The Appropriateness of Glycerin Enema in Pediatric Patients Visiting the Emergency Department
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
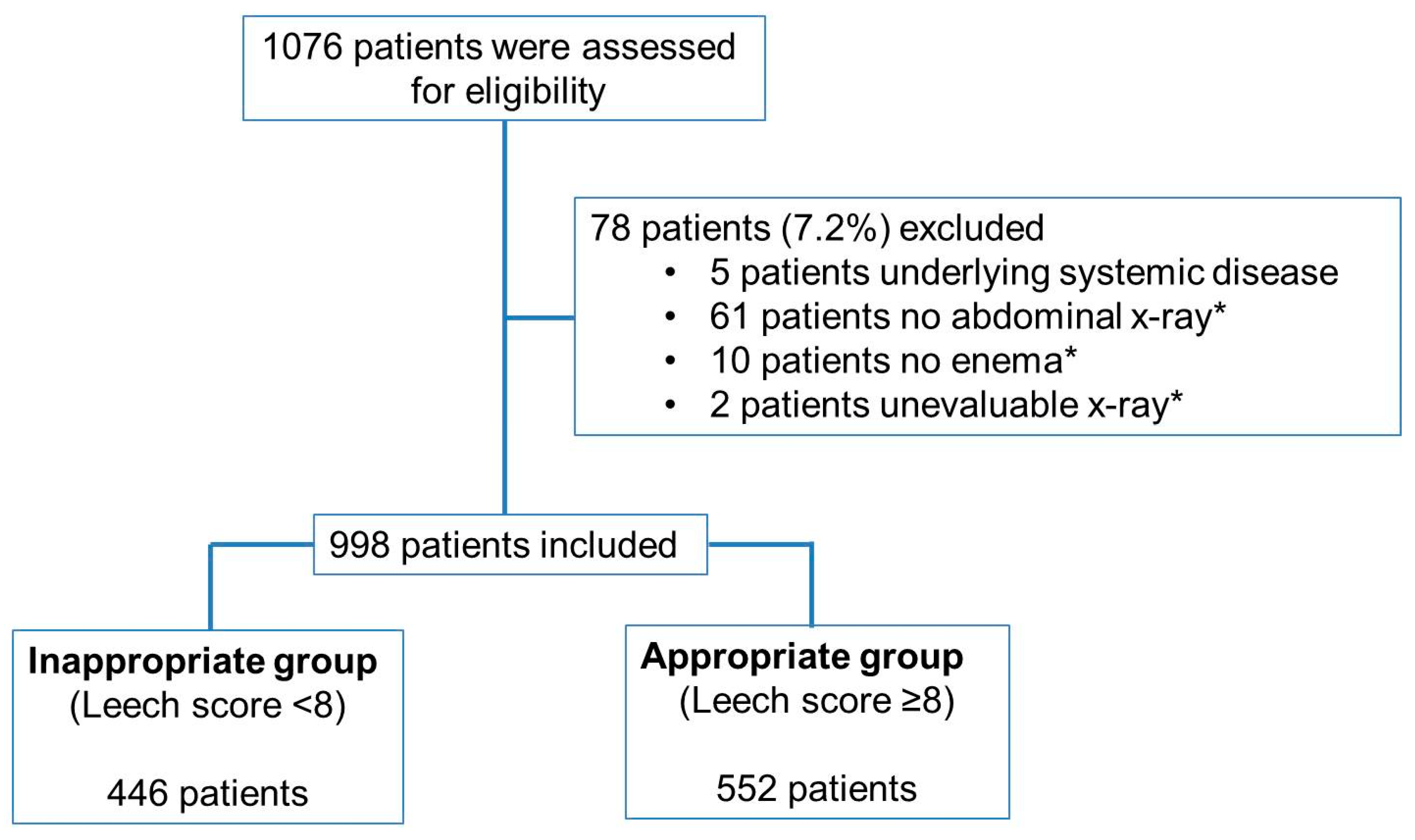
2.2. Selection of Participants
2.3. Data Collection
2.4. Procedures
2.5. Outcomes
2.6. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Miller, M.K.; Dowd, M.D.; Fraker, M. Emergency department management and short-term outcome of children with constipation. Pediatr. Emerg. Care 2007, 23, 1–4. [Google Scholar] [CrossRef]
- Bulloch, B.; Tenenbein, M. Constipation: Diagnosis and management in the pediatric emergency department. Pediatr. Emerg. Care 2002, 18, 254–258. [Google Scholar] [CrossRef]
- Doniger, S.J.; Dessie, A.; Latronica, C. Measuring the transrectal diameter on point-of-care ultrasound to diagnose constipation in children. Pediatr. Emerg. Care 2018, 34, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Chumpitazi, C.E.; Henkel, E.B.; Valdez, K.L.; Chumpitazi, B.P. Soap Suds Enema are Efficacious and Safe for Treating Fecal Impaction in Children with Abdominal Pain. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 15. [Google Scholar] [CrossRef]
- Molina, S.T.; Flores, I.H.; Macedo, J.T.; Delgado, A.G.; de la Garza, J.M. Association between abdominal pain and fecal impaction grade assessed through radiography in constipated patients at a pediatric emergency service. Rev. Gastroenterol. México Engl. Ed. 2020, 85, 235–239. [Google Scholar]
- Freedman, S.B.; Thull-Freedman, J.; Rumantir, M.; Eltorki, M.; Schuh, S. Pediatric constipation in the emergency department: Evaluation, treatment, and outcomes. J. Pediatr. Gastroenterol. Nutr. 2014, 59, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Nurko, S.; Baker, S.S.; Colletti, R.B.; Croffie, J.M. Managing constipation: Evidence put to practice. Contemp. Pediatr. 2001, 18, 56. [Google Scholar]
- Choi, H.-J.; Park, H.-G.; Maeng, T.-H.; Yoo, D.J.; Kim, S.S.; Chung, W.S. A case of ischemic colitis presenting as bloody diarrhea after glycerin enema in a patient on modified fasting therapy. J. Korean Med. Rehabi. 2013, 23, 185–191. [Google Scholar]
- Maeda, E.; Mori, Y.; Amano, E.; Akamatsu, T.; Okada, T. A case of the complications following glycerin enema which suggested malignant hyperthermia. Masui. Jpn. J. Anesthesiol. 2010, 59, 914–917. [Google Scholar]
- Ogihara, S.; Orii, M.; Adachi, W. A Case of Acute Renal Failure after Extraluminal Injection of Glycerin Enema. J. Jpn. Assoc. Rural Med. 2017, 66, 494–498. [Google Scholar]
