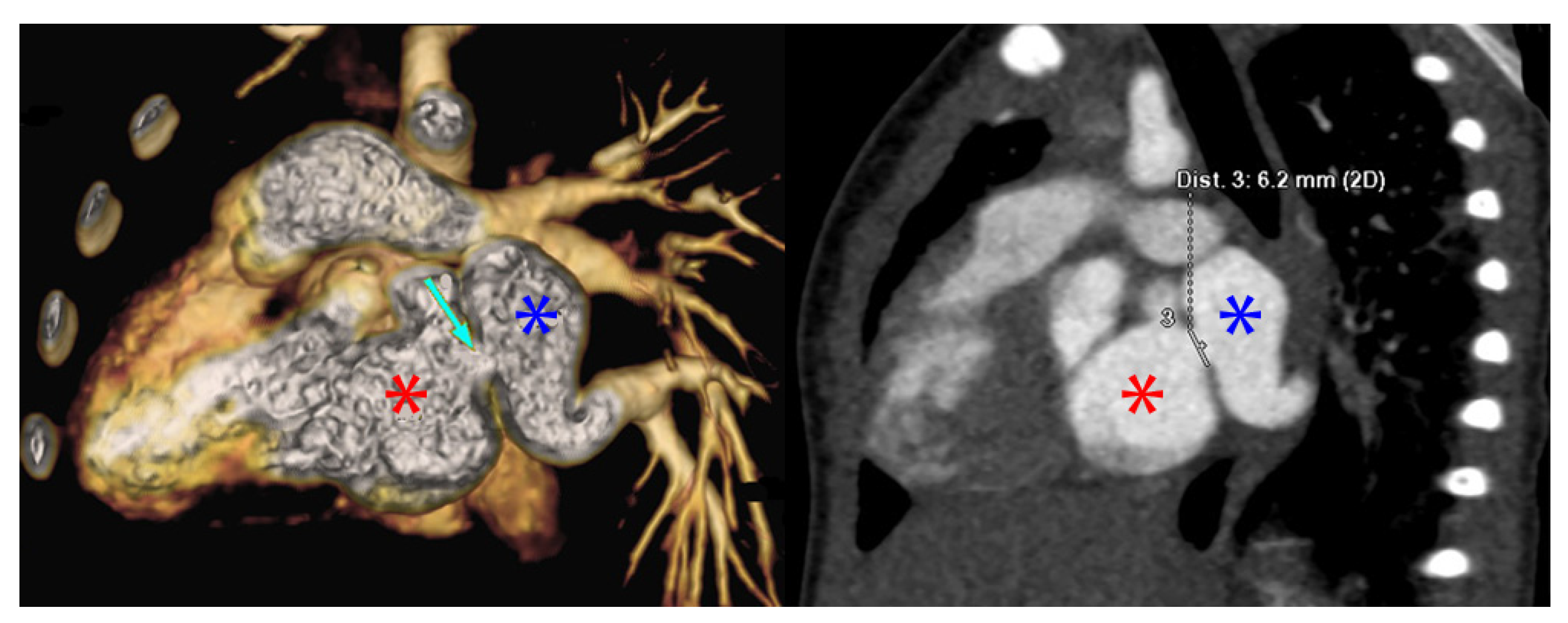
“The patient was a 9-month-old who presented due to cough and shortness of breath. An echocardiogram revealed a small perimembranous ventricular septal defect (VSD) that was not hemodynamically significant and routine follow up was recommended. She continued to have respiratory difficulty at home and re-presented. A repeat echocardiogram re-demonstrated the VSD and showed left pulmonary vein stenosis. She was admitted for a CT which showed 2 left pulmonary veins to a common left pulmonary vein with stenosis at the common vein to left atrial connection. Right pulmonary veins were normal. She underwent VSD closure and sutureless anastomosis for left pulmonary veins 2 months later. The repair was delayed because of other urgent cases at the institution (Figure 3).”—Dinh Quang Le Thanh, MD, MS, Pediatric General and Cardiac Surgeon, Children’s Hospital 1, Ho Chi Minh City, Vietnam
“The patient was an ex-full term 2-month-old who was admitted for a genetic syndrome evaluation and poor weight gain. He was hypoxemic with cardiomegaly on chest X-ray prompting an echocardiogram which revealed a VSD with pulmonary vein hypoplasia and stenosis. A CT done at that time revealed ostial stenosis of the pulmonary veins. The child underwent VSD closure and removal of the pulmonary venous membrane. He did well post-operatively, but was re-admitted to the cardiac intensive care unit 1 month later due to tachypnea and work of breathing. Repeat echocardiogram and CT demonstrated recurrent stenosis, right lower pulmonary vein hypoplasia, and right upper pulmonary vein atresia. Due to the rapidly progressive stenosis despite treatment, the child was deemed not a surgical candidate and was transferred to palliative care.”—Guillermo Moreno, MD, Head of Cardiac Intensive Care Unit, Hospital de Pediatria Professor Dr. Juan P Garrahan, Buenos Aires, Argentina
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nasr, V.G.; Callahan, R.; Wichner, Z.; Odegard, K.C.; DiNardo, J.A. Intraluminal Pulmonary Vein Stenosis in Children: A “New” Lesion. Anesth. Analg. 2019, 129, 27–40. [Google Scholar] [CrossRef]
- Quinonez, L.G.; Gauvreau, K.; Borisuk, M.; Ireland, C.; Marshall, A.M.; Mayer, J.E.; Jenkins, K.J.; Fynn-Thompson, F.E.; Baird, C.W. Outcomes of surgery for young children with multivessel pulmonary vein stenosis. J. Thorac. Cardiovasc. Surg. 2015, 150, 911–917. [Google Scholar] [CrossRef] [Green Version]
- Sadr, I.M.; Tan, P.E.; Kieran, M.W.; Jenkins, K.J. Mechanism of pulmonary vein stenosis in infants with normally connected veins. Am. J. Cardiol. 2000, 86, 577–579. [Google Scholar] [CrossRef]
- Riedlinger, W.F.J.; Juraszek, A.L.; Jenkins, K.J.; Nugent, A.W.; Balasubramanian, S.; Calicchio, M.L.; Kieran, M.W.; Collins, T. Pulmonary vein stenosis: Expression of receptor tyrosine kinases by lesional cells. Cardiovasc. Pathol. 2006, 15, 91–99. [Google Scholar] [CrossRef]
