Placental Neutrophil Infiltration Associated with Tobacco Exposure but Not Development of Bronchopulmonary Dysplasia
Abstract
:1. Introduction
2. Materials and Methods
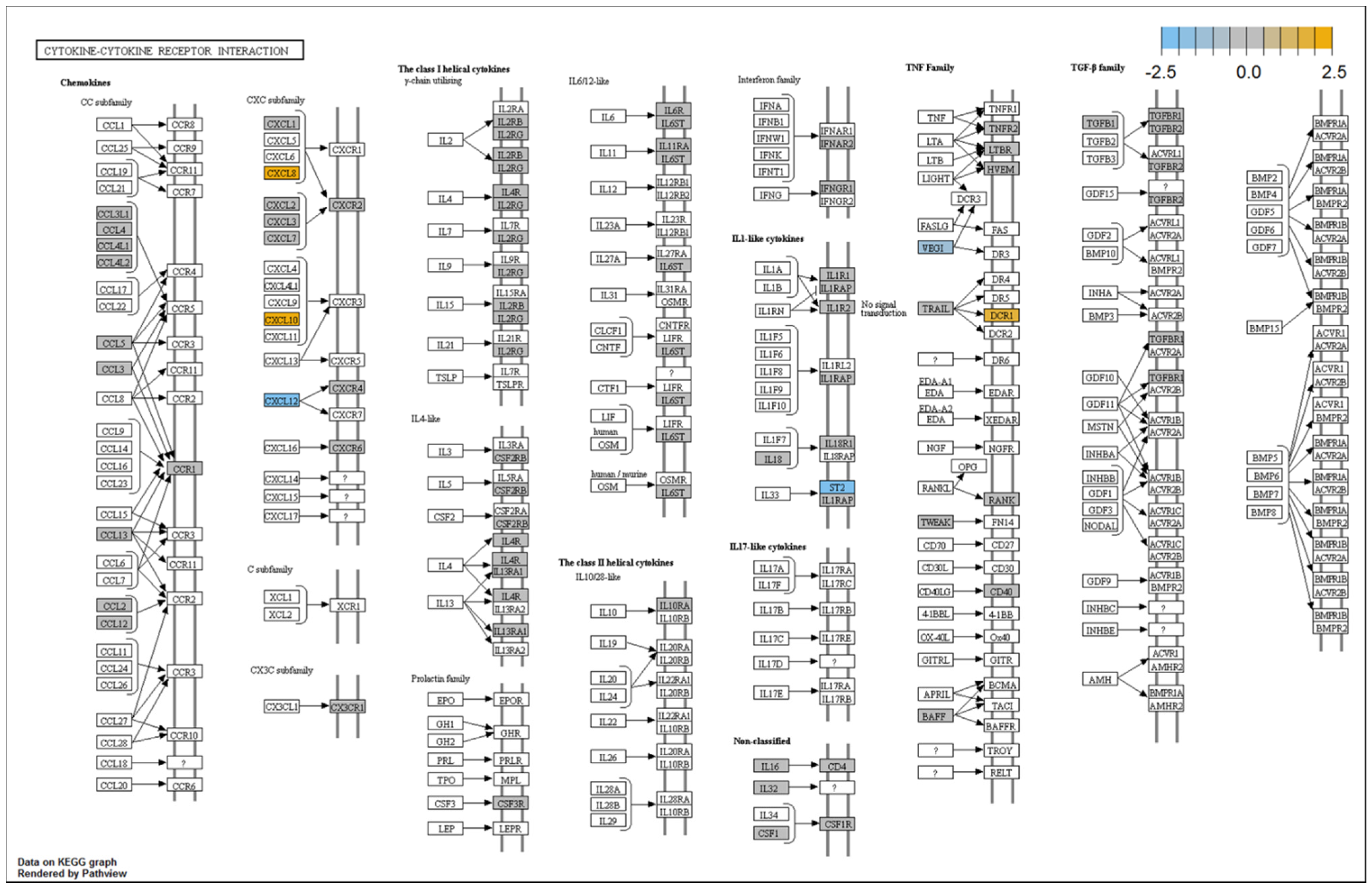
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A


| Maternal and Neonatal Demographic Data | ||||
|---|---|---|---|---|
| No BPD or Death | BPD or Death | |||
| (n = 22) | (n = 15) | Total (n = 39) | p Value | |
| Birth weight (g) | 1397.7 ± 355.1 | 711.7 ± 207.9 | 1133.8 ± 454.5 | <0.001 |
| Birth length (cm) | 39.4 ± 2.9 | 31.7 ± 2.6 | 36.5 ± 4.7 | <0.001 |
| Head circumference (cm) | 27.4 ± 1.8 | 22.5 ± 1.7 | 25.5 ± 3.0 | <0.001 |
| Gestational age (wk) | 29.8 ± 1.4 | 25.5 ± 1.9 | 28.2 ± 2.6 | <0.001 |
| Maternal age (yr) | 27.1 ± 5.6 | 28.2 ± 6.7 | 27.5 ± 6.0 | 0.643 |
| Sex | 0.083 | |||
| F | 14 (58.3) | 13 (86.7) | 27 (69.2) | |
| M | 10 (41.7) | 2 (13.3) | 12 (30.8) | |
| Maternal ethnicity | 0.233 | |||
| Black | 3 (12.5%) | 5 (33.3%) | 8 (20.5%) | |
| Black, Native American | 0 (0%) | 1 (6.7%) | 1 (2.6%) | |
| Hispanic | 7 (29.2%) | 1 (6.7%) | 8 (20.5%) | |
| Latino, White | 1 (4.2%) | 0 (0.0%) | 1 (2.6%) | |
| Native American | 3 (12.5%) | 1 (6.7%) | 4 (10.3%) | |
| White | 9 (37.5%) | 7 (46.7%) | 16(41.0%) | |
| White, Native American | 1 (4.2%) | 0 (0.0%) | 1 (2.6%) | |
| Antenatal steroid exposure | 23 (95.8) | 15 (100) | 38 (97.4) | 1.000 |
| Mode of delivery, C-Section | 14 (58.3) | 7 (46.7) | 21 (53.8) | 0.477 |
| Intubated in delivery room | 6 (25) | 12 (80) | 18 (46.2) | 0.001 |
| Intubated in NICU | 2 (8.3) | 9 (60.0) | 11 (28.2) | <0.001 |
| PDA medical treatment | 3 (12.5) | 8 (53.3) | 11 (28.2) | 0.010 |
| PDA surgical treatment | 0 (0) | 1 (6.7) | 1 (2.6) | 0.385 |
| IVH grade 3 or 4 | 1 (4.2) | 2 (13.3) | 3 (7.7) | 0.547 |
| Threshold ROP, yes | 0 (0) | 4 (26.7) | 4 (10.3) | 0.017 |
| IUGR <10th percentile, yes | 1 (4.2) | 2 (13.3) | 3 (7.7) | 0.547 |
| No BPD or Death | BPD or Death | |||
|---|---|---|---|---|
| (n = 24) | (n = 15) | Total (n = 39) | p Value | |
| Maternal diabetes | 4 (16.7) | 1 (6.7) | 5 (12.8) | 0.634 |
| Maternal hypertension | 3 (12.5) | 2 (13.3) | 5 (12.8) | 1.000 |
| Prolonged rupture of membranes (>18h) | 3 (12.5) | 4 (26.7) | 7 (17.9) | 0.396 |
| Histological chorioamnionitis | 12 (50) | 8 (53.3) | 20 (51.3) | 0.839 |
| Antepartum hemorrhage | 1 (4.2) | 7 (46.7) | 8 (20.5) | 0.003 |
| Maternal TE | 11 (45.8) | 6 (40) | 17 (43.6) | 0.721 |
| Maternal active smoking | 9 (37.5) | 3 (20) | 12 (30.8) | 0.305 |
| Maternal passive smoke exposure | 11 (45.8) | 7 (46.7) | 18 (46.2) | 0.959 |
| Illicit drugs, yes | 1 (4.21) | 1 (6.7) | 2 (5.1) | 0.765 |
| Gene | Log2-Fold Change | SE | Lower Confidence Limit (log2) | Upper Confidence Limit (log2) | p | Tentative Function |
|---|---|---|---|---|---|---|
| IL8 | 4.77 | 0.898 | 3.01 | 6.54 | 0.00034 | Cell Activation |
| S100A9 | 1.72 | 0.339 | 1.06 | 2.38 | 0.000477 | Cell–Cell Signaling |
| S100A8 | 3.33 | 0.912 | 1.54 | 5.12 | 0.00447 | Defense Response |
| IL1RL1 | −3.41 | 1.1 | −5.57 | −1.24 | 0.0115 | Receptor Signaling Protein Activity |
| CXCL10 | 3.06 | 1.09 | 0.922 | 5.21 | 0.0187 | Behavior |
| CD44 | 1.7 | 0.614 | 0.493 | 2.9 | 0.02 | Cell–Cell Signaling |
| TNFRSF10C | 1.53 | 0.562 | 0.433 | 2.64 | 0.0212 | Integral to Membrane |
| PLAUR | 1.78 | 0.676 | 0.454 | 3.11 | 0.0251 | Behavior |
| IRF7 | 1.08 | 0.415 | 0.269 | 1.9 | 0.0261 | Biopolymer Metabolic Process |
| MALT1 | −0.572 | 0.22 | −1 | −0.141 | 0.0263 | Cell Development |
| LILRB3 | 2.04 | 0.795 | 0.481 | 3.6 | 0.0281 | Cell Surface Receptor-Linked Signal Transduction |
| HLA-DRB1 | 2.74 | 1.14 | 0.502 | 4.99 | 0.0374 | Antigen Presentation |
| HLA-DRB3 | 1.78 | 0.746 | 0.316 | 3.24 | 0.0384 | Immune Response |
| HFE | −1.25 | 0.529 | −2.29 | −0.216 | 0.0394 | Cytoplasm |
| TNFSF15 | −1.43 | 0.604 | −2.61 | −0.244 | 0.0397 | Cell Development |
| CD99 | 1.12 | 0.475 | 0.186 | 2.05 | 0.0406 | Cytoplasm |
| PTPRC | 1.94 | 0.847 | 0.28 | 3.6 | 0.045 | Integral to Membrane |
| PTAFR | −2 | 0.881 | −3.73 | −0.273 | 0.0466 | Behavior |
| ZBTB16 | −2.01 | 0.888 | −3.75 | −0.272 | 0.0469 | Intracellular Organelle Part |
| PLA2G2A | −2.25 | 0.997 | −4.2 | −0.292 | 0.0479 | Cytoplasm |
| CXCL12 | −2.06 | 0.92 | −3.86 | −0.256 | 0.0492 | Behavior |
| HRAS | −1.39 | 0.621 | −2.6 | −0.169 | 0.0497 | Anatomical Structure Development |