- Poddar, U. Approach to constipation in children. Indian Pediatr. 2016, 53, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Guest, J.F.; Clegg, J.P. Modelling the costs and consequences of treating paediatric faecal impaction in Australia. Curr. Med. Res. Opin. 2006, 22, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Borowitz, S.M.; Cox, D.J.; Kovatchev, B.; Ritterband, L.M.; Sheen, J.; Sutphen, J. Treatment of childhood constipation by primary care physicians: Efficacy and predictors of outcome. Pediatrics 2005, 115, 873–877. [Google Scholar] [CrossRef]
- Choi, J.; Kwak, Y.H.; Kim, D.K.; Yi, J.H.; Jeong, J.H.; Kim, H.B.; Jung, J.Y.; Suh, D.B.; Cheon, J.E.; Choi, Y.H. Abdominal Radiography for the Evaluation of Acute Fecal Impaction in Children in Pediatric Emergency Department: Comparison of Three Scoring Methods. J. Korean Soc. Emerg. Med. 2013, 24, 224–229. [Google Scholar]
- De Lorijn, F.; van Rijn, R.R.; Heijmans, J.; Reitsma, J.B.; Voskuijl, W.P.; Henneman, O.D.; Taminiau, J.A.; Benninga, M.A. The Leech method for diagnosing constipation: Intra-and interobserver variability and accuracy. Pediatr. Radiol. 2006, 36, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Cunha, T.B.D.; Tahan, S.; Soares, M.F.; Lederman, H.M.; Morais, M.B.D. Abdominal radiograph in the assessment of fecal impaction in children with functional constipation: Comparing three scoring systems. J. Pediatr. 2012, 88, 317–322. [Google Scholar] [CrossRef] [Green Version]
- Bonett, D.G. Sample size requirements for estimating intraclass correlations with desired precision. Stat. Med. 2002, 21, 1331–1335. [Google Scholar] [CrossRef]
- Shakya, K.N.; Dangol, U.; Khadka, S. A Study of Abdomenal Pain in Children. J. Nepal Med. Assoc. 2008, 47, 193–196. [Google Scholar] [CrossRef]
- Lee, K.J.; Tchah, H. A Prospective Study on Emergency Room Utilization in Children with Nonsurgical Gastrointestinal Disorders. Pediatric Gastroenterol. Nutr. 2001, 4, 54–62. [Google Scholar] [CrossRef] [Green Version]
- Kim, Y.; An, D.; Baek, S.m. A Clinical Study on Children Visiting Emergency Room with Abdominal Pain. New Med. J. 1987, 30, 43–48. [Google Scholar]
- Miller, M.K.; Dowd, M.D.; Friesen, C.A.; Walsh-Kelly, C.M. A randomized trial of enema versus polyethylene glycol 3350 for fecal disimpaction in children presenting to an emergency department. Pediatr. Emerg. Care 2012, 28, 115–119. [Google Scholar] [CrossRef]
- Van den Berg, M.M.; Bongers, M.E.; Voskuijl, W.P.; Benninga, M.A. No role for increased rectal compliance in pediatric functional constipation. Gastroenterology 2009, 137, 1963–1969. [Google Scholar] [CrossRef]
