A Randomised Crossover Trial of Behaviour Guidance Techniques on Children with Special Health Care Needs during Dental Treatment: The Physiological Variations
Abstract
:1. Introduction
2. Materials and Methods
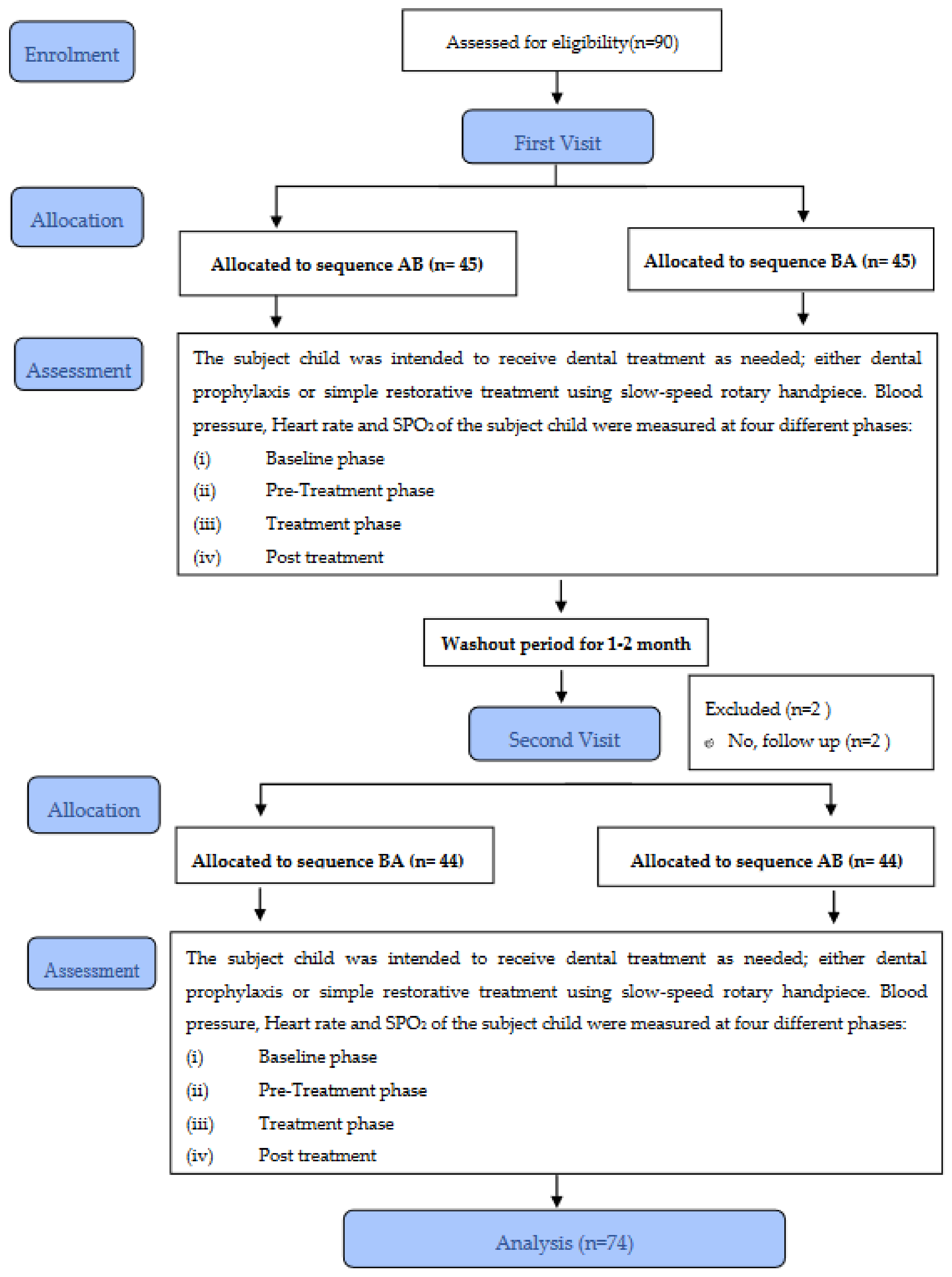
2.1. Study Design
2.2. Study Population
2.2.1. Inclusion Criteria
2.2.2. Exclusion Criteria
2.3. Study Visits and Procedures
Workflow for AB/BA Sequencing
2.4. Statistical Analysis
3. Results
3.1. Descriptive Analysis
3.2. Multivariate Analysis
3.2.1. Systolic Blood Pressure (SBP)
3.2.2. Diastolic Blood Pressure (DBP)
3.2.3. Heart Rate (HR)
3.2.4. Oxygen Saturation Level (SPO2)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pine, D.S.; Cohen, P.; Gurley, D.; Brook, J.; Ma, Y. The Risk for Early-Adulthood Anxiety and Depressive Disorders in Adolescents with Anxiety and Depressive Disorders. Arch. Gen. Psychiatry 1998, 55, 56–64. [Google Scholar] [CrossRef] [Green Version]
- Dharmani, C.K.K. Management of Children with Special Health Care Needs (SHCN) in The Dental Office. J. Med. Soc. 2018, 32, 1–6. [Google Scholar] [CrossRef]
- American Academy of Pediatric Dentistry. Behaviour Guidance for The Pediatric Dental Patient. In The Reference Manual of Pediatric Dentistry; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2021; pp. 306–324. [Google Scholar]
- Peretz, B.; Gluck, G.M. The Use of Restraint in The Treatment of Paediatric Dental Patients: Old and New Insights. Int. J. Paediatr. Dent. 2002, 12, 392–397. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatric Dentistry. Protective stabilization. In The Reference Manual of Pediatric Dentistry; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2021; pp. 325–331. [Google Scholar]
- De Jongh, A. Trauma-related Symptomatology in Dental Phobic Patient. J. Dent. Res. 2000, 79, 145. [Google Scholar]
- Tsuchihashi, N.; Uehara, N.; Takagi, Y.; Miwa, Z.; Sugimoto, K. Internal Stress in Children and Parental Attitude to Dental Treatment with Passive Restraint. Pediatr. Dent. J. 2012, 22, 170–177. [Google Scholar] [CrossRef]
- Chen, H.Y.; Yang, H.; Chi, H.J.; Chen, H.M. Physiologic and Behavioural Effects of Papoose Board on Anxiety in Dental Patients with Special Needs. J. Formos. Med. Assoc. 2014, 113, 94–101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shapiro, M.; Melmed, R.N.; Sgan-Cohen, H.D.; Eli, I.; Parush, S. Behavioural and Physiological Effect of Dental Environment Sensory Adaptation on Children’s Dental Anxiety. Eur. J. Oral Sci. 2007, 115, 479–483. [Google Scholar] [CrossRef] [PubMed]
- Sequeira, H.; Hot, P.; Silvert, L.; Delplanque, S. Electrical Autonomic Correlates of Emotion. Int. J. Psychophysiol. 2009, 71, 50–56. [Google Scholar] [CrossRef]