| SELL | 1.66 | 0.757 | 0.177 | 3.15 | 0.053 | Integral to Membrane |
| PSMB9 | 1.13 | 0.578 | −0.00586 | 2.26 | 0.0798 | Antigen Presentation |
| NT5E | 0.917 | 0.482 | −0.0275 | 1.86 | 0.0862 | Biopolymer Metabolic Process |
| CCL3 | 1.66 | 0.885 | −0.0776 | 3.39 | 0.0907 | Cell Fraction |
| CD83 | 1.64 | 0.884 | −0.0944 | 3.37 | 0.0935 | Defense Response |
| NFKBIA | 0.72 | 0.398 | −0.0604 | 1.5 | 0.101 | Apoptosis |
| HLA-DRA | 1.16 | 0.648 | −0.114 | 2.43 | 0.105 | Cytoplasm |
| CLEC4A | 1.27 | 0.71 | −0.125 | 2.66 | 0.105 | Cell Surface Receptor-Linked Signal Transduction |
| HLA-C | 1.22 | 0.686 | −0.124 | 2.57 | 0.106 | Antigen Presentation |
| CXCL1 | 1.66 | 0.942 | −0.184 | 3.51 | 0.108 | Behavior |
| BCL3 | 1.25 | 0.717 | −0.158 | 2.65 | 0.112 | Cytoplasm |
| ITGAX | 1.77 | 1.03 | −0.243 | 3.79 | 0.115 | Anatomical Structure Morphogenesis |
| HLA-DMA | 0.667 | 0.396 | −0.11 | 1.44 | 0.123 | Antigen Presentation |
| TRAF5 | −1.05 | 0.631 | −2.29 | 0.183 | 0.126 | IκB Kinase NFκB Cascade |
| HLA-A | 0.723 | 0.436 | −0.131 | 1.58 | 0.128 | Antigen Presentation |
| GATA3 | −1.13 | 0.679 | −2.46 | 0.204 | 0.128 | Anatomical Structure Morphogenesis |
| CD74 | 1.29 | 0.78 | −0.237 | 2.82 | 0.129 | Biosynthetic Process |
| LILRB2 | 1.22 | 0.737 | −0.228 | 2.66 | 0.13 | Cell–Cell Signaling |
| BST1 | 1.07 | 0.649 | −0.205 | 2.34 | 0.131 | Humoral Immune Response |
| LTB4R2 | −0.977 | 0.594 | −2.14 | 0.187 | 0.131 | Behavior |
| RARRES3 | −1.23 | 0.764 | −2.73 | 0.268 | 0.139 | Cell Proliferation |
| TNFSF13B | 0.903 | 0.566 | −0.207 | 2.01 | 0.142 | Cell Fraction |
| XBP1 | 1.34 | 0.84 | −0.307 | 2.99 | 0.142 | DNA Binding |
| CD24 | 1.22 | 0.778 | −0.299 | 2.75 | 0.146 | Cell Surface |
| NFKB2 | 0.877 | 0.56 | −0.221 | 1.98 | 0.148 | Biopolymer Metabolic Process |
| ITGAE | −0.775 | 0.505 | −1.77 | 0.215 | 0.156 | Integral to Membrane |
| VCAM1 | −1.04 | 0.69 | −2.39 | 0.312 | 0.162 | Leukocyte Adhesion |
| PSMD7 | 0.342 | 0.229 | −0.106 | 0.79 | 0.165 | Macromolecular Complex |
| ATG12 | −1.03 | 0.691 | −2.38 | 0.328 | 0.168 | Apoptosis |
| CXCL2 | 1.32 | 0.896 | −0.434 | 3.08 | 0.171 | Behavior |
| MAPK11 | 0.721 | 0.497 | −0.254 | 1.7 | 0.178 | Intracellular Signaling Cascade |
| IL11RA | −0.872 | 0.603 | −2.05 | 0.311 | 0.179 | Integral to Membrane |
| TAL1 | −1.01 | 0.702 | −2.39 | 0.364 | 0.18 | Cell Proliferation |
| PPBP | 1.06 | 0.736 | −0.382 | 2.5 | 0.18 | Establishment of Localization |
| TNFRSF14 | −0.854 | 0.601 | −2.03 | 0.324 | 0.186 | Cell Surface Receptor-Linked Signal Transduction |
| ITGAM | 0.932 | 0.659 | −0.359 | 2.22 | 0.187 | Integral to Membrane |
| C2 | −0.415 | 0.294 | −0.991 | 0.161 | 0.188 | Defense Response |
| CD59 | 0.626 | 0.446 | −0.247 | 1.5 | 0.19 | Cell Fraction |
| TGFB1 | 1.15 | 0.817 | −0.455 | 2.75 | 0.191 | DNA Metabolic Process |
| MIF | 0.686 | 0.489 | −0.272 | 1.65 | 0.191 | Biosynthetic Process |
| FCGR2A | 1.97 | 1.41 | −0.789 | 4.72 | 0.192 | Phagocytosis |
| BATF3 | −0.858 | 0.62 | −2.07 | 0.358 | 0.197 | Biopolymer Metabolic Process |
| CCL4 | 0.946 | 0.685 | −0.397 | 2.29 | 0.198 | Anatomical Structure Morphogenesis |
| IFI35 | −0.559 | 0.406 | −1.36 | 0.237 | 0.199 | Nucleus |
| HLA-DPB1 | 1.39 | 1.01 | −0.591 | 3.36 | 0.199 | Multi-Organism Process |
| FCER1G | 0.953 | 0.699 | −0.417 | 2.32 | 0.203 | Integral to Membrane |
| FCGR3A/B | 2.03 | 1.49 | −0.902 | 4.95 | 0.205 | Immune Response |
| HLA-DPA | 1.33 | 1 | −0.639 | 3.3 | 0.215 | Antigen Presentation |
| SRC | −0.655 | 0.497 | −1.63 | 0.32 | 0.217 | Cell Surface Receptor-Linked Signal Transduction |
| IL1R2 | 0.888 | 0.681 | −0.446 | 2.22 | 0.221 | Immune Response |
| CXCR2 | 0.877 | 0.675 | −0.447 | 2.2 | 0.223 | Receptor for IL-8 |
| ITGAL | 1.15 | 0.894 | −0.598 | 2.91 | 0.226 | Leukocyte Adhesion |
| CFD | −0.558 | 0.433 | −1.41 | 0.29 | 0.226 | Cellular Macromolecule Metabolic Process |
| SOCS3 | 0.87 | 0.681 | −0.464 | 2.2 | 0.23 | Cell Development |
| IL2RG | 0.973 | 0.763 | −0.522 | 2.47 | 0.231 | Cell Surface |
| PECAM1 | −0.491 | 0.386 | −1.25 | 0.265 | 0.232 | Membrane |
| TNFRSF1B | 1.34 | 1.06 | −0.729 | 3.41 | 0.233 | Receptor Activity |
| CASP8 | 1.27 | 1.02 | −0.725 | 3.27 | 0.241 | Cell Development |
| GBP1 | 1.41 | 1.13 | −0.81 | 3.63 | 0.242 | Cell Metabolism |
| TLR2 | 0.784 | 0.644 | −0.478 | 2.05 | 0.251 | Cell Development |
| CDKN1A | −0.618 | 0.51 | −1.62 | 0.381 | 0.253 | Cell Development |
