Levels of Physical Activity in Children with Extremity Fractures a Dutch Observational Cross-Sectional Study
Abstract
:1. Introduction
2. Methods and Materials
2.1. Study Design and Setting
2.2. Study Population
2.3. Data Collection
2.4. Data Analysis
3. Results
3.1. Study Population and Baseline Characteristics
3.2. PA and the WHO’s Global Recommendations on Physical Activity for Health
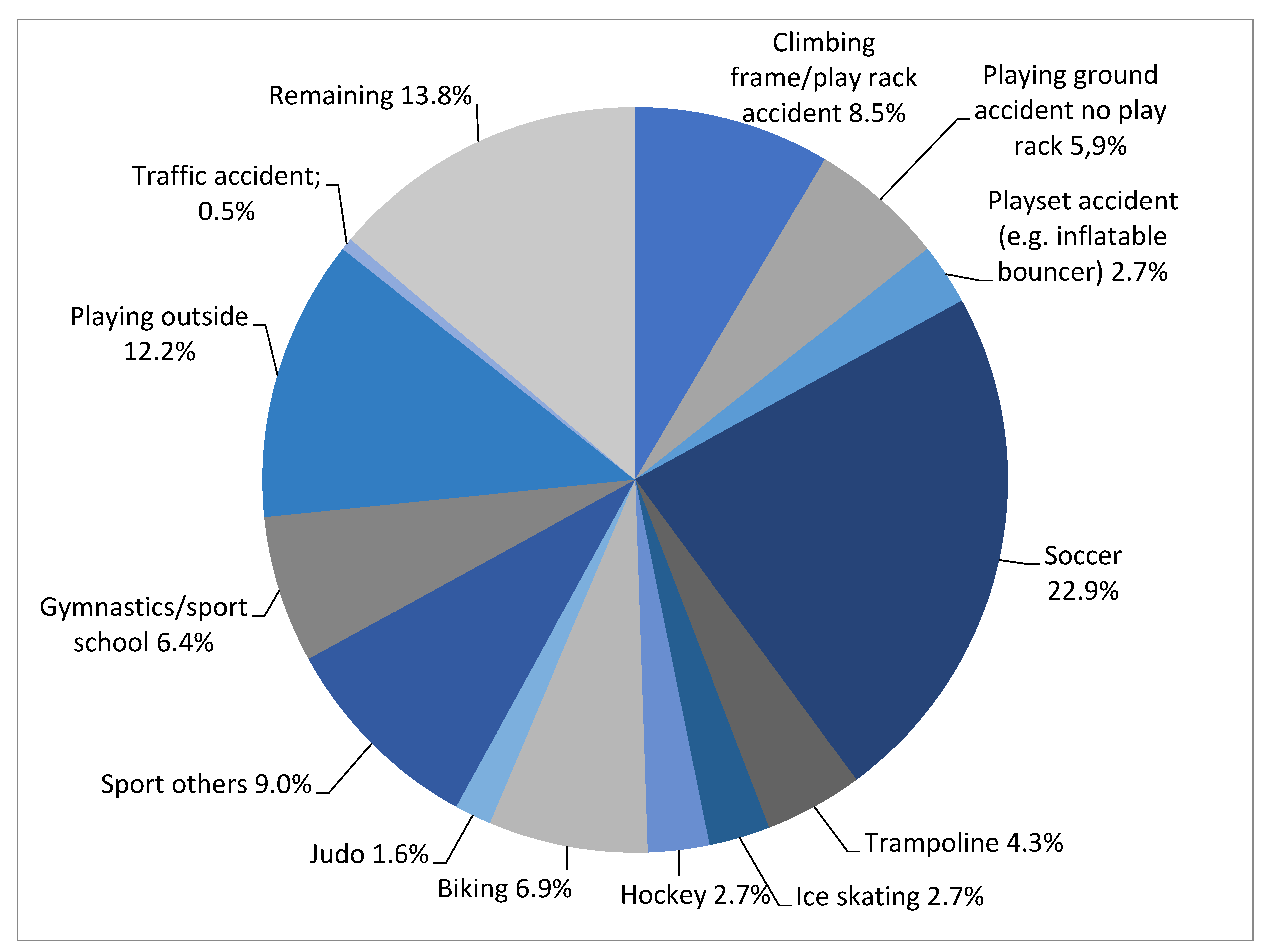
3.3. Trauma Mechanism and Type of Fracture
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Human Rights Statement
References
- Landin, L.A. Fracture patterns in children. Analysis of 8682 fractures with special reference to incidence, etiology and secular changes in a Swedish urban population 1950–1979. Acta Orthop. Scand. Suppl. 1983, 202, 1–109. [Google Scholar]
- Lyons, R.A.; Delahunty, A.M.; Kraus, D.; Heaven, M.; McCabe, M.; Allen, H.; Nash, P. Children’s fractures: A population based study. Inj. Prev. 1999, 5, 129–132. [Google Scholar] [CrossRef] [Green Version]
- Naranje, S.M.; Erali, R.A.; Warner, W.C., Jr.; Sawyer, J.R.; Kelly, D.M. Epidemiology of Pediatric Fractures Presenting to Emergency Departments in the United States. J. Pediatr. Orthop. 2016, 36, e45–e48. [Google Scholar] [CrossRef]
- Howe, A.S.; Asplund, C.A. General Principles of Fracture Management. Early and Late Complications. 2022, 17. Available online: https://www.uptodate.com/contents/general-principles-of-fracture-management-early-and-late-complications (accessed on 25 February 2022).
