Fully Immersive Virtual Reality Game-Based Training for an Adolescent with Spastic Diplegic Cerebral Palsy: A Case Report
Abstract
1. Introduction
2. Description of the Case
2.1. History and Systematic Review
2.2. Tests and Measures
2.2.1. Gross Motor Function Measure-88 (GMFM-88)
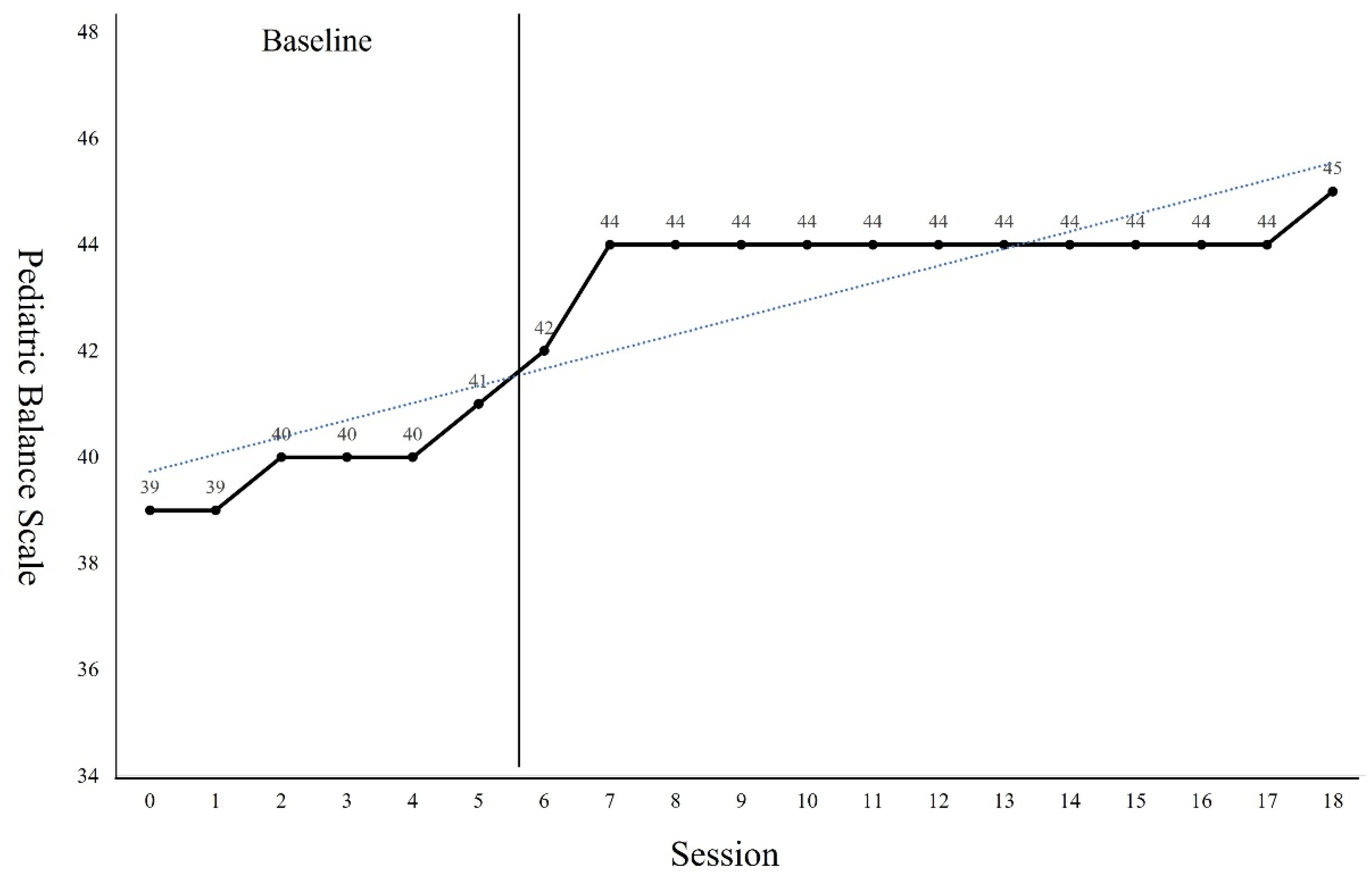
2.2.2. Pediatric Balance Scale (PBS)
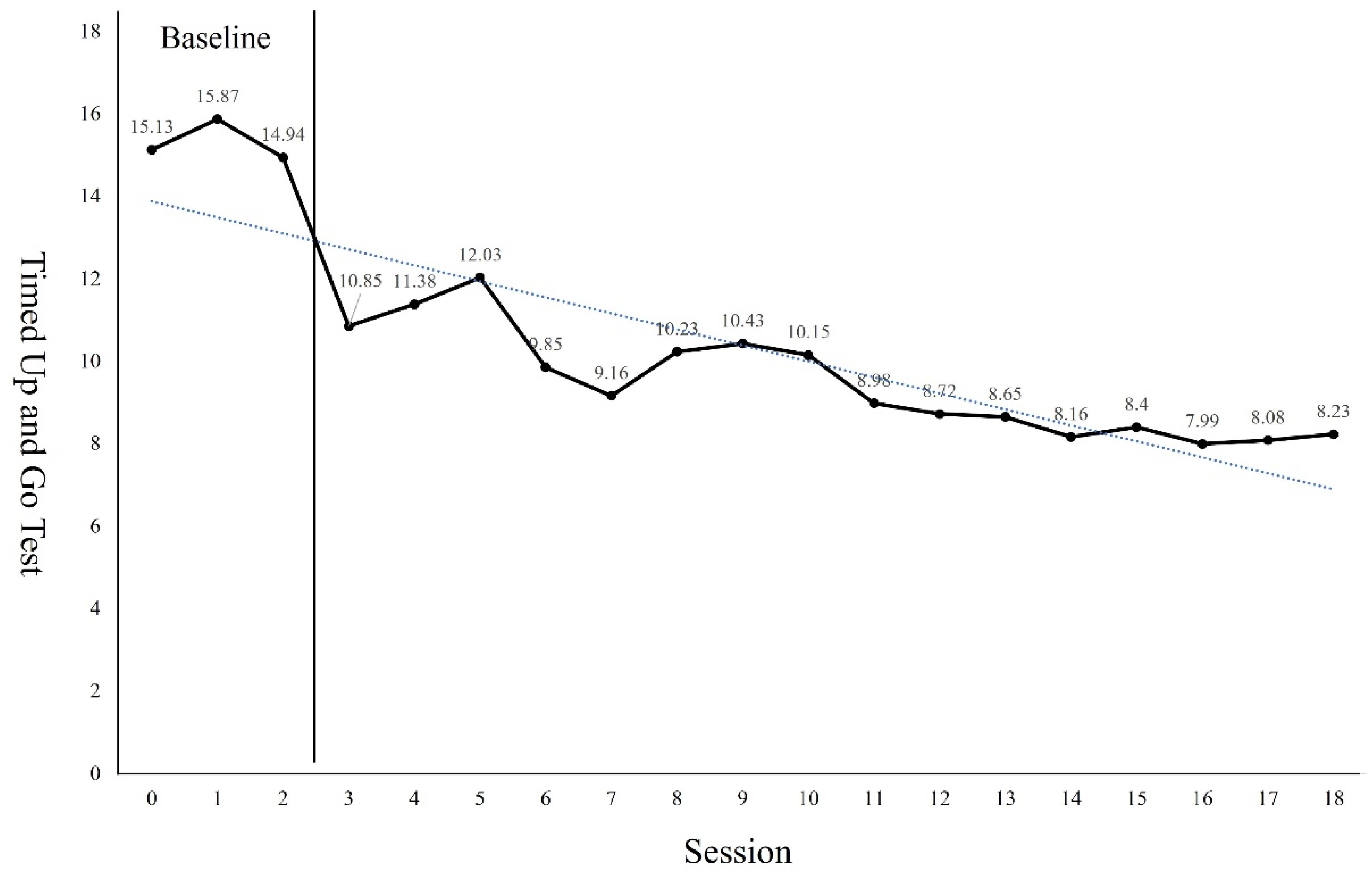
2.2.3. Timed up and Go Test (TUG)
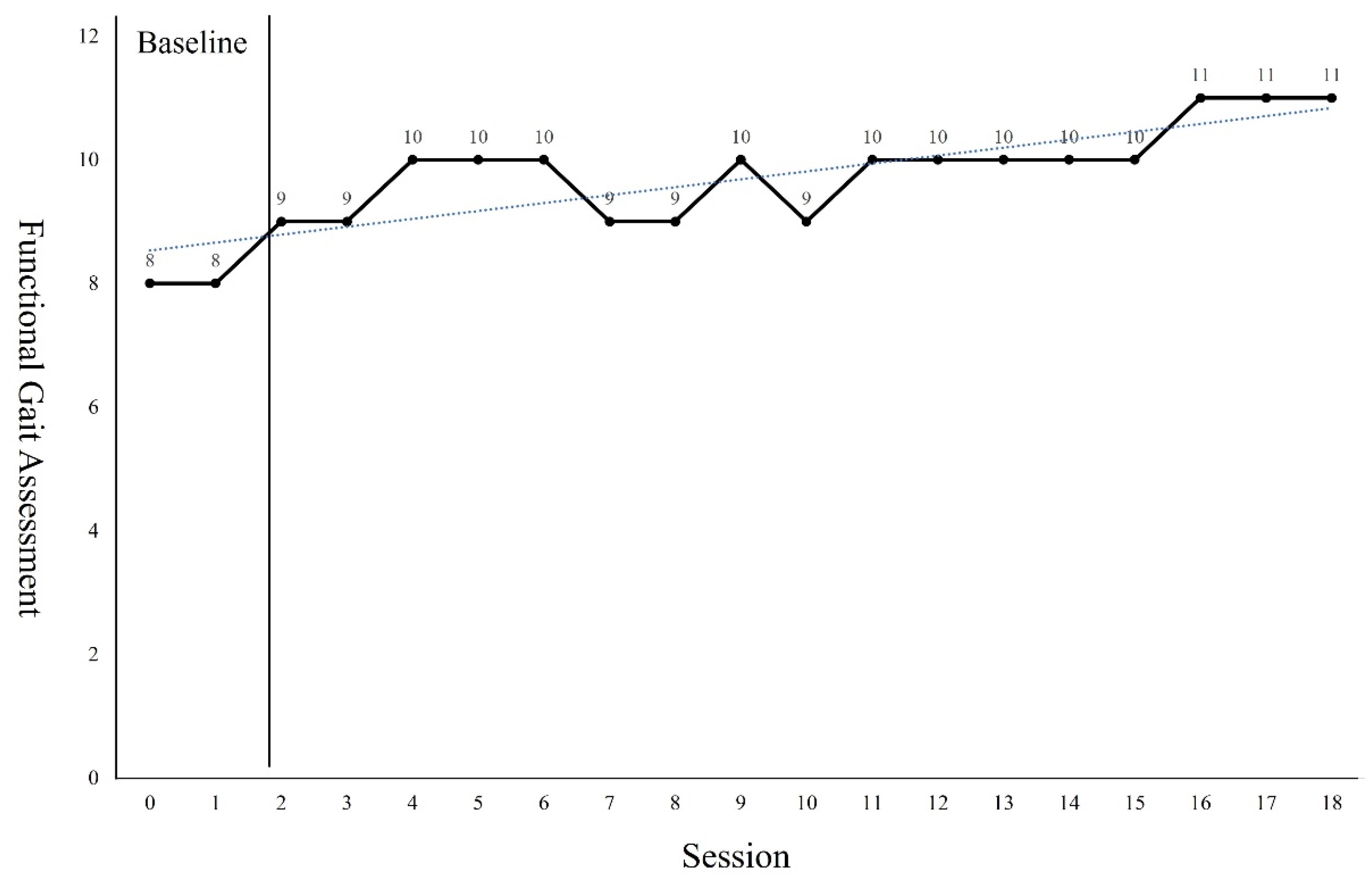
2.2.4. Functional Gait Assessment (FGA)
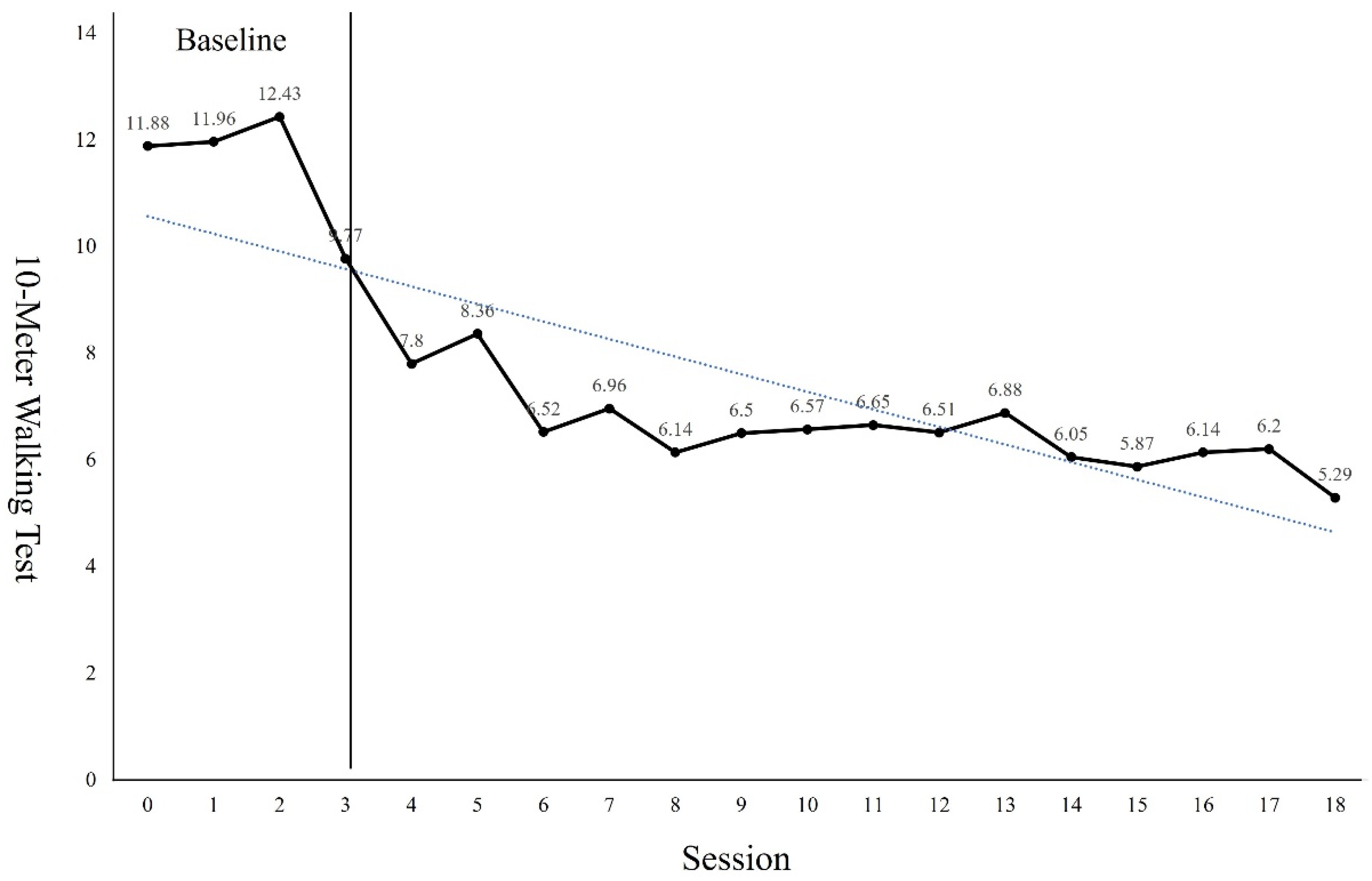
2.2.5. 10-Meter Walking Test (10MWT)
2.3. Clinical Impression
2.4. Intervention
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Cerebral palsy | CP |
| Virtual Reality | VR |
| virtual reality-based training | VR-based training |
| Gross Motor Function Measure-88 | GMFM-88 |
| Pediatric Balance Scale | PBS |
| Timed Up and Go | TUG |
| Functional Gait Assessment | FGA |
| 10-Meter Walking Test | 10MWT |
References
- Bax, M.; Goldstein, M.; Rosenbaum, P.; Leviton, A.; Paneth, N.; Dan, B.; Jacobsson, B.; Damiano, D. Proposed definition and classification of cerebral palsy, April 2005. Dev. Med. Child Neurol. 2005, 47, 571–576. [Google Scholar] [CrossRef] [PubMed]
- Jones, M.W.; Morgan, E.; Shelton, J.E.; Thorogood, C. Cerebral Palsy:Introduction and Diagnosis (Part I). J. Pediatr. Health Care. 2007, 21, 146–152. [Google Scholar] [CrossRef]
- Rosenbaum, P.A. Report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child Neurol. 2007, 49, 480. [Google Scholar] [CrossRef]
- Krigger, K.W. Cerebral palsy: An overview. Am. Fam. Physician. 2006, 73, 91–100. [Google Scholar] [PubMed]
- Woollacott, M.H.; Burtner, P.; Jensen, J. Development of postural response during standing in healthy children and children with spastic diplegia. Neurosci. Biobehavioral. Rev. 1998, 22, 583–589. [Google Scholar] [CrossRef]
- Scrutton, D.; Damiano, D.; Mayston, M. The Spectrum of Disorders Known as Cerebral Palsy: Management of the Motor Disorders of Children with Cerebral Palsy, 2nd ed.; Mac Keith Press: London, UK, 2004; ISBN 978-1-898-68332-2. [Google Scholar]