- Kato, H.; Fu, Y.Y.; Zhu, J.; Wang, L.; Aafaqi, S.; Rahkonen, O.; Slorach, C.; Traister, A.; Leung, C.H.; Chiasson, D.; et al. Pulmonary vein stenosis and the pathophysiology of “upstream” pulmonary veins. J. Thorac. Cardiovasc. Surg. 2014, 148, 245–253. [Google Scholar] [CrossRef] [Green Version]
- Pogoriler, J.E.; Kulik, T.J.; Casey, A.M.; Baird, C.W.; Mullen, M.P.; Jenkins, K.J.; Vargas, S.O. Lung Pathology in Pediatric Pulmonary Vein Stenosis. Pediatric Dev. Pathol. 2016, 19, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Kovach, A.E.; Magcalas, P.M.; Ireland, C.; McEnany, K.; Oliveira, A.M.; Kieran, M.W.; Baird, C.W.; Jenkins, K.; Vargas, S.O. Paucicellular Fibrointimal Proliferation Characterizes Pediatric Pulmonary Vein Stenosis: Clinicopathologic Analysis of 213 Samples From 97 Patients. Am. J. Surg. Pathol. 2017, 41, 1198–1204. [Google Scholar] [CrossRef]
- Callahan, R.; Kieran, M.W.; Baird, C.W.; Colan, S.D.; Gauvreau, K.; Ireland, C.M.; Marshall, A.C.; Sena, L.M.; Vargas, S.O.; Jenkins, K.J. Adjunct Targeted Biologic Inhibition Agents to Treat Aggressive Multivessel Intraluminal Pediatric Pulmonary Vein Stenosis. J. Pediatrics 2018, 198, 29–35. [Google Scholar] [CrossRef]
- Zimmerman, M.S.; Smith, A.G.C.; Sable, C.A.; Echko, M.M.; Wilner, L.B.; Olsen, H.E.; Atalay, H.T.; Awasthi, A.; Bhutta, Z.A.; Boucher, J.L.; et al. Global, regional, and national burden of congenital heart disease, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Child Adolesc. Health 2020, 4, 185–200. [Google Scholar] [CrossRef] [Green Version]
- Sen, A.C.; Morrow, D.F.; Balachandran, R.; Du, X.; Gauvreau, K.; Jagannath, B.R.; Kumar, R.K.; Kupiec, J.K.; Melgar, M.L.; Chau, N.T.; et al. Postoperative Infection in Developing World Congenital Heart Surgery Programs: Data From the International Quality Improvement Collaborative. Circ. Cardiovasc. Qual. Outcomes 2017, 10. [Google Scholar] [CrossRef] [PubMed]
- Hickey, P.A.; Connor, J.A.; Cherian, K.M.; Jenkins, K.; Doherty, K.; Zhang, H.; Gaies, M.; Pasquali, S.; Tabbutt, S.; St. Louis, J.D.; et al. International quality improvement initiatives. Cardiol. Young 2017, 27, S61–S68. [Google Scholar] [CrossRef]
- Schidlow, D.N.; Jenkins, K.J.; Gauvreau, K.; Croti, U.A.; Giang, D.T.C.; Konda, R.K.; Novick, W.M.; Sandoval, N.F.; Castañeda, A. Transposition of the Great Arteries in the Developing World: Surgery and Outcomes. J. Am. Coll. Cardiol. 2017, 69, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, K.J.; Castañeda, A.R.; Cherian, K.M.; Couser, C.A.; Dale, E.K.; Gauvreau, K.; Hickey, P.A.; Koch Kupiec, J.; Morrow, D.F.; Novick, W.M.; et al. Reducing mortality and infections after congenital heart surgery in the developing world. Pediatrics 2014, 134, e1422–e1430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, C.; Gauvreau, K.; Levy, P.; Callahan, R.; Jenkins, K.J.; Chen, M. Longer Exposure to Left-to-Right Shunts Is a Risk Factor for Pulmonary Vein Stenosis in Patients with Trisomy 21. Children 2021, 8, 19. [Google Scholar] [CrossRef]