- Kopjar, B.; Wickizer, T.M. Fractures among children: Incidence and impact on daily activities. Inj. Prev. 1998, 4, 194–197. [Google Scholar] [CrossRef]
- Peterson, H.A. Epiphyseal Growth Plate Fractures; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2007. [Google Scholar]
- Weaver, C.; Gordon, C.; Janz, K.; Kalkwarf, H.; Lappe, J.M.; Lewis, R.; O’Karma, M.; Wallace, T.; Zemel, B. The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: A systematic review and implementation recommendations. Osteoporos. Int. 2016, 27, 1281–1386. [Google Scholar] [CrossRef] [Green Version]
- Löfgren, B.; Daly, R.; Nilsson, J.-Å.; Dencker, M.; Karlsson, M. An increase in school-based physical education increases muscle strength in children. Med. Sci. Sports Exerc. 2013, 45, 997–1003. [Google Scholar] [CrossRef]
- Tveit, M.; Rosengren, B.; Nilsson, J.-Å.; Karlsson, M. Exercise in youth: High bone mass, large bone size, and low fracture risk in old age. Scand. J. Med. Sci. Sports 2015, 25, 453–461. [Google Scholar] [CrossRef]
- Cöster, M.E.; Fritz, J.; Nilsson, J.-Å.; Karlsson, C.; Rosengren, B.E.; Dencker, M.; Karlsson, M.K. How does a physical activity programme in elementary school affect fracture risk? A prospective controlled intervention study in Malmo, Sweden. BMJ Open 2017, 7, e012513. [Google Scholar] [CrossRef]
- Sandseter, E.B.H. Scaryfunny: A Qualitative Study of Risky Play Among Preschool Children. Ph.D. Thesis, Norwegian University of Science and Technology, Trondheim, Norway, 2010. [Google Scholar]
- Clark, E.M.; Ness, A.R.; Tobias, J.H. Vigorous physical activity increases fracture risk in children irrespective of bone mass: A prospective study of the independent risk factors for fractures in healthy children. J. Bone Miner. Res. 2008, 23, 1012–1022. [Google Scholar] [CrossRef] [Green Version]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The physical activity guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- World Health Organization. Physical Activity Factsheets for the 28 European Union Member States of the WHO European Region; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- World Health Organization. Prevalence of Insufficient Physical Activity: School Going Adolescents Aged 11–17 Years; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Sport, Ministerie van Volksgezondheid Welzijn en Sports. Hoeveel Mensen Voldoen aan de Door de Gezondheidsraad Geadviseerde Beweegrichtlijnen? Rijksinstituut voor Volksgezondheid en Gezondheid (RIVM): Bilthoven, The Netherlands, 2017. [Google Scholar]
- Randsborg, P.H.; Røtterud, J.J. No difference in the level of physical activity between children who have or have never sustained a fracture. Scand. J. Med. Sci. Sports 2017, 27, 1801–1805. [Google Scholar] [CrossRef] [Green Version]
- Clark, E.M. The epidemiology of fractures in otherwise healthy children. Curr. Osteoporos. Rep. 2014, 12, 272–278. [Google Scholar] [CrossRef]
- Wendel-Vos, W.; Schuit, J. Short Questionnaire to Assess Health Enhancing Physical Activity. SQUASH Bilthoven Neth. Inst. Public Health Environ. 2002. Available online: https://meetinstrumentenzorg.nl/wp-content/uploads/instrumenten/503_2_N.pdf (accessed on 25 February 2022).
- Wagenmakers, R.; van den Akker-Scheek, I.; Groothoff, J.W.; Zijlstra, W.; Bulstra, S.K.; Kootstra, J.W.; Wendel-Vos, G.W.; van Raaij, J.J.; Stevens, M. Reliability and validity of the short questionnaire to assess health-enhancing physical activity (SQUASH) in patients after total hip arthroplasty. BMC Musculoskelet. Disord. 2008, 9, 141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campbell, N.; Gaston, A.; Gray, C.; Rush, E.; Maddison, R.; Prapavessis, H. The Short QUestionnaire to ASsess Health-enhancing (SQUASH) physical activity in adolescents: A validation using doubly labeled water. J. Phys. Act. Health 2016, 13, 154–158. [Google Scholar] [CrossRef]
- Mota, J.; Coelho e Silva, M.; Raimundo, A.; Sardinha, L. Report Card on Physical Activity for Children and Youth. J. Physical Act. Health. 2016, 13 (Suppl. S2), 242–245. [Google Scholar] [CrossRef] [PubMed]
- Wren, T.A.; Shepherd, J.A.; Kalkwarf, H.J.; Zemel, B.S.; Lappe, J.M.; Oberfield, S.; Dorey, F.J.; Winer, K.K.; Gilsanz, V. Racial disparity in fracture risk between white and nonwhite children in the United States. J. Pediatr. 2012, 161, 1035–1040.e2. [Google Scholar] [CrossRef] [Green Version]
- Netherlands, S. StatLine: Leefstijl en (Preventief) Gezondheidsonderzoek: Persoonskenmerken 2021. Available online: https://opendata.cbs.nl/statline/#/CBS/nl/dataset/83021NED/table?ts=1645949292480 (accessed on 25 February 2022).
- Shanmugam, C.; Maffulli, N. Sports injuries in children. Br. Med. Bull. 2008, 86, 33–57. [Google Scholar] [CrossRef]
- Janssen, I.; LeBlanc, A.G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 40. [Google Scholar] [CrossRef] [Green Version]
- Branche, C.; Ozanne-Smith, J.; Oyebite, K.; Hyder, A.A. World Report on Child Injury Prevention; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Britton, J.W. Kids can’t fly: Preventing fall injuries in children. Off. Publ. State Med. Soc. Wis. 2005, 104, 33–36. [Google Scholar]
- Harvey, A.; Towner, E.; Peden, M.; Soori, H.; Bartolomeos, K. Injury prevention and the attainment of child and adolescent health. Bull. World Health Organ. 2009, 87, 390–394. [Google Scholar] [CrossRef]
- Kuiper, J.; Veiligheid, N.L.; van Rooijen, M. Position Paper Risicovol Spelen; Universiteit voor Humanistiek: Utrecht, The Netherlands, 2017. [Google Scholar]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Global trends in insufficient physical activity among adolescents: A pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc. Health 2020, 4, 23–35. [Google Scholar] [CrossRef]
- Randsborg, P.-H.; Gulbrandsen, P.; Benth, J.Š.; Sivertsen, E.A.; Hammer, O.-L.; Fuglesang, H.F.; Årøen, A.J. Fractures in children: Epidemiology and activity-specific fracture rates. JBJS 2013, 95, e42. [Google Scholar] [CrossRef] [PubMed]
- Wood, A.M.; Robertson, G.A.; Rennie, L.; Caesar, B.C.; Court-Brown, C.M. The epidemiology of sports-related fractures in adolescents. Injury 2010, 41, 834–838. [Google Scholar] [CrossRef] [PubMed]
- GGD. Gezondheidsmonitor Jeugd 2019; GGD’en en RIVM; GGD: Amsterdam, The Netherlands, 2019. [Google Scholar]
- GGD Gelderland Zuid. E-MOVO in Cijfers: Tabellenboek voor de Regio Nijmegen, Behorend tot E-MOVO Onderzoek 2015/2016; GGD: Amsterdam, The Netherlands, 2015. [Google Scholar]
- Mäyränpää, M. Fractures in Children: Epidemiology and Associated Bone Health Characteristics; Helsingin Yliopisto: Helsinki, Finland, 2012. [Google Scholar]
- Caine, D.; Maffulli, N.; Caine, C. Epidemiology of injury in child and adolescent sports: Injury rates, risk factors, and prevention. Clin. Sports Med. 2008, 27, 19–50. [Google Scholar] [CrossRef]
- Flynn, J.M.; Lou, J.E.; Ganley, T.J. Prevention of sports injuries in children. Clin. Sports Med. 2002, 14, 719–722. [Google Scholar] [CrossRef]
