Relationship between Admission Temperature and Risk of Cerebral Palsy in Infants Admitted to Special Care Unit in a Low Resource Setting: A Retrospective Single-Center Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
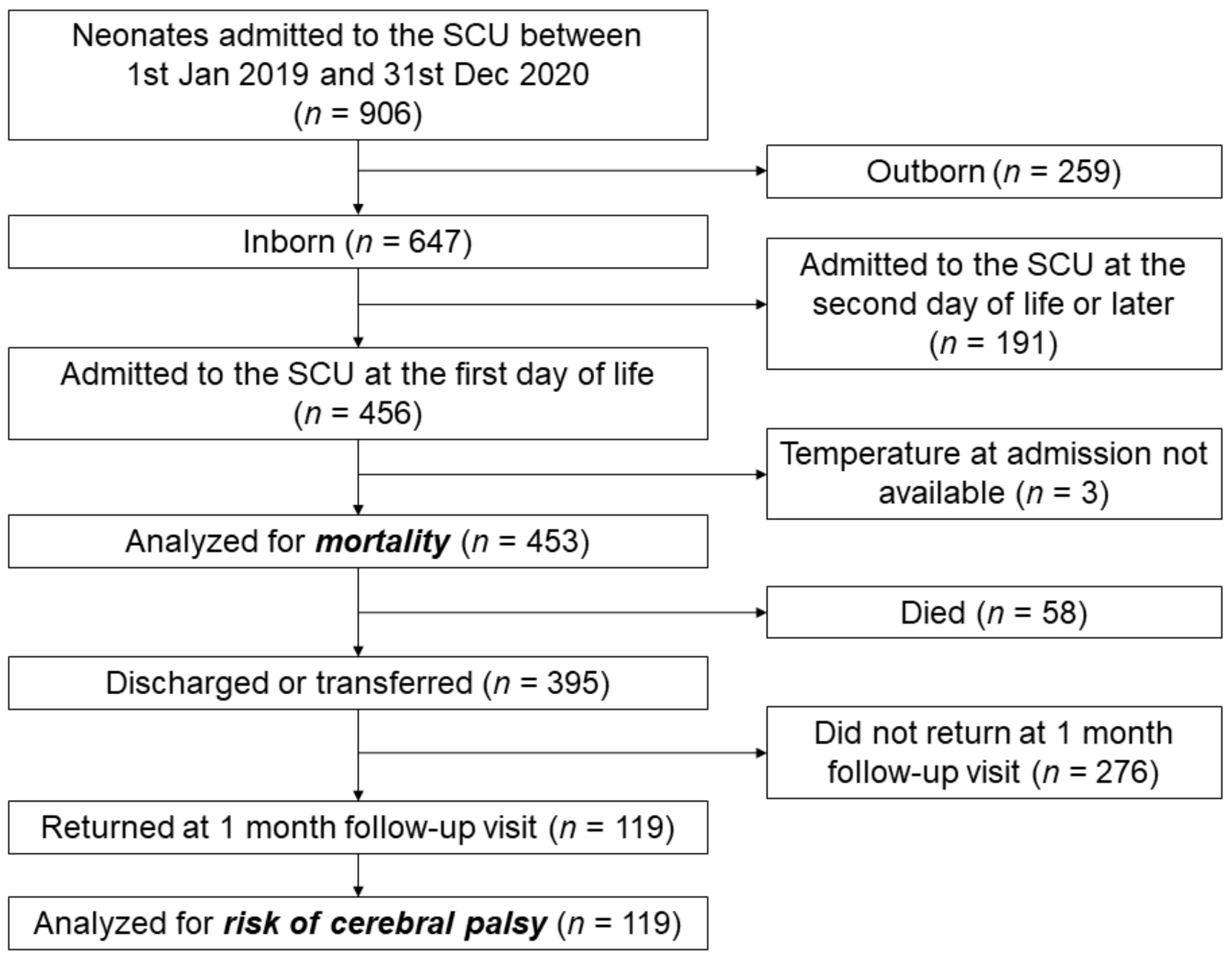
2.2. Patients
2.3. Data Collection
2.4. Neurological Examination
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Newborns: Improving Survival and Wellbeing. Available online: https://www.who.int/news-room/fact-sheets/detail/newbornsreducing-mortality (accessed on 23 December 2021).