| S1PR1 | 0.794 | 0.662 | −0.503 | 2.09 | 0.258 | S1P Receptor |
| IL18 | 0.562 | 0.475 | −0.369 | 1.49 | 0.264 | Anatomical Structure Morphogenesis |
| TFRC | −0.715 | 0.632 | −1.95 | 0.523 | 0.284 | Cytoplasm |
| VTN | −1.19 | 1.07 | −3.29 | 0.904 | 0.291 | Extracellular Region |
| GPI | 1.29 | 1.16 | −0.987 | 3.56 | 0.293 | Hemostasis |
| MR1 | −0.763 | 0.689 | −2.11 | 0.587 | 0.294 | Immune Response |
| PRKCD | 0.638 | 0.578 | −0.495 | 1.77 | 0.296 | Biopolymer Metabolic Process |
| BCL10 | 1.35 | 1.22 | −1.05 | 3.74 | 0.296 | Cytoplasm |
| MAPK14 | 1.55 | 1.4 | −1.21 | 4.3 | 0.297 | Behavior |
| ZEB1 | −0.667 | 0.607 | −1.86 | 0.521 | 0.297 | Biopolymer Metabolic Process |
| EBI3 | 0.721 | 0.661 | −0.574 | 2.02 | 0.301 | Biosynthetic Process |
| PTPN2 | 1.05 | 0.969 | −0.849 | 2.95 | 0.304 | Biopolymer Metabolic Process |
| TNFRSF11A | −0.464 | 0.43 | −1.31 | 0.379 | 0.306 | Cell–Cell Signaling |
| IL32 | 0.781 | 0.733 | −0.655 | 2.22 | 0.312 | Defense Response |
| C1QA | 1.34 | 1.27 | −1.15 | 3.84 | 0.317 | Cell–Cell Signaling |
| CHUK | 1.23 | 1.18 | −1.08 | 3.54 | 0.322 | Anatomical Structure Morphogenesis |
| AHR | −0.603 | 0.579 | −1.74 | 0.533 | 0.323 | Biopolymer Metabolic Process |
| TGFBR2 | −0.33 | 0.323 | −0.963 | 0.304 | 0.331 | Cell Proliferation |
| IL13RA1 | 0.217 | 0.214 | −0.202 | 0.637 | 0.334 | Cell Surface Receptor-Linked Signal Transduction |
| PDCD1LG2 | −0.741 | 0.732 | −2.18 | 0.694 | 0.335 | Antigen Presentation |
| ETS1 | −0.659 | 0.666 | −1.96 | 0.647 | 0.346 | Hemopoiesis |
| FADD | 0.531 | 0.538 | −0.524 | 1.58 | 0.347 | Cell Development |
| HLA-B | 1.45 | 1.47 | −1.43 | 4.33 | 0.348 | Cell Fraction |
| MYD88 | 1.15 | 1.17 | −1.15 | 3.45 | 0.352 | IκB Kinase NFκB Cascade |
| CR1 | 0.723 | 0.742 | −0.731 | 2.18 | 0.353 | Integral to Membrane |
| TGFBI | 1.51 | 1.55 | −1.53 | 4.54 | 0.353 | Cell Proliferation |
| TRAF6 | −0.132 | 0.137 | −0.401 | 0.136 | 0.358 | Biopolymer Metabolic Process |
| LTBR | 1.26 | 1.33 | −1.33 | 3.86 | 0.363 | IκB Kinase NFκB Cascade |
| TLR7 | −0.604 | 0.637 | −1.85 | 0.644 | 0.365 | Biosynthetic Process |
| BCAP31 | −0.968 | 1.02 | −2.97 | 1.03 | 0.366 | Integral to Membrane |
| CD45R0 | 0.666 | 0.707 | −0.719 | 2.05 | 0.368 | Integral to Membrane |
| PSMC2 | 1.35 | 1.45 | −1.5 | 4.19 | 0.375 | Cytoplasm |
| CUL9 | −0.547 | 0.596 | −1.72 | 0.622 | 0.381 | Microtubule Dynamics |
| MAP4K4 | 0.236 | 0.258 | −0.269 | 0.742 | 0.381 | Biopolymer Metabolic Process |
| TLR4 | 1.05 | 1.15 | −1.2 | 3.3 | 0.381 | Biosynthetic Process |
| STAT6 | 1.09 | 1.2 | −1.25 | 3.44 | 0.383 | DNA Binding |
| LTF | 1.28 | 1.4 | −1.47 | 4.02 | 0.384 | Endopeptidase Activity |
| STAT3 | 0.35 | 0.385 | −0.404 | 1.1 | 0.384 | Biopolymer Metabolic Process |
| BCL6 | 0.734 | 0.808 | −0.849 | 2.32 | 0.385 | Intracellular Non-Membrane-Bound Organelle |
| FYN | 0.626 | 0.695 | −0.735 | 1.99 | 0.389 | Behavior |
| IKBKAP | 0.885 | 0.986 | −1.05 | 2.82 | 0.39 | Cytoplasm |
| PPARG | 0.944 | 1.06 | −1.13 | 3.01 | 0.393 | Biopolymer Metabolic Process |
| IFITM1 | 1.26 | 1.42 | −1.52 | 4.05 | 0.395 | Cell Proliferation |
| CD40 | −0.655 | 0.741 | −2.11 | 0.797 | 0.398 | Defense Response |
| CASP3 | 1.03 | 1.17 | −1.26 | 3.33 | 0.398 | Cell Development |
| TAPBP | 0.332 | 0.383 | −0.42 | 1.08 | 0.407 | Cytoplasm |
| IFI16 | 1.09 | 1.27 | −1.4 | 3.58 | 0.411 | Cell Development |
| CD45RB | 0.708 | 0.825 | −0.91 | 2.33 | 0.411 | Integral to Membrane |
| GPR183 | −0.755 | 0.882 | −2.48 | 0.973 | 0.412 | Unknown |
| TAGAP | −0.671 | 0.79 | −2.22 | 0.877 | 0.416 | Rho GTPase Activation |
| ITGB2 | 0.619 | 0.732 | −0.815 | 2.05 | 0.417 | Behavior |
| NFATC2 | 0.97 | 1.15 | −1.28 | 3.22 | 0.418 | Biopolymer Metabolic Process |
| TAP2 | 0.575 | 0.682 | −0.761 | 1.91 | 0.419 | Cytoplasm |
| TBK1 | 1.12 | 1.33 | −1.49 | 3.74 | 0.42 | IκB Kinase NFκB Cascade |
| NCF4 | 0.51 | 0.607 | −0.681 | 1.7 | 0.421 | Cytoplasm |
| PTPN6 | 0.984 | 1.17 | −1.32 | 3.29 | 0.422 | Biopolymer Metabolic Process |
| ILF3 | 1.15 | 1.38 | −1.55 | 3.85 | 0.423 | Biopolymer Metabolic Process |
| CASP2 | 0.999 | 1.2 | −1.35 | 3.34 | 0.423 | Apoptosis |
| CD274 | 0.345 | 0.415 | −0.468 | 1.16 | 0.425 | Cell Proliferation |
| SPP1 | −0.645 | 0.779 | −2.17 | 0.882 | 0.427 | Osteoclast Attachment |
| FCGR1A/B | 0.507 | 0.613 | −0.695 | 1.71 | 0.428 | Establishment of Localization |
| RELA | 0.375 | 0.461 | −0.528 | 1.28 | 0.435 | Cell Development |
