Effects of Vision Therapy on Bilateral Amblyopia Unresponsive to Conventional Treatment: A Retrospective Comparative Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Study Population
2.3. Clinical Practice Protocol
2.4. Training Apparatus
2.5. Training Programs
2.6. Statistical Analysis
3. Results
3.1. Demographic and Clinical Characteristics of Patients
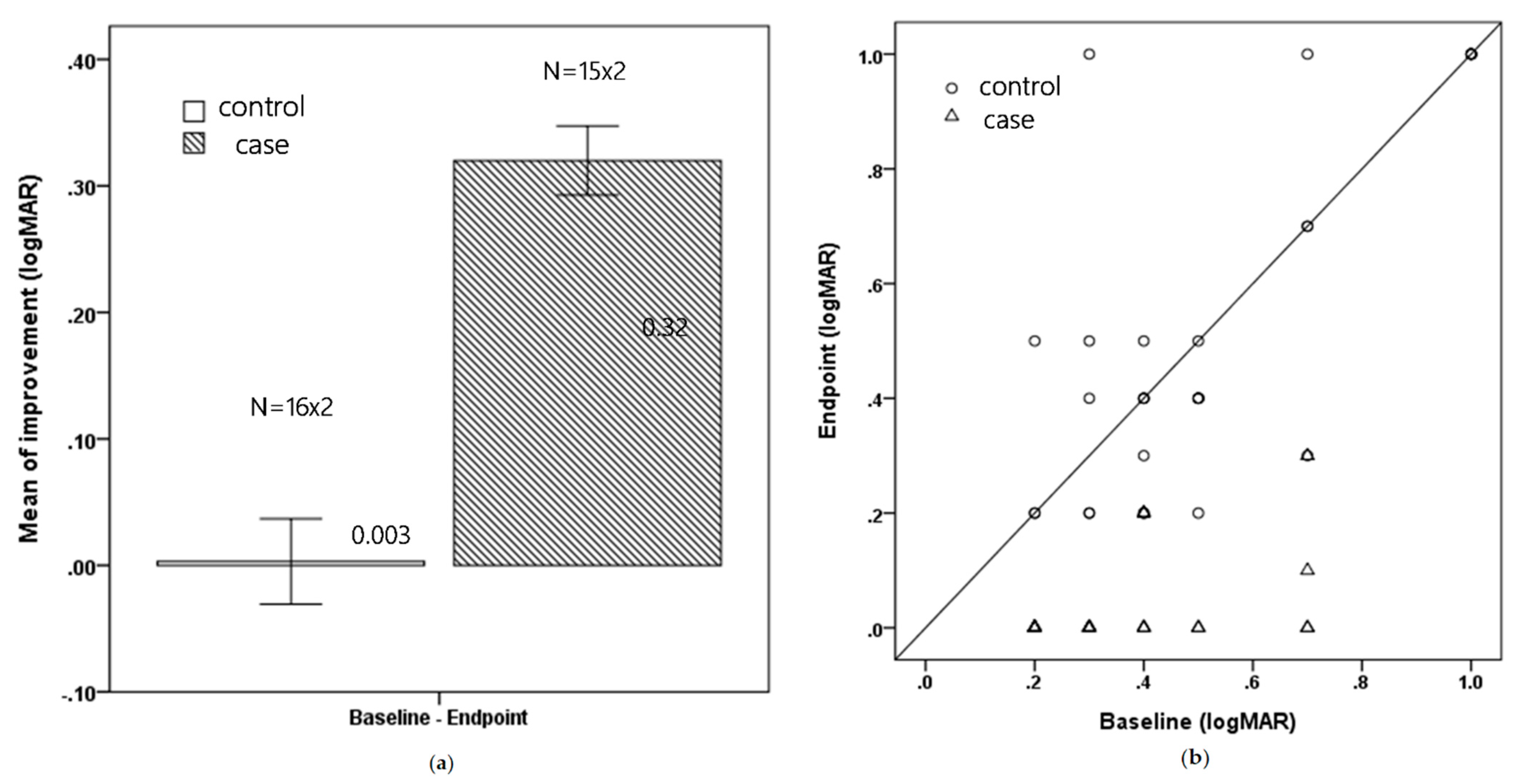
3.2. Visual Acuity
3.3. Timing of Visual Improvement
3.4. Stereoacuity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- McKee, S.P.; Levi, D.M.; Movshon, J.A. The pattern of visual deficits in amblyopia. J. Vis. 2003, 3, 380–405. [Google Scholar] [CrossRef]
- Snowdon, S.; Stewart-Brown, S. Effectiveness of preschool vision screening. Nurs. Stand. 1997, 12, 44–45. [Google Scholar] [CrossRef] [PubMed]
- Pediatric Eye Disease Investigator Group Writing Committee. A randomized trial comparing Bangerter filters and patching for the treatment of moderate amblyopia in children. Ophthalmology 2010, 117, 998–1004. [Google Scholar] [CrossRef] [Green Version]
- Felius, J.; Chandler, D.L.; Holmes, J.M.; Chu, R.H.; Cole, S.R.; Hill, M.; Huang, K.; Kulp, M.T.; Lazar, E.L.; Matta, N.S.; et al. Evaluating the burden of amblyopia treatment from the parent and child’s perspective. J. Am. Assoc. Pediatric Ophthalmol. Strabismus 2010, 14, 389–395. [Google Scholar] [CrossRef] [Green Version]
- Holmes, J.M.; Pediatric Eye Disease Investigator Group. A randomized pilot study of near activities versus non-near activities during patching therapy for amblyopia. J. Am. Assoc. Pediatric Ophthalmol. Strabismus 2005, 9, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Pediatric Eye Disease Investigator Group. A randomized trial of atropine versus patching for treatment of moderate amblyopia: Follow-up at 10 years of age. Arch. Ophthalmol. 2008, 126, 1039–1044. [Google Scholar] [CrossRef]
- Wallace, D.K.; Chandler, D.L.; Beck, R.W.; Arnold, R.W.; Bacal, D.A.; Birch, E.E.; Felius, J.; Frazier, M.; Holmes, J.M.; Hoover, D.; et al. Treatment of bilateral refractive amblyopia in children three to less than 10 years of age. Am. J. Ophthalmol. 2007, 144, 487–496. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klimek, D.L.; Cruz, O.A.; Scott, W.E.; Davitt, B.V. Isoametropic amblyopia due to high hyperopia in children. J. Am. Assoc. Pediatric Ophthalmol. Strabismus 2004, 8, 310–313. [Google Scholar] [CrossRef] [PubMed]
