Application of a Multiplex Polymerase Chain Reaction Test for Diagnosing Bacterial Enteritis in Children in a Real-Life Clinical Setting
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Study Design
2.2. Microbiological Test
2.3. Statistical Analysis
3. Results
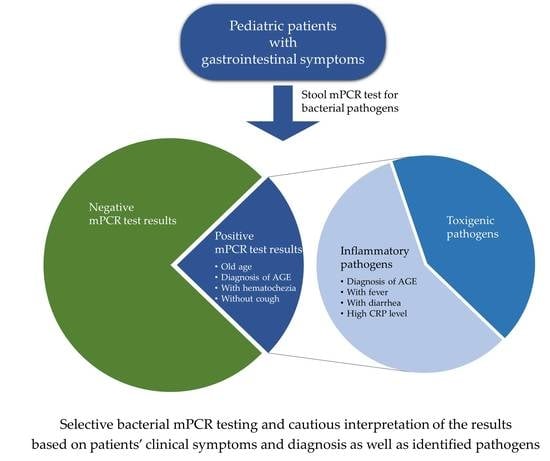
3.1. Comparison between the Positive and Negative mPCR Test Groups
3.2. Comparison between the Invasive Pathogen and Toxigenic Pathogen Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yi, J.; Shane, A. Approach to the diagnosis and management of gastrointestinal tract infections. In Principles and Practice of Pediatric Infectious Diseases, 5th ed.; Long, S.S., Prober, C.G., Fischer, M., Eds.; Elsevier: Philadelphia, PA, USA, 2018; pp. 376–383. [Google Scholar]
- Anderson, N.W.; Tarr, P.I. Multiplex nucleic acid amplification testing to diagnose gut infections: Challenges, opportunities, and result interpretation. Gastroenterol. Clin. N. Am. 2018, 47, 793–812. [Google Scholar] [CrossRef]
- Wohlwend, N.; Tiermann, S.; Risch, L.; Risch, M.; Bodmer, T. Evaluation of a multiplex real-time PCR assay for detecting major bacterial enteric pathogens in fecal specimens: Intestinal inflammation and bacterial load are correlated in Campylobacter infections. J. Clin. Microbiol. 2016, 54, 2262–2266. [Google Scholar] [CrossRef][Green Version]
- Kellner, T.; Parsons, B.; Chui, L.; Berenger, B.M.; Xie, J.; Burnham, C.A.; Tarr, P.I.; Lee, B.E.; Nettel-Aguirre, A.; Szelewicki, J.; et al. Comparative evaluation of enteric bacterial culture and a molecular multiplex syndromic panel in children with acute gastroenteritis. J. Clin. Microbiol. 2019, 57, e00205-19. [Google Scholar] [CrossRef]
- Cybulski, R.J., Jr.; Bateman, A.C.; Bourassa, L.; Bryan, A.; Beail, B.; Matsumoto, J.; Cookson, B.T.; Fang, F.C. Clinical impact of a multiplex gastrointestinal polymerase chain reaction panel in patients with acute gastroenteritis. Clin. Infect. Dis. 2018, 67, 1688–1696. [Google Scholar] [CrossRef]
- O’Leary, J.; Corcoran, D.; Lucey, B. Comparison of the EntericBio multiplex PCR system with routine culture for detection of bacterial enteric pathogens. J. Clin. Microbiol. 2009, 47, 3449–3453. [Google Scholar] [CrossRef]
- De Boer, R.F.; Ott, A.; Kesztyus, B.; Kooistra-Smid, A.M. Improved detection of five major gastrointestinal pathogens by use of a molecular screening approach. J. Clin. Microbiol. 2010, 48, 4140–4146. [Google Scholar] [CrossRef]
- Buss, S.N.; Leber, A.; Chapin, K.; Fey, P.D.; Bankowski, M.J.; Jones, M.K.; Rogatcheva, M.; Kanack, K.J.; Bourzac, K.M. Multicenter evaluation of the BioFire FilmArray gastrointestinal panel for etiologic diagnosis of infectious gastroenteritis. J. Clin. Microbiol. 2015, 53, 915–925. [Google Scholar] [CrossRef] [PubMed]