| SERPING1 | 1.26 | 1.55 | −1.78 | 4.3 | 0.436 | Regulation of Complement |
| TNFSF10 | 1.13 | 1.41 | −1.64 | 3.9 | 0.441 | Cell Development |
| CSF2RB | 0.579 | 0.732 | −0.856 | 2.01 | 0.447 | Integral to Membrane |
| NFKBIZ | 0.951 | 1.21 | −1.42 | 3.32 | 0.45 | Activation of IL-6 |
| PTK2 | 1.17 | 1.49 | −1.76 | 4.1 | 0.452 | Cell Surface Receptor-Linked Signal Transduction |
| RUNX1 | −0.403 | 0.52 | −1.42 | 0.617 | 0.456 | Biopolymer Metabolic Process |
| CTNNB1 | 1.44 | 1.86 | −2.2 | 5.08 | 0.457 | Cell Development |
| FCGR2B | −0.39 | 0.507 | −1.38 | 0.604 | 0.46 | Immune Response |
| TNFAIP3 | 0.511 | 0.665 | −0.792 | 1.81 | 0.46 | IκB Kinase NFκB Cascade |
| IL1R1 | −1 | 1.32 | −3.58 | 1.58 | 0.463 | Integral to Membrane |
| MAPKAPK2 | −0.436 | 0.573 | −1.56 | 0.687 | 0.464 | Biopolymer Metabolic Process |
| CD209 | 0.649 | 0.854 | −1.03 | 2.32 | 0.465 | Cell–Cell Adhesion |
| MX1 | −0.522 | 0.689 | −1.87 | 0.828 | 0.466 | Apoptosis |
| PSMB7 | 0.242 | 0.321 | −0.386 | 0.871 | 0.467 | Peptide Cleavage |
| ATG7 | 0.881 | 1.17 | −1.42 | 3.18 | 0.47 | Biopolymer Metabolic Process |
| CTSC | 1.31 | 1.74 | −2.11 | 4.72 | 0.47 | Cytoplasm |
| IL18R1 | −0.535 | 0.734 | −1.97 | 0.903 | 0.482 | Membrane |
| CCL5 | −0.467 | 0.648 | −1.74 | 0.803 | 0.487 | Behavior |
| LILRB4 | −0.632 | 0.877 | −2.35 | 1.09 | 0.488 | Antigen Binding |
| IL2RB | 0.594 | 0.83 | −1.03 | 2.22 | 0.491 | Cell Development |
| PSMB5 | −0.26 | 0.364 | −0.973 | 0.453 | 0.491 | Peptide Cleavage |
| CD46 | 1.35 | 1.9 | −2.37 | 5.08 | 0.492 | Integral to Membrane |
| C1QB | 1.2 | 1.7 | −2.12 | 4.53 | 0.494 | Extracellular Region |
| C14orf166 | 1.11 | 1.58 | −1.98 | 4.2 | 0.499 | Identical Protein Binding |
| FCGR2A/C | 1.08 | 1.59 | −2.03 | 4.19 | 0.513 | Phagocyte Cell Surface Receptor |
| LCP2 | 0.465 | 0.687 | −0.881 | 1.81 | 0.514 | Cell Surface Receptor-Linked Signal Transduction |
| EGR1 | −0.499 | 0.746 | −1.96 | 0.962 | 0.519 | Transcriptional Regulation |
| CD28 | −0.393 | 0.598 | −1.56 | 0.779 | 0.526 | Cell Development |
| TRAF2 | −0.126 | 0.194 | −0.506 | 0.253 | 0.528 | Macromolecular Complex Assembly |
| NOD2 | 0.524 | 0.806 | −1.06 | 2.1 | 0.531 | Cytoplasm |
| TLR1 | −0.302 | 0.468 | −1.22 | 0.616 | 0.534 | Biosynthetic Process |
| SMAD5 | 0.762 | 1.19 | −1.58 | 3.1 | 0.538 | Cell Surface Receptor-Linked Signal Transduction |
| PML | 0.387 | 0.607 | −0.803 | 1.58 | 0.538 | Cell Fraction |
| CXCR4 | 0.485 | 0.764 | −1.01 | 1.98 | 0.54 | Cell Development |
| IRF1 | −0.178 | 0.283 | −0.732 | 0.376 | 0.542 | Biopolymer Metabolic Process |
| LGALS3 | 1.02 | 1.63 | −2.17 | 4.2 | 0.545 | Carbohydrate Binding |
| ENTPD1 | −0.483 | 0.777 | −2.01 | 1.04 | 0.548 | Hemostasis |
| ICOSLG | −0.415 | 0.67 | −1.73 | 0.898 | 0.55 | Cell Activation |
| BCL2 | 0.496 | 0.801 | −1.07 | 2.06 | 0.55 | Cytoplasm |
| STAT2 | 0.804 | 1.3 | −1.74 | 3.35 | 0.55 | Biopolymer Metabolic Process |
| CD86 | −0.478 | 0.773 | −1.99 | 1.04 | 0.55 | Cell Proliferation |
| CD276 | 0.844 | 1.38 | −1.86 | 3.54 | 0.554 | Biosynthetic Process |
| MAF | 0.342 | 0.562 | −0.759 | 1.44 | 0.556 | Biopolymer Metabolic Process |
| IFIT2 | −0.568 | 0.944 | −2.42 | 1.28 | 0.56 | Innate Immune |
| CD14 | 0.893 | 1.49 | −2.02 | 3.81 | 0.561 | Apoptosis |
| CD81 | 1.08 | 1.8 | −2.45 | 4.61 | 0.562 | Integral to Membrane |
| ITGA5 | −0.459 | 0.784 | −2 | 1.08 | 0.571 | Integral to Membrane |
| DPP4 | 0.884 | 1.51 | −2.08 | 3.84 | 0.571 | Immune Response |
| CSF1R | −0.326 | 0.564 | −1.43 | 0.78 | 0.577 | Cell Proliferation |
| IRF3 | 0.227 | 0.393 | −0.544 | 0.997 | 0.577 | Biopolymer Metabolic Process |
| JAK2 | 0.736 | 1.29 | −1.79 | 3.26 | 0.581 | Anatomical Structure Development |
| ICAM1 | 0.383 | 0.673 | −0.936 | 1.7 | 0.581 | Integral to Membrane |
| FKBP5 | −0.396 | 0.697 | −1.76 | 0.969 | 0.582 | Cellular Macromolecule Metabolic Process |
| TNFSF12 | 0.344 | 0.608 | −0.847 | 1.54 | 0.583 | Cell Development |
| MRC1 | 0.841 | 1.5 | −2.09 | 3.77 | 0.587 | Carbohydrate Binding |
| SYK | 0.343 | 0.612 | −0.856 | 1.54 | 0.587 | Anatomical Structure Morphogenesis |
| RELB | 0.316 | 0.564 | −0.79 | 1.42 | 0.588 | DNA Binding |
| IRF5 | 0.369 | 0.666 | −0.935 | 1.67 | 0.591 | Immune Transcription Factor |
| IRF8 | 0.368 | 0.681 | −0.967 | 1.7 | 0.601 | Biopolymer Metabolic Process |
| SKI | 0.684 | 1.27 | −1.8 | 3.17 | 0.602 | Repressor of TGF-β |
