Sleep Power Topography in Children with Attention Deficit Hyperactivity Disorder (ADHD)
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.1.1. Patient Group
2.1.2. Control Group
2.2. Sleep Recordings
2.3. EEG Signal Power in NREM Sleep, in REM Sleep and Wake before Sleep Onset
2.4. NREM Sleep Homeostatic Regulation
2.5. Correlations between Power and Clinical Variables
2.6. Statistical Analysis
3. Results
3.1. EEG Signal Power in NREM Sleep, REM Sleep and Wake before Sleep Onset
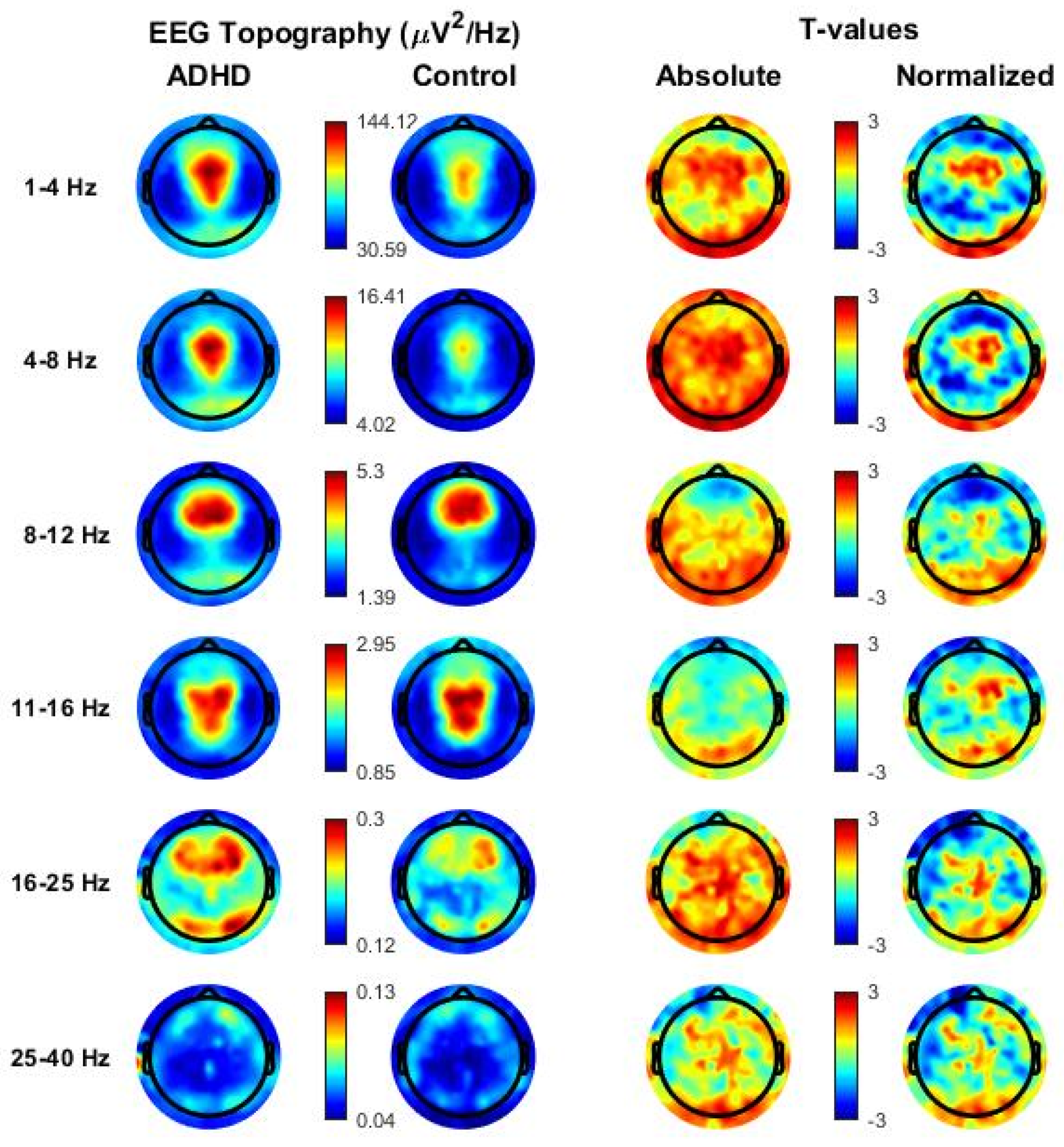
3.1.1. NREM Sleep
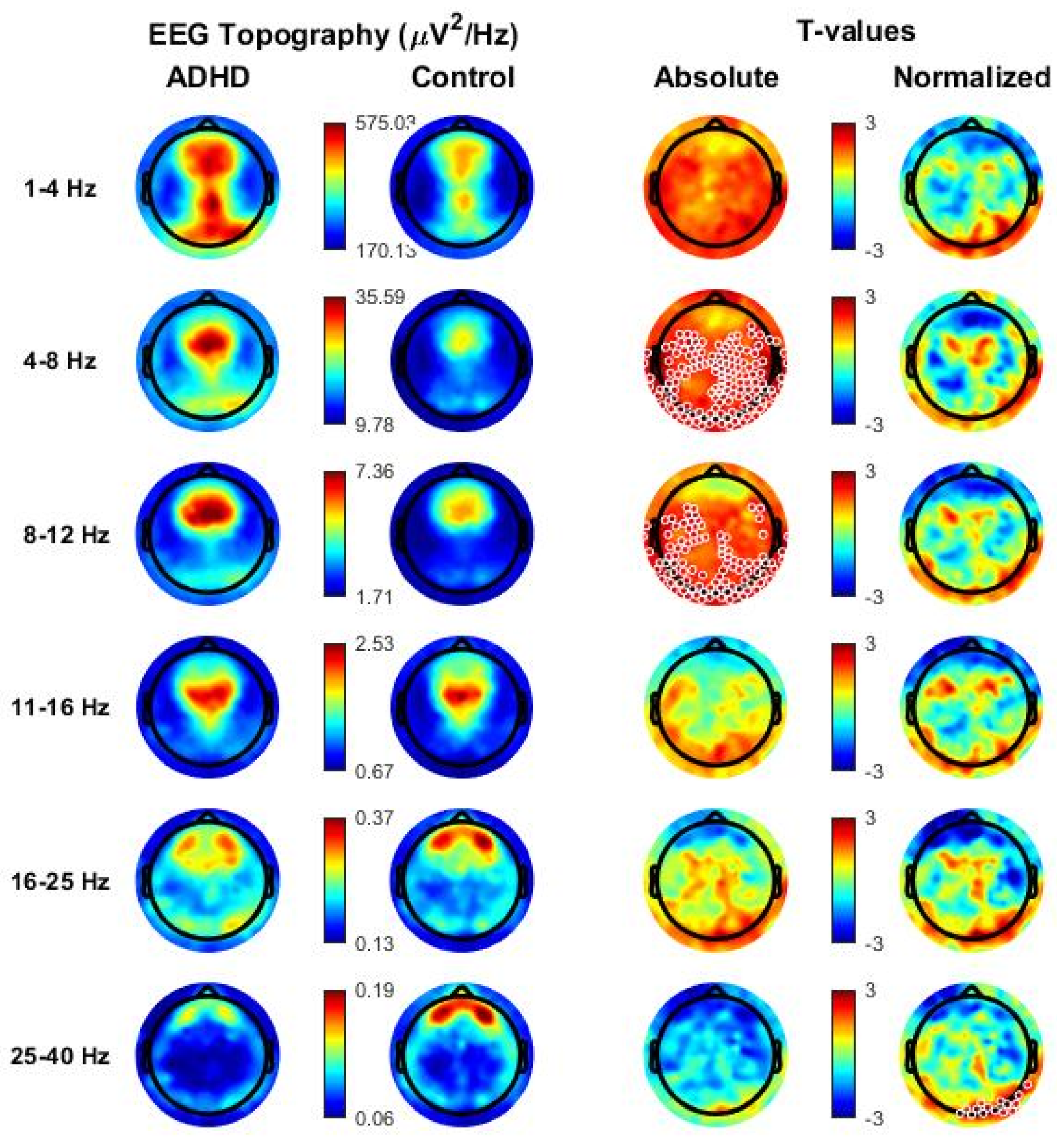
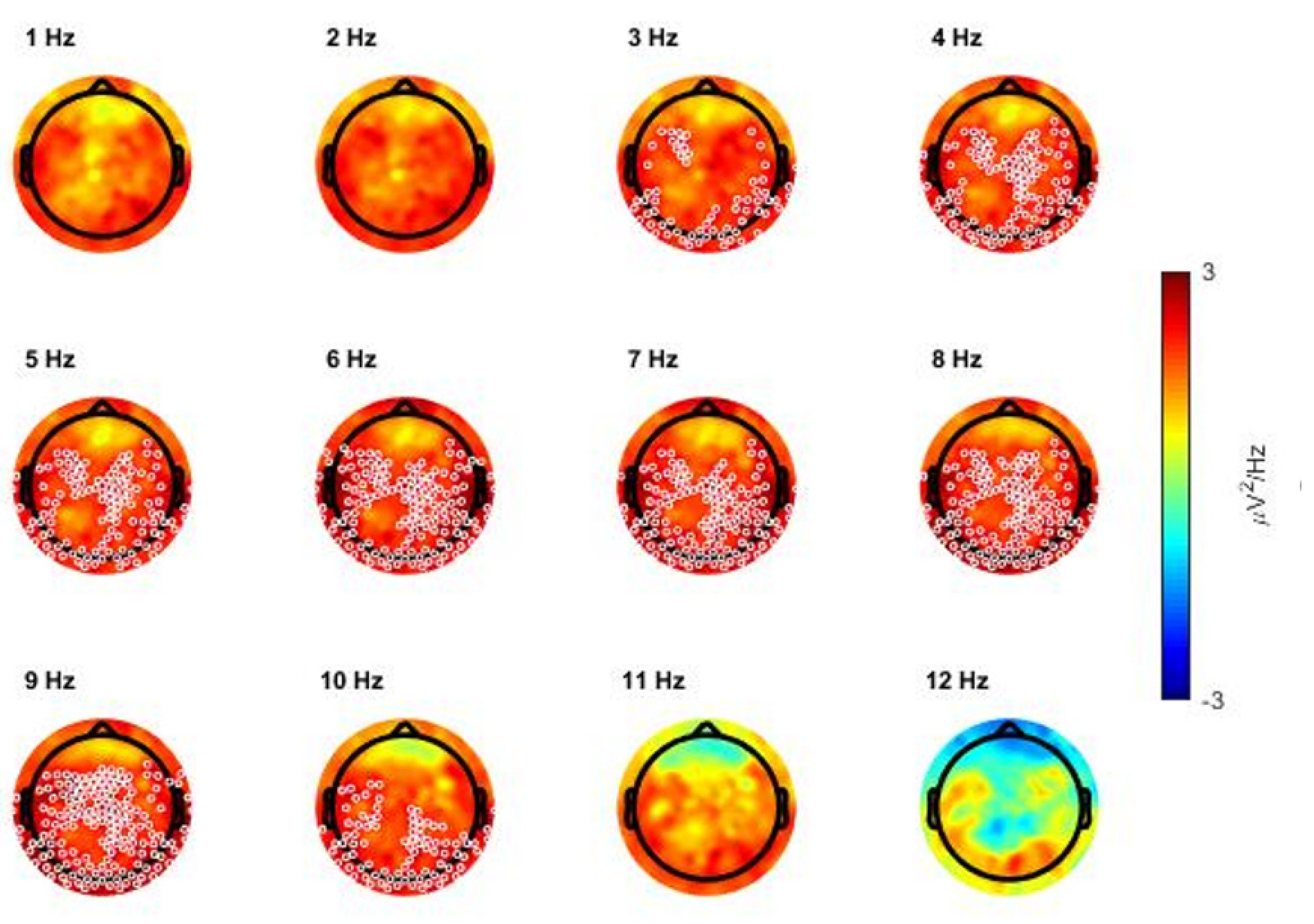
3.1.2. REM Sleep Power
3.1.3. Wake before Sleep Onset Power
3.2. NREM Sleep Homeostatic Regulation
3.3. Correlation Analysis between Low-Frequency Activity and Clinical Variables
4. Discussion
4.1. General Overview
4.2. Interpretation of Results
4.3. Limitations and Future Perspectives
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cabral, M.D.I.; Liu, S.; Soares, N. Attention-Deficit/Hyperactivity Disorder: Diagnostic Criteria, Epidemiology, Risk Factors and Evaluation in Youth. Transl. Pediatrics 2020, 9 (Suppl. 1), S104–S113. [Google Scholar] [CrossRef] [PubMed]
- Doshi, J.A.; Hodgkins, P.; Kahle, J.; Sikirica, V.; Cangelosi, M.J.; Setyawan, J.; Erder, M.H.; Neumann, P.J. Economic Impact of Childhood and Adult Attention-Deficit/Hyperactivity Disorder in the United States. J. Am. Acad. Child Adolesc. Psychiatry 2012, 51, 990–1002.e2. [Google Scholar] [CrossRef] [PubMed]
- Faraone, V.S.; Asherson, P.; Banaschewski, T.; Biederman, J.; Buitelaar, J.K.; Ramos-Quiroga, J.A.; Rohde, L.A.; Sonuga-Barke, E.J.S.S.; Tannock, R.; Franke, B. Attention-Deficit/Hyperactivity Disorder. Nat. Rev. Dis. Primers 2015, 1, 15020. [Google Scholar] [CrossRef] [PubMed]
- Steinhausen, H.-C.; Metzke, C.W.; Meier, M.; Kannenberg, R. Prevalence of Child and Adolescent Psychiatric Disorders: The Zürich Epidemiological Study. Acta Psychiatr. Scand. 1998, 98, 262–271. [Google Scholar] [CrossRef] [PubMed]
- Polanczyk, G.; de Lima, M.S.; Horta, B.L.; Biederman, J.; Rohde, L.A. The Worldwide Prevalence of ADHD: A Systematic Review and Metaregression Analysis. Am. J. Psychiatry 2007, 164, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Couture, J. A Review of the Pathophysiology, Etiology, and Treatment of Attention-Deficit Hyperactivity Disorder (ADHD). Ann. Pharmacother. 2014, 48, 209–225. [Google Scholar] [CrossRef]