- Van der Linden, M.L.; Hazlewood, M.E.; Aitchison, A.M.; Hillman, S.J.; Robb, J.E. Electrical stimulation of gluteus maximus in children with cerebral palsy: Effects on gait characteristics and muscle strength. Dev. Med. Child Neurol. 2003, 45, 385–390. [Google Scholar] [CrossRef]
- Scheker, L.R.; Chesher, S.P.; Ramirez, S. Neuromuscular electrical stimulation and dynamic bracing as a treatment for upper extremity spasticity in children with cerebral palsy. Br. J. Hand Surg. 1999, 24, 226–232. [Google Scholar] [CrossRef]
- Yavuzer, G.; Senel, A.; Atay, M.B.; Stam, H.J. “Playstation eyetoy games” improve upper extremity-related motor functioning in subacute stroke: A randomized controlled clinical trial. Eur. J. Phys. Rehabil. Med. 2008, 44, 237–244. [Google Scholar]
- Ketelaar, M.; Vermeer, A.; Hart, H.; van Petegem-van Beek, E.; Helders, P.J.M. Effects of a functional therapy program on motor abilities of children with cerebral palsy. Phys. Ther. 2001, 81, 1534–1545. [Google Scholar] [CrossRef]
- Harris, K.; Reid, D. The influence of virtual reality play on children’s motivation. Can. J. Occup. Ther. 2005, 72, 21–29. [Google Scholar] [CrossRef]
- Burdea, G.C. Virtual rehabilitation-benefits and challenges. Methods Inf. Med. 2003, 42, 519–523. [Google Scholar] [PubMed]
- Flynn, S.; Palma, P.; Bender, A. Feasibility of using the Sony PlayStation 2 gaming platform for an individual poststroke: A case report. J. Neurol. Phys. Ther. 2007, 31, 180–189. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, A.A.; Buckwalter, J.G. Virtual reality and cognitive assessment and rehabilitation: The state of the art. Stud. Health Technol. Inform. 1997, 44, 123–145. [Google Scholar] [PubMed]
- Beier, K.P. Virtual Reality: A Short Introduction. Available online: http://www-vrl.umich.edu/intro/index.html (accessed on 20 February 2004).