| C3 | 0.517 | 0.96 | −1.37 | 2.4 | 0.602 | Cell Surface Receptor-Linked Signal Transduction |
| PTGS2 | −0.508 | 0.945 | −2.36 | 1.34 | 0.603 | Cytoplasm |
| LITAF | 0.354 | 0.659 | −0.938 | 1.65 | 0.603 | Biopolymer Metabolic Process |
| BLNK | −0.312 | 0.586 | −1.46 | 0.836 | 0.606 | Anatomical Structure Development |
| IFNAR2 | 0.174 | 0.326 | −0.466 | 0.813 | 0.607 | Cell Surface Receptor-Linked Signal Transduction |
| MUC1 | 0.935 | 1.79 | −2.57 | 4.44 | 0.613 | Integral to Membrane |
| NOD1 | −0.62 | 1.2 | −2.97 | 1.73 | 0.616 | Biosynthetic Process |
| PDCD2 | 0.275 | 0.534 | −0.772 | 1.32 | 0.618 | Apoptosis |
| CD82 | −0.326 | 0.638 | −1.58 | 0.925 | 0.62 | Integral to Membrane |
| NFIL3 | 0.593 | 1.18 | −1.72 | 2.91 | 0.626 | Biopolymer Metabolic Process |
| TCF7 | 0.363 | 0.736 | −1.08 | 1.81 | 0.633 | Biopolymer Metabolic Process |
| ATG10 | −0.576 | 1.18 | −2.88 | 1.73 | 0.635 | Autophagocytosis |
| LILRB1 | 0.405 | 0.838 | −1.24 | 2.05 | 0.639 | Integral to Membrane |
| FCGRT | 0.757 | 1.58 | −2.33 | 3.85 | 0.641 | Immune Response |
| ICAM3 | −0.32 | 0.673 | −1.64 | 0.999 | 0.645 | Integral to Membrane |
| STAT1 | 0.33 | 0.695 | −1.03 | 1.69 | 0.645 | Biopolymer Metabolic Process |
| IL6ST | 0.905 | 1.91 | −2.84 | 4.65 | 0.645 | Cell Surface Receptor-Linked Signal Transduction |
| PDGFRB | −0.863 | 1.85 | −4.48 | 2.76 | 0.65 | Phosphotransferase Activity Alcohol Group as Acceptor |
| CSF1 | 0.335 | 0.722 | −1.08 | 1.75 | 0.653 | Cell Proliferation |
| IL1RAP | 0.358 | 0.782 | −1.17 | 1.89 | 0.657 | Cellular Component Assembly |
| MCL1 | 0.13 | 0.288 | −0.434 | 0.695 | 0.66 | Cell Development |
| NOTCH2 | 0.332 | 0.744 | −1.13 | 1.79 | 0.665 | Cell Development |
| IFNGR1 | 0.755 | 1.71 | −2.59 | 4.1 | 0.668 | Integral to Membrane |
| NFATC1 | −0.346 | 0.782 | −1.88 | 1.19 | 0.668 | Biopolymer Metabolic Process |
| SMAD3 | −0.262 | 0.594 | −1.43 | 0.902 | 0.668 | Macromolecular Complex |
| STAT4 | −0.358 | 0.812 | −1.95 | 1.23 | 0.669 | DNA Binding |
| C1S | −0.607 | 1.39 | −3.33 | 2.11 | 0.671 | Endopeptidase Activity |
| CX3CR1 | 0.364 | 0.859 | −1.32 | 2.05 | 0.681 | Behavior |
| LTB4R | 0.322 | 0.77 | −1.19 | 1.83 | 0.685 | Cell Surface Receptor-Linked Signal Transduction |
| ARHGDIB | 0.307 | 0.741 | −1.15 | 1.76 | 0.687 | Cytoplasm |
| JAK3 | 0.239 | 0.59 | −0.917 | 1.4 | 0.693 | Biopolymer Metabolic Process |
| TLR8 | 0.301 | 0.749 | −1.17 | 1.77 | 0.696 | Biosynthetic Process |
| RAF1 | 0.533 | 1.33 | −2.07 | 3.14 | 0.697 | Biopolymer Metabolic Process |
| CSF3R | 0.22 | 0.556 | −0.87 | 1.31 | 0.701 | Defense Response |
| SIGIRR | 0.272 | 0.693 | −1.09 | 1.63 | 0.703 | Membrane |
| ATG16L1 | −0.436 | 1.13 | −2.66 | 1.79 | 0.709 | Autophagy |
| SOCS1 | −0.553 | 1.46 | −3.41 | 2.3 | 0.712 | Biopolymer Metabolic Process |
| POU2F2 | 0.26 | 0.694 | −1.1 | 1.62 | 0.715 | Biopolymer Metabolic Process |
| HLA-DMB | −0.311 | 0.839 | −1.96 | 1.33 | 0.719 | Antigen Presentation |
| MAP4K2 | −0.52 | 1.41 | −3.28 | 2.24 | 0.72 | Biopolymer Metabolic Process |
| IFIH1 | 0.186 | 0.509 | −0.812 | 1.18 | 0.722 | B-Cell Differentiation |
| TGFBR1 | 0.5 | 1.38 | −2.21 | 3.21 | 0.726 | Biopolymer Metabolic Process |
| B2M | −0.212 | 0.59 | −1.37 | 0.944 | 0.726 | Antimicrobial Protein |
| STAT5A | −0.286 | 0.804 | −1.86 | 1.29 | 0.729 | DNA Binding |
| IGF2R | 0.436 | 1.27 | −2.05 | 2.92 | 0.738 | Cytoplasm |
| CD34 | −0.175 | 0.516 | −1.19 | 0.836 | 0.741 | Carbohydrate Binding |
| ITGB1 | −0.191 | 0.563 | −1.29 | 0.912 | 0.741 | Cell–Cell Adhesion |
| TLR3 | −0.329 | 0.974 | −2.24 | 1.58 | 0.742 | Biosynthetic Process |
| CCL13 | −0.311 | 0.926 | −2.13 | 1.5 | 0.744 | Behavior |
| LAMP3 | 0.248 | 0.739 | −1.2 | 1.7 | 0.744 | Cell Proliferation |
| CCBP2 | −0.174 | 0.522 | −1.2 | 0.85 | 0.746 | Behavior |
| IDO1 | 0.261 | 0.787 | −1.28 | 1.8 | 0.747 | Tryptophan Catabolism |
| MME | 0.244 | 0.739 | −1.2 | 1.69 | 0.748 | Cell–Cell Signaling |
| MSR1 | 0.487 | 1.48 | −2.4 | 3.38 | 0.748 | Establishment of Localization |
| C7 | −0.292 | 0.908 | −2.07 | 1.49 | 0.754 | Integral to Membrane |
| CD36 | 0.603 | 1.88 | −3.09 | 4.3 | 0.755 | Cell Fraction |
| IL16 | −0.147 | 0.462 | −1.05 | 0.759 | 0.757 | Extracellular Region |
| CISH | −0.232 | 0.733 | −1.67 | 1.21 | 0.759 | Suppressor of Cytokine Signaling |
| CCL2 | 0.256 | 0.827 | −1.37 | 1.88 | 0.763 | Biopolymer Metabolic Process |
| CD163 | −0.265 | 0.886 | −2 | 1.47 | 0.771 | Integral to Membrane |
