Weight Is More Accurate than Gestational Age When Estimating the Optimal Endotracheal Tube Depth in Neonates
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Subjects
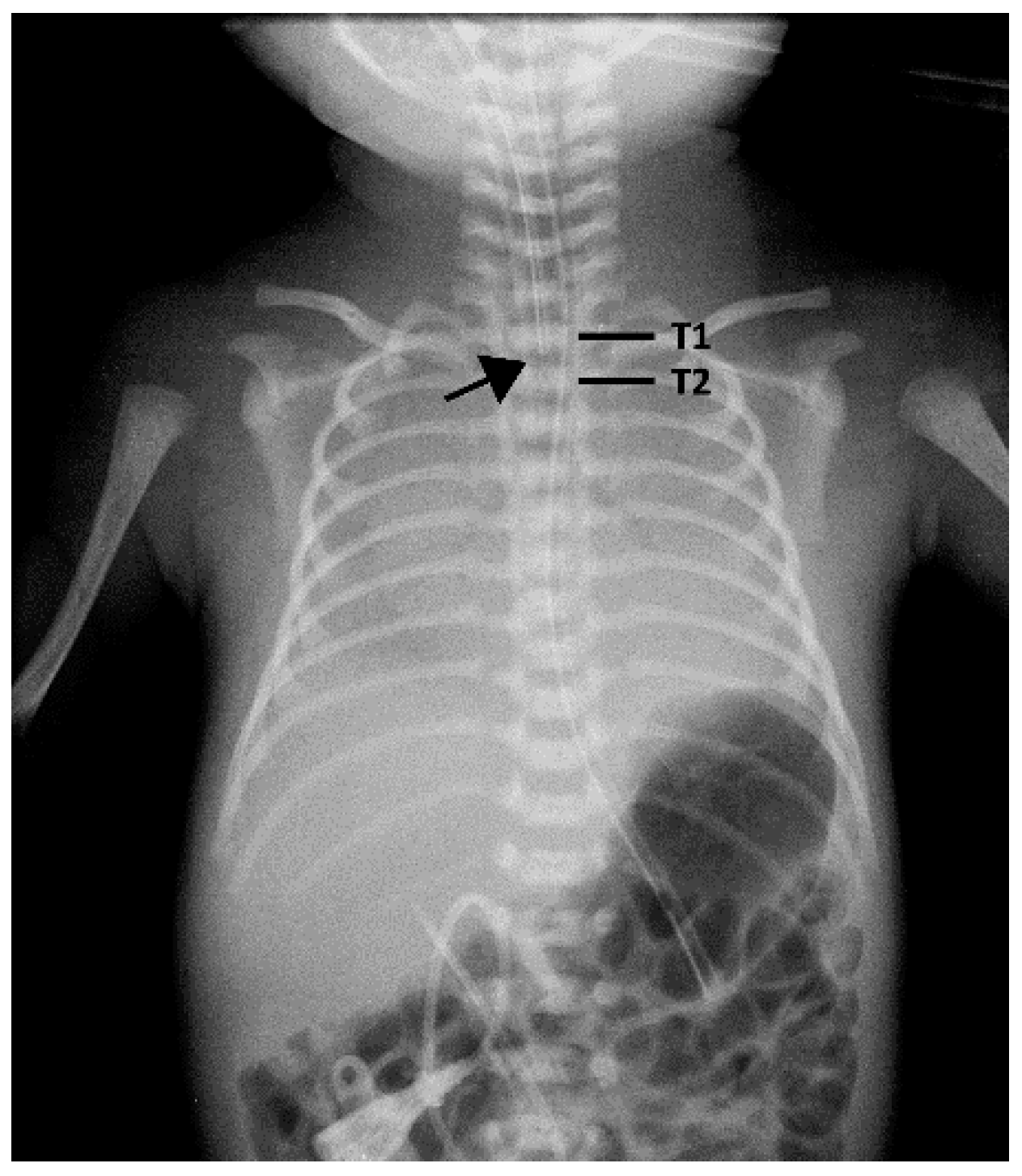
2.2. Depth of Endotracheal Tube
2.3. Statistical Analysis
3. Results
3.1. Comparison of the Consistent and Inconsistent Groups
3.2. Multivariable Linear Regression
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Peterson, J.; Johnson, N.; Deakins, K.; Wilson-Costello, D.; Jelovsek, J.E.; Chatburn, R. Accuracy of the 7-8-9 rule for endotracheal tube placement in the neonate. J. Perinatol. 2006, 26, 333–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thayyil, S.; Nagakumar, P.; Gowers, H.; Sinha, A. Optimal endotracheal tube tip position in extremely premature infants. Am. J. Perinatol. 2008, 25, 13–16. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.; Mele, P.C.; Hou, W.; Decristofaro, J.D.; Maduekwe, E.T. The oro-helical length accurately predicts endotracheal tube insertion depth in neonates. J. Pediatr. 2018, 200, 265–269.e2. [Google Scholar] [CrossRef] [PubMed]
- Volsko, T.A.; McNinch, N.L.; Prough, D.S.; Bigham, M.T. Adherence to endotracheal tube depth guidelines and incidence of malposition in infants and children. Respir. Care 2018, 63, 1111–1117. [Google Scholar] [CrossRef] [PubMed]
- Sakhuja, P.; Finelli, M.; Hawes, J.; Whyte, H. Is it time to review guidelines for ETT positioning in the NICU? SCEPTIC-survey of challenges encountered in placement of endotracheal tubes in Canadian NICUs. Int. J. Pediatr. 2016, 7283179. [Google Scholar] [CrossRef] [Green Version]
- Weiner, G.M. (Ed.) Textbook of Neonatal Resuscitation (NRP), 7th ed.; American Academy of Pediatrics: Elk Grove Village, IL, USA, 2016; p. 326. [Google Scholar]
- Kempley, S.T.; Moreiras, J.W.; Petrone, F.L. Endotracheal tube length for neonatal intubation. Resuscitation 2008, 77, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Oestergaard, M.Z.; Inoue, M.; Yoshida, S.; Mahanani, W.R.; Gore, F.M.; Cousens, S.; Lawn, J.E.; Mathers, C.D.; United Nations Inter-Agency Group for Child Mortality Estimation and the Child Health Epidemiology Reference Group. Neonatal mortality levels for 193 countries in 2009 with trends since 1990: A systematic analysis of progress, projections, and priorities. PLoS Med. 2011, 8, e1001080. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- United Nations Inter-agency Group for Child Mortality Estimation (UNIGME). ‘Levels & Trends in Child Mortality: Report 2019, Estimates Developed by the United Nations Inter-Agency Group for Child Mortality Estimation’, United Nations Children’s Fund, New York. 2019. Available online: https://www.unicef.org/reports/levels-and-trends-child-mortality-report-2019 (accessed on 11 February 2021).