- Weiss, P.L.; Rand, D.; Katz, N.; Kizony, R. Video capture virtual reality as a flexible and effective rehabilitation tool. J. NeuroEng. Rehabil. 2004, 1, 12. [Google Scholar] [CrossRef]
- Graf, D.L.; Pratt, L.V.; Hester, C.N.; Short, K.R. Playing active video games increases energy expenditure in children. Pediatrics. 2009, 124, 534–540. [Google Scholar] [CrossRef]
- Bartlett, D.J.; Palisano, R.J. Physical therapists’ perceptions of factors influencing the acquisition of motor abilities of children with cerebral palsy: Implications for clinical reasoning. Phys. Ther. 2002, 82, 237–248. [Google Scholar] [CrossRef]
- Law, M.; Darrah, J.; Pollock, N.; King, G.; Rosenbaum, P.; Russell, D.; Palisano, R.; Harris, S.; Armstrong, R.; Watt, J. Family—Centred functional therapy for children with cerebral palsy: An emerging practice model. Phys. Occup. Ther. Pediatr. 1998, 18, 83–102. [Google Scholar] [CrossRef]
- Cramer, S.C.; Sur, M.; Dobkin, B.H.; O’Brien, C.; Sanger, T.D.; Trojanowski, J.Q.; Rumsey, J.M.; Hicks, R.; Cameron, J.; Chen, D.; et al. Harnessing neuroplasticity for clinical applications. Brain. 2011, 134, 1591–1609. [Google Scholar] [CrossRef]
- Danzl, M.M.; Etter, N.M.; Andreatta, R.D.; Kitzman, P.H. Facilitating neurorehabilitation through principles of engagement. J. Allied Health. 2012, 41, 35–41. [Google Scholar]
- Chambers, R.A.; Taylor, J.R.; Potenza, M.N. Developmental neurocircuitry of motivation in adolescence: A critical period of addiction vulnerability. Am. J. Psychiatry. 2003, 160, 1041–1052. [Google Scholar] [CrossRef]
- Roettl, J.; Terlutter, R. The same video game in 2D, 3D or virtual reality–How does technology impact game evaluation and brand placements? PLoS ONE 2018, 13, 24. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Nahrstedt, K.; Cui, Y.; Yu, B.; Liang, J.; Jung, S.H.; Bajscy, R. TEEVE: The next generation architecture for tele-immersive environments. In Proceedings of the IEEE International Symposium on Multimedia (ISM), Irvine, CA, USA, 12–14 December 2005; pp. 112–119. [Google Scholar] [CrossRef]