- Barry, A.R.; Egan, G.; Turgeon, R.D.; Leung, M. Evaluation of Physical Assessment Education for Practising Pharmacists: A Cross-Sectional Survey. Can. J. Hosp. Pharm. 2019, 72, 27. [Google Scholar] [CrossRef] [Green Version]
- Clemen, N.M.; Blacker, B.C.; Floen, M.J.; Schweinle, W.E.; Huber, J.N. Work-life balance in women physicians in South Dakota: Results of a state-wide assessment survey. S. D. Med. 2018, 71, 550–558. [Google Scholar]

| Characteristics | Study Population (n = 188) | Non-Respondents (n = 891) | p-Value |
|---|---|---|---|
| Gender–n (%) ‡ | |||
| Boys | 108 (57.4%) | 528 (59.3%) | 0.646 |
| Girls | 80 (42.6%) | 363 (40.7%) | |
| Mean age–years † | |||
| Total | 11.2 (SD = 3.7, Range 4–18) | 11.2 (SD = 3.9, Range 4–18) | 0.816 |
| Boys | 11.7 (SD = 3.9, Range 4–18) | 11.8(SD = 3.8, Range 4–18) | |
| Girls | 10.6 (SD = 3.37, Range 4–18) | 10.2 (SD = 3.7, Range 4–18) | |
| Age group–n (%) † | |||
| 4–12 years | 109 (58.0%) | 520 (58.4%) | 0.923 |
| 13–18 years | 79 (42.0%) | 371 (41.6%) | |
| n = 188 Children with Fractures | Children Meeting the Recommendations for Health (n = 95, 50.5%) | Children not Meeting the Recommendations for Health (n = 93, 49.5%) | p-Value |
|---|---|---|---|
| Age † (mean in years) | 10.97 (SD = 3.6) | 11.49 (SD = 3.8) | 0.080 |
| Gender ‡ (boy vs. girl n, %) | 57 vs. 38 60% vs. 40% | 51 vs. 42 55% vs. 45% | 0.477 |
| BMI *,† (mean) | 18 (SD = 3.4) | 17.8 (SD = 2.8) | 0.332 |
| Screentime † (mean min/day) | 191 (SD = 131.8) | 220 (SD = 171.3) | 0.384 |
| Type of fracture ‡ (Upper vs. lower extremity n, %) | 79 vs. 16 83% vs. 17% | 75 vs. 18 81% vs. 19% | 0.654 |
| Trauma occurred during sports **,‡ (n, %) | 56 (53%) | 49 (47%) | 0.337 |
| Time spent on sports † (mean in hours/week) | 7 (SD = 6.7) | 4.5 (SD = 3.2) | 0.004 |
| Time playing outside † (Mean min/day) | 26.1 (SD = 55.5) | 17.8 (SD = 35.2) | 0.226 |
| Total Population | Boys | Girls | p-Value * | 4–12 Years | 13–18 Years | p-Value * | |
|---|---|---|---|---|---|---|---|
| (n = 188) | |||||||
| Trauma mechanism ** | |||||||
| Sports-related | 105 (57.4%) | 59 (55.1%) | 46 (60.5%) | 0.468 | 47 (44.8%) | 58 (74.4%) | 0.001 |
| Fall from 0.5–3 m | 52 (28.4%) | 37 (34.6%) | 15 (19.7%) | 0.028 | 40 (38.1%) | 12 (15.3%) | 0.001 |
| Fall from 0.5 m or less | 26 (14.2%) | 11 (10.3%) | 15 (19.7%) | 0.071 | 18 (17.1%) | 8 (10.3%) | 0.187 |
| Physical activity | |||||||
| Achieved physical activity norm | 95 (50.5%) | 57 (52.8%) | 38 (47.5%) | 0.474 | 61 (56%) | 34 (43%) | 0.080 |
| Mean hours/day performing intensive activity | 2.4 (SD = 1.5) | 2.5 (SD = 1.5) | 2.4 (SD = 1.5) | 0.978 | 2.6 (SD = 1.4) | 2.2 (SD = 1.6) | 0.076 |
| Mean hours/week spent on sports | 5.8 (SD = 2.5) | 6.3 (SD = 6.0) | 5.2 (SD = 4.5) | 0.165 | 4.5(SD = 2.8) | 7.8 (SD = 7.2) | 0.001 |
| Mean minutes/day playing outside | 37.6 (SD = 56.2) | 21.9 (SD = 51.5) | 22.1 (SD = 39.6) | 0.978 | 29.7 (SD = 56.3) | 11.4 (SD = 2.9) | 0.003 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Traa, A.C.; Sir, O.; Frazer, S.W.T.; van de Kerkhof-van Bon, B.; Blatter, B.; Tan, E.C.T.H. Levels of Physical Activity in Children with Extremity Fractures a Dutch Observational Cross-Sectional Study. Children 2022, 9, 325. https://doi.org/10.3390/children9030325
Traa AC, Sir O, Frazer SWT, van de Kerkhof-van Bon B, Blatter B, Tan ECTH. Levels of Physical Activity in Children with Extremity Fractures a Dutch Observational Cross-Sectional Study. Children. 2022; 9(3):325. https://doi.org/10.3390/children9030325
Chicago/Turabian StyleTraa, Amber Carlijn, Ozcan Sir, Sanne W. T. Frazer, Brigitte van de Kerkhof-van Bon, Birgitte Blatter, and Edward C. T. H. Tan. 2022. "Levels of Physical Activity in Children with Extremity Fractures a Dutch Observational Cross-Sectional Study" Children 9, no. 3: 325. https://doi.org/10.3390/children9030325






