Aerosolized Surfactant for Preterm Infants with Respiratory Distress Syndrome
Abstract
1. Introduction
2. The Challenging Road towards Successful Clinical Application: Historical Narrative
3. Nebulizers
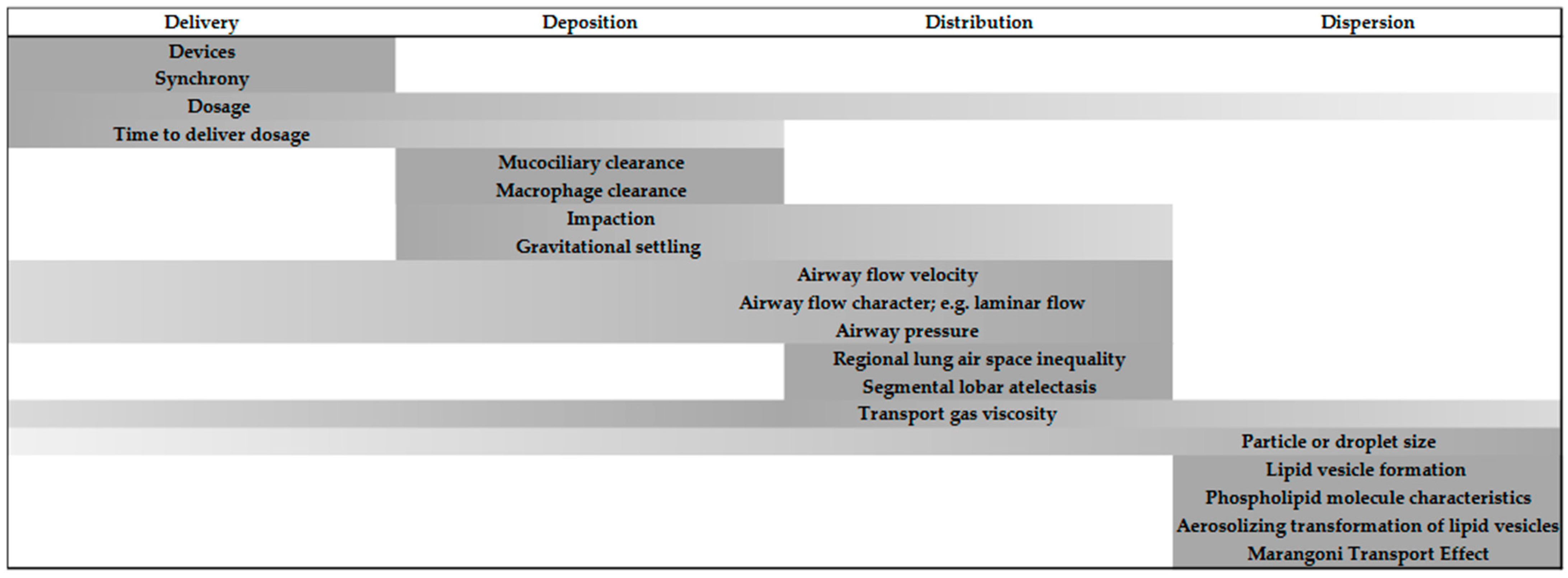
4. Delivery, Deposition, Distribution, and Dispersion of Aerosolized Surfactant
4.1. Delivery of Aerosolized Surfactant
4.2. Deposition of Aerosolized Surfactant
4.3. Distribution of Aerosolized Surfactant
4.4. Dispersion of Aerosolized Surfactant
5. The Potential Benefit of Aerosolized Surfactant
6. Conclusions
Funding
Conflicts of Interest
References
- Donda, K.; Vijayakanthi, N.; Dapaah-Siakwan, F.; Bhatt, P.; Rastogi, D.; Rastogi, S. Trends in epidemiology and outcomes of respiratory distress syndrome in the United States. Pediatr. Pulmonol. 2019, 54, 405–414. [Google Scholar] [CrossRef]
- Trembath, A.; Hornik, C.P.; Clark, R.; Smith, P.B.; Daniels, J.; Laughon, H. Comparative effectiveness of surfactant preparations in premature infants. J. Pediatr. 2013, 163, 955–960.e951. [Google Scholar] [CrossRef]
- Isayama, T.; Iwami, H.; McDonald, S.; Beyene, J. Association of Noninvasive Ventilation Strategies with Mortality and Bronchopulmonary Dysplasia among Preterm Infants: A Systematic Review and Meta-analysis. JAMA 2016, 316, 611–624. [Google Scholar] [CrossRef]
- Isayama, T.; Chai-Adisaksopha, C.; McDonald, S.D. Noninvasive Ventilation with VS without Early Surfactant to Prevent Chronic Lung Disease in Preterm Infants: A Systematic Review and Meta-analysis. JAMA Pediatr. 2015, 169, 731–739. [Google Scholar] [CrossRef]
- Finer, N.N.; Allen Merritt, T.; Bernstein, G.; Job, L.; Mazela, J.; Segal, R. An Open Label, Pilot Study of Aerosurf Combined with nCPAP to Prevent RDS in Preterm Neonates. J. Aerosol. Med. Pulm. Drug Deliv. 2010, 23, 303–309. [Google Scholar] [CrossRef]
- Minocchieri, S.; Berry, C.A.; Pillow, J.J.; CureNeb Study Team. Nebulised surfactant to reduce severity of respiratory distress: A blinded, parallel, randomised controlled trial. Arch. Dis. Child Fetal. Neonatal. Ed. 2019, 104, F313–F319. [Google Scholar] [CrossRef]
- Sood, B.G.; Cortez, J.; Kolli, M.; Sharma, A.; Delaney-Black, V.; Chen, X. Aerosolized surfactant in neonatal respiratory distress syndrome: Phase I study. Early Hum. Dev. 2019, 134, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Cummings, J.J.; Gerday, E.; Minton, S.; Katheria, A.; Albert, G.; Flores-Torres, J.; Famuyide, M.; Lampland, A.; Guthrie, S.; Kuehn, D.; et al. Aerosolized Calfactant for Newborns With Respiratory Distress: A Randomized Trial. Pediatrics 2020, 146. [Google Scholar] [CrossRef] [PubMed]
- Robillard, E.; Alarie, Y.; Dagenais-Perusse, P.; Baril, E.; Guilbeault, A. Microaerosol Administration of Synthetic β-γ-Dipalmitoyl-L-α-Lecithin in the Respiratory Distress Syndrome: A Preliminary Report. Can. Med. Assoc. J. 1964, 90, 55–57. [Google Scholar] [PubMed]