- World Health Organization. Maternal Health and Safe Motherhood Programme & Meeting of Technical Working Group on Thermal Control of the Newborn (1992: Geneva, Switzerland). Thermal Control of the Newborn: A Practical Guide. Published online 1993. Available online: https://apps.who.int/iris/handle/10665/60042 (accessed on 13 January 2022).
- Lyu, Y.; Shah, P.S.; Ye, X.Y.; Warre, R.; Piedboeuf, B.; Deshpandey, A.; Dunn, M.; Lee, S.K. Canadian Neonatal Network Association between admission temperature and mortality and major morbidity in preterm infants born at fewer than 33 weeks’ gestation. JAMA Pediatr. 2015, 169, 150277. [Google Scholar] [CrossRef] [PubMed]
- Cavallin, F.; Calgaro, S.; Brugnolaro, V.; Wingi, O.M.; Muhelo, A.R.; Da Dalt, L.; Pizzol, D.; Putoto, G.; Trevisanuto, D. Non-linear association between admission temperature and neonatal mortality in a low-resource setting. Sci. Rep. 2020, 10, 20800. [Google Scholar] [CrossRef] [PubMed]
- Lunze, K.; Hamer, D.H. Thermal protection of the newborn in resource-limited environments. J. Perinatol. 2012, 32, 317–324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mullany, L.C. Neonatal hypothermia in low-resource settings. Semin. Perinatol. 2010, 34, 426–433. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lunze, K.; Bloom, D.E.; Jamison, D.T.; Hamer, D.H. The global burden of neonatal hypothermia: Systematic review of a major challenge for newborn survival. BMC Med. 2013, 11, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Trevisanuto, D.; Testoni, D.; de Almeida, M.F.B. Maintaining normothermia: Why and how? Semin. Fetal Neonatal. Med. 2018, 23, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Beletew, B.; Mengesha, A.; Wudu, M.; Abate, M. Prevalence of neonatal hypothermia and its associated factors in East Africa: A systematic review and meta-analysis. BMC Pediatr. 2020, 20, 148. [Google Scholar] [CrossRef] [PubMed]
- Kasdorf, E.; Perlman, J.M. Hyperthermia, inflammation, and perinatal brain injury. Pediatr. Neurol. 2013, 49, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Novak, I.; Morgan, C.; Adde, L.; Blackman, J.; Boyd, R.N.; Brunstrom-Hernandez, J.; Cioni, G.; Damiano, D.; Darrah, J.; Eliasson, A.C.; et al. Early, Accurate Diagnosis and Early Intervention in Cerebral Palsy: Advances in Diagnosis and Treatment. JAMA Pediatr. 2017, 171, 897–907. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Thermal Protection of the Newborn: A Practical Guide; Report No.: WHO/RHT/MSM/97.2; World Health Organization: Geneva, Switzerland, 1997. [Google Scholar]
- Kramer, L.I. Advancement of Dermal Icterus in the Jaundiced Newborn. Am. J. Dis. Child. 1969, 118, 454–458. [Google Scholar] [CrossRef] [PubMed]
- Spittle, A.J.; Walsh, J.; Olsen, J.E.; McInnes, E.; Eeles, A.L.; Brown, N.C.; Anderson, P.J.; Doyle, L.W.; Cheong, J.L. Neurobehaviour and neurological development in the first month after birth for infants born between 32–42 weeks’ gestation. Early Hum. Dev. 2016, 96, 7–14. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria. 2021. Available online: https://www.R-project.org/ (accessed on 13 January 2022).