- Sharma, A.; Pant, R.; Priyadarshi, S.; Agarwal, N.; Tripathi, S.; Chaudhary, M. Cardiovascular Changes Due to Dental Anxiety During Local Anesthesia Injection for Extraction. J. Oral Maxillofac. Surg. 2019, 18, 80–87. [Google Scholar] [CrossRef]
- Kushki, A.; Drumm, E.; Pla Mobarak, M.; Tanel, N.; Dupuis, A.; Chau, T.; Anagnostou, E. Investigating the Autonomic Nervous System Response to Anxiety in Children with Autism Spectrum Disorders. PLoS ONE 2013, 8, e59730. [Google Scholar]
- Noteboom, J.T.; Barnholt, K.R.; Enoka, R.M. Activation of The Arousal Response and Impairment of Performance Increase with Anxiety and Stressor Intensity. J. Appl. Physiol. 2001, 91, 2093–2101. [Google Scholar] [CrossRef]
- Mokhtar, I.W.; Suhaimi, A.S.M.; Ahmad, M.S.; Baharuddin, I.H.; Andytan, N.I.I. The Papoose Board: Parents’ Perceptions and Attitudes of Its Usage in Their Child’s Dental Treatment. J. Dent. Indones. 2019, 26, 133–139. [Google Scholar]
- Hill, B.; Fadavi, S.; Le Hew, C.W.; Rada, R. Effect of Caregiver’s Race and Ethnicity on Acceptance of Passive Immobilization for Their Child’s Dental Treatment. J. Dent. Child. 2019, 86, 3–9. [Google Scholar]
- Kupietzky, A.; Ram, D. Effects of a positive verbal presentation on parental acceptance of passive medical stabilization for the dental treatment of young children. Pediatr. Dent. 2005, 27, 380–384. [Google Scholar]
- Aarvik, R.S.; Agdal, M.L.; Svendsen, E.J. Restraint in paediatric dentistry: A qualitative study to explore perspectives among public, non-specialist dentists in Norway. Acta Odontol. Scand. 2021, 79, 443–450. [Google Scholar] [CrossRef]
- Batista, K.B.D.S.L.; Thiruvenkatachari, B.; O’Brien, K. Intention-To-Treat Analysis: Are We Managing Dropouts and Missing Data Properly in Research on Orthodontic Treatment? A Systematic Review. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 19–27. [Google Scholar]
- Maenner, M.J.; Shaw, K.A.; Bakian, A.V.; Bilder, D.A.; Durkin, M.S.; Esler, A.; Furnier, S.M.; Hallas, L.; Hall-Lande, J.; Hudson, A.; et al. Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years—Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2018. MMWR Surveill. Summ. 2021, 70, 1–16. [Google Scholar] [CrossRef]
- Mackey, A.; Gass, S. Second Language Research: Methodology and Design, 2nd ed.; Routledge: New York, NY, USA, 2015; 452p. [Google Scholar] [CrossRef]
- Irving, C.A.; Chaudhari, M.P. Cardiovascular Abnormalities in Down’s Syndrome: Spectrum, Management and Survival Over 22 Years. Arch. Dis. Child. 2012, 97, 326–330. [Google Scholar] [CrossRef] [Green Version]