- Bailenson, J.N.; Swinth, K.R.; Hoyt, C.L.; Persky, S.; Dimov, A.; Blascovich, J. The independent and interactive effects of embodied agent appearance and behaviour on self-report, cognitive, and behavioural markers of copresence in immersive virtual environments. PRESENCE Teleoperators Virtual Environ. 2005, 14, 379–393. [Google Scholar] [CrossRef]
- Mujber, T.S.; Szecsi, T.; Hashmi, M.S.J. Virtual reality applications in manufacturing process simulation. J. Mater. Process. Technol. 2004, 155–156, 1834–1838. [Google Scholar] [CrossRef]
- Bohannon, R.W.; Smith, M.B. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys. Ther. 1987, 67, 206–207. [Google Scholar] [CrossRef]
- Bottos, M.; Benedetti, M.G.; Salucci, P. Botilinum toxin with and without casting in ambulant children with spastic diplegia: A clinical and functional assessment. Dev. Med. Child Neurol. 2003, 45, 758–762. [Google Scholar] [CrossRef]
- Tieman, B.J.; Palisano, R.J.; Gracely, E.J. Gross motor capability and performance of mobility in children with cerebral palsy: A comparison across home, school, and outdoors/community settings. Phys. Ther. 2004, 84, 419–429. [Google Scholar] [CrossRef]
- Palisano, R.J.; Hanna, S.E.; Rosenbaum, P.L.; Russell, D.J.; Walter, S.D.; Wood, E.P.; Raina, P.S.; Galuppi, B.E. Validation of a model of gross motor function for children with cerebral palsy. Phys. Ther. 2000, 80, 974–985. [Google Scholar] [CrossRef]
- Nordmark, E.; Hagglund, G.; Jarnlo, G.B. Reliability of the gross motor function measure in cerebral palsy. Scand. J. Rehabil. Med. 1997, 29, 25–28. [Google Scholar]
- Franjoine, M.R.; Gunther, J.S.; Taylor, M.J. Pediatric balance scale: A modified version of the berg balance scale for the school-age child with mild to moderate motor impairment. Pediatr. Phys. Ther. 2003, 15, 114–128. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [CrossRef]
- Thieme, H.; Ritschel, C.; Zange, C. Reliability and validity of the functional gait assessment(German version) in subacute stroke patients. Arch. Phys. Med. Rehabil. 2009, 90, 1565–1570. [Google Scholar] [CrossRef] [PubMed]
