Clinical Significance of Gray to White Matter Ratio after Cardiopulmonary Resuscitation in Children
Abstract
:1. Introduction
2. Methods
Statistical Analyses
3. Results
3.1. Patient Characteristics
3.2. EEG Findings after Cardiac Arrest
3.3. Neurologic Outcome after Cardiac Arrest: GOS-E Peds Score
3.4. Comparison of Absolute Attenuation and GWR among Survivor, Non-Survivor and Controls
3.5. Logistic Regression of Absolute Attenuation in Hounsfield Units and Grey/White Matter Ratio According to Survival
3.6. Logistic Regression of Absolute Attenuation in Hounsfield Units and Grey/White Matter Ratio According to Neurologic Outcome
3.7. ROC Analyses
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Böttiger, B.W.; Grabner, C.; Bauer, H.; Bode, C.; Weber, T.; Motsch, J.; Martin, E. Long term outcome after out-of-hospital cardiac arrest with physician staffed emergency medical services: The Utstein style applied to a midsized urban/suburban area. Heart 1999, 82, 674–679. [Google Scholar] [CrossRef] [PubMed]
- Huang, B.Y.; Castillo, M. Hypoxic-ischemic brain injury: Imaging findings from birth to adulthood. Radiographics 2008, 28, 417–439; quiz 617. [Google Scholar] [CrossRef]
- Hofmeijer, J.; Beernink, T.M.; Bosch, F.H.; Beishuizen, A.; Tjepkema-Cloostermans, M.C.; van Putten, M.J. Early EEG contributes to multimodal outcome prediction of postanoxic coma. Neurology 2015, 85, 137–143. [Google Scholar] [CrossRef] [Green Version]
- Choi, S.P.; Park, H.K.; Park, K.N.; Kim, Y.M.; Ahn, K.J.; Choi, K.H.; Lee, W.J.; Jeong, S.K. The density ratio of grey to white matter on computed tomography as an early predictor of vegetative state or death after cardiac arrest. Emerg. Med. J. 2008, 25, 666–669. [Google Scholar] [CrossRef]
- Scheel, M.; Storm, C.; Gentsch, A.; Nee, J.; Luckenbach, F.; Ploner, C.J.; Leithner, C. The prognostic value of gray-white-matter ratio in cardiac arrest patients treated with hypothermia. Scand. J. Trauma Resusc. Emerg. Med. 2013, 21, 23. [Google Scholar] [CrossRef] [Green Version]
- Starling, R.M.; Shekdar, K.; Licht, D.; Nadkarni, V.M.; Berg, R.A.; Topjian, A.A. Early Head CT Findings Are Associated With Outcomes After Pediatric Out-of-Hospital Cardiac Arrest. Pediatr. Crit. Care Med. 2015, 16, 542–548. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, D.; Ryoo, E.; Kim, H.J. Combination of Early EEG, Brain CT. Ammonia Level Is Useful to Predict Neurologic Outcome in Children Resuscitated From Cardiac Arrest. Front. Pediatr. 2019, 7, 223. [Google Scholar] [CrossRef] [PubMed]