- Chu, J.; Clements, J.A.; Cotton, E.K.; Klaus, M.H.; Sweet, A.Y.; Tooley, W.H.; Bradley, B.L.; Brandorff, L.C. Neonatal Pulmonary Ischemia. Pediatrics 1967, 40, 709–782. [Google Scholar]
- Lewis, J.F.; Ikegami, M.; Jobe, A.H.; Tabor, B. Aerosolized surfactant treatment of preterm lambs. J. Appl. Physiol. 1991, 70, 869–876. [Google Scholar] [CrossRef] [PubMed]
- Henry, M.D.; Rebello, C.M.; Ikegami, M.; Jobe, A.H.; Langenback, E.G.; Davis, J.M. Ultrasonic Nebulized in Comparison with Instilled Surfactant Treatment of Preterm Lambs. Am. J. Respir. Crit. Care Med. 1996, 154, 366–375. [Google Scholar] [CrossRef] [PubMed]
- Fai Fok, T.; Al-Essa, M.; Dolovich, M.; Rasid, F.; Kirpalani, H. Nebulisation of surfactants in an animal model of neonatal respiratory distress. Arch. Dis. Child. Fetal Neonatol. Ed. 1998, 78, F3–F9. [Google Scholar] [CrossRef]
- Ellyett, K.M.; Broadbent, R.S.; Fawcett, E.R.; Campbell, A.J. Surfactant Aerosol Treatment of Respiratory Distress Syndrome in the Spontaneously Breathing Premature Rabbit. Pediatr. Res. 1996, 39, 953–957. [Google Scholar] [CrossRef][Green Version]
- Jorch, G.; Weller, E.; Murlat, A.; Hentschel, R. Feasibility study on nebulization of bovine surfactant (SF-RI 1) by pharyngeal continuous positive airway pressure (CPAP). Biol. Neonate 1994, 66. [Google Scholar]
- Berggren, E.; Liljedahl, M.; Winbladh, B.; Andreasson, B.; Curstedt, T.; Robertson, B.; Schollin, J. Pilot study of nebulized surfactant therapy for neonatal respiratory distress syndrome. Acta Pediatr. 2000, 89, 460–464. [Google Scholar] [CrossRef]
- Lampland, A.L.; Wolfson, M.R.; Mazela, J.; Henderson, C.; Gregory, T.J.; Meyers, P.; Plumm, B.; Worwa, C.; Mammel, M.C. Aerosolized KL4 surfactant improves short-term survival and gas exchange in spontaneously breathing newborn pigs with hydrochloric acid-induced acute lung injury. Pediatr. Pulmonol. 2014, 49, 482–489. [Google Scholar] [CrossRef]
- Pearson, R.; Pippins, M.; Niven, R.; Johnson, M.E. 185 Treatment of RDS Using Aerosolized KL4 Lung Surfactant in Combination with nCPAP. Pediatr. Res. 2005, 58, 386. [Google Scholar] [CrossRef][Green Version]
- Donn, S.; Sinha, S. Aerosolized lucinactant: A potential alternative to intratracheal surfactant replacement therapy. Expert Opin. Pharm. 2008, 9, 475–478. [Google Scholar] [CrossRef] [PubMed]
- Gaertner, V.D.; Bassler, D.; Ruegger, C.M. Does surfactant nebulization prevent early intubation in preterm infants? A protocol for a systematic review and meta-analysis. Syst. Rev. 2021, 10, 9. [Google Scholar] [CrossRef]
- Ari, A. Jet, Ultrasonic, and Mesh Nebulizers: An Evaluation of Nebulizers for Better Clinical Outcomes. Eurasian J. Pulmonol. 2014, 16, 1–7. [Google Scholar] [CrossRef]
- Gardenhire, D.S.; Burnett, D.; Strickland, S.; Myers, T.R. A Guide to Aerosol Delivery Devices for Respiratory Therapists. In Care AAfR, 4th ed.; AARC: Washington, DC, USA, 2017. [Google Scholar]