| STAT5B | 0.502 | 1.69 | −2.8 | 3.81 | 0.772 | DNA Binding |
| SLC2A1 | −0.123 | 0.419 | −0.944 | 0.698 | 0.776 | Cell Fraction |
| IRAK4 | −0.372 | 1.29 | −2.91 | 2.16 | 0.779 | Activates NFκB |
| DUSP4 | 0.203 | 0.708 | −1.18 | 1.59 | 0.78 | Biopolymer Metabolic Process |
| CEBPB | −0.158 | 0.553 | −1.24 | 0.925 | 0.78 | Biopolymer Metabolic Process |
| ITGA4 | 0.213 | 0.748 | −1.25 | 1.68 | 0.782 | Identical Protein Binding |
| CTSS | 0.22 | 0.819 | −1.39 | 1.83 | 0.794 | Cellular Macromolecule Metabolic Process |
| IKZF2 | −0.362 | 1.35 | −3.01 | 2.28 | 0.794 | Lymphocyte Development |
| LY96 | 0.189 | 0.711 | −1.2 | 1.58 | 0.796 | Cell Surface Receptor-Linked Signal Transduction |
| CLEC7A | 0.214 | 0.812 | −1.38 | 1.81 | 0.797 | Cell Activation |
| HAVCR2 | −0.207 | 0.787 | −1.75 | 1.34 | 0.798 | Th1 Surface Protein |
| ICAM2 | −0.388 | 1.48 | −3.29 | 2.51 | 0.798 | Integral to Membrane |
| PSMB8 | 0.354 | 1.35 | −2.3 | 3 | 0.799 | Antigen Presentation |
| C1R | −0.243 | 0.945 | −2.09 | 1.61 | 0.802 | Endopeptidase Activity |
| ABL1 | −0.375 | 1.48 | −3.27 | 2.52 | 0.805 | Biopolymer Metabolic Process |
| TLR5 | −0.117 | 0.466 | −1.03 | 0.796 | 0.807 | Innate Immunity |
| BST2 | −0.406 | 1.64 | −3.63 | 2.81 | 0.81 | IκB Kinase NFκB Cascade |
| IL6R | 0.159 | 0.653 | −1.12 | 1.44 | 0.813 | Cell Surface Receptor-Linked Signal Transduction |
| TMEM173 | 0.139 | 0.642 | −1.12 | 1.4 | 0.833 | Innate Immunity |
| IL10RA | −0.18 | 0.835 | −1.82 | 1.46 | 0.833 | Interleukin Binding |
| CDH5 | −0.401 | 1.9 | −4.13 | 3.33 | 0.837 | Cell–Cell Adhesion |
| PSMB10 | 0.273 | 1.31 | −2.3 | 2.85 | 0.839 | Humoral Immune Response |
| NFATC3 | 0.257 | 1.24 | −2.17 | 2.68 | 0.84 | Biopolymer Metabolic Process |
| BCL2L11 | 0.108 | 0.551 | −0.972 | 1.19 | 0.849 | Apoptosis |
| EDNRB | −0.308 | 1.62 | −3.49 | 2.87 | 0.853 | Integral to Membrane |
| TICAM1 | 0.119 | 0.632 | −1.12 | 1.36 | 0.854 | IκB Kinase NFκB Cascade |
| JAK1 | −0.286 | 1.56 | −3.35 | 2.77 | 0.858 | Interferon Signal Transduction |
| MAP4K1 | 0.115 | 0.632 | −1.12 | 1.35 | 0.859 | Biopolymer Metabolic Process |
| C1QBP | −0.0783 | 0.452 | −0.964 | 0.807 | 0.866 | Immune Response |
| CD97 | 0.302 | 1.76 | −3.15 | 3.75 | 0.867 | Cell–Cell Signaling |
| CMKLR1 | −0.271 | 1.6 | −3.41 | 2.86 | 0.869 | Behavior |
| ABCB1 | −0.109 | 0.655 | −1.39 | 1.17 | 0.871 | Cell Fraction |
| ITGA6 | −0.0569 | 0.384 | −0.81 | 0.696 | 0.885 | Cellular Component Assembly |
| CFI | −0.123 | 0.832 | −1.75 | 1.51 | 0.885 | Endopeptidase Activity |
| TOLLIP | −0.227 | 1.55 | −3.27 | 2.81 | 0.886 | Cell–Cell Signaling |
| CFH | −0.144 | 1.02 | −2.14 | 1.85 | 0.89 | Extracellular Region |
| NFKB1 | −0.177 | 1.26 | −2.65 | 2.3 | 0.891 | Biopolymer Metabolic Process |
| FN1 | −0.0987 | 0.729 | −1.53 | 1.33 | 0.895 | Cytoplasm |
| IRAK3 | 0.114 | 0.846 | −1.54 | 1.77 | 0.896 | Biopolymer Metabolic Process |
| CXCR6 | 0.0995 | 0.75 | −1.37 | 1.57 | 0.897 | Cell Surface Receptor-Linked Signal Transduction |
| TCF4 | 0.0836 | 0.707 | −1.3 | 1.47 | 0.908 | Biopolymer Metabolic Process |
| LILRB5 | 0.0831 | 0.747 | −1.38 | 1.55 | 0.914 | Cell Surface Receptor-Linked Signal Transduction |
| IKBKB | 0.0595 | 0.55 | −1.02 | 1.14 | 0.916 | Activates NFκB |
| IKBKE | 0.0559 | 0.578 | −1.08 | 1.19 | 0.925 | Biopolymer Metabolic Process |
| CD19 | 0.126 | 1.36 | −2.54 | 2.79 | 0.928 | Cell Surface Receptor-Linked Signal Transduction |
| IRAK1 | −0.119 | 1.39 | −2.85 | 2.61 | 0.934 | Cellular Component Assembly |
| UBE2L3 | −0.112 | 1.49 | −3.03 | 2.8 | 0.942 | Biopolymer Metabolic Process |
| CD53 | 0.126 | 1.73 | −3.26 | 3.52 | 0.943 | Membrane |
| TRAF4 | −0.1 | 1.41 | −2.87 | 2.67 | 0.945 | DNA Binding |
| THY1 | −0.0637 | 0.979 | −1.98 | 1.86 | 0.949 | Cell Surface |
| ATG5 | −0.108 | 1.75 | −3.53 | 3.31 | 0.952 | Cytoplasm |
| CEACAM1 | 0.0489 | 0.824 | −1.57 | 1.66 | 0.954 | Cell Fraction |
| CCND3 | 0.0844 | 1.55 | −2.96 | 3.13 | 0.958 | Biopolymer Metabolic Process |
| MAPK1 | −0.0932 | 1.94 | −3.89 | 3.7 | 0.963 | Behavior |
| CD164 | −0.0906 | 1.98 | −3.96 | 3.78 | 0.964 | Cell–Cell Adhesion |
| NOTCH1 | 0.03 | 0.657 | −1.26 | 1.32 | 0.965 | Cell Development |
| CRADD | −0.0272 | 0.617 | −1.24 | 1.18 | 0.966 | Apoptosis |
| TP53 | −0.0682 | 1.76 | −3.52 | 3.38 | 0.97 | Cell Fraction |
| BAX | 0.0666 | 1.81 | −3.47 | 3.61 | 0.971 | Cytoplasm |
| CASP1 | 0.0524 | 1.43 | −2.75 | 2.86 | 0.971 | Cellular Protein Metabolic Process |