- Watson, S.I.; Arulampalam, W.; Petrou, S.; Marlow, N.; Morgan, A.S.; Draper, E.S.; Modi, N.; Neonatal data analysis unit (NDAU) and the neonatal economic, staffing, and clinical outcomes project (NESCOP) group. The effects of a one-to-one nurse-to-patient ratio on the mortality rate in neonatal intensive care: A retrospective, longitudinal, population-based study. Arch. Dis. Child Fetal Neonatal Ed. 2016, 101, F195–F200. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niemarkt, H.J.; Hütten, M.C.; Kramer, B.W. Surfactant for respiratory distress syndrome: New ideas on a familiar drug with innovative applications. Neonatology 2017, 111, 408–414. [Google Scholar] [CrossRef] [PubMed]
- Moya, F.R.; Mazela, J.; Shore, P.M.; Simonson, S.G.; Segal, R.; Simmons, P.D.; Gregory, T.J.; Guardia, C.G.; Varga, J.R.; Finer, N.N.; et al. Prospective observational study of early respiratory management in preterm neonates less than 35 weeks of gestation. BMC Pediatr. 2019, 19, 147. [Google Scholar] [CrossRef] [PubMed]
- Diblasi, R.M. Nasal continuous positive airway pressure (CPAP) for the respiratory care of the newborn infant. Respir. Care 2009, 54, 1209–1235. [Google Scholar] [PubMed]
- Bartle, R.M.; Miller, A.G.; Diez, A.J.; Smith, P.B.; Gentile, M.A.; Puia-Dumitrescu, M. Evaluating endotracheal tube depth in infants weighing less than 1 kilogram. Respir. Care 2019, 64, 243–247. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.W.; Lee, W.T.; Chen, H.L. Reexamining the ideal depth of endotracheal tube in neonates. Pediatr. Neonatol. 2018, 59, 258–262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takeuchi, S.; Arai, J.; Nagafuji, M.; Hinata, A.; Kamakura, T.; Hoshino, Y.; Yukitake, Y. Ideal endotracheal tube insertion depth in neonates with a birthweight less than 750 g. Pediatr. Int. 2020, 62, 932–936. [Google Scholar] [CrossRef] [PubMed]
- Leung, C. Optimal insertion depth for endotracheal tubes in extremely low-birth-weight infants. Pediatr. Crit. Care Med. 2018, 19, 328–331. [Google Scholar] [CrossRef] [PubMed]