- Mazela, J.; Polin, R.A. Aerosol delivery to ventilated newborn infants: Historical challenges and new directions. Eur. J. Pediatr. 2011, 170, 433–444. [Google Scholar] [CrossRef] [PubMed]
- Pritchard, J.N.; Hatley, R.H.; Denyer, J.; von Hollen, D. Mesh nebulizers have become the first choice for new nebulized pharmaceutical drug developments. Ther. Deliv. 2018, 9, 121–136. [Google Scholar] [CrossRef] [PubMed]
- Kohler, E.; Jilg, G.; Avenarius, S.; Jorch, G. Lung deposition after inhalation with various nebulisers in preterm infants. Arch. Dis. Child Fetal Neonatal. Ed. 2008, 93, F275–F279. [Google Scholar] [CrossRef] [PubMed]
- Bianco, F.; Ricci, F.; Catozzi, C.; Murgia, X.; Schlun, M.; Bucholski, A.; Hetzer, U.; Bonelli, S.; Lombardini, M.; Pasini, E. From bench to bedside: In vitro and in vivo evaluation of a neonate-focused nebulized surfactant delivery strategy. Respir. Res. 2019, 20, 134. [Google Scholar] [CrossRef] [PubMed]
- Nord, A.; Bianco, F.; Salomone, F.; Ricci, F.; Schlun, M.; Linner, R.; Cunha-Goncalves, D. Nebulization of High-Dose Poractant Alfa in Newborn Piglets on Nasal Continuous Positive Airway Pressure Yields Therapeutic Lung Doses of Phospholipids. Am. J. Perinatol. 2020. [Google Scholar] [CrossRef]
- Milesi, I.; Tingay, D.G.; Zannin, E.; Bianco, F.; Tagliabue, P.; Mosca, F.; Lavizzari, A.; Ventura, M.L.; Zonneveld, C.E.; Perkins, E.J. Intratracheal atomized surfactant provides similar outcomes as bolus surfactant in preterm lambs with respiratory distress syndrome. Pediatr. Res. 2016, 80, 92–100. [Google Scholar] [CrossRef]
- Bianco, F.; Pasini, E.; Nutini, M.; Murgia, X.; Stoeckl, C.; Schlun, M.; Hetzer, U.; Bonelli, S.; Lombardini, M.; Milesi, I.; et al. Extended Pharmacopeial Characterization of Surfactant Aerosols Generated by a Customized eFlow Neos Nebulizer Delivered through Neonatal Nasal Prongs. Pharmaceutics 2020, 12, 319. [Google Scholar] [CrossRef]
- Rey-Santano, C.; Mielgo, V.; Gomez-Solaetxe, M.A.; Ricci, F.; Bianco, F.; Salomone, F.; Loureiro, B. Dose-Response Study on Surfactant Nebulization Therapy During Nasal Continuous Positive Airway Pressure Ventilation in Spontaneously Breathing Surfactant-Deficient Newborn Piglets. Pediatr. Crit. Care Med. 2020, 21, e456–e466. [Google Scholar] [CrossRef] [PubMed]
- Darquenne, C.; Schmid, O.; Kim Prisk, G. Aerosols and the Human Lung; World Scientific: Singapore, 2020. [Google Scholar]
- Cunha-Goncalves, D.; Nord, A.; Bianco, F.; Salomone, F.; Ricci, F.; Schlun, M.; Linner, R.; Perez-de-Sa, V. Impact of Body Position on Lung Deposition of Nebulized Surfactant in Newborn Piglets on Nasal Continuous Positive Airway Pressure. Neonatology 2020, 117, 467–473. [Google Scholar] [CrossRef]
- Asgharian, B.; Kelly, J.T.; Tewksbury, E.W. Respiratory deposition and inhalability of monodisperse aerosols in Long-Evans rats. Toxicol. Sci. 2003, 71, 104–111. [Google Scholar] [CrossRef]