- Eidlitz-Markus, T.; Mimouni, M.; Zeharia, A.; Nussinovitch, M.; Amir, J. Occult constipation: A common cause of recurrent abdominal pain in childhood. Isr. Med. Assoc. J. 2004, 6, 677–680. [Google Scholar] [PubMed]
- Brusciano, L.; Limongelli, P.; Del Genio, G.; Rossetti, G.; Sansone, S.; Healey, A.; Maffettone, V.; Napolitano, V.; Pizza, F.; Tolone, S.; et al. Clinical and instrumental parameters in patients with constipation and incontinence: Their potential implications in the functional aspects of these disorders. Int. J. Colorectal Dis. 2009, 24, 961–967. [Google Scholar] [CrossRef]
- Brusciano, L.; Gambardella, C.; Tolone, S.; Del Genio, G.; Terracciano, G.; Gualtieri, G.; Visconte, S.M.; Docimo, L. An imaginary cuboid: Chest, abdomen, vertebral column and perineum, different parts of the same whole in the harmonic functioning of the pelvic floor. Tech. Coloproctol. 2019, 23, 603–605. [Google Scholar] [CrossRef]
- Van den Berg, M.-M.; Dijkgraaf, M.G.; van Wijk, M.P.; Bongers, M.E.; Liem, O.; Benninga, M.A. Rectal fecal impaction treatment in childhood constipation: Enemas versus high doses oral PEG. Pediatrics 2009, 124, e1108–e1115. [Google Scholar]
- Corban, C.; Sommers, T.; Sengupta, N.; Jones, M.; Cheng, V.; Friedlander, E.; Bollom, A.; Lembo, A. Fecal impaction in the emergency department: An analysis of frequency and associated charges in 2011. J. Clin. Gastroenterol. 2016, 50, 572–577. [Google Scholar] [CrossRef]
- Rezazadeh, A.; Javaherizadeh, H.; Chahardahcherik, F.; Yavarahmadi, M.H.; Sadjadei, N.; Tahmasebi, M. Reliability of Barr, Leech, and Blethyn score in using of plain radiography in determining fecal impaction in children with and without constipation. Arq. Gastroenterol. 2016, 53, 141–145. [Google Scholar] [CrossRef] [Green Version]
- Leech, S.C.; McHugh, K.; Sullivan, P. Evaluation of a method of assessing faecal loading on plain abdominal radiographs in children. Pediatr. Radiol. 1999, 29, 255–258. [Google Scholar] [CrossRef] [PubMed]
- Pensabene, L.; Buonomo, C.; Fishman, L.; Chitkara, D.; Nurko, S. Lack of utility of abdominal X-rays in the evaluation of children with constipation: Comparison of different scoring methods. J. Pediatr. Gastroenterol. Nutr. 2010, 51, 155. [Google Scholar] [CrossRef] [Green Version]
- Ryoo, E. Management of abdominal pain in pediatric emergency departments. Pediatr. Emerg. Med. J. 2018, 5, 38–43. [Google Scholar] [CrossRef]