- Brin, T.A.; Chow, A.; Carter, C.; Oremus, M.; Bobier, W.; Thompson, B. Efficacy of vision-based treatments for children and teens with amblyopia: A systematic review and meta-analysis of randomised controlled trials. BMJ Open Ophthalmol. 2021, 6, e000657. [Google Scholar] [CrossRef] [PubMed]
- Bernell Corporation. Available online: https://www.bernell.com/category/Vision-Therapy (accessed on 1 February 2022).
- Ziylan, S.; Yabas, O.; Zorlutuna, N.; Serin, D. Isoametropic amblyopia in highly hyperopic children. Acta Ophthalmol. Scand. 2007, 85, 111–113. [Google Scholar] [CrossRef]
- Lin, P.W.; Chang, H.W.; Lai, I.C.; Teng, M.C. Visual outcomes after spectacles treatment in children with bilateral high refractive amblyopia. Clin. Exp. Optom. 2016, 99, 550–554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hernández-Rodríguez, C.J.; Piñero, D.P. Active Vision Therapy for Anisometropic Amblyopia in Children: A Systematic Review. J. Ophthalmol. 2020, 2020, 4282316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garzia, R.P. Efficacy of vision therapy in amblyopia: A literature review. Am. J. Optom. Physiol. Opt. 1987, 64, 393–404. [Google Scholar] [CrossRef] [PubMed]
- Li, R.W.; Levi, D.M. Characterizing the mechanisms of improvement for position discrimination in adult amblyopia. J. Vis. 2004, 4, 476–487. [Google Scholar] [CrossRef]
- Yalcin, E.; Balci, O. Efficacy of perceptual vision therapy in enhancing visual acuity and contrast sensitivity function in adult hypermetropic anisometropic amblyopia. Clin. Ophthalmol. 2014, 8, 49–53. [Google Scholar]
- Gopal, S.K.S.; Kelkar, J.; Kelkar, A.; Pandit, A. Simplified updates on the pathophysiology and recent developments in the treatment of amblyopia: A review. Indian J. Ophthalmol. 2019, 67, 1392–1399. [Google Scholar]
- Li, R.W.; Young, K.G.; Hoenig, P.; Levi, D.M. Perceptual learning improves visual performance in juvenile amblyopia. Investig. Ophthal. Vis. Sci. 2005, 46, 3161–3168. [Google Scholar] [CrossRef]
- Levi, D.M.; Li, R.W. Perceptual learning as a potential treatment for amblyopia: A mini-review. Vis. Res. 2009, 49, 2535–2549. [Google Scholar] [CrossRef] [Green Version]
- Gibson, E.J. Perceptual learning. Annu. Rev. Psychol. 1963, 14, 29–56. [Google Scholar] [CrossRef]
- Xi, J.; Jia, W.L.; Feng, L.X.; Lu, Z.L.; Huang, C.B. Perceptual learning improves stereoacuity in amblyopia. Investig. Ophthalmol. Vis. Sci. 2014, 55, 2384–2391. [Google Scholar] [CrossRef]
- Papageorgiou, E.; Asproudis, I.; Maconachie, G.; Tsironi, E.E.; Gottlob, I. The treatment of amblyopia: Current practice and emerging trends. Graefes Arch. Clin. Exp. Ophthalmol. 2019, 257, 1061–1078. [Google Scholar] [CrossRef]