- DiLorenzo, M.P.; Santo, A.; Rome, J.J.; Zhang, H.; Faerber, J.A.; Mercer-Rosa, L.; Hopper, R.K. Pulmonary Vein Stenosis: Outcomes in Children With Congenital Heart Disease and Prematurity. Semin. Thorac. Cardiovasc. Surg. 2019, 31, 266–273. [Google Scholar] [CrossRef] [PubMed]
- Seale, A.N.; Webber, S.A.; Uemura, H.; Partridge, J.; Roughton, M.; Ho, S.Y.; McCarthy, K.P.; Jones, S.; Shaughnessy, L.; Sunnegardh, J.; et al. Pulmonary vein stenosis: The UK, Ireland and Sweden collaborative study. Heart 2009, 95, 1944–1949. [Google Scholar] [CrossRef]
- Kalfa, D.; Belli, E.; Bacha, E.; Lambert, V.; di Carlo, D.; Kostolny, M.; Salminen, J.; Nosal, M.; Poncelet, A.; Horer, J.; et al. Primary Pulmonary Vein Stenosis: Outcomes, Risk Factors, and Severity Score in a Multicentric Study. Ann. Thorac. Surg. 2017, 104, 182–189. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Backes, C.H.; Nealon, E.; Armstrong, A.K.; Cua, C.L.; Mitchell, C.; Krishnan, U.; Vanderlaan, R.D.; Song, M.K.; Viola, N.; Smith, C.V.; et al. Pulmonary Vein Stenosis in Infants: A Systematic Review, Meta-Analysis, and Meta-Regression. J. Pediatrics 2018, 198, 36–45. [Google Scholar] [CrossRef]
- Azakie, A.; Lavrsen, M.J.; Johnson, N.C.; Sapru, A. Early outcomes of primary sutureless repair of the pulmonary veins. Ann. Thorac. Surg. 2011, 92, 666–671. [Google Scholar] [CrossRef] [PubMed]
- Viola, N.; Alghamdi, A.A.; Perrin, D.G.; Wilson, G.J.; Coles, J.G.; Caldarone, C.A. Primary pulmonary vein stenosis: The impact of sutureless repair on survival. J. Thorac. Cardiovasc. Surg. 2011, 142, 344–350. [Google Scholar] [CrossRef] [Green Version]
- Sandoval, N.; Carreño, M.; Novick, W.M.; Agarwal, R.; Ahmed, I.; Balachandran, R.; Balestrini, M.; Cherian, K.M.; Croti, U.; Du, X.; et al. Tetralogy of Fallot Repair in Developing Countries: International Quality Improvement Collaborative. Ann. Thorac. Surg. 2018, 106, 1446–1451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yun, T.J.; Coles, J.G.; Konstantinov, I.E.; Al-Radi, O.O.; Wald, R.M.; Guerra, V.; de Oliveira, N.C.; Van Arsdell, G.S.; Williams, W.G.; Smallhorn, J.; et al. Conventional and sutureless techniques for management of the pulmonary veins: Evolution of indications from postrepair pulmonary vein stenosis to primary pulmonary vein anomalies. J. Thorac. Cardiovasc. Surg. 2005, 129, 167–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Institution |
|---|
| Shanghai Children’s Medical Center (Shanghai, China) |
| TEDA International Cardiovascular Hospital (Tianjin China) |
| First Hospital of Lanzhou University (Lanzhou, Gansu Province, China) |
| Nhi Dong 1 (Children’s Hospital #1) (Ho Chi Minh City, Vietnam) |
| Vietnam National Children’s Hospital (Hanoi, Vietnam) |
| Tam Duc Heart Hospital (Ho Chi Minh City, Vietnam) |
| Institut Jantung Negara (Kuala Lumpur, Malaysia) |
| Amrita Institute of Medical Science (Kochi, India) |
| Kokilaben Dhirubhai Ambani Hospital & Medical Research Center (Mumbai, India) |
| Frontier Lifeline Hospital (Chennai, India) |