- Wajszilber, D.; Santiseban, J.A.; Gruber, R. Sleep Disorders in Patients with ADHD: Impact and Management Challenges. Nat. Sci. Sleep 2018, 10, 453–480. [Google Scholar] [CrossRef] [Green Version]
- Baddam, S.K.R.; Canapari, C.A.; van Noordt, S.J.R.; Crowley, M.J. Sleep Disturbances in Child and Adolescent Mental Health Disorders: A Review of the Variability of Objective Sleep Markers. Med. Sci. 2018, 6, 46. [Google Scholar] [CrossRef] [Green Version]
- Gorgoni, M.; Scarpelli, S.; Reda, F.; De Gennaro, L. Sleep EEG Oscillations in Neurodevelopmental Disorders without Intellectual Disabilities. Sleep Med. Rev. 2020, 49, 101224. [Google Scholar] [CrossRef]
- Miano, S.; Castelnovo, A.; Bruni, O.; Manconi, M. Sleep Microstructure in Attention Deficit Hyperactivity Disorder According to the Underlying Sleep Phenotypes. J. Sleep Res. 2021, 31, e13426. [Google Scholar] [CrossRef]
- Biancardi, C.; Sesso, G.; Masi, G.; Faraguna, U.; Sicca, F. Sleep EEG Microstructure in Children and Adolescents with Attention Deficit Hyperactivity Disorder: A Systematic Review and Meta-Analysis. Sleep 2021, 44, zsab006. [Google Scholar] [CrossRef] [PubMed]
- Prehn-Kristensen, A.; Göder, R.; Fischer, J.; Wilhelm, I.; Seeck-Hirschner, M.; Aldenhoff, J.; Baving, L. Reduced Sleep-Associated Consolidation of Declarative Memory in Attention-Deficit/Hyperactivity Disorder. Sleep Med. 2011, 12, 672–679. [Google Scholar] [CrossRef] [PubMed]
- Prehn-Kristensen, A.; Munz, M.; Molzow, I.; Wilhelm, I.; Wiesner, C.D.; Baving, L. Sleep Promotes Consolidation of Emotional Memory in Healthy Children but Not in Children with Attention-Deficit Hyperactivity Disorder. PLoS ONE 2013, 8, e65098. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saletin, J.M.; Coon, W.G.; Carskadon, M.A. Stage 2 Sleep EEG Sigma Activity and Motor Learning in Childhood ADHD: A Pilot Study. J. Clin. Child Adolesc. Psychol. 2017, 46, 188–197. [Google Scholar] [CrossRef] [Green Version]
- Cremone, A.; Lugo-Candelas, C.I.; Harvey, E.A.; McDermott, J.M.; Spencer, R.M.C.C. REM Theta Activity Enhances Inhibitory Control in Typically Developing Children but Not Children with ADHD Symptoms. Exp. Brain Res. 2017, 235, 1491–1500. [Google Scholar] [CrossRef] [Green Version]
