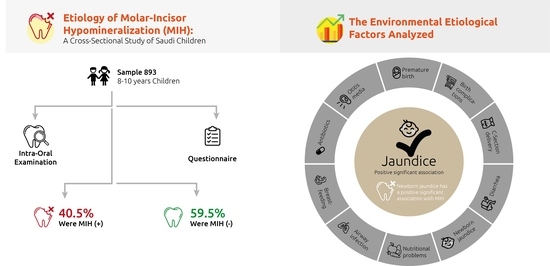
Etiology of Molar-Incisor Hypomineralization (MIH): A Cross-Sectional Study of Saudi Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting and Study Population
- Children aged 8–10 years
- Saudi children who were lifelong residents of Riyadh
- Erupted first permanent molars, and a minimum of six permanent incisors
- Children with signs of fluorosis, tetracycline staining, amelogenesis imperfecta, and generalized enamel hypoplasia
- Undergoing orthodontic treatment
- Opacities confined to the incisors only
- Absence of parental consent to participate
2.2. Examination
2.3. Questionnaire
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Weerheijm, K.L.; Jälevik, B.; Alaluusua, S. Molar-incisor hypomineralisation. Caries Res. 2001, 35, 390–391. [Google Scholar] [CrossRef]
- Fayle, S.A. Molar incisor hypomineralisation: Restorative management. Eur. J. Paediatr. Dent. 2003, 4, 121–126. [Google Scholar]
- Humphreys, J.; Albadri, S. Management of molar incisor hypomineralisation (MIH): A 1-year retrospective study in a specialist secondary care centre in the UK. Children 2020, 7, 252. [Google Scholar] [CrossRef]
- Americano, G.C.; Jacobsen, P.E.; Soviero, V.M.; Haubek, D. A systematic review on the association between molar incisor hypomineralization and dental caries. Int. J. Paediatr. Dent. 2017, 27, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Murri Dello Diago, A.; Cadenaro, M.; Ricchiuto, R.; Banchelli, F.; Spinas, E.; Checchi, V.; Giannetti, L. Hypersensitivity in molar incisor hypomineralization: Superficial infiltration treatment. Appl. Sci. 2021, 11, 1823. [Google Scholar] [CrossRef]
- Zhao, D.; Dong, B.; Yu, D.; Ren, Q.; Sun, Y. The prevalence of molar incisor hypomineralization: Evidence from 70 studies. Int. J. Paediatr. Dent. 2018, 28, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, M.; Boj, J.R.; Espasa, E. Do we really know the prevalence of MIH? J. Clin. Pediatr. Dent. 2016, 40, 259–263. [Google Scholar] [CrossRef] [PubMed]
- Zawaideh, F.I.; Al-Jundi, S.H.; Al-Jaljoli, M.H. Molar incisor hypomineralisation: Prevalence in Jordanian children and clinical characteristics. Eur. Arch. Paediatr. Dent. 2011, 12, 31–36. [Google Scholar] [CrossRef]
- Ghanim, A.; Mariño, R.; Morgan, M.; Bailey, D.; Manton, D. An in vivo investigation of salivary properties, enamel hypomineralisation, and carious lesion severity in a group of Iraqi schoolchildren. Int. J. Paediatr. Dent. 2013, 23, 2–12. [Google Scholar] [CrossRef]
- Allazzam, S.M.; Alaki, S.M.; El Meligy, O.A. Molar incisor hypomineralization, prevalence, and etiology. Int. J. Dent. 2014, 2014, 234508. [Google Scholar] [CrossRef]
- Al-Hammad, N.S.; Al-Dhubaiban, M.; Alhowaish, L.; Bello, L.L. Prevalence and clinical characteristics of molar-incisor-hypomineralization in school children in riyadh, Saudi Arabia. Int. J. Med. Sci. Clin. Invent. 2018, 5, 3570–3576. [Google Scholar] [CrossRef]
- Alaluusua, S. Aetiology of Molar-Incisor Hypomineralisation: A systematic review. Eur. Arch. Paediatr. Dent. 2010, 11, 53–58. [Google Scholar] [CrossRef]