- Harrington, S.M.; Buchan, B.W.; Doern, C.; Fader, R.; Ferraro, M.J.; Pillai, D.R.; Rychert, J.; Doyle, L.; Lainesse, A.; Karchmer, T.; et al. Multicenter evaluation of the BD max enteric bacterial panel PCR assay for rapid detection of Salmonella spp., Shigella spp., Campylobacter spp. (C. jejuni and C. coli), and Shiga toxin 1 and 2 genes. J. Clin. Microbiol. 2015, 53, 1639–1647. [Google Scholar] [CrossRef] [PubMed]
- Claas, E.C.; Burnham, C.A.; Mazzulli, T.; Templeton, K.; Topin, F. Performance of the xTAG(R) gastrointestinal pathogen panel, a multiplex molecular assay for simultaneous detection of bacterial, viral, and parasitic causes of infectious gastroenteritis. J. Microbiol. Biotechnol. 2013, 23, 1041–1045. [Google Scholar] [CrossRef]
- Onori, M.; Coltella, L.; Mancinelli, L.; Argentieri, M.; Menichella, D.; Villani, A.; Grandin, A.; Valentini, D.; Raponi, M.; Russo, C. Evaluation of a multiplex PCR assay for simultaneous detection of bacterial and viral enteropathogens in stool samples of paediatric patients. Diagn. Microbiol. Infect. Dis. 2014, 79, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R. Diarrhea. In Pediatric Gastrointestinal and Liver Disease, 5th ed.; Wyllie, R., Hyams, J.S., Kay, M., Eds.; Elsevier: Philadelphia, PA, USA, 2016; pp. 104–114. [Google Scholar]
- Li, B.; Kovaci, K. Vomiting. In Pediatric Gastrointestinal and Liver Disease, 5th ed.; Wyllie, R., Hyams, J.S., Kay, M., Eds.; Elsevier: Philadelphia, PA, USA, 2016; pp. 84–103. [Google Scholar]
- Kotloff, K.L. Acute gastroenteritis in children. In Nelson Textbook of Pediatrics, 21th ed.; Kliegman, R.M., St Geme, J.W., Blum, N.J., Shah, S.S., Tasker, R.C., Wilson, K.M., Eds.; Elsevier: Philadelphia, PA, USA, 2020; pp. 2012–2033. [Google Scholar]
- Friesema, I.H.; de Boer, R.F.; Duizer, E.; Kortbeek, L.M.; Notermans, D.W.; Norbruis, O.F.; Bezemer, D.D.L.; van Heerbeek, H.; van Andel, R.N.J.; van Enk, J.G.; et al. Etiology of acute gastroenteritis in children requiring hospitalization in the Netherlands. Eur. J. Clin. Microbiol. Infect. Dis. 2012, 31, 405–415. [Google Scholar] [CrossRef]
- Xie, J.; Nettel-Aguirre, A.; Lee, B.E.; Chui, L.; Pang, X.L.; Zhuo, R.; Parsons, B.; Vanderkooi, O.G.; Tarr, P.I.; Ali, S.; et al. Relationship between enteric pathogens and acute gastroenteritis disease severity: A prospective cohort study. Clin. Microbiol. Infect. 2019, 25, 454–461. [Google Scholar] [CrossRef]
- Fisher, R.G.; Boyce, T.G.; Correa, A.G. Moffet’s Pediatric Infectious Diseases: A Problem-Oriented Approach, 5th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2017; pp. 1–12. [Google Scholar]
- Schutze, G.E.; Willoughby, R.E.; Committee on Infectious Diseases; American Academy of Pediatrics. Clostridium difficile infection in infants and children. Pediatrics 2013, 131, 196–200. [Google Scholar] [PubMed]