- Ringli, M.; Souissi, S.; Kurth, S.; Brandeis, D.; Jenni, O.G.; Huber, R. Topography of Sleep Slow Wave Activity in Children with Attention-Deficit/Hyperactivity Disorder. Cortex 2013, 49, 340–347. [Google Scholar] [CrossRef]
- Miano, S.; Amato, N.; Garbazza, C.; Abbafati, M.; Foderaro, G.; Pezzoli, V.; Ramelli, G.P.; Manconi, M.; Giuseppe, F.; Valdo, P. Shooting a High-Density Electroencephalographic Picture on Sleep in Children with Attention-Deficit/Hyperactivity Disorder. Sleep 2019, 42, zsz167. [Google Scholar] [CrossRef]
- Furrer, M.; Jaramillo, V.; Volk, C.; Ringli, M.; Aellen, R.; Wehrle, F.M.; Pugin, F.; Kurth, S.; Brandeis, D.; Schmid, M.; et al. Sleep EEG Slow-Wave Activity in Medicated and Unmedicated Children and Adolescents with Attention-Deficit/Hyperactivity Disorder. Transl. Psychiatry 2019, 9, 324. [Google Scholar] [CrossRef] [Green Version]
- Kurth, S.; Ringli, M.; Geiger, A.; LeBourgeois, M.; Jenni, O.G.; Huber, R. Mapping of Cortical Activity in the First Two Decades of Life: A High-Density Sleep Electroencephalogram Study. J. Neurosci. 2010, 30, 13211–13219. [Google Scholar] [CrossRef] [Green Version]
- Miano, S.; Amato, N.; Foderaro, G.; Pezzoli, V.; Ramelli, G.P.; Toffolet, L.; Manconi, M. Sleep Phenotypes in Attention Deficit Hyperactivity Disorder. Sleep Med. 2019, 60, 123–131. [Google Scholar] [CrossRef]
- Bioulac, S.; Taillard, J.; Philip, P.; Sagaspe, P. Excessive Daytime Sleepiness Measurements in Children With Attention Deficit Hyperactivity Disorder. Front. Psychiatry 2020, 11, 3. [Google Scholar] [CrossRef] [PubMed]
- Scott, N.; Blair, P.S.; Emond, A.M.; Fleming, P.J.; Humphreys, J.S.; Henderson, J.; Gringras, P. Sleep Patterns in Children with ADHD: A Population-Based Cohort Study from Birth to 11 Years. J. Sleep Res. 2013, 22, 121–128. [Google Scholar] [CrossRef]
- Scarpelli, S.; Gorgoni, M.; D’Atri, A.; Reda, F.; De Gennaro, L. Advances in Understanding the Relationship between Sleep and Attention Deficit-Hyperactivity Disorder (ADHD). J. Clin. Med. 2019, 8, 1737. [Google Scholar] [CrossRef] [Green Version]
- Neto, F.K.; Noschang, R.; Nunes, M.L. The Relationship between Epilepsy, Sleep Disorders, and Attention Deficit Hyperactivity Disorder (ADHD) in Children: A Review of the Literature. Sleep Sci. 2016, 9, 158–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaufman, J.; Birmaher, B.; Brent, D.; Rao, U.; Flynn, C.; Moreci, P.; Williamson, D.; Ryan, N. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial Reliability and Validity Data. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 980–988. [Google Scholar] [CrossRef] [PubMed]