| IKBKG | −0.0416 | 1.19 | −2.37 | 2.28 | 0.973 | Cell Development |
| TYK2 | 0.0467 | 1.37 | −2.63 | 2.73 | 0.973 | Biopolymer Metabolic Process |
| CLEC4E | −0.0351 | 1.08 | −2.16 | 2.09 | 0.975 | Carbohydrate Binding |
| CFB | 0.0283 | 0.901 | −1.74 | 1.79 | 0.976 | Complement Activation |
| LAIR1 | −0.0191 | 0.739 | −1.47 | 1.43 | 0.98 | Inhibitory Receptor |
| CD58 | −0.0354 | 1.4 | −2.79 | 2.72 | 0.98 | T Cell Activation |
| KCNJ2 | 0.00799 | 0.384 | −0.744 | 0.76 | 0.984 | Establishment of Localization |
| PLAU | −0.016 | 0.788 | −1.56 | 1.53 | 0.984 | Behavior |
| TRAF3 | 0.0112 | 0.57 | −1.11 | 1.13 | 0.985 | Apoptosis |
| CCR1 | 0.0271 | 1.38 | −2.68 | 2.74 | 0.985 | Cell–Cell Signaling |
| CD9 | −0.0138 | 0.765 | −1.51 | 1.48 | 0.986 | Anatomical Structure Morphogenesis |
| APP | −0.00668 | 0.389 | −0.769 | 0.756 | 0.987 | Cell Surface |
| ARG2 | 0.0106 | 0.761 | −1.48 | 1.5 | 0.989 | Cytoplasm |
| IL4R | 0.0159 | 1.64 | −3.21 | 3.24 | 0.992 | Immune Response |
| CD4 | 0.0114 | 1.48 | −2.88 | 2.91 | 0.994 | Cell Activation |
| CYBB | 0.00269 | 0.554 | −1.08 | 1.09 | 0.996 | Defense Response |
| KIT | −4.48 × 10 −16 | 0.576 | −1.13 | 1.13 | 1 | Phosphotransferase Activity Alcohol Group as Acceptor |
References
- Drake, P.; Driscoll, A.K.; Mathews, T.J. Cigarette Smoking During Pregnancy; NCHS Data Brief: Hyattsville, MD, USA, 2018; pp. 1–8. [Google Scholar]
- Spencer, K.; Cowans, N.J. Accuracy of self-reported smoking status in first trimester aneuploidy screening. Prenat. Diagn. 2013, 33, 245–250. [Google Scholar] [CrossRef] [PubMed]
- Kyrklund-Blomberg, N.B.; Cnattingius, S. Preterm birth and maternal smoking: Risks related to gestational age and onset of delivery. J. Obstet. Gynaecol. 1998, 179, 1051–1055. [Google Scholar] [CrossRef]
- Nicoletti, D. Maternal smoking during pregnancy and birth defects in children: A systematic review with meta-analysis. Cad. Saude Publica 2014, 30, 2491–2529. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hackshaw, A.; Rodeck, C.; Boniface, S. Maternal smoking in pregnancy and birth defects: A systematic review based on 173 687 malformed cases and 11.7 million controls. Hum. Reprod. Update 2011, 17, 589–604. [Google Scholar] [CrossRef] [Green Version]
- Antonucci, R.; Contu, P.; Porcella, A.; Atzeni, C.; Chiappe, S. Intrauterine smoke exposure: A new risk factor for bronchopulmonary dysplasia? J. Perinat. Med. 2004, 32, 272–277. [Google Scholar] [CrossRef]
- Jensen, E.A.; Schmidt, B. Epidemiology of bronchopulmonary dysplasia. Birth Defects Res. Part A Clin. Mol. Teratol. 2014, 100, 145–157. [Google Scholar] [CrossRef]
- Morrow, L.A.; Wagner, B.D.; Ingram, D.A.; Poindexter, B.B.; Schibler, K.; Cotten, C.M.; Dagle, J.; Sontag, M.K.; Mourani, P.M.; Abman, S.H. Antenatal Determinants of Bronchopulmonary Dysplasia and Late Respiratory Disease in Preterm Infants. Am. J. Respir. Crit. Care Med. 2017, 196, 364–374. [Google Scholar] [CrossRef] [Green Version]
- Watterberg, K.L.; Demers, L.M.; Scott, S.M.; Murphy, S. Chorioamnionitis and Early Lung Inflammation in Infants in Whom Bronchopulmonary Dysplasia Develops. Pediatrics 1996, 97, 210–215. [Google Scholar] [CrossRef]
- Hansen, A.R.; Barnés, C.M.; Folkman, J.; McElrath, T.F. Maternal Preeclampsia Predicts the Development of Bronchopulmonary Dysplasia. J. Pediatrics 2010, 156, 532–536. [Google Scholar] [CrossRef]
- Eriksson, L.; Haglund, B.; Odlind, V.; Altman, M.; Ewald, U.; Kieler, H. Perinatal conditions related to growth restriction and inflammation are associated with an increased risk of bronchopulmonary dysplasia. Acta Paediatr. 2015, 104, 259–263. [Google Scholar] [CrossRef]
- Gemmell, L.; Martin, L.; Murphy, K.E.; Modi, N.; Håkansson, S.; Reichman, B.; Lui, K.; Kusuda, S.; Sjörs, G.; Mirea, L.; et al. Hypertensive disorders of pregnancy and outcomes of preterm infants of 24 to 28 weeks’ gestation. J. Perinatol. 2016, 36, 1067–1072. [Google Scholar] [CrossRef] [PubMed]
- Xu, S.; Venge, P. Lipocalins as biochemical markers of disease. Biochim. Biophys. Acta (BBA)-Protein Struct. Mol. Enzymol. 2000, 1482, 298–307. [Google Scholar] [CrossRef]
- Inoue, H.; Ohga, S.; Kusuda, T.; Kitajima, J.; Kinjo, T.; Ochiai, M.; Takahata, Y.; Honjo, S.; Hara, T. Serum neutrophil gelatinase-associated lipocalin as a predictor of the development of bronchopulmonary dysplasia in preterm infants. Early Hum. Dev 2013, 89, 425–429. [Google Scholar] [CrossRef] [PubMed]