- Franchini, K.G.; Cowley, A.W., Jr. Autonomic Control of Cardiac Function. In Primer on The Autonomic Nervous System, 2nd ed.; Academic Press: Cambridge, MA, USA, 2011; pp. 134–138. [Google Scholar]
- Marshall, J.; Sheller, B.; Mancl, L.; Williams, B.J. Parental attitudes regarding behavior guidance of dental patients with autism. Pediatr. Dent. 2008, 30, 400–407. [Google Scholar]
- Lidstone, J.; Uljarević, M.; Sullivan, J.; Rodgers, J.; McConachie, H.; Freeston, M.; Le Couteur, A.; Prior, M.; Leekam, S. Relations Among Restricted and Repetitive Behaviors, Anxiety and Sensory Features in Children with Autism Spectrum Disorders. Res. Autism Spectr. Disord. 2014, 8, 82–92. [Google Scholar] [CrossRef]
- Eickmann, S.H.; Emond, A.M.; Lima, M. Evaluation of Child Development: Beyond the Neuromotor Aspect. J. Pediatr. 2016, 92 (Suppl. S1), 71–83. [Google Scholar] [CrossRef] [Green Version]
- Duric, N.S.; Assmus, J.; Gundersen, D.; Duric, G.A.; Elgen, I.B. Multimodal Treatment in Children and Adolescents with Attention-Deficit/Hyperactivity Disorder: A 6-Month Follow-up. Nord. J. Psychiatry 2017, 71, 386–394. [Google Scholar] [CrossRef] [Green Version]
- American Academy of Pediatric Dentistry. Management of dental patients with special health care needs. In The Reference Manual of Pediatric Dentistry; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2021; pp. 325–331. [Google Scholar]
- Nunn, J.; Foster, M.; Master, S.; Greening, S. British Society of Paediatric Dentistry: A Policy Document on Consent and The Use of Physical Intervention in The Dental Care of Children. Int. J. Pediatr. Dent. 2008, 18, 39–46. [Google Scholar] [CrossRef] [PubMed]
- Townsend, J.A. Protective stabilization in the dental setting. In Dental Care for Children with Special Health Care Needs; Nelson, T.M., Webb, J.R., Eds.; Springer: Cham, Switzerland, 2019; pp. 247–267. [Google Scholar]
- Hallonsten, A.L.; Jensen, B.; Raadal, M.; Veerkamp, J.; Hosey, M.; Poulsen, S. EAPD Guidelines on Sedation in Paediatric Dentistry. Eur. J. Paedtr. Dent. 2013, 7, 12. [Google Scholar]
- Al Zoubi, L.; Schmoeckel, J.; Mustafa, A.M.; Splieth, C.H. Parental Acceptance of Advanced Behaviour Management Techniques in Paediatric Dentistry in Families with Different Cultural Background. Eur. Arch. Paediatr. Dent. 2021, 22, 707–713. [Google Scholar] [CrossRef]





| Phase | Time of Measurement |
|---|---|
| Baseline | Subject child in the waiting room/surgery room sitting on chair |
| Pre-treatment | Subject child lying down on the dental chair and proposed BGT (Exposure A) or wrap in Papoose board (Exposure B) will be applied to subject child for 1–2 min. |
| Treatment | Chosen treatment either prophylaxis or caries excavation (using slow speed handpiece; inside the oral cavity for 1–2 min. |