- Conners, C.K.; Sitarenios, G.; Parker, J.D.; Epstein, J.N. The Revised Conners’ Parent Rating Scale (CPRS-R): Factor Structure, Reliability, and Criterion Validity. J. Abnorm. Child Psychol. 1998, 26, 257–268. [Google Scholar] [CrossRef]
- Wechsler, D. Wechsler Intelligence Scale for Children-Fourth Edition (WISC-IV); Giunti Organizzazioni Speciali; Italian Adaptation by Orsini, Pezzuti, Picone: Firenze, Italy, 2012. [Google Scholar]
- Korkman, M.; Kirk, U.; Kemp, S.L. NEPSY–II: Second Edition; Giunti Organizzazioni Speciali; Italian Adaptation by Urgesi, Campanella and Fabbro: Firenze, Italy, 2011. [Google Scholar]
- American Psychiatric Association. Neurodevelopmental Disorders: Attention-Deficit/Hyperactivity Disorder. In Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5); American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar] [CrossRef] [Green Version]
- Berry, R.B.; Brooks, R.; Gamaldo, C.E.; Harding, S.M.; Marcus, C.L.; Vaughn, B.V.; Vaughn, V.B. The AASM Manual for the Scoring of Sleep and Associated Events. Am. Acad. Sleep Med. 2013, 53, 1689–1699. [Google Scholar] [CrossRef]
- Delorme, A.; Makeig, S. EEGLAB: An Open Source Toolbox for Analysis of Single-Trial EEG Dynamics Including Independent Component Analysis. J. Neurosci. Methods 2004, 134, 9–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castelnovo, A.; Zago, M.; Casetta, C.; Zangani, C.; Donati, F.; Canevini, M.; Riedner, B.A.; Tononi, G.; Ferrarelli, F.; Sarasso, S.; et al. Slow Wave Oscillations in Schizophrenia First-Degree Relatives: A Confirmatory Analysis and Feasibility Study on Slow Wave Traveling. Schizophr. Res. 2020, 221, 37–43. [Google Scholar] [CrossRef]
- Nichols, T.E.; Holmes, A.P. Nonparametric Permutation Tests for Functional Neuroimaging: A Primer with Examples. Hum. Brain Mapp. 2002, 15, 1–25. [Google Scholar] [CrossRef] [Green Version]
- Riedner, B.A.; Hulse, B.K.; Murphy, M.J.; Ferrarelli, F.; Tononi, G. Temporal Dynamics of Cortical Sources Underlying Spontaneous and Peripherally Evoked Slow Waves. Prog. Brain Res. 2011, 193, 201–218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castelnovo, A.; D’Agostino, A.; Casetta, C.; Sarasso, S.; Ferrarelli, F. Sleep Spindle Deficit in Schizophrenia: Contextualization of Recent Findings. Curr. Psychiatry Rep. 2016, 18, 72. [Google Scholar] [CrossRef] [PubMed]