- McDonald, L.C.; Gerding, D.N.; Johnson, S.; Bakken, J.S.; Carroll, K.C.; Coffin, S.E.; Dubberke, E.R.; Garey, K.W.; Gould, C.V.; Kelly, C.; et al. Clinical Practice Guidelines for Clostridium difficile infection in adults and children: 2017 update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin. Infect. Dis. 2018, 66, e1–e48. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.; Ahmed, S.; Sheng, Y.J.; Sun, C.; Deng, C.L.; Ojhac, S.C. Diagnostic accuracy of nucleic acid amplification-based assays for Clostridium perfringens-associated diseases: A systematic review and meta-analysis. J. Clin. Microbiol. 2020, 58, e00363-20. [Google Scholar] [CrossRef] [PubMed]
- Muller, M.; Overturf, G.D. Clostridial intoxication and infection. In Feigin and Cherry’s Textbook of Pediatric Infectious Diseases, 8th ed.; Cherry, J.D., Harrison, G.J., Kaplan, S.L., Steinbach, W.J., Hotez, P.J., Eds.; Elsevier: Philadelphia, PA, USA, 2019; pp. 1291–1298. [Google Scholar]
- Janssen, R.; Krogfelt, K.A.; Cawthraw, S.A.; van Pelt, W.; Wagenaar, J.A.; Owen, R.J. Host-pathogen interactions in Campylobacter infections: The host perspective. Clin. Microbiol. Rev. 2008, 21, 505–518. [Google Scholar] [CrossRef]
- Gal-Mor, O. Persistent infection and long-term carriage of typhoidal and nontyphoidal salmonellae. Clin. Microbiol. Rev. 2019, 32, e00088-18. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.; Hong, S.; Chun, J.; Hwang, K.J. Laboratory-based surveillance of water- and food-borne infectious disease-causing bacteria in the Republic of Korea, 2016–2018. Public Health Wkly. Rep. 2019, 12, 898–903. [Google Scholar]
- Spina, A.; Kerr, K.G.; Cormican, M.; Barbut, F.; Eigentler, A.; Zerva, L.; Tassios, P.; Popescu, G.A.; Rafila, A.; Eerola, E.; et al. Spectrum of enteropathogens detected by the FilmArray GI Panel in a multicentre study of community-acquired gastroenteritis. Clin. Microbiol. Infect. 2015, 21, 719–728. [Google Scholar] [CrossRef] [PubMed]
- Shane, A.L.; Mody, R.K.; Crump, J.A.; Tarr, P.I.; Steiner, T.S.; Kotloff, K.; Langley, J.M.; Wanke, C.; Warren, C.A.; Cheng, A.C.; et al. 2017 Infectious Diseases Society of America Clinical Practice Guidelines for the diagnosis and management of infectious diarrhea. Clin. Infect. Dis. 2017, 65, e45–e80. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, H.J.; Lim, S.; Bae, K.S.; Han, S.B.; Jeong, D.C.; Kang, J.H.; Shin, G.J.; Lee, G.D.; Park, Y.J. Community-acquired Escherichia coli enteritis in Korean children: The clinical application of a stool polymerase chain reaction assay. Infect. Chemother. 2017, 49, 275–281. [Google Scholar] [CrossRef] [PubMed]
| Bacteria | Number of Patients (n = 199) |
|---|---|
| Campylobacter spp. | 56 (28.1) |
| Clostridium difficile | 44 (22.1) |
| Salmonella spp. | 39 (19.6) |
| Clostridium perfringens | 26 (13.1) |
| Aeromonas spp. | 7 (3.5) |
| Verotoxin-producing Escherichia coli | 3 (1.5) |
| Shigella spp. | 1 (0.5) |
| E. coli O157/H7 | 1 (0.5) |
| Yersinia spp. | 1 (0.5) |
| Vibrio spp. | 0 (0.0) |
| Co-detection | 21 (10.6) |
| Salmonella spp. and C. perfringens | 5 (2.5) |