- Syedain, Z.H.; Naqwi, A.A.; Dolovich, M.; Somani, A. In Vitro Evaluation of a Device for Intra-Pulmonary Aerosol Generation and Delivery. Aerosol. Sci. Technol. 2015, 49, 747–752. [Google Scholar] [CrossRef] [PubMed]
- Aramendia, I.; Fernandez-Gamiz, U.; Lopez-Arraiza, A.; Rey-Santano, C.; Mielgo, V.; Basterretxea, F.J.; Sancho, J.; Gomez-Solaetxe, M.A. Experimental and Numerical Modeling of Aerosol Delivery for Preterm Infants. Int. J. Environ. Res. Public Health 2018, 15, 423. [Google Scholar] [CrossRef] [PubMed]
- Borghardt, J.M.; Kloft, C.; Sharma, A. Inhaled Therapy in Respiratory Disease: The Complex Interplay of Pulmonary Kinetic Processes. Can. Respir. J. 2018, 2018, 2732017. [Google Scholar] [CrossRef] [PubMed]
- Hatch, L.D.; Grubb, P.H.; Lea, A.S.; Walsh, W.F.; Markham, M.H.; Whitney, G.M.; Slaughter, J.C.; Stark, A.R.; Ely, E.W. Endotracheal Intubation in Neonates: A Prospective Study of Adverse Safety Events in 162 Infants. J. Pediatr. 2016, 168, 62–66.e66. [Google Scholar] [CrossRef] [PubMed]
- Foglia, E.E.; Ades, A.; Napolitano, N.; Leffelman, J.; Nadkarni, V.; Nishisaki, A. Factors Associated with Adverse Events during Tracheal Intubation in the NICU. Neonatology 2015, 108, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Marshall, T.A.; Deeder, R.; Pai, S.; Berkowitz, G.P.; Austin, T.L. Physiologic changes associated with endotracheal intubation in preterm infants. Crit. Care Med. 1984, 12, 501–503. [Google Scholar] [CrossRef]
- Kelly, M.A.; Finer, N.N. Nasotracheal intubation in the neonate: Physiologic responses and effects of atropine and pancuronium. J. Pediatr. 1984, 105, 303–309. [Google Scholar] [CrossRef]
- Rentea, R.M.; St Peter, S.D. Neonatal and pediatric esophageal perforation. Semin. Pediatr. Surg. 2017, 26, 87–94. [Google Scholar] [CrossRef]
- O’Donnell, C.P.; Kamlin, C.O.; Davis, P.G.; Morley, C.J. Endotracheal intubation attempts during neonatal resuscitation: Success rates, duration, and adverse effects. Pediatrics 2006, 117, e16–e21. [Google Scholar] [CrossRef]
- Lane, B.; Finer, N.; Rich, W. Duration of intubation attempts during neonatal resuscitation. J. Pediatr. 2004, 145, 67–70. [Google Scholar] [CrossRef]
- Easley, R.B.; Segeleon, J.E.; Haun, S.E.; Tobias, J.D. Prospective study of airway management of children requiring endotracheal intubation before admission to a pediatric intensive care unit. Crit. Care Med. 2000, 28, 2058–2063. [Google Scholar] [CrossRef] [PubMed]
- Bismilla, Z.; Finan, E.; McNamara, P.J.; LeBlanc, V.; Jefferies, A.; Whyte, H. Failure of pediatric and neonatal trainees to meet Canadian Neonatal Resuscitation Program standards for neonatal intubation. J. Perinatol. 2010, 30, 182–187. [Google Scholar] [CrossRef] [PubMed]
- Parmekar, S.; Arnold, J.L.; Anselmo, C.; Pammi, M.; Hagan, J.; Fernandes, C.J.; Lingappan, K. Mind the gap: Can videolaryngoscopy bridge the competency gap in neonatal endotracheal intubation among pediatric trainees? a randomized controlled study. J. Perinatol. 2017, 37, 979–983. [Google Scholar] [CrossRef] [PubMed]