- Castelnovo, A.; Ferri, R.; Punjabi, N.M.; Castronovo, V.; Garbazza, C.; Zucconi, M.; Ferini-Strambi, L.; Manconi, M. The Paradox of Paradoxical Insomnia: A Theoretical Review towards a Unifying Evidence-Based Definition. Sleep Med. Rev. 2019, 44, 70–82. [Google Scholar] [CrossRef] [PubMed]
- Spiess, M.; Bernardi, G.; Kurth, S.; Ringli, M.; Wehrle, F.M.; Jenni, O.G.; Huber, R.; Siclari, F. How Do Children Fall Asleep? A High-Density EEG Study of Slow Waves in the Transition from Wake to Sleep. NeuroImage 2018, 178, 23–35. [Google Scholar] [CrossRef] [Green Version]
- Massimini, M.; Huber, R.; Ferrarelli, F.; Hill, S.; Tononi, G. The Sleep Slow Oscillation as a Traveling Wave. J. Neurosci. 2004, 24, 6862–6870. [Google Scholar] [CrossRef] [PubMed]
- Huber, R.; Ghilardi, M.F.; Massimini, M.; Ferrarelli, F.; Riedner, B.A.; Peterson, M.J.; Tononi, G. Arm Immobilization Causes Cortical Plastic Changes and Locally Decreases Sleep Slow Wave Activity. Nat. Neurosci. 2006, 9, 1169–1176. [Google Scholar] [CrossRef]
- Clarke, A.R.; Barry, R.J.; Johnstone, S.J.; Mccarthy, R.; Selikowitz, M. EEG Development in Attention Deficit Hyperactivity Disorder: From Child to Adult. Clin. Neurophysiol. 2019, 130, 1256–1262. [Google Scholar] [CrossRef]
- Corsi-Cabrera, M.; Guevara, M.A.; Del Río-Portilla, Y.; Arce, C.; Villanueva-Hernández, Y. EEG Bands during Wakefulness, Slow-Wave and Paradoxical Sleep as a Result of Principal Component Analysis in Man. Sleep 2000, 23, 738–744. [Google Scholar] [CrossRef]
- Gorgoni, M.; D’Atri, A.; Scarpelli, S.; Reda, F.; De Gennaro, L. Sleep Electroencephalography and Brain Maturation: Developmental Trajectories and the Relation with Cognitive Functioning. Sleep Med. 2020, 66, 33–50. [Google Scholar] [CrossRef]
- De Gennaro, L.; Marzano, C.; Veniero, D.; Moroni, F.; Fratello, F.; Curcio, G.; Ferrara, M.; Ferlazzo, F.; Novelli, L.; Concetta Pellicciari, M.; et al. Neurophysiological Correlates of Sleepiness: A Combined TMS and EEG Study. NeuroImage 2007, 36, 1277–1287. [Google Scholar] [CrossRef]