- Liu, X.Y.; Zhang, Y.W.; Gao, F.; Chen, F.; Zhang, J.Y. Dichoptic Perceptual Training in Children With Amblyopia With or Without Patching History. Investig. Ophthalmol. Vis. Sci. 2021, 62, 4. [Google Scholar] [CrossRef]
- Liu, X.Y.; Zhang, J.Y. Dichoptic training in adults with amblyopia: Additional stereoacuity gains over monocular training. Vis. Res. 2018, 152, 84–90. [Google Scholar] [CrossRef]
- Shoshany, T.N.; Michalak, S.; Staffa, S.J.; Chinn, R.N.; Bishop, K.; Hunter, D.G. Effect of Primary Occlusion Therapy in Asymmetric, Bilateral Amblyopia. Am. J. Ophthalmol. 2020, 211, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Wang, J. Compliance and patching and atropine amblyopia treatments. Vis. Res. 2015, 114, 31–34. [Google Scholar] [CrossRef]
- Wallace, M.P.; Stewart, C.E.; Moseley, M.J.; Stephens, D.A.; Fielder, A.R.; Monitored Occlusion Treatment Amblyopia Study (MOTAS) Cooperatives; Randomized Occlusion Treatment Amblyopia Study (ROTAS) Cooperatives. Compliance with occlusion therapy for childhood amblyopia. Investig. Ophthalmol. Vis. Sci. 2013, 17, 6158–6166. [Google Scholar] [CrossRef] [PubMed]
- Choi, D.D.; Kim, D.H.; Kim, U.S.; Baek, S.H. Effect of refractive error type in the amblyopic eyes on factors for treatment success in anisometropic amblyopia. Sci. Rep. 2021, 11, 21927. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.-Y.; Kim, D.H.; Kim, U.S.; Baek, S.-H. Anisometropic amblyopia: Distribution of refractive errors and clinical characteristics of patients from an eye hospital. Ann. Optom. Contact Lens 2020, 2020, 11–17. [Google Scholar]

| Study (n= 15) | Control (n = 16) | p Value | |
|---|---|---|---|
| Age | 7.60 (0.74) | 7.63 (0.72) | 0.924 |
| Sex | 0.108 | ||
| Male | 6 (40.0%) | 11 (68.8%) | |
| Female | 9 (60.0%) | 5 (31.3%) | |
| History of patching | 0.693 | ||
| 2 (13.3%) | 3 (18.8%) | ||
| Anisometropia or Isometropia | 1.000 | ||
| A | 4 (26.7%) | 5 (31.3%) | |
| I | 11 (73.3%) | 11 (68.8%) | |
| Refractive error | |||
| 0 D to +1.00 D | 0 (0%) | 3 (18.8%) | |
| +1.00 D to <+2.00 D | 0 (0%) | 1 (6.2%) | |
| +2.00 D to <+3.00 D | 0 (0%) | 1 (6.2%) | |
| +3.00 D to <+4.00 D | 0 (0%) | 1 (6.2%) | |
| +4.00 D to <+5.00 D | 0 (0%) | 0 (0%) | |
| ≥+5.00 D | 1 (6.7%) | 2 (12.5%) | |
| −1.00 D to 0 D | 1 (6.7%) | 1 (6.2%) | |
| −2.00 D to <−1.00 D | 2 (13.3%) | 2 (12.5%) | |
| −3.00 D to <−2.00 D | 0 (0%) | 1 (6.2%) | |
| −4.00 D to <−3.00 D | 1 (6.7%) | 1 (6.2%) | |
| −5.00 D to <−4.00 D | 0 (0%) | 2 (12.5%) | |
| <−5.00 D | 10 (66.7%) | 1 (6.2%) | |
| Depth of Amblyopia | 0.3342 | ||
| severe (>0.7 logMAR) | 1 (6.7%) | 3 (18.7%) | |
| moderate (0.3 to 0.7 logMAR) | 8 (53.3%) | 10 (62.5%) | |
| mild (<0.3 logMAR) | 6 (40%) | 3 (18.7%) | |
| Mean follow up period (m) | 0.95 | ||
| 6.4 | 6.32 |
| Variables | Δ0−1 | Δ0−2 | Δ0−3 | Δ0−4 | Δ0-E | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C | T | p | C | T | p | C | T | p | C | T | p | C | T | p | |
| Number | 24 | 30 | 16 | 12 | 8 | 8 | 8 | 4 | 32 | 30 | |||||
| logMAR | 0.00 (0.00, 0.08) | 0.20 (0.20, 0.33) | <0.001 * | 0.00 (0.00, 0.10) | 0.20 (0.20, 0.30) | <0.001 * | 0.00 (0.00, 0.10) | 0.35 (0.20, 0.58) | 0.001 * | 0.00 (−0.08, 0.00) | 0.45 (0.33, 0.58) | <0.001 * | 0.00 (0.00, 0.10) | 0.30 (0.20, 0.40) | <0.001 * |
| Baseline | 3rd m | p | Baseline | 6th m | p | Baseline | 9th m | p | Baseline | 12th m | p | Baseline | Endpoint | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | 0.50 (0.33, 1.00) | 0.40 (0.33, 1.00) | 0.299 | 0.40 (0.30, 0.93) | 0.50 (0.20, 1.00) | 0.777 | 0.70 (0.30, 1.00) | 0.60 (0.20, 1.00) | 0.102 | 0.85 (0.40, 1.00) | 1.00 (0.28, 1.00) | 0.593 | 0.50 (0.33, 0.70) | 0.40 (0.30, 1.00) | 0.613 |
| Case | 0.30 (0.20, 0.40) | 0.00 (0.00, 0.20) | <0.001 * | 0.30 (0.20, 0.40) | 0.00 (0.00, 0.18) | 0.002 * | 0.45 (0.23, 0.65) | 0.05 (0.00, 0.10) | 0.011 * | 0.45 (0.33, 0.65) | 0.00 (0.00, 0.08) | 0.068 | 0.30 (0.20, 0.40) | 0.00 (0.00, 0.00) | <0.001 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, Y.-T.; Lin, H.-J.; Liao, W.-L.; Tsai, Y.-Y.; Hsieh, Y.-C. Effects of Vision Therapy on Bilateral Amblyopia Unresponsive to Conventional Treatment: A Retrospective Comparative Study. Children 2022, 9, 205. https://doi.org/10.3390/children9020205
Huang Y-T, Lin H-J, Liao W-L, Tsai Y-Y, Hsieh Y-C. Effects of Vision Therapy on Bilateral Amblyopia Unresponsive to Conventional Treatment: A Retrospective Comparative Study. Children. 2022; 9(2):205. https://doi.org/10.3390/children9020205
Chicago/Turabian StyleHuang, Yu-Te, Hui-Ju Lin, Wen-Ling Liao, Yi-Yu Tsai, and Yi-Ching Hsieh. 2022. "Effects of Vision Therapy on Bilateral Amblyopia Unresponsive to Conventional Treatment: A Retrospective Comparative Study" Children 9, no. 2: 205. https://doi.org/10.3390/children9020205
APA StyleHuang, Y.-T., Lin, H.-J., Liao, W.-L., Tsai, Y.-Y., & Hsieh, Y.-C. (2022). Effects of Vision Therapy on Bilateral Amblyopia Unresponsive to Conventional Treatment: A Retrospective Comparative Study. Children, 9(2), 205. https://doi.org/10.3390/children9020205