- Gieteling, M.J.; Lisman-van Leeuwen, Y.; van der Wouden, J.C.; Schellevis, F.G.; Berger, M.Y. Childhood nonspecific abdominal pain in family practice: Incidence, associated factors, and management. Ann. Fam. Med. 2011, 9, 337–343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Elliott, E.J. Acute gastroenteritis in children. BMJ 2007, 334, 35–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Leech Score | p-Value | ||
|---|---|---|---|
| <8 Inappropriate (N = 446) | ≥8 Appropriate (N = 552) | ||
| Age (year), mean ± SD | 4.2 ± 3.1 | 3.6 ± 2.4 | 0.000 |
| Male, N (%) | 252 (56.5) | 299 (54.2) | 0.461 |
| Admission, N (%) | 14 (3.1) | 17 (3.1) | 0.957 |
| Diagnosis, N (%) | 0.002 | ||
| Fecal impaction | 193 (43.3) | 315 (57.1) | |
| Nonspecific abdominal pain | 37 (8.3) | 29 (5.3) | |
| Acute gastroenteritis | 182 (40.8) | 161 (29.1) | |
| Acute gastritis | 2 (0.5) | 0 (0) | |
| Acute appendicitis | 3 (0.7) | 2 (0.4) | |
| Intussusception | 1 (0.2) | 0 (0) | |
| Upper respiratory infection | 21 (4.7) | 35 (6.3) | |
| Lower respiratory infection | 4 (0.9) | 4 (0.7) | |
| Urinary tract infection | 2 (0.5) | 1 (0.2) | |
| Physician grade, N (%) | 0.900 | ||
| Low grade resident | 344 (77.5) | 437 (79.3) | |
| High grade resident | 13 (2.9) | 16 (2.9) | |
| Pediatric emergency specialist | 61 (13.7) | 67 (12.2) | |
| Revisit, N (%) | |||
| OPD_appointment | 140 (32.9) | 138 (25.5) | 0.029 |
| OPD_visit | 99 (22.6) | 90 (16.6) | 0.017 |
| OPD_Same cause | 51 (15.7) | 46 (14.9) | 0.529 |
| ED Revisit | 27 (6.2) | 33 (6.1) | 0.955 |
| Gastrointestinal symptoms, N (%) | 0.035 | ||
| Abdominal pain | 290 (65.9) | 335 (63.3) | |
| Vomiting | 140 (31.8) | 156 (29.5) | |
| Constipation | 5 (1.1) | 15 (2.8) | |
| Irritability | 4 (0.9) | 16 (3.0) | |
| Flank pain | 1 (0.2) | 2 (0.4) | |
| Poor oral intake | 0 | 4 (0.8) | |
| Melena | 0 | 1 (0.2) | |
| Previous constipation history, N (%) | 82 (23.9) | 102 (27.8) | 0.238 |
| Laboratory test, N (%) | 133 (29.8) | 142 (25.7) | 0.150 |
| Ultrasound, N (%) | 38 (8.5) | 50 (9.1) | 0.766 |
| The number of enemas (≥2), N (%) | 8 (1.8) | 11 (2.0) | 0.821 |
| Oral hydration therapy, N (%) | 72 (16.1) | 57 (10.3) | 0.006 |
| IV hydration before enema, N (%) | 87 (19.5) | 112 (20.3) | 0.758 |
| IV hydration after enema, N (%) | 64 (14.4) | 53 (9.6) | 0.02 |
| Length of stay in ED, min, mean ± SD | 181.3 ± 146.0 | 176.6 ± 164.0 | |
| Univariate Analysis | Multivariate Analysis | |||||||
|---|---|---|---|---|---|---|---|---|