- Flinn, A.M.; Travers, C.P.; Laffan, E.E.; O’Donnell, C.P. Estimating the endotracheal tube insertion depth in newborns using weight or gestation: A randomised trial. Neonatology 2015, 107, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.S.; Yang, C.C. Tracheal length of infants under three months old. Ann. Otol. Rhinol. Laryngol. 2001, 110, 268–270. [Google Scholar] [CrossRef] [PubMed]
- Mi, W.; Zhang, C.; Wang, H.; Cao, J.; Li, C.; Yang, L.; Guo, F.; Wang, X.; Yang, T. Measurement and analysis of the tracheobronchial tree in Chinese population using computed tomography. PLoS ONE 2015, 10, e0130239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saboo, A.R.; Dutta, S.; Sodhi, K.S. Digital palpation of endotracheal tube tip as a method of confirming endotracheal tube position in neonates: An open-label, three-armed randomized controlled trial. Paediatr. Anaesth. 2013, 23, 934–939. [Google Scholar] [CrossRef] [PubMed]


| Gestational Age (Weeks) | Endotracheal Tube Insertion Depth (cm) | Body Weight (grams) |
|---|---|---|
| 23–24 | 5.5 | 500–600 |
| 25–26 | 6.0 | 700–800 |
| 27–29 | 6.5 | 900–1000 |
| 30–32 | 7.0 | 1100–1400 |
| 33–34 | 7.5 | 1500–1800 |
| 35–37 | 8.0 | 1900–2400 |
| 38–40 | 8.5 | 2500–3100 |
| 41–43 | 9.0 | 3200–4200 |
| Characteristics (N = 180) | |
|---|---|
| Gestational age, weeks | 33.66 ± 5.46 |
| Term, n (%) | 63 (35.0%) |
| Preterm (n = 117) (GA 1) | |
| 34–36 weeks | 29 (24.8%) |
| <34 weeks | 88 (75.2%) |
| Birth weight (grams) | 1986.50 ± 914.45 |
| ≧2500 | 65 (36.1%) |
| Low Birth Weight (1500–2499) | 49 (27.2%) |
| Very Low Birth Weight (1000–1499) | 29 (16.1%) |
| Extremely Low Birth Weight (<1000) | 37 (20.6%) |
| Appropriate for Gestational Age 1 | 135 (75%) |
| Small for Gestational Age 2 | 36 (20%) |
| Large for Gestational Age 3 | 9 (5%) |
| Birth weight (Z-score 4) | −0.41 ± 0.98 |
| Male, n (%) | 111 (61.7%) |
| Vaginal delivery | 72 (40.0%) |
| Apgar score at 1 min | 5.4 ± 2.4 |
| Apgar score at 5 min | 7.2 ± 2.1 |
| Reasons for intubation | |
| Respiratory distress syndrome, n (%) | 83 (46.1%) |
| Hypoxic-ischemic encephalopathy, n (%) | 19 (10.6%) |
| For operation, n (%) | 26 (14.4%) |
| Sepsis, n (%) | 13 (7.2%) |
| Congenital cyanotic heart disease | 9 (5%) |
| Persistent pulmonary hypertension of newborn, n (%) | 4 (2.2%) |
| Meconium aspiration syndrome, n (%) | 3 (1.7%) |
| Others 5 | 23 (12.8%) |
| Endotracheal tube depth at 1st attempt | |
| Tochen’s formula (Before 2016), n = 96 | |
| Correct | 62 (64.6%) |
| Inappropriate | 34 (35.4%) |
| After 2017, n = 84 | |
| Correct | 57 (67.9%) |
| Inappropriate | 27 (32.1%) |