| Salmonella spp. and Aeromonas spp. | 1 (0.5) |
| Salmonella spp., C. perfringens and Aeromonas spp. | 1 (0.5) |
| Campylobacter spp. and C. perfringens | 4 (2.0) |
| Campylobacter spp. and Aeromonas spp. | 2 (1.0) |
| Campylobacter spp. and C. difficile | 1 (0.5) |
| Campylobacter spp., C. difficile and Aeromonas spp. | 1 (0.5) |
| C. difficile and C. perfringens | 5 (2.5) |
| C. difficile and Shigella spp. | 1 (0.5) |
| Factor | Negative mPCR Test Group (n = 511) | Positive mPCR Test Group (n = 199) | p-Value |
|---|---|---|---|
| Demographic factor | |||
| Male sex | 284 (55.6) | 116 (58.3) | 0.513 |
| Age, years, median (IQR) | 4 (1–8) | 6 (3–11) | <0.001 |
| Clinical diagnosis | <0.001 | ||
| AGE | 304 (59.5) | 163 (81.9) | |
| Non-AGE | 207 (40.5) | 36 (18.1) | |
| URI | 79 (15.5) | 13 (6.5) | |
| LRI | 47 (9.2) | 6 (3.0) | |
| Other GI disorders | 28 (5.5) | 5 (2.5) | |
| FWLS | 17 (3.3) | 4 (2.0) | |
| Urinary tract infection | 12 (2.3) | 1 (0.5) | |
| Exanthem subitum | 9 (1.8) | 3 (1.5) | |
| CNS disorders | 7 (1.4) | 3 (1.5) | |
| Others | 8 (1.6) | 1 (0.5) | |
| Clinical symptoms | |||
| Fever | 383 (75.0) | 173 (86.9) | 0.001 |
| Vomiting | 310 (60.7) | 106 (53.3) | 0.072 |
| Diarrhea | 314 (61.4) | 156 (78.8) | <0.001 |
| Abdominal pain | 279 (54.7) | 144 (72.4) | <0.001 |
| Hematochezia | 27 (5.3) | 35 (17.6) | <0.001 |
| Cough | 143 (28.0) | 18 (9.0) | <0.001 |
| Rhinorrhea | 147 (28.8) | 27 (13.6) | <0.001 |
| Sputum | 109 (21.3) | 16 (8.0) | <0.001 |
| Sore throat | 18 (3.5) | 6 (3.0) | 0.737 |
| Laboratory finding, median (IQR) | |||
| WBC count, cells/μL | 10,450 (7500–13,600) | 9900 (7000–13,100) | 0.153 |
| ANC, cells/μL | 6474 (4046–9840) | 7050 (4320–10,350) | 0.365 |
| ALC, cells/μL | 2085 (1290–3289) | 1463 (1068–2496) | <0.001 |
| ESR, mm/h | 7 (2–17) | 13 (5–21) | <0.001 |
| CRP, mg/dL | 1.12 (0.17–3.99) | 3.63 (0.78–7.83) | <0.001 |
| Factor | Odds Ratio | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Age, years | 1.099 | 1.044–1.158 | <0.001 |
| Diagnosis of AGE (vs. non-AGE) | 1.935 | 1.105–3.389 | 0.021 |
| Fever | 2.877 | 1.628–5.082 | <0.001 |
| Diarrhea | 1.552 | 0.962–2.504 | 0.072 |
| Abdominal pain | 0.889 | 0.548–1.442 | 0.633 |
| Hematochezia | 5.011 | 2.675–9.385 | <0.001 |
| Cough | 0.203 | 0.069–0.602 | 0.004 |
| Rhinorrhea | 1.779 | 0.785–4.027 | 0.167 |
| Sputum | 1.153 | 0.407–3.270 | 0.789 |
| ALC, cells/μL | 1.000 | 1.000–1.000 | 0.619 |
| ESR, mm/h | 1.001 | 0.991–1.010 | 0.906 |
| CRP, mg/dL | 1.033 | 0.987–1.082 | 0.156 |
| Factor | Invasive Pathogen Group (n = 95) | Toxigenic Pathogen Group (n = 70) | p-Value |
|---|---|---|---|
| Demographic factor | |||
| Male sex | 56 (58.9) | 41 (58.6) | 0.961 |
| Age, years, median (IQR) | 8 (4–12) | 5 (1–11) | 0.009 |
| Age group | 0.009 | ||
| <2 years | 8 (8.4) | 18 (25.7) | |
| 2–8 years | 43 (45.3) | 28 (40.0) | |
