The Status of Laparoscopic Inguinal Hernia Surgery in Children: A Nationwide Assessment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Survey among All Pediatric Surgical Departments of Germany
- How many patients do you operate on with inguinal hernia per year?
- What technique is used for inguinal hernia repair?
- What kind of technique do you use for laparoscopic hernia repair?
- What is the reason to choose a specific technique?
- What kind of technique do you use for relapse?
- What size of instruments do you use?
- Who performs the surgery?
- Do you perform this surgery in incarcerated inguinal hernia?
2.2. Analysis of the National Database on Administrative Claims Data for Hospital Patients of Germany
2.3. Analysis of the Quality Reports of Germany
3. Results
3.1. Survey among All Pediatric Surgical Departments of Germany
3.2. Analysis of the National Database on Administrative Claims Data for Hospital Patients of Germany
3.3. Analysis of the Quality Reports of Germany
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Esposito, C.; Escolino, M.; Turrà, F.; Roberti, A.; Cerulo, M.; Farina, A.; Caiazzo, S.; Cortese, G.; Servillo, G.; Settimi, A. Current Concepts in the Management of Inguinal Hernia and Hydrocele in Pediatric Patients in Laparoscopic Era. Semin. Pediatr. Surg. 2016, 25, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Ein, S.H.; Njere, I.; Ein, A. Six Thousand Three Hundred Sixty-One Pediatric Inguinal Hernias: A 35-Year Review. J. Pediatr. Surg. 2006, 41, 980–986. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.-J.; Chen, J.Y.-C.; Hsu, C.-K.; Chuang, F.-C.; Yang, S.S.-D. The Incidence of Inguinal Hernia and Associated Risk Factors of Incarceration in Pediatric Inguinal Hernia: A Nation-Wide Longitudinal Population-Based Study. Hernia 2016, 20, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Raveenthiran, V.; Agarwal, P. Choice of Repairing Inguinal Hernia in Children: Open Versus Laparoscopy. Indian J. Pediatr. 2017, 84, 555–563. [Google Scholar] [CrossRef]
- Yilmaz, E.; Afsarlar, C.E.; Senel, E.; Cavusoglu, Y.H.; Karaman, I.; Karaman, A.; Ozguner, I.F. A Novel Technique for Laparoscopic Inguinal Hernia Repair in Children: Single-Port Laparoscopic Percutaneous Extraperitoneal Closure Assisted by an Optical Forceps. Pediatr. Surg. Int. 2015, 31, 639–646. [Google Scholar] [CrossRef]
- Davies, D.A.; Rideout, D.A.; Clarke, S.A. The International Pediatric Endosurgery Group Evidence-Based Guideline on Minimal Access Approaches to the Operative Management of Inguinal Hernia in Children. J. Laparoendosc. Adv. Surg. Tech. A 2020, 30, 221–227. [Google Scholar] [CrossRef]
- Alzahem, A. Laparoscopic versus Open Inguinal Herniotomy in Infants and Children: A Meta-Analysis. Pediatr. Surg. Int. 2011, 27, 605–612. [Google Scholar] [CrossRef]
- Kantor, N.; Travis, N.; Wayne, C.; Nasr, A. Laparoscopic versus Open Inguinal Hernia Repair in Children: Which Is the True Gold-Standard? A Systematic Review and Meta-Analysis. Pediatr. Surg. Int. 2019, 35, 1013–1026. [Google Scholar] [CrossRef]
- Feng, S.; Zhao, L.; Liao, Z.; Chen, X. Open Versus Laparoscopic Inguinal Herniotomy in Children: A Systematic Review and Meta-Analysis Focusing on Postoperative Complications. Surg. Laparosc. Endosc. Percutan. Tech. 2015, 25, 275–280. [Google Scholar] [CrossRef] [Green Version]
- Mahmood, B.; Christoffersen, M.; Miserez, M.; Bisgaard, T. Laparoscopic or Open Paediatric Inguinal Hernia Repair—A Systematic Review. Dan. Med. J. 2020, 67, A12190725. [Google Scholar]
- Zani, A.; Eaton, S.; Hoellwarth, M.E.; Puri, P.; Tovar, J.; Fasching, G.; Bagolan, P.; Lukac, M.; Wijnen, R.; Kuebler, J.F.; et al. International Survey on the Management of Esophageal Atresia. Eur. J. Pediatr. Surg. 2014, 24, 3–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olesen, C.S.; Andersen, K.; Öberg, S.; Deigaard, S.L.; Rosenberg, J. Variations in Open and Laparoscopic Repair of Paediatric Inguinal Hernia. Dan. Med. J. 2020, 67, A12190687. [Google Scholar] [PubMed]
- Schmedding, A.; Rolle, U. Decentralized Rather than Centralized Pediatric Surgery Care in Germany. Eur. J. Pediatr. Surg. 2017, 27, 399–406. [Google Scholar] [CrossRef]
- DGKCH Kinderchirurgische Kliniken Und Praxen. Available online: https://www.dgkch.de/menu-kinderchirurgie-in-deutschland/menu-kinderchirurgische-kliniken-praxen (accessed on 21 June 2020).