- Falck, A.J.; Escobedo, M.B.; Baillargeon, J.G.; Villard, L.G.; Gunkel, J.H. Proficiency of pediatric residents in performing neonatal endotracheal intubation. Pediatrics 2003, 112, 1242–1247. [Google Scholar] [CrossRef]
- Carvalho, C.G.; Silveira, R.C.; Procianoy, R.S. Ventilator-induced lung injury in preterm infants. Rev. Bras. Ter. Intensiva 2013, 25, 319–326. [Google Scholar] [CrossRef]
- Jobe, A.H. Mechanisms of Lung Injury and Bronchopulmonary Dysplasia. Am. J. Perinatol. 2016, 33, 1076–1078. [Google Scholar] [CrossRef] [PubMed]
- Bjorklund, L.J.; Ingimarsson, J.; Curstedt, T.; John, J.; Robertson, B.; Werner, O.; Vilstrup, C.T. Manual ventilation with a few large breaths at birth compromises the therapeutic effect of subsequent surfactant replacement in immature lambs. Pediatr. Res. 1997, 42, 348–355. [Google Scholar] [CrossRef] [PubMed]
- Thomson, M.A.; Yoder, B.A.; Winter, V.T.; Giavedoni, L.; Chang, L.Y.; Coalson, J.J. Delayed extubation to nasal continuous positive airway pressure in the immature baboon model of bronchopulmonary dysplasia: Lung clinical and pathological findings. Pediatrics 2006, 118, 2038–2050. [Google Scholar] [CrossRef] [PubMed]
- Garland, J.S. Strategies to prevent ventilator-associated pneumonia in neonates. Clin. Perinatol. 2010, 37, 629–643. [Google Scholar] [CrossRef] [PubMed]
- Attar, M.A.; Donn, S.M. Mechanisms of ventilator-induced lung injury in premature infants. Semin Neonatol. 2002, 7, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Bancalari, E.; Gerhardt, T. Bronchopulmonary dysplasia. Pediatr. Clin. N. Am. 1986, 33, 1–23. [Google Scholar] [CrossRef]
- Strong, R.M.; Passy, V. Endotracheal intubation. Complications in neonates. Arch. Otolaryngol. 1977, 103, 329–335. [Google Scholar] [CrossRef] [PubMed]
- Knisely, A.S.; Leal, S.M.; Singer, D.B. Abnormalities of diaphragmatic muscle in neonates with ventilated lungs. J. Pediatr. 1988, 113, 1074–1077. [Google Scholar] [CrossRef]
- Powers, S.K.; Kavazis, A.N.; Levine, S. Prolonged mechanical ventilation alters diaphragmatic structure and function. Crit. Care Med. 2009, 37, S347–S353. [Google Scholar] [CrossRef] [PubMed]
- Sassoon, C.S. Ventilator-associated diaphragmatic dysfunction. Am. J. Respir. Crit. Care Med. 2002, 166, 1017–1018. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Denson, S.E.; Mancuso, T.J.; Committee on Fetus and Newborn; Section on Anesthesiology and Pain Medicine. Premedication for nonemergency endotracheal intubation in the neonate. Pediatrics 2010, 125, 608–615. [Google Scholar] [CrossRef] [PubMed]
- A Dose-Ranging Study to Determine the Efficacy, Safety and Tolerability of AeroFact. Available online: https://ClinicalTrials.gov/show/NCT03969992 (accessed on 17 December 2020).