| G. Kuppuswamy Naidu Memorial Hospital (Coimbatore, India) |
| Fortis Child Heart Mission, Fortis Hospital, Mulund (Mumbai, India) |
| Mother and Child Health Institute (Belgrade, Serbia) |
| Hospital Garrahan (Buenos Aires, Argentina) |
| Hospital de Niños (Córdoba, Argentina) |
| Clínica Cardio VID (Medellin, Columbia) |
| Fundación Cardioinfantil de Bogota (Bogota, Colombia) |
| Fundación Valle del Lili (Cali, Colombia) |
| Hospital do Coração (Sao Paolo, Brazil) |
| Instituto do Coração (Sao Paolo, Brazil) |
| Dr. Carlos Alberto Studart Gomes Hospital (Fortaleza, Brazil) |
| Hospital de criança e Maternidade (Sao Jose do Rio Preto, Brazil) |
| Instituto Nacional de Pediatría Mexico City, Mexico |
| Hospital Nacional de Niños (San Jose, Costa Rica) |
| Variable | Percentage of Total or Median (n or IQR) |
|---|---|
| Age <1 year | 57.9% (33) |
| Age 1–5 years | 26.3% (15) |
| Age 6–14 years | 15.8% (9) |
| % Male | 56.1% (32) |
| Prematurity | 10.5% (6) |
| Major non-cardiac structural anomaly | 3.5% (2) |
| Major chromosomal anomaly | 3.5% (2) |
| Major medical illness | 7.0% (4) |
| Weight | 6.0 kg (4.5–9.5 kg) |
| Hematocrit | 36% (33–40%) |
| Systemic saturation | 95% (90–99%) |
| Primary Procedure | Number | Percentage of Total Cohort (n = 57) |
|---|---|---|
| Isolated PVS repair | 17 | 29.8% |
| Anomalous pulmonary vein repair | 20 | 35.1% |
| Left to right shunt repair | 15 | 26.3% |
| VSD repair | 5 | |
| ASD repair | 5 | |
| VSD and ASD repair | 2 | |
| Transitional AV Canal repair | 2 | |
| PDA ligation | 1 | |
| Pulmonary outflow tract obstruction relief | 4 | 7% |
| Bidirectional Glenn | 2 | 3.6% |
| Outcome | Percent or Number of Patients with Outcome |
|---|---|
| Infections | 10.5% (n = 6) |
| Bacterial sepsis | 4 |
| Surgical site infection | 1 |
| Both | 1 |
| Mortality | |
| In hospital mortality | 17.5% (n = 10) |
| 30-day mortality | 21.6% * (n = 11) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schramm, J.; Sivalingam, S.; Moreno, G.E.; Thanh, D.Q.L.; Gauvreau, K.; Doherty-Schmeck, K.; Jenkins, K.J. Pulmonary Vein Stenosis: A Rare Disease with a Global Reach. Children 2021, 8, 198. https://doi.org/10.3390/children8030198
Schramm J, Sivalingam S, Moreno GE, Thanh DQL, Gauvreau K, Doherty-Schmeck K, Jenkins KJ. Pulmonary Vein Stenosis: A Rare Disease with a Global Reach. Children. 2021; 8(3):198. https://doi.org/10.3390/children8030198
Chicago/Turabian StyleSchramm, Jennifer, Sivakumar Sivalingam, Guillermo E. Moreno, Dinh Quang Le Thanh, Kimberlee Gauvreau, Kaitlin Doherty-Schmeck, and Kathy J. Jenkins. 2021. "Pulmonary Vein Stenosis: A Rare Disease with a Global Reach" Children 8, no. 3: 198. https://doi.org/10.3390/children8030198
APA StyleSchramm, J., Sivalingam, S., Moreno, G. E., Thanh, D. Q. L., Gauvreau, K., Doherty-Schmeck, K., & Jenkins, K. J. (2021). Pulmonary Vein Stenosis: A Rare Disease with a Global Reach. Children, 8(3), 198. https://doi.org/10.3390/children8030198