- Salbach, N.M.; Mayo, N.E.; Higgins, J.; Ahmed, S.; Finch, L.E.; Richards, C.L. Responsiveness and predictability of gait speed and other disability measures in acute stroke. Arch. Phys. Med. Rehabil. 2001, 82, 1204–1212. [Google Scholar] [CrossRef]
- Pimentel, K.; Teixeira, K. Virtual Reality: Through the New Looking Glass; McGraw-Hill Inc.: New York, NY, USA, 1995; pp. 3–8, 41–202. [Google Scholar]
- Weiss, P.L.; Kizony, K.; Feintuch, U.; Katz, N. Virtual reality in neurorehabilitation. In Textbook of Neural Repair and Neurorehabilitation; Selzer, M.E., Cohen, L., Gage, F.H., Clarke, S., Duncan, P.W., Eds.; Cambridge University Press: Cambridge, UK, 2006. [Google Scholar]
- Fung, J.; Richards, C.L.; Malouin, F.; McFadyen, B.J.; Lamontagne, A. A treadmill and motion coupled virtual reality system for gait training post-stroke. Cyber Psychol. Behav. 2006, 9, 157–162. [Google Scholar] [CrossRef]
- Jaffe, D.L.; Brown, D.A.; Pierson-Carey, C.D.; Buckley, E.L.; Lew, H.L. Stepping over obstacles to improve walking in individuals with poststroke hemiplegia. J. Rehabil. Res. Dev. 2004, 41, 283–292. [Google Scholar] [CrossRef]
- Parijat, P.; Lockhart, T.E.; Liu, J. Effects of perturbation-based slip training using a virtual reality environment on slip-induced falls. Ann. Biomed. Eng. 2015, 43, 958–967. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Neira, C.; Sandin, D.J.; DeFanti, T.A. Surround screen projection-based virtual reality: The design and implementation of the CAVE. In Proceedings of the 20th Annual Conference on Computer Graphics and Interactive Techniques, Online, 1 September 1993; pp. 135–142. [Google Scholar] [CrossRef]
- Cruz-Neira, C.; Sandin, D.J.; DeFanti, T.A.; Kenyon, R.; Hart, J.C. The CAVE, Audio Visual Experience Automatic Virtual Environment. Commun. ACM 1992, 38, 64–72. [Google Scholar] [CrossRef]
- Kim, A.; Darakjian, N.; Finley, J.M. Walking in fully immersive virtual environments: An evaluation of potential adverse effects in older adults and individuals with Parkinson’s disease. J. NeuroEng. Rehabil. 2017, 14, 16. [Google Scholar] [CrossRef]