- Vieira, A.R.; Kup, E. On the etiology of molar-incisor hypomineralization. Caries Res. 2016, 50, 166–169. [Google Scholar] [CrossRef] [PubMed]
- Fagrell, T.G.; Ludvigsson, J.; Ullbro, C.; Lundin, S.A.; Koch, G. Aetiology of severe demarcated enamel opacities--an evaluation based on prospective medical and social data from 17,000 children. Swed. Dent. J. 2011, 35, 57–67. [Google Scholar]
- Bandeira Lopes, L.; Machado, V.; Botelho, J.; Haubek, D. Molar-incisor hypomineralization: An umbrella review. Acta Odontol. Scand. 2021, 1–11. [Google Scholar] [CrossRef]
- Fatturi, A.L.; Wambier, L.M.; Chibinski, A.C.; Assunção, L.; Brancher, J.A.; Reis, A.; Souza, J.F. A systematic review and meta-analysis of systemic exposure associated with molar incisor hypomineralization. Community Dent. Oral Epidemiol. 2019, 47, 407–415. [Google Scholar] [CrossRef]
- Silva, M.J.; Scurrah, K.J.; Craig, J.M.; Manton, D.J.; Kilpatrick, N. Etiology of molar incisor hypomineralization—A systematic review. Community Dent. Oral Epidemiol. 2016, 44, 342–353. [Google Scholar] [CrossRef]
- Sidaly, R.; Schmalfuss, A.; Skaare, A.B.; Sehic, A.; Stiris, T.; Espelid, I. Five-minute Apgar score ≤ 5 and Molar Incisor Hypomineralisation (MIH)—A case control study. BMC Oral Health 2016, 17, 25. [Google Scholar] [CrossRef]
- Weerheijm, K.L.; Duggal, M.; Mejàre, I.; Papagiannoulis, L.; Koch, G.; Martens, L.C.; Hallonsten, A.L. Judgement criteria for molar incisor hypomineralisation (MIH) in epidemiologic studies: A summary of the European meeting on MIH held in Athens, 2003. Eur. J. Paediatr. Dent. 2003, 4, 110–113. [Google Scholar] [PubMed]
- Lygidakis, N.A.; Wong, F.; Jälevik, B.; Vierrou, A.M.; Alaluusua, S.; Espelid, I. Best Clinical Practice Guidance for clinicians dealing with children presenting with Molar-Incisor-Hypomineralisation (MIH): An EAPD policy document. Eur. Arch. Paediatr. Dent. 2010, 11, 75–81. [Google Scholar] [CrossRef]
- Soviero, V.; Haubek, D.; Trindade, C.; Da Matta, T.; Poulsen, S. Prevalence and distribution of demarcated opacities and their sequelae in permanent 1st molars and incisors in 7 to 13-year-old Brazilian children. Acta Odontol. Scand. 2009, 67, 170–175. [Google Scholar] [CrossRef]
- Elfrink, M.E.; Ghanim, A.; Manton, D.J.; Weerheijm, K.L. Standardised studies on Molar Incisor Hypomineralisation (MIH) and Hypomineralised Second Primary Molars (HSPM): A need. Eur. Arch. Paediatr. Dent. 2015, 16, 247–255. [Google Scholar] [CrossRef]
- Mishra, A.; Pandey, R.K. Molar incisor hypomineralization: An epidemiological study with prevalence and etiological factors in Indian pediatric population. Int. J. Clin. Pediatr. Dent. 2016, 9, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.Y.; Ki, Y.; Chu, V. Molar incisor hypomineralization in Hong Kong Chinese children. Int. J. Paediatr. Dent. 2008, 18, 348–352. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Wang, J.; Li, Y.H.; Yang, Z.Y.; Zhou, Z. Association of molar incisor hypomineralization with premature birth or low birth weight: Systematic review and meta-analysis. J. Matern. Fetal. Neonatal. Med. 2020, 33, 1700–1708. [Google Scholar] [CrossRef] [PubMed]