- Laptook, A.R.; Salhab, W.; Bhaskar, B. Neonatal Research Network. Admission temperature of low-birth-weight infants: Predictors and associated morbidities. Pediatrics 2007, 119, e643–e649. [Google Scholar] [CrossRef] [PubMed]
- Wilson, E.; Maier, R.F.; Norman, M.; Misselwitz, B.; Howell, E.A.; Zeitlin, J.; Bonamy, A.K.; Van Reempts, P.; Martens, E.; Martens, G.; et al. Admission Hypothermia in Very Preterm Infants and Neonatal Mortality and Morbidity. J. Pediatr. 2016, 175, 61–67.e4. [Google Scholar] [CrossRef] [PubMed]
- Chang, H.Y.; Sung, Y.H.; Wang, S.M.; Lung, H.L.; Chang, J.H.; Hsu, C.H.; Jim, W.T.; Lee, C.H.; Hung, H.F. Short- and Long-Term Outcomes in Very Low Birth Weight Infants with Admission Hypothermia. PLoS ONE 2015, 10, e0131976. [Google Scholar] [CrossRef] [PubMed]
- Ng’eny, J.C.; Velaphi, S. Hypothermia among neonates admitted to the neonatal unit at a tertiary hospital in South Africa. J Perinatol. 2020, 40, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Miller, S.S.; Lee, H.C.; Gould, J.B. Hypothermia in very low birth weight infants: Distribution, risk factors and outcomes. J. Perinatol. 2011, 31 (Suppl. S1), S49–S56. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, Y.H.; Wang, L.; Huang, L.; Wang, L.L.; Huang, X.Y.; Fan, X.F.; Ding, Y.J.; Zhang, C.Y.; Liu, Q.; Sun, A.R.; et al. Association between admission hypothermia and outcomes in very low birth weight infants in China: A multicentre prospective study. BMC Pediatr. 2020, 20, 321. [Google Scholar] [CrossRef] [PubMed]
- Brown, V.B.; Oluwatosin, O.A. Feasibility of implementing a cellphone-based reminder/recall strategy to improve childhood routine immunization in a low-resource setting: A descriptive report. BMC Health Serv. Res. 2017, 17 (Suppl. S2), 703. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pietravalle, A.; Scilipoti, M.; Cavallin, F.; Lonardi, M.; Tshikamb, I.M.; Robbiati, C.; Trevisanuto, D.; Putoto, G. Nutritional education during rehabilitation of children 6–24 months with acute malnutrition, under unavailability of therapeutic/supplementary foods: A retrospective study in rural Angola. BMC Pediatr. 2021, 21, 94. [Google Scholar] [CrossRef] [PubMed]
- Lacerda Gontijoa, M.; Cardosoa, A.A.; da Silva Dittzb, E.; de Castro Magalhãesa, L. Drop out in a clinic of preterm development follow-up: Rates and causes. Cad. Bras. Ter. Ocup. 2018, 26, 73–83. [Google Scholar]


| Risk | HNNE |
|---|---|
| Low risk | 27–33 |
| Medium risk | 25.4–26.9 or 33.1–33.5 |
| High risk | <25.4 or >33.5 |
| Admitted Neonates (n = 453) | Newborns at 1 Month Follow-Up (n = 119) | |
|---|---|---|
| Males | 237 (52.3) | 65 (54.6) |
| Birth weight, grams a | 2750 (1940–3180) | 2610 (1795–3055) |
| Birth weight: | ||
| Normal birth weight (≥2500 g) | 269 (59.4) | 62 (52.1) |
| Low birth weight (1500–2499 g) | 130 (28.7) | 43 (36.1) |
| Very low birth weight (1000–1499 g) | 42 (9.3) | 14 (11.8) |
| Extremely low birth weight (<1000 g) | 12 (2.6) | 0 (0.0) |