- Naeye, R.L. Effects of maternal cigarette smoking on the fetus and placenta. BJOG. Int. J. Obstet. 1978, 85, 732–737. [Google Scholar] [CrossRef]
- Jobe, A.H. Mechanisms of lung injury and bronchopulmonary dysplasia. Am. J. Perinatol. 2016, 33, 1076–1078. [Google Scholar] [CrossRef]
- Gonzalez-Luis, G.E.; Westering-Kroon, E.V.; Villamor-Martinez, E.; Huizing, M.J.; Kilani, M.A.; Kramer, B.W.; Villamor, E. Tobacco smoking during pregnancy is associated with increased risk of moderate/severe bronchopulmonary dysplasia: A systematic review and Meta-Analysis. Front. Pediatrics 2020, 8, 160. [Google Scholar] [CrossRef]
- Gibbs, K.; Collaco, J.M.; McGrath-Morrow, S.A. Impact of tobacco smoke and nicotine exposure on lung development. Chest 2016, 149, 552–561. [Google Scholar] [CrossRef] [Green Version]
- Been, J.V.; Millett, C. Reducing the global burden of preterm births. Lancet Glob. Health 2019, 7, 414. [Google Scholar] [CrossRef] [Green Version]
- Wagijo, M.A.; Sheikh, A.; Duijts, L.; Been, J.V. Reducing tobacco smoking and smoke exposure to prevent preterm birth and its complications. Paediatr. Respir. 2017, 22, 3–10. [Google Scholar] [CrossRef]
- Lauren Comarda, J.E. Maternal Tobacco Exposure Leads to Cytokine Dysregulation in Placental Membranes Stimulated with Lipopolysaccharide. In Proceedings of the Pediatric Academic Society, Toronto, ON, Canada, 18 September 2018; pp. 397–412. [Google Scholar]
- Jobe, A.H.; Bancalari, E. Bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 2001, 163, 1723–1729. [Google Scholar] [CrossRef]
- Fajardy, I.; Moitrot, E.; Vambergue, A.; Vandersippe-Millot, M.; Deruelle, P.; Rousseaux, J. Time course analysis of RNA stability in human placenta. BMC Mol. Biol. 2009, 10, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davidson, L.M.; Berkelhamer, S.K. Bronchopulmonary Dysplasia: Chronic Lung Disease of Infancy and Long-Term Pulmonary Outcomes. J. Clin. Med. 2017, 6, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheong, J.L.Y.; Doyle, L.W. An update on pulmonary and neurodevelopmental outcomes of bronchopulmonary dysplasia. Semin. Perinatol. 2018, 42, 478–484. [Google Scholar] [CrossRef] [PubMed]
- Tadesse, S.; Luo, G.; Park, J.S.; Kim, B.J.; Snegovskikh, V.V.; Zheng, T.; Hodgson, E.J.; Arcuri, F.; Toti, P.; Parikh, C.R.; et al. Intra-amniotic infection upregulates neutrophil gelatinase-associated lipocalin (NGAL) expression at the maternal-fetal interface at term: Implications for infection-related preterm birth. Reprod. Sci. 2011, 18, 713–722. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.; Taneja, V.; Vassallo, R. Cigarette smoking and inflammation: Cellular and molecular mechanisms. J. Dent. Res. 2012, 91, 142–149. [Google Scholar] [CrossRef] [Green Version]
- Gonçalves, R.B.; Coletta, R.D.; Silvério, K.G.; Benevides, L.; Casati, M.Z.; da Silva, J.S.; Nociti, F.H. Impact of smoking on inflammation: Overview of molecular mechanisms. Inflamm. Res. 2011, 60, 409–424. [Google Scholar] [CrossRef]
- Yoon, B.H.; Romero, R.; Jun, J.K.; Park, K.H.; Park, J.D.; Ghezzi, F.; Kim, B.I. Amniotic fluid cytokines (interleukin-6, tumor necrosis factor-alpha, interleukin-1 beta, and interleukin-8) and the risk for the development of bronchopulmonary dysplasia. Am. J. Obstet. Gynecol. 1997, 177, 825–830. [Google Scholar] [CrossRef]
- Shimoya, K.; Moriyama, A.; Matsuzaki, N.; Ogata, I.; Koyama, M.; Azuma, C.; Saji, F.; Murata, Y. Human placental cells show enhanced production of interleukin (IL)-8 in response to lipopolysaccharide (LPS), IL-1 and tumour necrosis factor (TNF)-alpha, but not to IL-6. Mol. Hum. Reprod. 1999, 5, 885. [Google Scholar] [CrossRef]
- Nair, R.R.; Khanna, A.; Singh, K. Role of inflammatory proteins S100A8 and S100A9 in pathophysiology of recurrent early pregnancy loss. Placenta 2013, 34, 824–827. [Google Scholar] [CrossRef]
- Isayama, T.; Shah, P.S.; Ye, X.Y.; Dunn, M.; Da Silva, O.; Alvaro, R.; Lee, S.K. Adverse Impact of Maternal Cigarette Smoking on Preterm Infants: A Population-Based Cohort Study. Am. J. Perinatol. 2015, 32, 1105–1111. [Google Scholar] [CrossRef]
- Spinillo, A.; Ometto, A.; Stronati, M.; Piazzi, G.; Iasci, A.; Rondini, G. Epidemiologic association between maternal smoking during pregnancy and intracranial hemorrhage in preterm infants. J. Pediatrics 1995, 127, 472–478. [Google Scholar] [CrossRef]


| