Relationship between Dental Occlusion and Maximum Tongue Pressure in Preschool Children Aged 4–6 Years
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethics Statement
2.2. Participants
2.3. Dental Occlusion Assessment
2.4. Maximum Tongue Pressure
2.5. Statistical Analysis
3. Results
3.1. Prevalence of Malocclusion
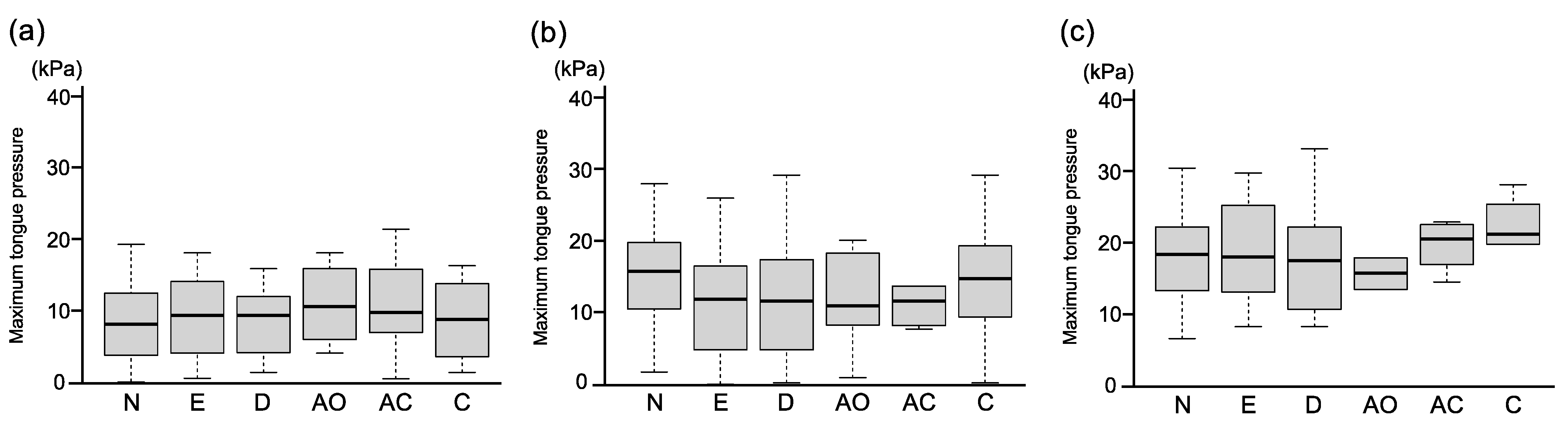
3.2. Maximum Tongue Pressure
3.3. 1-Year Follow-Up Study in the Same Children
4. Discussion
4.1. Prevalence of Malocclusion
4.2. Maximum Tongue Pressure
4.3. Maximum Tongue Pressure and Malocclusion
4.4. Development of Maximum Tongue Pressure
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Abreu, L.G. Orthodontics in Children and Impact of Malocclusion on Adolescents’ Quality of Life. Pediatr. Clin. N. Am. 2018, 65, 995–1006. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.; Liu, F.; Shen, S.; Shang, L.; Shang, L.; Wang, X. Prevalence of and factors affecting malocclusion in primary dentition among children in Xi’an, China. BMC Oral Health 2016, 16, 91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corruccini, R.S.; Townsend, G.C.; Richards, L.C.; Brown, T. Genetic and environmental determinants of dental occlusal variation in twins of different nationalities. Hum. Biol. 1990, 62, 353–367. [Google Scholar] [PubMed]
- Ovsenik, M. Incorrect orofacial functions until 5 years of age and their association with posterior crossbite. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 375–381. [Google Scholar] [CrossRef]
- Moimaz, S.A.S.; Garbin, A.; Ísper, J.; Lima, A.M.C.; Lolli, L.F.; Saliba, O.; Garbin, C. Longitudinal study of habits leading to malocclusion development in childhood. BMC Oral Health 2014, 14, 96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Onyeaso, C.O.; Isiekwe, M.C. Occlusal Changes from Primary to Mixed Dentitions in Nigerian Children. Angle Orthod. 2008, 78, 64–69. [Google Scholar] [CrossRef] [Green Version]
- Kluba, S.; Roßkopf, F.; Kraut, W.; Peters, J.P.; Calgeer, B.; Reinert, S.; Krimmel, M. Malocclusion in the primary dentition in children with and without deformational plagiocephaly. Clin. Oral Investig. 2016, 20, 2395–2401. [Google Scholar] [CrossRef]
- Góis, E.G.; Vale, M.P.; Paiva, S.M.; Abreu, M.H.; Serra-Negra, J.M.; Pordeus, I.A. Incidence of malocclusion between primary and mixed dentitions among Brazilian children: A 5-year longitudinal study. Angle Orthod. 2012, 82, 495–500. [Google Scholar] [CrossRef] [Green Version]
- Dimberg, L.; Lennartsson, B.; Söderfeldt, B.; Bondemark, L. Malocclusions in children at 3 and 7 years of age: A longitudinal study. Eur. J. Orthod. 2011, 35, 131–137. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, X.; Zhang, Y.; Wang, Y.; Zhang, H.; Chen, L.; Liu, Y. Prevalence of Malocclusion in 3- to 5-Year-Old Children in Shanghai, China. Int. J. Environ. Res. Public Health 2017, 14, 328. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shen, L.; He, F.; Zhang, C.; Jiang, H.; Wang, J. Prevalence of malocclusion in primary dentition in mainland China, 1988–2017: A systematic review and meta-analysis. Sci. Rep. 2018, 8, 4716. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marmaite, U.; Kasparaviciene, K.; Sidlauskas, A.; Zasciurinskiene, E.; Vasiliauskas, A.; Juodzbalys, G. The Prevalence of Malocclusion and Oral Habits among 5–7-Year-Old Children. Med. Sci. Monit. 2014, 20, 2036–2042. [Google Scholar] [CrossRef] [Green Version]
- Corrêa-Faria, P.; De Abreu, M.H.N.G.; Jordão, L.M.R.; Freire, M.D.C.M.; Costa, L.R. Association of breastfeeding and malocclusion in 5-year-old children: Multilevel approach. Int. J. Paediatr. Dent. 2018, 28, 602–607. [Google Scholar] [CrossRef]
- Grabowski, M.H.R.; Stahl, F.; Gaebel, M.; Kundt, G. Relationship between Occlusal Findings and Orofacial Myofunctional Status in Primary and Mixed Dentition. J. Orofac. Orthop. Fortschr. Kieferorthop. 2007, 68, 26–37. [Google Scholar] [CrossRef]
- Stahl, F.; Grabowski, R. Malocclusion and caries prevalence: Is there a connection in the primary and mixed dentitions? Clin. Oral Investig. 2003, 8, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Dimberg, L.; Bondemark, L.; Söderfeldt, B.; Lennartsson, B. Prevalence of malocclusion traits and sucking habits among 3-year-old children. Swed. Dent. J. 2010, 34, 35–42. [Google Scholar] [PubMed]
- Normando, T.S.; Barroso, R.F.F.; Normando, D. Influence of the socioeconomic status on the prevalence of malocclusion in the primary dentition. Dent. Press J. Orthod. 2015, 20, 74–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopes-Freire, G.M.; Cárdenas, A.B.C.; De Deza, J.E.E.S.; Ustrell-Torrent, J.M.; Oliveira, L.B.; Quesada, J.R.B. Exploring the association between feeding habits, non-nutritive sucking habits, and malocclusions in the deciduous dentition. Prog. Orthod. 2015, 16, 43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Knösel, M.; Nüser, C.; Jung, K.; Helms, H.-J.; Engelke, W.; Sandoval, P. Interaction between deglutition, tongue posture, and malocclusion: A comparison of intraoral compartment formation in subjects with neutral occlusion or different types of malocclusion. Angle Orthod. 2016, 86, 697–705. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Dyck, C.; Dekeyser, A.; Vantricht, E.; Manders, E.; Goeleven, A.; Fieuws, S.; Willems, G. The effect of orofacial myofunctional treatment in children with anterior open bite and tongue dysfunction: A pilot study. Eur. J. Orthod. 2016, 38, 227–234. [Google Scholar] [CrossRef] [Green Version]
- Stahl, F.; Grabowski, R. Orthodontic Findings in the Deciduous and Early Mixed Dentition—Inferences for a Preventive Strategy. J. Orofac. Orthop. Fortschr. Kieferorthop. 2003, 64, 401–416. [Google Scholar] [CrossRef]
- Proffit, W.R. Equilibrium theory revisited: Factors influencing position of the teeth. Angle Orthod. 1978, 48, 175–186. [Google Scholar] [PubMed]
- Straub, W.J. Malfunction of the tongue: Part II. The abnormal swallowing habit: Its causes, effects, and results in relation to orthodontic treatment and speech therapy. Am. J. Orthod. 1961, 47, 596–617. [Google Scholar] [CrossRef]
- Yashiro, K.; Takada, K. Tongue muscle activity after orthodontic treatment of anterior open bite: A case report. Am. J. Orthod. Dentofac. Orthop. 1999, 115, 660–666. [Google Scholar] [CrossRef]
- Fujiki, T.; Inoue, M.; Miyawaki, S.; Nagasaki, T.; Tanimoto, K.; Takano-Yamamoto, T. Relationship between maxillofacial morphology and deglutitive tongue movement in patients with anterior open bite. Am. J. Orthod. Dentofac. Orthop. 2004, 125, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Shaker, R.; Cook, I.J.S.; Dodds, W.J.; Hogan, W.J. Pressure-flow dynamics of the oral phase of swallowing. Dysphagia 1988, 3, 79–84. [Google Scholar] [CrossRef]
- Schwab, R.J.; Pasirstein, M.; Pierson, R.; Mackley, A.; Hachadoorian, R.; Arens, R.; Maislin, G.; Pack, A. Identification of Upper Airway Anatomic Risk Factors for Obstructive Sleep Apnea with Volumetric Magnetic Resonance Imaging. Am. J. Respir. Crit. Care Med. 2003, 168, 522–530. [Google Scholar] [CrossRef]
- Huang, Y.-S.; Guilleminault, C. Pediatric Obstructive Sleep Apnea and the Critical Role of Oral-Facial Growth: Evidences. Front. Neurol. 2013, 3, 184. [Google Scholar] [CrossRef] [Green Version]
- Potter, N.L.; Short, R. Maximal Tongue Strength in Typically Developing Children and Adolescents. Dysphagia 2009, 24, 391–397. [Google Scholar] [CrossRef]
- Ono, T.; Hori, K.; Nokubi, T. Pattern of Tongue Pressure on Hard Palate during Swallowing. Dysphagia 2004, 19, 259–264. [Google Scholar] [CrossRef]
- Ichikawa, M.; Fujita, Y.; Hamaguchi, A.; Chaweewannakorn, W.; Maki, K. Association of tongue pressure with masticatory performance and dental conditions in Japanese children. Pediatr. Dent. J. 2016, 26, 51–59. [Google Scholar] [CrossRef]
- Fujita, Y.; Ichikawa, M.; Hamaguchi, A.; Maki, K. Comparison of masticatory performance and tongue pressure between children and young adults. Clin. Exp. Dent. Res. 2018, 4, 52–58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Azevedo, N.D.; Lima, J.C.; Furlan, R.M.M.M.; Motta, A.R. Tongue pressure measurement in children with mouth-breathing behaviour. J. Oral Rehabil. 2018, 45, 612–617. [Google Scholar] [CrossRef] [PubMed]
- Utanohara, Y.; Hayashi, R.; Yoshikawa, M.; Yoshida, M.; Tsuga, K.; Akagawa, Y. Standard Values of Maximum Tongue Pressure Taken Using Newly Developed Disposable Tongue Pressure Measurement Device. Dysphagia 2008, 23, 286–290. [Google Scholar] [CrossRef]
- Potter, N.L.; Kent, R.D.; Lazarus, J.-A.C. Oral and Manual Force Control in Preschool-Aged Children: Is There Evidence for Common Control? J. Mot. Behav. 2009, 41, 66–82. [Google Scholar] [CrossRef]
- Asami, T.; Ishizaki, A.; Ogawa, A.; Kwon, H.; Kasama, K.; Tanaka, A.; Hironaka, S. Analysis of factors related to tongue pressure during childhood. Dent. Oral Craniofac. Res. 2017, 3, 1–7. [Google Scholar] [CrossRef]
- Kurabeishi, H.; Tatsuo, R.; Makoto, N.; Kazunori, F. Relationship between tongue pressure and maxillofacial morphology in Japanese children based on skeletal classification. J. Oral Rehabil. 2018, 45, 684–691. [Google Scholar] [CrossRef] [PubMed]
- Hegde, S.; Panwar, S.; Bolar, D.R.; Sanghavi, M.B. Characteristics of occlusion in primary dentition of preschool children of Udaipur, India. Eur. J. Dent. 2012, 6, 051–055. [Google Scholar] [CrossRef] [Green Version]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Tallgren, A.; Solow, B. Long-term changes in hyoid bone position and craniocervical posture in complete denture wearers. Acta Odontol. Scand. 1984, 42, 257–267. [Google Scholar] [CrossRef]
- Pae, E.-K.; Lowe, A.A.; Sasaki, K.; Price, C.; Tsuchiya, M.; Fleetham, J.A. A cephalometric and electromyographic study of upper airway structures in the upright and supine positions. Am. J. Orthod. Dentofac. Orthop. 1994, 106, 52–59. [Google Scholar] [CrossRef]
- Takahashi, S.; Ono, T.; Ishiwata, Y.; Kuroda, T. Effect of changes in the breathing mode and body position on tongue pressure with respiratory-related oscillations. Am. J. Orthod. Dentofac. Orthop. 1999, 115, 239–246. [Google Scholar] [CrossRef]
- Christensen, M.S.; Hanson, M.L. An Investigation of the Efficacy of Oral Myofunctional Therapy as a Precursor to Articulation Therapy for Pre-First Grade Children. J. Speech Hear. Disord. 1981, 46, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Melsen, B.; Attina, L.; Santuari, M.; Attina, A. Relationships between swallowing pattern, mode of respiration, and development of malocclusion. Angle Orthod. 1987, 57, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Mew, J. Infantile swallowing. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 298–299. [Google Scholar] [CrossRef] [PubMed]
- Tsuga, K.; Yoshikawa, M.; Oue, H.; Okazaki, Y.; Tsuchioka, H.; Maruyama, M.; Yoshida, M.; Akagawa, Y. Maximal voluntary tongue pressure is decreased in Japanese frail elderly persons. Gerodontology 2012, 29, e1078–e1085. [Google Scholar] [CrossRef]
- Yamaoka, M.; Furusawa, K.; Uematsu, T.; Okafuji, N.; Kayamoto, D.; Kurihara, S. Relationship of the hyoid bone and posterior surface of the tongue in prognathism and micrognathia. J. Oral Rehabil. 2003, 30, 914–920. [Google Scholar] [CrossRef]
- Urzal, V.; Braga, A.C.; Ferreira, A.P. Hyoid bone position and vertical skeletal pattern-open bite/deep bite. Oral Health Dent. Manag. 2014, 13, 341–347. [Google Scholar]
- Peltomäki, T. The effect of mode of breathing on craniofacial growth—Revisited. Eur. J. Orthod. 2007, 29, 426–429. [Google Scholar] [CrossRef] [Green Version]
- Liégeois, F.; Albert, A.; Limme, M. Comparison between tongue volume from magnetic resonance images and tongue area from profile cephalograms. Eur. J. Orthod. 2010, 32, 381–386. [Google Scholar] [CrossRef] [Green Version]

| Occlusal Traits | 4 Years Old | 5 Years Old | 6 Years Old | Total |
|---|---|---|---|---|
| (n = 160) | (n = 217) | (n = 100) | (n = 477) | |
| Sagittal relationship | 28.8% | 23.0% | 36.0% | 27.6% |
| Anterior crossbite | 9.4% | 6.9% | 7.0% | 7.7% |
| (mild/moderate) | (1.9%/7.5%) | (2.8%/4.1%) | (2.0%/5.0%) | (2.3%/5.5%) |
| Excessive overjet | 19.4% | 16.1% | 29.0% | 19.9% |
| Vertical relationship | 26.9% | 28.1% | 28.0% | 27.7% |
| Deep overbite | 18.1% | 22.1% | 18.0% | 19.9% |
| Anterior open bite | 8.8% | 6.0% | 10.0% | 7.8% |
| Transversal relationship | 0% | 0% | 0% | 0% |
| Posterior crossbite | 0% | 0% | 0% | 0% |
| Scissors bite | 0% | 0% | 0% | 0% |
| Space discrepancies | ||||
| Crowding | 10.0% | 12.4% | 9.0% | 10.9% |
| Age | 4 Years Old | 5 Years Old | 6 Years Old | |||
|---|---|---|---|---|---|---|
| (n = 155) | (n = 213) | (n = 100) | ||||
| Maximum tongue pressure (kPa) | 9.39 ± 5.42 | 14.18 ± 7.44 a | 18.37 ± 6.67 a,b | |||
| Dental occlusion | Normal | Malocclusion | Normal | Malocclusion | Normal | Malocclusion |
| (n = 74) | (n = 81) | (n = 103) | (n = 110) | (n = 42) | (n = 58) | |
| Maximum tongue pressure (kPa) | 8.77 ± 5.65 | 9.96 ± 5.17 | 15.62 ± 7.27 | 12.86 ± 7.41 c | 17.82 ± 6.49 | 18.72 ± 6.89 |
| Sex | Boys | Girls | Boys | Girls | Boys | Girls |
| (n = 81) | (n = 74) | (n = 104) | (n = 109) | (n = 59) | (n = 41) | |
| Maximum tongue pressure (kPa) | 10.16 ± 5.67 | 8.55 ± 5.04 | 14.47 ± 7.65 | 13.90 ± 7.28 | 18.89 ± 7.19 | 17.63 ± 5.85 |
| Degree of Freedom | F Value | p Value | |
|---|---|---|---|
| Sex | 1 | 3.203 | 0.074 |
| Occlusion | 1 | 2.925 | 0.088 |
| Age | 1 | 39.834 | <0.001 |
| Sex: Occlusion | 1 | 3.354 | 0.068 |
| Sex: Age | 1 | 2.939 | 0.087 |
| Occlusion: Age | 1 | 3.649 | 0.057 |
| Sex: Occlusion: Age | 1 | 3.837 | 0.051 |
| Residuals | 460 |
| Number | Age (Y) | Boy (%) | Maximum Tongue Pressure (kPa) | Increase Amount | Increase Rate | ||
|---|---|---|---|---|---|---|---|
| Before | After | (kPa) | (%) | ||||
| Normal | 35 | 4.7 ± 0.3 | 51.4% | 8.47 ± 6.05 | 16.01 ± 6.41 | 7.54 ± 5.05 | 89.0 |
| Malocclusion | 37 | 4.7 ± 0.3 | 51.4% | 9.33 ± 5.97 | 13.32 ± 6.44 | 3.99 ± 6.67 | 42.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sasaki, Y.; Otsugu, M.; Sasaki, H.; Fujikawa, N.; Okawa, R.; Kato, T.; Nakano, K. Relationship between Dental Occlusion and Maximum Tongue Pressure in Preschool Children Aged 4–6 Years. Children 2022, 9, 141. https://doi.org/10.3390/children9020141
Sasaki Y, Otsugu M, Sasaki H, Fujikawa N, Okawa R, Kato T, Nakano K. Relationship between Dental Occlusion and Maximum Tongue Pressure in Preschool Children Aged 4–6 Years. Children. 2022; 9(2):141. https://doi.org/10.3390/children9020141
Chicago/Turabian StyleSasaki, Yumi, Masatoshi Otsugu, Hidekazu Sasaki, Naho Fujikawa, Rena Okawa, Takafumi Kato, and Kazuhiko Nakano. 2022. "Relationship between Dental Occlusion and Maximum Tongue Pressure in Preschool Children Aged 4–6 Years" Children 9, no. 2: 141. https://doi.org/10.3390/children9020141