- Tetsuhara, K.; Kaku, N.; Watanabe, Y.; Kumamoto, M.; Ichimiya, Y.; Mizuguchi, S.; Higashi, K.; Matsuoka, W.; Motomura, Y.; Sanefuji, M.; et al. Predictive values of early head computed tomography for survival outcome after cardiac arrest in childhood: A pilot study. Sci. Rep. 2021, 11, 12090. [Google Scholar] [CrossRef]
- Metter, R.B.; Rittenberger, J.C.; Guyette, F.X.; Callaway, C.W. Association between a quantitative CT scan measure of brain edema and outcome after cardiac arrest. Resuscitation 2011, 82, 1180–1185. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jennett, B.; Bond, M. Assessment of outcome after severe brain damage. Lancet 1975, 1, 480–484. [Google Scholar] [CrossRef]
- Beers, S.R.; Wisniewski, S.R.; Garcia-Filion, P.; Tian, Y.; Hahner, T.; Berger, R.P.; Bell, M.J.; Adelson, P.D. Validity of a pediatric version of the Glasgow Outcome Scale-Extended. J. Neurotrauma. 2012, 29, 1126–1139. [Google Scholar] [CrossRef] [Green Version]
- Michelson, K.A.; Hudgins, J.D.; Monuteaux, M.C.; Bachur, R.G.; Finkelstein, J.A. Cardiac Arrest Survival in Pediatric and General Emergency Departments. Pediatrics 2018, 141, e20172741. [Google Scholar] [CrossRef] [Green Version]
- Atkins, D.L.; Everson-Stewart, S.; Sears, G.K.; Daya, M.; Osmond, M.H.; Warden, C.R.; Berg, R.A. Epidemiology and outcomes from out-of-hospital cardiac arrest in children: The Resuscitation Outcomes Consortium Epistry-Cardiac Arrest. Circulation 2009, 119, 1484–1491. [Google Scholar] [CrossRef] [Green Version]
- Jayaram, N.; McNally, B.; Tang, F.; Chan, P.S. Survival After Out-of-Hospital Cardiac Arrest in Children. J. Am. Heart Assoc. 2015, 4, e002122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajan, S.; Wissenberg, M.; Folke, F.; Hansen, C.M.; Lippert, F.K.; Weeke, P.; Karlsson, L.; Søndergaard, K.B.; Kragholm, K.; Christensen, E.F.; et al. Out-of-hospital cardiac arrests in children and adolescents: Incidences, outcomes, household socioeconomic status. Resuscitation 2015, 88, 12–19. [Google Scholar] [CrossRef]
- Bouwes, A.; Binnekade, J.M.; Kuiper, M.A.; Bosch, F.H.; Zandstra, D.F.; Toornvliet, A.C.; Biemond, H.S.; Kors, B.M.; Koelman, J.H.; Verbeek, M.M.; et al. Prognosis of coma after therapeutic hypothermia: A prospective cohort study. Ann. Neurol 2012, 71, 206–212. [Google Scholar] [CrossRef] [PubMed]