- Dewar, R.; Love, S.; Johnston, L.M. Exercise interventions improve postural control in children with cerebral palsy: A systematic review. Dev. Med. Child Neurol. 2015, 57, 504–520. [Google Scholar] [CrossRef]
- Tinderholt, M.H.; Ostensjo, S.; Larun, L.; Odgaard-Jensen, J.; Jahnsen, R. Intensive training of motor function and functional skills among young children with cerebral palsy: A systematic review and meta-analysis. BMC. Pediatr. 2014, 14, 292. [Google Scholar] [CrossRef]
- Page, S.J.; Levine, P.; Sisto, S.; Bond, Q.; Johnston, M.V. Stroke patients’ and therapists’ opinions of constraint-induced movement therapy. Clin. Rehabil. 2002, 16, 55–60. [Google Scholar] [CrossRef]
- Levin, M.F. Can virtual reality offer enriched environments for rehabilitation? Expert Rev. Neurother. 2011, 11, 153–155. [Google Scholar] [CrossRef] [PubMed]
- Deutsch, J.E.; Borbely, M.; Filler, J.; Huhn, K.; Guarrera-Bowlby, P. Use of a low-cost, commercially available gaming console (Wii) for rehabilitation of an adolescent with cerebral palsy. Phys. Ther. 2008, 88, 1196–1207. [Google Scholar] [CrossRef] [PubMed]
- Kiryu, T.; So, R.H. Sensation of presence and cybersickness in applications of virtual reality for advanced rehabilitation. J. NeuroEng. Rehabil. 2007, 4, 34. [Google Scholar] [CrossRef]
- Weech, S.; Kenny, S.; Barnett-Cowan, M. Presence and cybersickness in virtual reality are negatively related: A review. Front. Psychol. 2019, 10, 158. [Google Scholar] [CrossRef] [PubMed]
- Weech, S.; Varghese, J.P.; Barnett-Cowan, M. Estimating the sensorimotor components of cybersickness. J. Neurophysiol. 2018, 120, 2201–2217. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.H.; Seo, D.I.; Kim, H.T.; Yoo, B.H. An Integrated Model of Cybersickness: Understanding User’s Discomfort in Virtual Reality. J. KISE 2018, 45, 251–279. [Google Scholar] [CrossRef]