- Administration of Surfactant through an Instillation Device Infasurf® (Calfactant) in Neonates—A Pilot Study. Available online: https://ClinicalTrials.gov/show/NCT04056741 (accessed on 17 December 2020).
- Surfactant Nebulization for the Early Aeration of the Preterm Lung. Available online: https://ClinicalTrials.gov/show/NCT04315636 (accessed on 17 December 2020).
| Study | Population (n) | Nebulizer (Type) | Interface | Surfactant | Dose | Flow | Particle Size | Comparison | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| Jorch et al., 1994 | 28–35 wk GA (20) | Intersurgical RO252/ME (jet) | Modified nasopharyngeal tube placed behind soft palate | Beractant | 150 mg/kg per treatment | 8 L/min | <4 µm | Pre/post treatment | Significant improvement of A-a gradient, PaCO2, and Silverman score |
| Berggren et al., 2000 | 27–34 wk GA (34) | Aiolos ® (jet) | Infant Flow System® nasal CPAP | Poractant alfa | 480 mg | 7 L/min | <2 µm | Aerosolized surfactant vs. CPAP alone | No benefit in treatment group |
| Finer et al., 2010 | 28–32 wk GA (17) | Aeroneb Pro ® (vibrating mesh) | Fisher-Paykel nasal prongs | Lucinactant | 72 mg per treatment | 1 L/min | 1.9 ± 0.3 µm | Pre/post treatment Historic control intubation rate | Mean FiO2 decreased after treatment. 30–32 wk GA infant intubation rate lower than historic control |
| Sood et al., 2019 | 24–36 wk GA (17) | Low Flow MiniHeart (jet) | Short binasal prongs | Beractant | 100–200 mg/kg per treatment | 2 L/min or less | Not reported | Pre/post treatment | Decrease in heart rate and pCO2; increase in pH |
| Minocchieri et al., 2019 | 29–33.6 wk GA (64) | eFlow-Neos (vibrating mesh) | Face mask (not specified) | Poractant alfa | 200 mg/kg per treatment | 6–8 L/min | Not reported | Aerosolized surfactant vs. CPAP alone | Decreased intubation rate in treated 32–33.6 wk GA subgroup |
| Cummings et al., 2020 | 23–41 wk GA (457) | Modified Solarys (pneumatically driven) | Custom pacifier mouthpiece | Calfactant | 210 mg/kg per treatment | 8–10 L/min | 4.5 µm | Aerosolized surfactant vs. usual care | Decreased intubation rate in treated infants |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brasher, M.; Raffay, T.M.; Cunningham, M.D.; Abu Jawdeh, E.G. Aerosolized Surfactant for Preterm Infants with Respiratory Distress Syndrome. Children 2021, 8, 493. https://doi.org/10.3390/children8060493
Brasher M, Raffay TM, Cunningham MD, Abu Jawdeh EG. Aerosolized Surfactant for Preterm Infants with Respiratory Distress Syndrome. Children. 2021; 8(6):493. https://doi.org/10.3390/children8060493
Chicago/Turabian StyleBrasher, Mandy, Thomas M. Raffay, M. Douglas Cunningham, and Elie G. Abu Jawdeh. 2021. "Aerosolized Surfactant for Preterm Infants with Respiratory Distress Syndrome" Children 8, no. 6: 493. https://doi.org/10.3390/children8060493
APA StyleBrasher, M., Raffay, T. M., Cunningham, M. D., & Abu Jawdeh, E. G. (2021). Aerosolized Surfactant for Preterm Infants with Respiratory Distress Syndrome. Children, 8(6), 493. https://doi.org/10.3390/children8060493