- Institute for the Hospital Remuneration System (INEK). Available online: https://www.g-drg.de/ (accessed on 30 January 2022).
- Federal Joint Committee (G-BA). Quality Reports of the Hospitals—Federal Joint Committee (G-BA). Available online: https://www.g-ba.de/themen/qualitaetssicherung/datenerhebung-zur-qualitaetssicherung/datenerhebung-qualitaetsbericht/ (accessed on 30 January 2022).
- Federal Institute for Drugs and Medical Devices BfArM—ICD-10-GM. Available online: https://www.bfarm.de/EN/Code-systems/Classifications/ICD/ICD-10-GM/_node.html;jsessionid=5F02DD5528CD7BF691E6F56ADE7CEEEB.intranet372 (accessed on 30 January 2022).
- Federal Institute for Drugs and Medical Devices BfArM—OPS. Available online: https://www.bfarm.de/EN/Code-systems/Classifications/OPS-ICHI/OPS/_node.html (accessed on 30 January 2022).
- Heydweiller, A.; Kurz, R.; Schröder, A.; Oetzmann von Sochaczewski, C. Inguinal Hernia Repair in Inpatient Children: A Nationwide Analysis of German Administrative Data. BMC Surg. 2021, 21, 372. [Google Scholar] [CrossRef]
- Fujiogi, M.; Michihata, N.; Matsui, H.; Fushimi, K.; Yasunaga, H.; Fujishiro, J. Outcomes Following Laparoscopic versus Open Surgery for Pediatric Inguinal Hernia Repair: Analysis Using a National Inpatient Database in Japan. J. Pediatr. Surg. 2019, 54, 577–581. [Google Scholar] [CrossRef]
- Chan, Y.Y.; Durbin-Johnson, B.; Kurzrock, E.A. Pediatric Inguinal and Scrotal Surgery—Practice Patterns in U.S. Academic Centers. J. Pediatr. Surg. 2016, 51, 1786–1790. [Google Scholar] [CrossRef] [Green Version]
- Dreuning, K.; Maat, S.; Twisk, J.; van Heurn, E.; Derikx, J. Laparoscopic versus Open Pediatric Inguinal Hernia Repair: State-of-the-Art Comparison and Future Perspectives from a Meta-Analysis. Surg. Endosc. 2019, 33, 3177–3191. [Google Scholar] [CrossRef] [Green Version]
- Nah, S.A.; Giacomello, L.; Eaton, S.; de Coppi, P.; Curry, J.I.; Drake, D.P.; Kiely, E.M.; Pierro, A. Surgical Repair of Incarcerated Inguinal Hernia in Children: Laparoscopic or Open? Eur. J. Pediatr. Surg. 2011, 21, 8–11. [Google Scholar] [CrossRef] [Green Version]
- Kaya, M.; Hückstedt, T.; Schier, F. Laparoscopic Approach to Incarcerated Inguinal Hernia in Children. J. Pediatr. Surg. 2006, 41, 567–569. [Google Scholar] [CrossRef]