- Samaniego, E.A.; Mlynash, M.; Caulfield, A.F.; Eyngorn, I.; Wijman, C.A. Sedation confounds outcome prediction in cardiac arrest survivors treated with hypothermia. Neurocrit. Care 2011, 15, 113–119. [Google Scholar] [CrossRef] [Green Version]
- Koenig, M.A.; Kaplan, P.W.; Thakor, N.V. Clinical neurophysiologic monitoring and brain injury from cardiac arrest. Neurol. Clin. 2006, 24, 89–106. [Google Scholar] [CrossRef]
- Gendo, A.; Kramer, L.; Häfner, M.; Funk, G.C.; Zauner, C.; Sterz, F.; Holzer, M.; Bauer, E.; Madl, C. Time-dependency of sensory evoked potentials in comatose cardiac arrest survivors. Intensive Care Med. 2001, 27, 1305–1311. [Google Scholar] [CrossRef]
- Yanagawa, Y.; Un-no, Y.; Sakamoto, T.; Okada, Y. Cerebral density on CT immediately after a successful resuscitation of cardiopulmonary arrest correlates with outcome. Resuscitation 2005, 64, 97–101. [Google Scholar] [CrossRef]
- Torbey, M.T.; Selim, M.; Knorr, J.; Bigelow, C.; Recht, L. Quantitative analysis of the loss of distinction between gray and white matter in comatose patients after cardiac arrest. Stroke 2000, 31, 2163–2167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kjos, B.O.; Brant-Zawadzki, M.; Young, R.G. Early CT findings of global central nervous system hypoperfusion. AJR Am. J. Roentgenol. 1983, 141, 1227–1232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geraghty, M.C.; Torbey, M.T. Neuroimaging and serologic markers of neurologic injury after cardiac arrest. Neurol. Clin. 2006, 24, 107–121. [Google Scholar] [CrossRef] [PubMed]



| Characteristics | Total (n = 56) | Survivor (n = 24) | Non-Survivor (n = 32) | p Value |
|---|---|---|---|---|
| Age (yrs) | 5.5 (0–13) | 5.5 (0.5–13) | 2.5 (1–8.5) | 0.555 |
| Female, n (%) | 18 (32.1) | 7 (29.2) | 11 (34.4) | 0.197 |
| Primary cause of arrest | 0.010 | |||
| Cardiac, n (%) | 13 (23.2) | 8 (33.3) | 5 (15.6) | |
| Respiratory, n (%) | 28 (50.0) | 15 (62.5) | 13 (40.6) | |
| Other, n (%) | 15 (26.8) | 1 (4.2) | 14 (43.6) | |
| Shockable arrhythmia, n (%) | 14 (25.0) | 8 (33.3) | 6 (18.8) | 0.216 |
| Seizure, n (%) | 28 (50.0) | 17 (70.8) | 11 (34.4) | 0.006 |
| Sepsis, n (%) | 4 (7.1) | 1 (4.2) | 3 (9.4) | 0.099 |