| Post-treatment | Subject child remains lying on the dental chair without Exposure A or Exposure B which lasted 1–2 min. |
| MEAN (SD) | F TEST (DF) | PARTIAL ETA SQUARED (η2) | p-VALUE | |||||
|---|---|---|---|---|---|---|---|---|
| PAPOOSE BOARD | BASIC BGT | |||||||
| SYSTOLIC BLOOD PRESSURE (mmHg) | 0.34 (3144) * | 0.01 | 0.80 | |||||
| Baseline | 112.19 (18.95) | 116.05 (21.27) | ||||||
| Pre-operative | 117.39 (23.50) | 114.15 (18.95) | ||||||
| Intra-operative | 116.84 (21.14) | 112.23 (19.92) | ||||||
| Post-Operative | 114.08 (19.14) | 115.86 (19.42) | ||||||
| DIASTOLIC BLOOD PRESSURE (mmHg) | 1.17 (3144) * | 0.02 | 0.32 | |||||
| Baseline | 73.96 (15.94) | 78.15 (17.69) | ||||||
| Pre-operative | 81.28 (25.21) | 77.22 (16.64) | ||||||
| Intra-operative | 77.66 (18.273) | 75.45 (17.68) | ||||||
| Post-operative | 75.15 (15.56) | 77.99 (20.06) | ||||||
| HEART RATE (beat/min) | 1.93 (3144) * | 0.04 | 0.13 | |||||
| Baseline | 88.03 (14.51) | 85.78 (18.47) | ||||||
| Pre-operative | 88.07 (19.64) | 90.11 (18.09) | ||||||
| Intra-operative | 90.97 (20.50) | 90.97 (20.50) | ||||||
| Post-operative | 87.86 (17.20) | 88.52 (17.89) | ||||||
| OXYGEN SATURATION LEVEL (%) | 0.42 (3144) * | 0.01 | 0.74 | |||||
| Baseline | 97.72 (2.02) | 97.84 (2.20) | ||||||
| Pre-operative | 97.97 (2.13) | 97.76 (2.35) | ||||||
| Intra-operative | 97.69 (4.49) | 98.03 (1.86) | ||||||
| Post-operative | 97.81 (1.67) | 97.51 (3.84) | ||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ismail, N.; Isa, K.A.M.; Wan Mokhtar, I. A Randomised Crossover Trial of Behaviour Guidance Techniques on Children with Special Health Care Needs during Dental Treatment: The Physiological Variations. Children 2022, 9, 1526. https://doi.org/10.3390/children9101526
Ismail N, Isa KAM, Wan Mokhtar I. A Randomised Crossover Trial of Behaviour Guidance Techniques on Children with Special Health Care Needs during Dental Treatment: The Physiological Variations. Children. 2022; 9(10):1526. https://doi.org/10.3390/children9101526
Chicago/Turabian StyleIsmail, Norsaima, Khairil Anuar Md Isa, and Ilham Wan Mokhtar. 2022. "A Randomised Crossover Trial of Behaviour Guidance Techniques on Children with Special Health Care Needs during Dental Treatment: The Physiological Variations" Children 9, no. 10: 1526. https://doi.org/10.3390/children9101526
APA StyleIsmail, N., Isa, K. A. M., & Wan Mokhtar, I. (2022). A Randomised Crossover Trial of Behaviour Guidance Techniques on Children with Special Health Care Needs during Dental Treatment: The Physiological Variations. Children, 9(10), 1526. https://doi.org/10.3390/children9101526