- Garot, E.; Manton, D.; Rouas, P. Peripartum events and molar-incisor hypomineralisation (MIH) amongst young patients in southwest France. Eur. Arch. Paediatr. Dent. 2016, 17, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Serna, C.; Vicente, A.; Finke, C.; Ortiz, A.J. Drugs related to the etiology of molar incisor hypomineralization: A systematic review. J. Am. Dent. Assoc. 2016, 147, 120–130. [Google Scholar] [CrossRef] [PubMed]
- Lauer, B.J.; Spector, N.D. Hyperbilirubinemia in the newborn. Pediatr. Rev. 2011, 32, 341–349. [Google Scholar] [CrossRef]
- Wan, A.; Daud, S.M.; Teh, S.; Choo, Y.; Kutty, F. Management of neonatal jaundice in primary care. Malays Fam. Physician 2016, 11, 16–19. [Google Scholar]
- Muchowski, K.E. Evaluation and treatment of neonatal hyperbilirubinemia. Am. Fam. Physician 2014, 89, 873–878. [Google Scholar]
| The question given to mothers of participating children |
| Age? |
| Gender? |
| Place of residence and birth? |
| Was your child full term/pre-term? |
| Were there any birth complications? |
| Was the child delivery normal/Caesarean? |
| Did your child have asthma at or before the age of three? |
| Did your child have airway infection at or before the age of three? |
| Did your child have otitis media at or before the age of three? |
| Did your child have diarrhea at or before the age of three? |
| Was your child diagnosed with new-born jaundice requiring treatment under light? |
| Did your child have nutrition problems? |
| Was your child breastfed? |
| Did your child receive treatment with antibiotics at or before the age of three? |
| Any other medical events you would like to mention? |
| MIH + (362) | MIH- (531) | Total (893) | ||||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p-Value | ||
| Sex | Male | 168 | 38.9 | 264 | 61.1 | 432 | 48.4 | 0.341 |
| Female | 194 | 42.1 | 267 | 57.9 | 461 | 51.6 | ||
| Age | 8 years | 105 | 29 | 168 | 31.64 | 273 | 30.6 | 0.167 |
| 9 years | 143 | 39.5 | 177 | 33.33 | 320 | 35.8 | ||
| 10 years | 114 | 31.5 | 186 | 35.02 | 300 | 33.6 | ||
| Etiological Factors | MIH + (362) | MIH- (531) | Total (893) | |||||
|---|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | p-Value | ||
| Premature birth | yes | 17 | 4.7 | 25 | 4.7 | 42 | 4.7 | 0.993 |
| no | 345 | 95.3 | 506 | 95.3 | 851 | 95.3 | ||
| Childbirth complications | yes | 16 | 4.4 | 20 | 3.8 | 36 | 4 | 0.626 |
| no | 346 | 95.6 | 511 | 96.2 | 857 | 96 | ||
| Diarrhea | yes | 49 | 13.5 | 79 | 14.9 | 128 | 14.3 | 0.574 |
| no | 313 | 86.5 | 452 | 85.1 | 765 | 85.7 | ||
| Asthma | yes | 68 | 18.8 | 91 | 17.1 | 159 | 17.8 | 0.528 |
| no | 294 | 81.2 | 440 | 82.9 | 734 | 82.2 | ||
| Otitis media | yes | 68 | 18.8 | 86 | 16.2 | 154 | 17.2 | 0.368 |
| no | 294 | 81.2 | 445 | 83.8 | 739 | 82.8 | ||
| Normal birth | yes | 312 | 86.2 | 457 | 86.1 | 769 | 86.1 | 0.949 |
| no | 50 | 13.8 | 74 | 13.9 | 124 | 13.9 | ||
| Newborn jaundice | yes | 117 | 32.3 | 138 | 26.0 | 255 | 28.6 | 0.040 * |
| no | 245 | 67.7 | 393 | 74.0 | 638 | 71.4 | ||