| Duration of CPR (min) | 15 (5–28.3) | 5 (2.0–10.0) | 18 (13.7–30) | <0.001 |
| CT after ROCS (hr) | 3 (1–12.2) | 5 (1.3–20.7) | 2(1–5.5) | 0.141 |
| Length of ICU stay (day) | 10 (3–30) | 13.5 (9.0–24.5) | 8 (3.0–22.6) | 0.174 |
| Initial NSE (ng/mL) | 43.2 (31.0–56.5) | 37.8 (26.4–51.3) | 43.2 (38.2–109.9) | 0.241 |
| Lactate (mmol/L) | 10.7 (4.9–15.7) | 9.4 (4.9–11.9) | 12.3 (4.2–17.2) | 0.138 |
| Antiepileptics, n (%) | 33 (58.9) | 20 (83.3) | 13 (40.6) | 0.001 |
| Use of ECMO, n (%) | 2 (3.6) | 1 (4.2) | 1 (3.1) | 0.836 |
| EEG done, n (%) | 38 (67.8) | 21(87.5) | 17 (53.1) | 0.006 |
| EEG finding | 0.003 | |||
| Normal, n (%) | 2 (5.3) | 1 (4.8) | 1 (5.9) | |
| Spikes, n (%) | 7 (18.4) | 6 (28.6) | 1 (5.9) | |
| Delta waves, n (%) | 21 (55.3) | 14 (66.7) | 7 (41.2) | |
| Near flat or flat, n (%) | 8 (21.1) | 0 (0) | 8 (47.1) | |
| Glasgow coma scale | 3 (3–4.5) | 3 (3–7.2) | 3 (3–4) | 0.428 |
| GOS-E Peds score | <0.001 | |||
| GOS-E Peds 1–3 | 6 (10.7%) | 6 (25.0) | 0 (0) | |
| GOS-E Peds 4–6 | 7 (12.5%) | 7 (29.1) | 0 (0) | |
| GOS-E Peds 7–8 | 43(76.7%) | 11 (45.8) | 32 (100) |
| Total (n = 56) | Survivors (n = 24) | Non Survivors (n = 32) | p Value | |
|---|---|---|---|---|
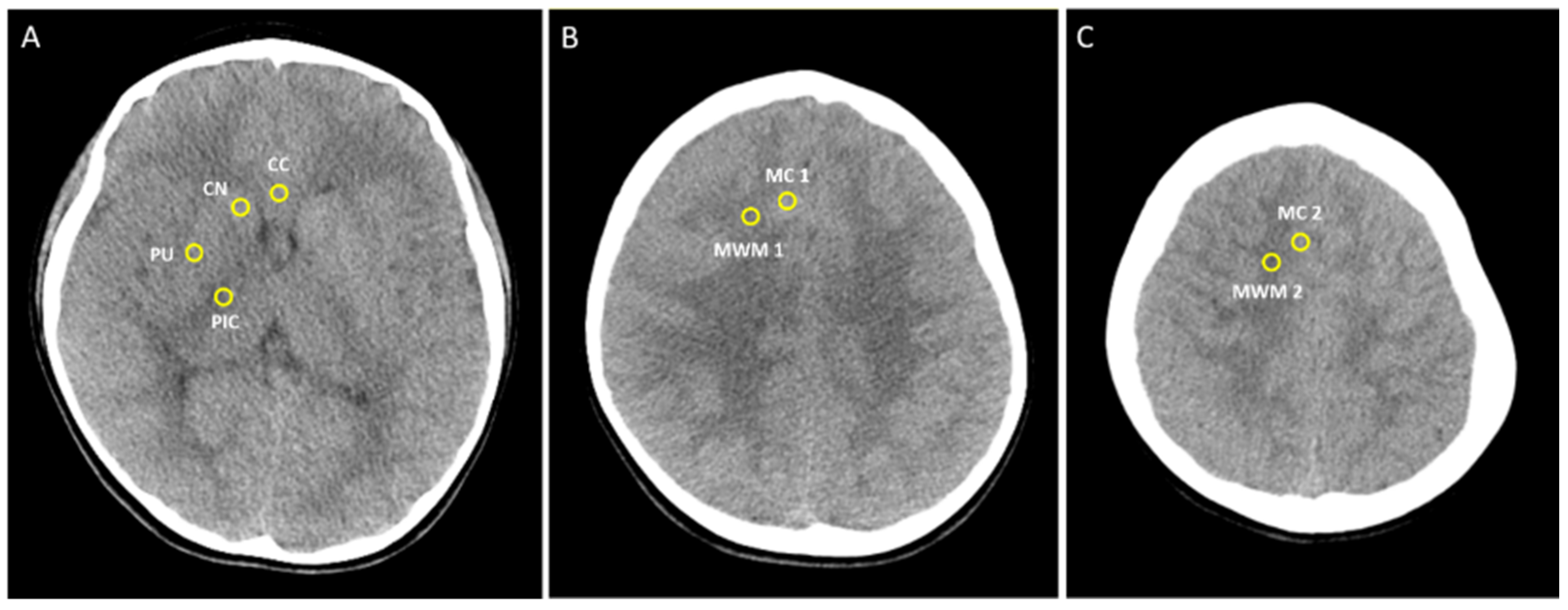
| Caudate nucleus | 32.0 (27.5–36.0) | 32.5 (27.5–36.5) | 28.5 (25.0–32.5) | 0.014 |
| Putamen | 31.0 (28.0–34.5) | 30.5 (27.5–34.5) | 30.0 (25.0–32.0) | 0.288 |
| Corpus callosum | 26.0 (23.5–31.0) | 27.5 (21.5–31.0) | 25.5 (23.0–28.5) | 0.652 |
| Post limb of internal capsule | 27.0 (24.0–30.0) | 27.5 (22.0–31.0) | 26.0 (24.5–29.0) | 0.535 |
| Medial cortex1 | 31.0 (26.2–34.0) | 32.0 (27.7–34.5) | 27.5 (25.0–31.0) | 0.004 |
| Medial white matter 1 | 25.0 (22.2–28.7) | 28.0 (24.0–30.0) | 23.0 (22.0–26.0) | 0.005 |
| Medial cortex2 | 32.0 (28.0–35.0) | 34.0 (28.7–35.0) | 29.5 (25.0–32.0) | 0.012 |
| Medial white matter 2 | 26.0 (23.0–28.0) | 27.0 (23.0–29.0) | 24.0 (23.0–27.0) | 0.104 |
| GWR in Basal ganglia | 1.19 (1.09–1.27) | 1.17 (1.09–1.21) | 1.12 (0.98–1.22) | 0.187 |
| GWR in cerebrum | 0.78 (0.70–0.85) | 0.74 (0.68–0.82) | 0.83 (0.75–0.91) | 0.026 |
| Average GWR | 1.18 (1.08–1.26) | 1.18 (1.13–1.22) | 1.10 (1.01–1.17) | 0.034 |
| Odds Ratio | 95% CI | p-Value | |
|---|---|---|---|
| Caudate nucleus | 1.11 | 0.85–1.44 | 0.415 |
| Medial cortex 1 | 0.80 | 0.67–0.95 | 0.011 |
| Medial white matter 1 | 0.68 | 0.41–1.13 | 0.138 |