- Takehara, H.; Yakabe, S.; Kameoka, K. Laparoscopic Percutaneous Extraperitoneal Closure for Inguinal Hernia in Children: Clinical Outcome of 972 Repairs Done in 3 Pediatric Surgical Institutions. J. Pediatr. Surg. 2006, 41, 1999–2003. [Google Scholar] [CrossRef]
- Maat, S.; Dreuning, K.; Nordkamp, S.; van Gemert, W.; Twisk, J.; Visschers, R.; van Heurn, E.; Derikx, J. Comparison of Intra- and Extra-Corporeal Laparoscopic Hernia Repair in Children: A Systematic Review and Pooled Data-Analysis. J. Pediatr. Surg. 2021, 56, 1647–1656. [Google Scholar] [CrossRef]
- Bruns, N.E.; Glenn, I.C.; McNinch, N.L.; Rosen, M.J.; Ponsky, T.A. Treatment of Routine Adolescent Inguinal Hernia Vastly Differs between Pediatric Surgeons and General Surgeons. Surg. Endosc. 2017, 31, 912–916. [Google Scholar] [CrossRef] [PubMed]
- Lobe, T.E.; Bianco, F.M. Adolescent Inguinal Hernia Repair: A Review of the Literature and Recommendations for Selective Management. Hernia J. Hernias Abdom. Wall Surg. 2022. [Google Scholar] [CrossRef] [PubMed]
- Yoshimura, S.; Migita, M.; Matsufuji, H. The Clinical Outcomes of Pediatric Inguinal Hernia Repairs Operated by Surgical Residents. Asian J. Surg. 2020, 43, 730–734. [Google Scholar] [CrossRef] [PubMed]
- Shibuya, S.; Fujiwara, N.; Ochi, T.; Wada, M.; Takahashi, T.; Lee, K.D.; Miyazaki, E. The Learning Curve of Laparoscopic Percutaneous Extraperitoneal Closure (LPEC) for Inguinal Hernia: Protocoled Training in a Single Center for Six Pediatric Surgical Trainees. BMC Surg. 2019, 19, 6. [Google Scholar] [CrossRef]

| Question | Respondents | Answers | Percentage |
|---|---|---|---|
| What is your clinical setting? | 52 | ||
| · Hospital department | 49 | 94.2% | |
| · Private practice with hospital beds | 3 | 5.8% | |
| Do you operate on children (0–14 years old) with indirect inguinal hernia in your department? | 48 | ||
| · Yes | 47 | 97.9% | |
| · No | 1 | 2.1% | |
| How many patients with inguinal hernia do you operate on per year? | 51 | ||
| · <50 | 6 | 11.8% | |
| · <100 | 12 | 23.5% | |
| · <150 | 17 | 33.3% | |
| · More than 150 | 16 | 31.4% | |
| What kind of technique do you use for inguinal hernia repair? | 51 | ||
| · Open surgery only | 24 | 47.1% | |
| · Laparoscopic surgery only | 3 | 5.9% | |