| OR | Standard Error | p-Value | 95% CI | OR | Standard Error | p-Value | 95% CI | |
| Gender | ||||||||
| Male | 1 | |||||||
| Female | 1.10 | 0.14 | 0.461 | 0.86–1.41 | 1.07 | 0.19 | 0.687 | 0.76–1.52 |
| Age (years) | 0.93 | 0.02 | 0.001 | 0.89–0.97 | ||||
| <1 | 1 | |||||||
| 1–2 | 1.66 | 0.53 | 0.114 | 0.89–3.11 | 2.09 | 1.06 | 0.147 | 0.77–5.67 |
| 2–4 | 2.44 | 0.74 | 0.003 | 1.35-4.41 | 4.24 | 2.11 | 0.004 | 1.59–11.26 |
| 4–8 | 1.69 | 0.50 | 0.079 | 0.94–3.03 | 2.83 | 1.43 | 0.039 | 1.05–7.61 |
| 8–14 | 1.15 | 0.40 | 0.689 | 0.58–2.26 | 2.44 | 1.35 | 0.108 | 0.82–7.23 |
| ≥14 | 0.23 | 0.26 | 0.194 | 0.03–2.09 | - | |||
| Physician grade | ||||||||
| Low grade resident | 1 | |||||||
| High grade resident | 0.97 | 0.37 | 0.934 | 0.46–2.04 | 0.97 | 0.54 | 0.960 | 0.33–2.91 |
| Pediatric emergency specialist | 0.86 | 0.17 | 0.446 | 0.60–1.26 | 0.82 | 0.22 | 0.459 | 0.48–1.89 |
| Gastrointestinal symptoms | ||||||||
| Abdominal pain | 1 | |||||||
| Vomiting | 0.96 | 0.14 | 0.799 | 0.73–1.27 | 1.72 | 0.41 | 0.023 | 1.08–2.76 |
| Constipation | 2.6 | 1.36 | 0.068 | 0.93–7.23 | 2.41 | 1.55 | 0.170 | 0.69–8.48 |
| Irritability | 3.46 | 1.96 | 0.028 | 1.15–10.47 | 5.32 | 4.52 | 0.049 | 1.00–28.15 |
| Flank pain | 1.73 | 2.12 | 0.655 | 0.16–19.19 | - | |||
| Constipation history | 1.23 | 0.21 | 0.238 | 0.87–1.72 | 0.97 | 0.21 | 0.906 | 0.64–1.49 |
| Last defecation day | 1.22 | 0.76 | 0.002 | 1.08–1.38 | 1.2 | 0.10 | 0.034 | 1.01–1.42 |
| Laboratory test | 0.82 | 0.12 | 0.150 | 0.62–1.08 | 1.14 | 0.46 | 0.738 | 0.52–2.51 |
| Ultrasonography | 1.07 | 0.24 | 0.766 | 0.69–1.66 | 1.43 | 0.51 | 0.314 | 0.71–2.87 |
| IV hydration pre enema | 1.05 | 0.17 | 0.758 | 0.77–1.44 | 1.3 | 0.48 | 0.477 | 0.63–2.67 |
| IV hydration post enema | 0.63 | 0.13 | 0.021 | 0.43–0.93 | 0.86 | 0.32 | 0.679 | 0.42–1.75 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, M.-J.; Choi, Y.-J.; Lee, J.-H.; Kwon, H.; Suh, D. The Appropriateness of Glycerin Enema in Pediatric Patients Visiting the Emergency Department. Children 2021, 8, 364. https://doi.org/10.3390/children8050364
Kim M-J, Choi Y-J, Lee J-H, Kwon H, Suh D. The Appropriateness of Glycerin Enema in Pediatric Patients Visiting the Emergency Department. Children. 2021; 8(5):364. https://doi.org/10.3390/children8050364
Chicago/Turabian StyleKim, Min-Jung, Yoo-Jin Choi, Jin-Hee Lee, Hyuksool Kwon, and Dongbum Suh. 2021. "The Appropriateness of Glycerin Enema in Pediatric Patients Visiting the Emergency Department" Children 8, no. 5: 364. https://doi.org/10.3390/children8050364