- Arnoni, J.L.B.; Pavao, S.L.; dos Santos Silva, F.P.; Rocha, N. Effects of virtual reality in body oscillation and motor performance of children with cerebral palsy: A preliminary randomized controlled clinical trial. Complement. Ther. Clin. Pract. 2019, 35, 189–194. [Google Scholar] [CrossRef]
- Okmen, B.M.; Aslan, M.D.; Nakipoglu, Y.G.F.; Ozgirgin, N. Effect of virtual reality therapy on functional development in children with cerebral palsy: A single-blind, prospective, randomized-controlled study. Turk. J. Phys. Med. Rehabil. 2019, 65, 371–378. [Google Scholar] [CrossRef]
- Ghai, S.; Ghai, I. Virtual reality enhances gait in cerebral palsy: A training dose-response meta-analysis. Front. Neurol. 2019, 10, 236. [Google Scholar] [CrossRef]
- Pourazar, M.; Bagherzadeh, F.; Mirakhori, F. Virtual reality training improves dynamic balance in children with cerebral palsy. Int. J. Dev. Disabil. 2019, 67, 429–434. [Google Scholar] [CrossRef]
- Park, S.H.; Son, S.M.; Choi, J.Y. Effect of posture control training using virtual reality program on sitting balance and trunk stability in children with cerebral palsy. NeuroRehabilitation 2021, 48, 247–254. [Google Scholar] [CrossRef]
- Mirelman, A.; Maidan, I.; Deutsch, J.E. Virtual reality and motor imagery: Promising tools for assessment and therapy in Parkinson’s disease. Mov. Disord. 2013, 28, 1597–1608. [Google Scholar] [CrossRef] [PubMed]
- Van Diest, M.; Lamoth, C.J.C.; Stegenga, J.; Verkerke, G.J.; Postema, K. Exergaming for balance training of elderly: State of the art and future developments. J. Neuroeng. Rehabil. 2013, 10, 101. [Google Scholar] [CrossRef] [PubMed]
- Lange, B.; Koenig, S.; Chang, C.; McConnell, E.; Suma, E.; Bolas, M.; Rizzo, A. Designing informed game-based rehabilitation tasks leveraging advances in virtual reality. Disabil. Rehabil. 2012, 34, 1863–1870. [Google Scholar] [CrossRef] [PubMed]
- Damiano, D.L. Activity, activity, activity: Rethinking our physical therapy approach to cerebral palsy. Phys. Ther. 2006, 86, 1534–1540. [Google Scholar] [CrossRef] [PubMed]