- Marzano, C.; Ferrara, M.; Curcio, G.; De Gennaro, L. The Effects of Sleep Deprivation in Humans: Topographical Electroencephalogram Changes in Non-Rapid Eye Movement (NREM) Sleep versus REM Sleep. J. Sleep Res. 2010, 19, 260–268. [Google Scholar] [CrossRef] [PubMed]
- Campbell, I.G.; Feinberg, I. Longitudinal Trajectories of Non-Rapid Eye Movement Delta and Theta EEG as Indicators of Adolescent Brain Maturation. Proc. Natl. Acad. Sci. USA 2009, 106, 5177–5180. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ringli, M.; Huber, R. Developmental Aspects of Sleep Slow Waves: Linking Sleep, Brain Maturation and Behavior. Prog. Brain Res. 2011, 193, 63–82. [Google Scholar] [CrossRef] [PubMed]
- Tarokh, L.; Carskadon, M.A. Developmental Changes in the Human Sleep EEG during Early Adolescence. Sleep 2010, 33, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Chu, C.J.; Leahy, J.; Pathmanathan, J.; Kramer, M.A.; Cash, S.S. The Maturation of Cortical Sleep Rhythms and Networks over Early Development. Clin. Neurophysiol. Off. J. Int. Fed. Clin. Neurophysiol. 2014, 125, 1360–1370. [Google Scholar] [CrossRef] [Green Version]
- Somsen, R.J.; van’t Klooster, B.J.; van der Molen, M.W.; van Leeuwen, H.M.; Licht, R. Growth Spurts in Brain Maturation during Middle Childhood as Indexed by EEG Power Spectra. Biol. Psychol. 1997, 44, 187–209. [Google Scholar] [CrossRef]
- D’Atri, A.; Novelli, L.; Ferrara, M.; Bruni, O.; De Gennaro, L. Different Maturational Changes of Fast and Slow Sleep Spindles in the First Four Years of Life. Sleep Med. 2018, 42, 73–82. [Google Scholar] [CrossRef]
- Novelli, L.; D’atri, A.; Marzano, C.; Finotti, E.; Ferrara, M.; Bruni, O.; De Gennaro, L. Mapping Changes in Cortical Activity during Sleep in the First 4 Years of Life. J. Sleep Res. 2016, 25, 381–389. [Google Scholar] [CrossRef] [Green Version]
- Faraone, S.V.; Biederman, J.; Mick, E. The Age-Dependent Decline of Attention Deficit Hyperactivity Disorder: A Meta-Analysis of Follow-up Studies. Psychol. Med. 2006, 36, 159–165. [Google Scholar] [CrossRef]
- Jenni, O.G.; Carskadon, M.A. Spectral Analysis of the Sleep Electroencephalogram during Adolescence. Sleep 2004, 27, 774–783. [Google Scholar]
- Tononi, G.; Cirelli, C. Sleep Function and Synaptic Homeostasis. Sleep Med. Rev. 2006, 10, 49–62. [Google Scholar] [CrossRef]