| Group 1 (N = 86) | Group 2 (N = 94) | p * | |
|---|---|---|---|
| Sex | 0.99 | ||
| Male | 53 | 58 | |
| Female | 33 | 36 | |
| Age of intubation (GA 1 or PMA 2, weeks) | 35.8 (29.0–39.0) | 34.0 (29.1–38.0) | 0.52 |
| Body weight (gram) | 2036.5 (1014.5–2846.5) | 1955.0 (1280.5–2846.3) | 0.81 |
| Body height 3 (cm) | 45.0 (36.0–49.0) | 44.5 (35.8–49.0) | 0.98 |
| Head circumference 4 (cm) | 34.5 (26.0–33.9) | 31.0 (25.7–33.5) | 0.71 |
| Mode of delivery | 0.27 | ||
| Vaginal delivery | 38 | 34 | |
| Cesarean section | 48 | 60 | |
| Apgar score 5 | |||
| 1 min | 6.0 (4.0–8.0) | 6.0 (4.0–7.0) | 0.84 |
| 5 min | 8.0 (6.0–9.0) | 8.0 (70–9.0) | 0.47 |
| Initial ETT 6 depth (cm) | 8.0 (7.0–9.0) | 8.0 (7.0–8.5) | 0.82 |
| The ETT depth at 1st attempt | 0.32 | ||
| Correct | 60 | 59 | |
| Need revision | 26 | 35 | |
| Depth of adjustment (cm) | 0.0 (0.0–0.0) | 0.0 (0.0–0.0) | 0.79 |
| Appropriate for Gestational Age 7 | 0.11 | ||
| Yes | 66 | 62 | |
| No | 20 | 32 | |
| ETT depth adjustment for Age based formula (cm) | 0.5 (0.0–0.5) | 0.5 (0.0–1.0) | 0.008 |
| ETT depth adjustment for BW 8 based formula (cm) | 0.5 (0.0–0.5) | 0.0 (0.0–0.5) | 0.08 |
| Crude | Adjusted | |||
|---|---|---|---|---|
| Variables | B 4 (95% CI 5) | p | B 4 (95% CI 5) | p |
| Age (GA 1 or PMA 2) | 0.17 (0.16 to 0.19) | <0.001 | 0.04 (−0.00 to 0.08) | 0.08 |
| Body weight | 0.00 (0.00 to 0.00) | <0.001 | 0.00 (0.001 to 0.001) | <0.001 |
| Body length | 0.12 (0.11 to 0.14) | <0.001 | 0.00 (−0.02 to 0.03) | 0.83 |
| Sex | 0.42 (0.11 to 0.74) | <0.05 | 0.10 (−0.04 to 0.25) | 0.16 |
| Non-AGA 3 | 0.07 (−0.28 to 0.41) | 0.71 | −0.01 (−0.19 to 0.16) | 0.88 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, H.-K.; Yang, Y.-N.; Tey, S.-L.; Wu, P.-L.; Yang, S.-N.; Wu, C.-Y. Weight Is More Accurate than Gestational Age When Estimating the Optimal Endotracheal Tube Depth in Neonates. Children 2021, 8, 324. https://doi.org/10.3390/children8050324
Liu H-K, Yang Y-N, Tey S-L, Wu P-L, Yang S-N, Wu C-Y. Weight Is More Accurate than Gestational Age When Estimating the Optimal Endotracheal Tube Depth in Neonates. Children. 2021; 8(5):324. https://doi.org/10.3390/children8050324
Chicago/Turabian StyleLiu, Hsien-Kuan, Yung-Ning Yang, Shu-Leei Tey, Pei-Ling Wu, San-Nan Yang, and Chien-Yi Wu. 2021. "Weight Is More Accurate than Gestational Age When Estimating the Optimal Endotracheal Tube Depth in Neonates" Children 8, no. 5: 324. https://doi.org/10.3390/children8050324