- Lang, C.E.; Macdonald, J.R.; Reisman, D.S. Observation of amounts of movement practice provided during stroke rehabilitation. Arch. Phys. Med. Rehabil. 2009, 90, 1692–1698. [Google Scholar] [CrossRef]
- Chen, Y.P.; Lee, S.Y.; Howard, A.M. Effect of virtual reality on upper extremity function in children with cerebral palsy: A meta-analysis. Pediatr. Phys. Ther. 2014, 26, 289–300. [Google Scholar] [CrossRef]


| Examination | Grade or Descriptions |
|---|---|
| Muscle tone by MAS | 0 to +1 |
| Motor function by GMFCS | Level II |
| LOM | Knee extension, Ankle dorsiflexion and inversion |
| Postures | Forward head posture in sitting and standing positions was unable to position her neck at midline had thoracic kyphosis, scapular protraction, and rounded shoulders; and experienced shoulder joint internal rotation. had difficulty in weight bearing and weight transfer left or right in a standing position Due to miserable malalignment syndrome, femoral excessive anteversion, genu valgum, tibial lateral torsion, subtalar joint hyperpronation, and pronated foot |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, K.; Oh, H.; Lee, G. Fully Immersive Virtual Reality Game-Based Training for an Adolescent with Spastic Diplegic Cerebral Palsy: A Case Report. Children 2022, 9, 1512. https://doi.org/10.3390/children9101512
Lee K, Oh H, Lee G. Fully Immersive Virtual Reality Game-Based Training for an Adolescent with Spastic Diplegic Cerebral Palsy: A Case Report. Children. 2022; 9(10):1512. https://doi.org/10.3390/children9101512
Chicago/Turabian StyleLee, Kyeongbong, HyeJin Oh, and GyuChang Lee. 2022. "Fully Immersive Virtual Reality Game-Based Training for an Adolescent with Spastic Diplegic Cerebral Palsy: A Case Report" Children 9, no. 10: 1512. https://doi.org/10.3390/children9101512
APA StyleLee, K., Oh, H., & Lee, G. (2022). Fully Immersive Virtual Reality Game-Based Training for an Adolescent with Spastic Diplegic Cerebral Palsy: A Case Report. Children, 9(10), 1512. https://doi.org/10.3390/children9101512