- Riedner, B.A.; Vyazovskiy, V.V.; Huber, R.; Massimini, M.; Esser, S.; Murphy, M.; Tononi, G. Sleep Homeostasis and Cortical Synchronization: III. A High-Density EEG Study of Sleep Slow Waves in Humans. Sleep 2007, 30, 1643–1657. [Google Scholar] [CrossRef] [PubMed]
- Hubbard, J.; Gent, T.C.; Hoekstra, M.M.B.; Emmenegger, Y.; Mongrain, V.; Landolt, H.-P.; Adamantidis, A.R.; Franken, P. Rapid Fast-Delta Decay Following Prolonged Wakefulness Marks a Phase of Wake-Inertia in NREM Sleep. Nat. Commun. 2020, 11, 3130. [Google Scholar] [CrossRef] [PubMed]
- Buchmann, A.; Ringli, M.; Kurth, S.; Schaerer, M.; Geiger, A.; Jenni, O.G.; Huber, R. EEG Sleep Slow-Wave Activity as a Mirror of Cortical Maturation. Cereb. Cortex 2011, 21, 607–615. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Touchette, E.; Petit, D.; Séguin, J.R.; Boivin, M.; Tremblay, R.E.; Montplaisir, J.Y. Associations between Sleep Duration Patterns and Behavioral/Cognitive Functioning at School Entry. Sleep 2007, 30, 1213–1219. [Google Scholar] [CrossRef] [PubMed]


| ADHD (n = 30) | CONTROL (n = 23) | |||||||
|---|---|---|---|---|---|---|---|---|
| M ± SD | Median | Min–Max | M ± SD | Median | Min–Max | |||
| Age (y) | 10.48 ± 2.06 | 10.33 | 7.80–13.83 | 10.15 ± 1.56 | 10.00 | 7.92–13.67 | ||
| BMI (kg/m2) | 18.71 ± 4.43 | 17.05 | 13.60–34.20 | 17.43 ± 2.71 | 17.10 | 13.80–23.60 | ||
| CPRS-R (tot) | 76.11 ± 10.78 | 78 | 59–99 | |||||
| WISC-IV (tot) | 100.19 ± 9.02 | 98 | 84–114 | |||||
| K-SADS-PL (tot) | 2.93 ± 0.26 | 3 | 2–3 | |||||
| Sex | Male | n = 21 | Male | n = 12 | ||||
| ADHD Subtypes | Inattentive | n = 6 | ||||||
| Hyperactive | n = 2 | |||||||
| Combined | n = 22 | |||||||
| Sleep Phenotypes | Epileptic EEG abnormalities | n = 10 | ||||||
| Sleep onset insomnia | n = 5 | |||||||
| PLMI > 5 events/hour | n = 8 | |||||||
| OSAS | n = 15 | |||||||
| Narcoleptic-like | n = 4 | |||||||
| v-PSG § | ||||||||
| M ± SD | Median | Min–Max | M ± SD | Median | Min–Max | P | ES | |
| TIB (min) | 493.40 ± 39.81 | 493.82 | 384.73–568.77 | 503.44 ± 41.04 | 506.55 | 390.00–567.80 | 0.377 | |
| TST (min) | 408.96 ± 58.73 | 423.00 | 215.95–478.50 | 430.69 ± 52.02 | 440.42 | 275.27–499.93 | 0.17 | |
| SL (min) | 29.72 ± 23.39 | 22.72 | 1.35–81.87 | 23.08 ± 14.32 | 23.98 | 3.29–58.58 | 0.578 * | |
| REML (min) | 135.47 ± 56.75 | 116.38 | 55.50–299.57 | 111.01 ± 45.55 | 93.08 | 57.40–252.39 | 0.066 * | |
| WASO (min) | 54.71 ± 55.31 | 28.58 | 7.24–216.45 | 50.84 ± 45.01 | 31.98 | 10.11–199.67 | 0.787 | |