| Temperature at admission, °C a | 35.4 (34.7–36.1) | 35.4 (24.8–35.9) |
| Temperature at admission: | ||
| 36.5–37.5 °C | 71 (15.7) | 16 (13.5) |
| 36–36.5 °C | 66 (14.6) | 13 (10.9) |
| <36 °C | 316 (69.7) | 90 (75.6) |
| HIV-positive mother | 35/450 (7.8) | 13/118 (11.0) |
| Maternal VDRL b | 7/438 (1.6) | 1/117 (0.9) |
| Apgar score at 1 min a | 5 (3–7) | 5 (2–8) |
| Apgar score at 5 min a | 7 (5–10) | 8 (5–10) |
| PROM c | 86 (19.0) | 22 (18.5) |
| Meconium-stained amniotic fluid | 133 (29.4) | 34 (28.6) |
| Maternal fever | 12 (2.6) | 2 (1.7) |
| Dexamethasone: | ||
| None | 414 (91.4) | 99 (84.2) |
| Complete cycle (24 mg) | 26 (5.7) | 14 (11.8) |
| Incomplete cycle (12 mg) | 13 (2.9) | 6 (5.0) |
| Mode of delivery | ||
| Spontaneous vaginal delivery | 221 (48.8) | 63 (52.9) |
| Assisted vaginal delivery | 42 (9.3) | 11 (9.3) |
| Caesarean section | 190 (41.9) | 45 (37.8) |
| Twin pregnancy | 61/452 (13.5) | 24 (20.2) |
| Birth asphyxia | 171 (37.7) | 49 (41.2) |
| Respiratory distress | 308 (68.0) | 83 (69.7) |
| Early-onset sepsis | 22 (4.9) | 6 (5.0) |
| Late-onset sepsis | 18 (4.0) | 5 (4.2) |
| Hypoglycemia | 20/428 (4.7) | 7/114 (6.1) |
| Jaundice | 85 (18.8) | 29 (24.4) |
| Weight loss | 10 (2.2) | 2 (1.7) |
| Skin infection | 14 (3.1) | 8 (6.7) |
| Major malformations or chromosomopathies d | 19 (4.2) | 2 (1.7) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guadagno, C.; Cavallin, F.; Brasili, L.; Maziku, D.M.; Leluko, D.E.; Azzimonti, G.; Putoto, G.; Pietravalle, A.; Trevisanuto, D. Relationship between Admission Temperature and Risk of Cerebral Palsy in Infants Admitted to Special Care Unit in a Low Resource Setting: A Retrospective Single-Center Study. Children 2022, 9, 352. https://doi.org/10.3390/children9030352
Guadagno C, Cavallin F, Brasili L, Maziku DM, Leluko DE, Azzimonti G, Putoto G, Pietravalle A, Trevisanuto D. Relationship between Admission Temperature and Risk of Cerebral Palsy in Infants Admitted to Special Care Unit in a Low Resource Setting: A Retrospective Single-Center Study. Children. 2022; 9(3):352. https://doi.org/10.3390/children9030352
Chicago/Turabian StyleGuadagno, Chiara, Francesco Cavallin, Luca Brasili, Donald Micah Maziku, Dionis Erasto Leluko, Gaetano Azzimonti, Giovanni Putoto, Andrea Pietravalle, and Daniele Trevisanuto. 2022. "Relationship between Admission Temperature and Risk of Cerebral Palsy in Infants Admitted to Special Care Unit in a Low Resource Setting: A Retrospective Single-Center Study" Children 9, no. 3: 352. https://doi.org/10.3390/children9030352
APA StyleGuadagno, C., Cavallin, F., Brasili, L., Maziku, D. M., Leluko, D. E., Azzimonti, G., Putoto, G., Pietravalle, A., & Trevisanuto, D. (2022). Relationship between Admission Temperature and Risk of Cerebral Palsy in Infants Admitted to Special Care Unit in a Low Resource Setting: A Retrospective Single-Center Study. Children, 9(3), 352. https://doi.org/10.3390/children9030352