| · Both techniques | 24 | 47.1% | |
| Which technique do you perform in laparoscopic inguinal hernia repair? | 30 | ||
| · Percutaneous closure (1 trocar) | 10 | 33.3% | |
| · Intracorporal suture with cut of the peritoneum (2–3 trocar) | 9 | 30.0% | |
| · Intracorporal technique with sling (2–3 trocar) | 2 | 6.7% | |
| · Intracorporal suture without cut (2–3 trocar) | 8 | 26.7% | |
| · Other technique | 4 | 13.3% | |
| Indication for the kind of surgical technique of laparoscopic inguinal hernia repair. | 31 | ||
| · Age of the child | 16 | 51.6% | |
| · Sex of the child | 12 | 38.7% | |
| · Pre-existing condition of the child | 15 | 48.4% | |
| · Preference of the surgeon | 10 | 32.3% | |
| · Request of parents | 15 | 48.4% | |
| · Other | 8 | 25.8% | |
| Do you perform laparoscopic inguinal hernia repair in incarcerated hernia? | 30 | ||
| · Yes | 6 | 20.0% | |
| · No | 24 | 80.0% | |
| What kind of technique do you use in recurrent hernia? | 46 | ||
| · Always open surgery | 27 | 58.7% | |
| · Always minimal-invasive surgery | 5 | 10.9% | |
| · Change of technique (dependent on the method used before) | 13 | 28.3% | |
| What kind of instruments do you use for minimal-invasive surgery? | 30 | ||
| · 5 mm instruments | 10 | 33.3% | |
| · 3 mm instruments | 14 | 46.7% | |
| · 2 mm instruments | 6 | 20.0% | |
| What is your setting for minimal-invasive surgery? | 26 | ||
| · Outpatient procedure | 6 | 23.1% | |
| · Inpatient procedure | 13 | 50.0% | |
| · Inpatient and outpatient procedure | 7 | 26.9% | |
| Who is performing the laparoscopic inguinal hernia repair? | 31 | ||
| · Fully trained pediatric surgeons only | 16 | 51.6% | |
| · Fully trained pediatric surgeons and trainees | 14 | 45.2% | |
| · Trainees only | 1 | 3.2% |
| All | Open | Laparoscopic | ||||
|---|---|---|---|---|---|---|
| all | 9718 | 8926 | 91.9% | 801 | 8.2% | |
| males | 7968 | 82.0% | 7363 | 84.0% | 497 | 62.0% |
| females | 1750 | 18.0% | 1402 | 16.0% | 304 | 38.0% |
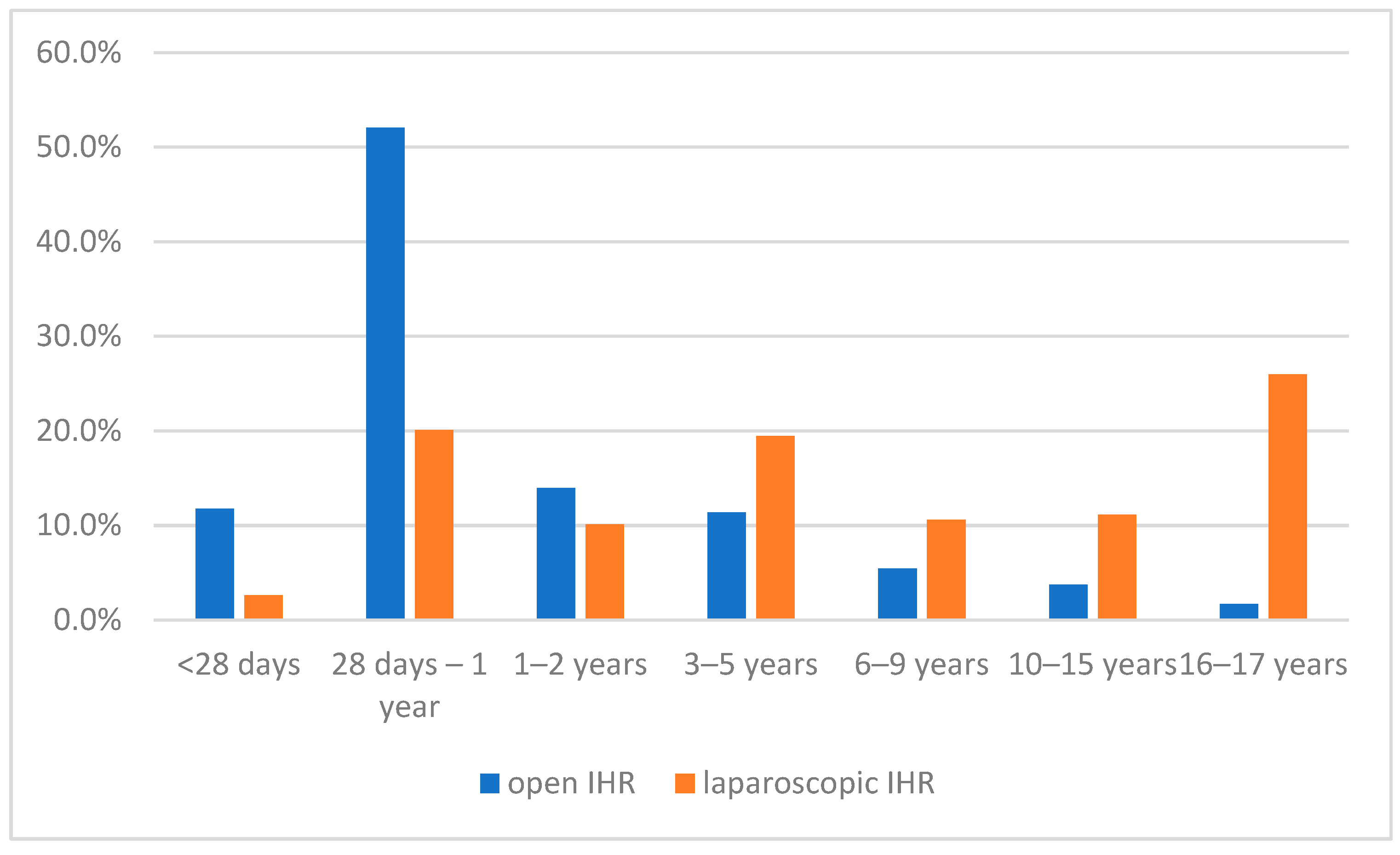
| 0–28 days | 1067 | 11.0% | 1046 | 11.7% | 21 | 2.6% |
| 29 days–1 year | 4757 | 49.0% | 4602 | 51.6% | 161 | 20.1% |
| 1–2 years | 1343 | 13.8% | 1263 | 14.1% | 81 | 10.1% |
| 3–5 years | 1192 | 12.3% | 1037 | 11.6% | 156 | 19.5% |