| >8 years | 44 (46.3) | 24 (34.3) | |
| Clinical diagnosis | <0.001 | ||
| AGE | 92 (96.8) | 44 (62.9) | |
| Non-AGE | 3 (3.2) | 26 (37.1) | |
| URI | 1 (1.1) | 10 (14.3) | |
| LRI | 0 (0.0) | 5 (7.1) | |
| Other GI disorders | 1 (1.1) | 3 (4.3) | |
| FWLS | 1 (1.1) | 1 (1.4) | |
| Urinary tract infection | 0 (0.0) | 1 (1.4) | |
| Exanthem subitum | 0 (0.0) | 2 (2.9) | |
| CNS disorders | 0 (0.0) | 3 (4.3) | |
| Others | 0 (0.0) | 1 (1.4) | |
| Clinical symptoms | |||
| Fever | 94 (98.9) | 51 (72.9) | <0.001 |
| Vomiting | 44 (46.3) | 45 (64.3) | 0.022 |
| Diarrhea | 91 (95.8) | 39 (56.5) | <0.001 |
| Abdominal pain | 83 (87.4) | 39 (55.7) | <0.001 |
| Hematochezia | 22 (23.2) | 8 (11.4) | 0.054 |
| Cough | 4 (4.2) | 12 (17.1) | 0.006 |
| Rhinorrhea | 7 (7.4) | 15 (21.7) | 0.008 |
| Sputum | 3 (3.2) | 10 (14.3) | 0.009 |
| Sore throat | 4 (4.2) | 0 (0.0) | 0.138 |
| Laboratory finding, median (IQR) | |||
| WBC count, cells/μL | 9900 (6900–12,850) | 9600 (6700–12,950) | 0.765 |
| ANC, cells/μL | 7050 (4906–10,042) | 5588 (3234–10,946) | 0.215 |
| ALC, cells/μL | 1380 (1045–1730) | 1970 (938–3661) | 0.019 |
| ESR, mm/h | 17 (11–23) | 5 (2–13) | <0.001 |
| CRP, mg/dL | 6.53 (3.04–9.89) | 0.56 (0.21–2.47) | <0.001 |
| Factor | Odds Ratio | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Age, years | 1.013 | 0.892–1.150 | 0.847 |
| Diagnosis of AGE (vs. non-AGE) | 37.846 | 3.498–409.472 | 0.003 |
| Fever | 13.394 | 1.350–132.889 | 0.027 |
| Vomiting | 0.417 | 0.145–1.197 | 0.104 |
| Diarrhea | 5.007 | 1.050–23.874 | 0.043 |
| Abdominal pain | 2.014 | 0.492–8.252 | 0.330 |
| Cough | 0.145 | 0.003–6.807 | 0.326 |
| Rhinorrhea | 1.807 | 0.113–28.976 | 0.676 |
| Sputum | 9.399 | 0.382–231.491 | 0.170 |
| ALC, cells/μL | 1.000 | 1.000–1.000 | 0.855 |
| ESR, mm/h | 1.059 | 0.997–1.125 | 0.064 |
| CRP, mg/dL | 1.187 | 1.021–1.379 | 0.025 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.-W.; Han, S.-B.; Rhim, J.-W. Application of a Multiplex Polymerase Chain Reaction Test for Diagnosing Bacterial Enteritis in Children in a Real-Life Clinical Setting. Children 2021, 8, 538. https://doi.org/10.3390/children8070538
Lee H-W, Han S-B, Rhim J-W. Application of a Multiplex Polymerase Chain Reaction Test for Diagnosing Bacterial Enteritis in Children in a Real-Life Clinical Setting. Children. 2021; 8(7):538. https://doi.org/10.3390/children8070538
Chicago/Turabian StyleLee, Hyun-Woo, Seung-Beom Han, and Jung-Woo Rhim. 2021. "Application of a Multiplex Polymerase Chain Reaction Test for Diagnosing Bacterial Enteritis in Children in a Real-Life Clinical Setting" Children 8, no. 7: 538. https://doi.org/10.3390/children8070538
APA StyleLee, H.-W., Han, S.-B., & Rhim, J.-W. (2021). Application of a Multiplex Polymerase Chain Reaction Test for Diagnosing Bacterial Enteritis in Children in a Real-Life Clinical Setting. Children, 8(7), 538. https://doi.org/10.3390/children8070538