| Medial cortex 2 | 1.04 | 0.72–1.52 | 0.805 |
| GWR in cerebrum | 3.35 | 0.00–35.4 | 0.774 |
| Average GWR | 0.00 | 0.00–0.53 | 0.032 |
| GOS 1–4 (n = 6) | GOS 5–8 (n = 50) | p-Value | |
|---|---|---|---|
| Caudate nucleus | 36.0 (31.0–37.0) | 30.0 (26.0–33.0) | 0.049 |
| Putamen | 33.5 (30.0–37.0) | 30.0 (26.0–32.0) | 0.177 |
| Corpus callosum | 31.0 (29.0–31.0) | 25.5 (23.0–29.0) | 0.114 |
| Post limb of internal capsule | 30.5 (26.0–31.0) | 26.0 (23.0–29.0) | 0.117 |
| Medial cortex1 | 33.5 (32.0–36.0) | 29.0 (25.0–32.0) | 0.013 |
| Medial white matter 1 | 29.0 (28.0–30.0) | 24.0 (22.0–27.0) | 0.009 |
| Medial cortex2 | 35.0 (35.0–36.0) | 30.0 (25.7–33.0) | 0.002 |
| Medial white matter 2 | 28.0 (27.0–29.0) | 24.0 (22.7–27.0) | 0.018 |
| GWR in Basal ganglia | 1.14 (1.10–1.20) | 1.13 (1.02–1.22) | 0.851 |
| GWR in cerebrum | 0.70 (0.68–0.75) | 0.80 (0.74–0.90) | 0.049 |
| Average GWR | 1.20 (1.17–1.22) | 1.13 (1.02–1.19) | 0.063 |
| Odds Ratio | 95% CI | p | |
|---|---|---|---|
| Cudate nucleus | 0.99 | 0.81–1.22 | 0.976 |
| Medial cortex 1 | 0.83 | 0.68–0.99 | 0.043 |
| Medial white matter 1 | 0.96 | 0.65–1.41 | 0.831 |
| Medial cortex 2 | 0.93 | 0.64–1.34 | 0.699 |
| Medial white matter 2 | 1.14 | 0.74–1.74 | 0.542 |
| GWR in cerebrum | 14.7 | 0.00–34.7 | 0.496 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.-Y.; Choi, I.; Lee, S.-J.; Jeong, I.-S.; Kim, Y.-O.; Woo, Y.-J.; Cho, H.-J. Clinical Significance of Gray to White Matter Ratio after Cardiopulmonary Resuscitation in Children. Children 2022, 9, 36. https://doi.org/10.3390/children9010036
Lee Y-Y, Choi I, Lee S-J, Jeong I-S, Kim Y-O, Woo Y-J, Cho H-J. Clinical Significance of Gray to White Matter Ratio after Cardiopulmonary Resuscitation in Children. Children. 2022; 9(1):36. https://doi.org/10.3390/children9010036
Chicago/Turabian StyleLee, Yun-Young, Insu Choi, Seung-Jae Lee, In-Seok Jeong, Young-Ok Kim, Young-Jong Woo, and Hwa-Jin Cho. 2022. "Clinical Significance of Gray to White Matter Ratio after Cardiopulmonary Resuscitation in Children" Children 9, no. 1: 36. https://doi.org/10.3390/children9010036
APA StyleLee, Y.-Y., Choi, I., Lee, S.-J., Jeong, I.-S., Kim, Y.-O., Woo, Y.-J., & Cho, H.-J. (2022). Clinical Significance of Gray to White Matter Ratio after Cardiopulmonary Resuscitation in Children. Children, 9(1), 36. https://doi.org/10.3390/children9010036