| Airway infection | yes | 14 | 3.9 | 14 | 2.6 | 28 | 3.1 | 0.300 |
| no | 348 | 96.1 | 517 | 97.4 | 865 | 96.9 | ||
| Nutrition problems | yes | 3 | 0.8 | 2 | 0.4 | 5 | 0.6 | 0.374 |
| no | 359 | 99.2 | 529 | 99.6 | 888 | 99.4 | ||
| Breast feeding | yes | 297 | 82.0 | 442 | 83.2 | 739 | 82.8 | 0.643 |
| no | 65 | 18.0 | 89 | 16.8 | 154 | 17.2 | ||
| Antibiotics use | yes | 205 | 56.8 | 299 | 82.8 | 504 | 56.5 | 0.107 |
| no | 97 | 26.9 | 167 | 46.3 | 264 | 29.6 | ||
| I don’t know | 60 | 16.6 | 64 | 17.7 | 124 | 13.9 | ||
| Multivariate Binary Logistic Regression Analysis (Full Model) | Goodness of Fit of the Model | ||||||
|---|---|---|---|---|---|---|---|
| Explainatory Variable | B | OR | p-Value | 95% CI | Tests of Model Coefficients | Hosmer and Lemeshow Test | Percentage Correct Classification |
| Age | −0.028 | 0.973 | 0.748 | 0.748–1.152 | 0.798 | 0.678 | 60.2% |
| Gender | 0.146 | 1.157 | 0.299 | 0.299–1.523 | |||
| Premature birth | −0.042 | 0.959 | 0.899 | 0.497–1.848 | |||
| Birth complications | 0.088 | 1.092 | 0.802 | 0.548–2.175 | |||
| Diarrhea | −0.175 | 0.840 | 0.391 | 0.564–1.251 | |||
| Asthma | 0.127 | 1.136 | 0.491 | 0.790–1.631 | |||
| Otitis media | 0.160 | 1.173 | 0.396 | 0.811–1.697 | |||
| Normal birth | −0.037 | 0.963 | 0.854 | 0.648–1.433 | |||
| Jaundice | 0.300 | 1.349 | 0.047 * | 0.999–1.822 | |||
| Nutritional problems | 0.621 | 1.861 | 0.504 | 0.301–11.499 | |||
| Airway infection | 0.347 | 1.415 | 0.376 | 0.656–3.054 | |||
| Brest feeding | 0.212 | 1.236 | 0.800 | 0.241–6.345 | |||
| Antibiotics use | −0.048 | 0.953 | 0.743 | 0.717–1.268 | |||
| Constant | −0.280 | 0.756 | 0.727 | ||||
| Forward Stepwise (Wald) Multivariate Binary Logistic Regression Equation (Reduced Model) | Model Goodness of Fit | ||||||
|---|---|---|---|---|---|---|---|
| Explainatory Variable | B | OR | p-Value | 95% CI | Tests of Model Coefficients | Hosmer and Lemeshow Test | Percentage Correct Classification |
| Newborn Jaundice | 0.307 | 1.360 | 0.040 * | 1.014–1.824 | 0.04 | 0.124 | 59.50% |
| Constant | −0.473 | 0.623 | 0.000 | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alhowaish, L.; Baidas, L.; Aldhubaiban, M.; Bello, L.L.; Al-Hammad, N. Etiology of Molar-Incisor Hypomineralization (MIH): A Cross-Sectional Study of Saudi Children. Children 2021, 8, 466. https://doi.org/10.3390/children8060466
Alhowaish L, Baidas L, Aldhubaiban M, Bello LL, Al-Hammad N. Etiology of Molar-Incisor Hypomineralization (MIH): A Cross-Sectional Study of Saudi Children. Children. 2021; 8(6):466. https://doi.org/10.3390/children8060466
Chicago/Turabian StyleAlhowaish, Latifa, Laila Baidas, Mohammed Aldhubaiban, Lanre L. Bello, and Nouf Al-Hammad. 2021. "Etiology of Molar-Incisor Hypomineralization (MIH): A Cross-Sectional Study of Saudi Children" Children 8, no. 6: 466. https://doi.org/10.3390/children8060466
APA StyleAlhowaish, L., Baidas, L., Aldhubaiban, M., Bello, L. L., & Al-Hammad, N. (2021). Etiology of Molar-Incisor Hypomineralization (MIH): A Cross-Sectional Study of Saudi Children. Children, 8(6), 466. https://doi.org/10.3390/children8060466