| 6–10 years | 578 | 5.9% | 493 | 5.5% | 85 | 10.6% |
| 11–15 years | 424 | 4.4% | 336 | 3.8% | 89 | 11.1% |
| 16–17 years | 357 | 3.7% | 149 | 1.7% | 208 | 26.0% |
| Inguinal hernia as main diagnosis | 7359 | 75.7% | 6643 | 68.4% | 718 | 89.6% |
| Recurrent inguinal hernia | 225 | 2.3% | 174 | 1.9% | 47 | 5.9% |
| Incarcerated inguinal hernia | 1089 | 11.2% | 1028 | 11.5% | 45 | 5.6% |
| Bilateral inguinal hernia | 1175 | 12.1% | 986 | 11.0% | 190 | 23.7% |
| Age Group | All | 0–9 | 10–17 | |||
|---|---|---|---|---|---|---|
| IHR without the use of any material | 364 | 45.3% | 317 | 62.9% | 47 | 15.6% |
| 68 | 8.5% | 61 | 12.1% | 7 | 2.3% |
| 296 | 36.8% | 256 | 50.8% | 40 | 13.3% |
| IHR with the use of any material | 440 | 54.7% | 187 | 37.1% | 253 | 84.3% |
| 354 | 44.0% | 186 | 36.9% | 168 | 56.0% |
| 86 | 10.7% | 1 | 0.2% | 85 | 28.3% |
| Material | ||||||
| 194 | 44.1% | 155 | 82.9% | 39 | 15.4% |
| 103 | 23.4% | 28 | 15.0% | 75 | 29.6% |
| 143 | 32.5% | 4 | 2.1% | 139 | 54.9% |
| Hospitals | Number of Laparoscopic IHR | ||||
|---|---|---|---|---|---|
| Number | % | Median | 1st Quartile | 3rd Quartile | |
| All hospitals | 40 | 4 | 1 | 16.5 | |
| - inpatient | 37 | 92.5% | 3 | 1 | 15 |
| - outpatient | 13 | 32.5% | 1 | 1 | 13 |
| University hospitals | 11 | 9.5 | 1.8 | 20 | |
| - inpatient | 9 | 81.8% | 8 | 2.5 | 19 |
| - outpatient | 5 | 45.5% | 1 | 1 | 17 |
| Non-university hospitals | 29 | 3 | 1 | 13 | |
| - inpatient | 28 | 96.6% | 3 | 1 | 11.5 |
| - outpatient | 7 | 24.1% | 1 | 1 | 1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schmedding, A.; Alsweed, A.; Muensterer, O.; Leonhardt, J. The Status of Laparoscopic Inguinal Hernia Surgery in Children: A Nationwide Assessment. Children 2022, 9, 348. https://doi.org/10.3390/children9030348
Schmedding A, Alsweed A, Muensterer O, Leonhardt J. The Status of Laparoscopic Inguinal Hernia Surgery in Children: A Nationwide Assessment. Children. 2022; 9(3):348. https://doi.org/10.3390/children9030348
Chicago/Turabian StyleSchmedding, Andrea, Ahmad Alsweed, Oliver Muensterer, and Johannes Leonhardt. 2022. "The Status of Laparoscopic Inguinal Hernia Surgery in Children: A Nationwide Assessment" Children 9, no. 3: 348. https://doi.org/10.3390/children9030348