| SE (%) | 83.12 ± 11.73 | 86.23 | 48.49–97.45 | 85.74 ± 9.44 | 89.02 | 55.22–97.45 | 0.388 | |
| N1 (min) | 23.16 ± 8.85 | 21.66 | 9.50–39.50 | 24.93 ± 10.48 | 23.70 | 11.00–56.01 | 0.512 | |
| N1 (%TST) | 5.89 ± 2.84 | 5.28 | 2.03–15.03 | 5.86 ± 2.62 | 5.49 | 2.89–12.36 | 0.971 | |
| N2 (min) | 151.47 ± 38.84 | 153.50 | 17.00–199.88 | 160.40 ± 24.71 | 165.48 | 93.00–199.70 | 0.343 | |
| N2 (%TST) | 36.51 ± 7.97 | 37.07 | 7.87–49.67 | 37.31 ± 4.51 | 35.46 | 29.58–46.87 | 0.668 | |
| N3 (min) | 141.45 ± 26.35 | 137.35 | 104.50–195.00 | 147.70 ± 19.14 | 144.50 | 109.50–181.96 | 0.345 | |
| N3 (%TST) | 35.12 ± 7.34 | 33.38 | 24.65–56.49 | 34.52 ± 4.08 | 34.35 | 27.20–42.47 | 0.727 | |
| REM (min) | 92.87 ± 23.56 | 97.25 | 44.50–129.13 | 97.66 ± 28.84 | 101.00 | 39.00–161.50 | 0.512 | |
| REM (%TST) | 22.48 ± 3.68 | 22.20 | 15.18–28.30 | 22.30 ± 4.82 | 22.01 | 14.03–33.00 | 0.881 | |
| AI (n/h) | 13.48 ± 3.44 | 13.90 | 7.42–19.67 | 12.74 ± 3.1 | 12.67 | 6.96–18.15 | 0.422 | |
| AHI (n/h) | 2.04 ± 1.70 | 1.40 | 0.00–6.90 | 0.67 ± 0.8 | 0.40 | 0.00–3.10 | 0.002 | −1.002 |
| PLMI (n/h) | 2.96 ± 2.81 | 2.80 | 0.00–9.60 | 2.74 ± 3.55 | 1.50 | 0.00–12.70 | 0.807 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castelnovo, A.; Lividini, A.; Bernardi, G.; Pezzoli, V.; Foderaro, G.; Ramelli, G.P.; Manconi, M.; Miano, S. Sleep Power Topography in Children with Attention Deficit Hyperactivity Disorder (ADHD). Children 2022, 9, 197. https://doi.org/10.3390/children9020197
Castelnovo A, Lividini A, Bernardi G, Pezzoli V, Foderaro G, Ramelli GP, Manconi M, Miano S. Sleep Power Topography in Children with Attention Deficit Hyperactivity Disorder (ADHD). Children. 2022; 9(2):197. https://doi.org/10.3390/children9020197
Chicago/Turabian StyleCastelnovo, Anna, Althea Lividini, Giulio Bernardi, Valdo Pezzoli, Giuseppe Foderaro, Gian Paolo Ramelli, Mauro Manconi, and Silvia Miano. 2022. "Sleep Power Topography in Children with Attention Deficit Hyperactivity Disorder (ADHD)" Children 9, no. 2: 197. https://doi.org/10.3390/children9020197
APA StyleCastelnovo, A., Lividini, A., Bernardi, G., Pezzoli, V., Foderaro, G., Ramelli, G. P., Manconi, M., & Miano, S. (2022). Sleep Power Topography in Children with Attention Deficit Hyperactivity Disorder (ADHD). Children, 9(2), 197. https://doi.org/10.3390/children9020197







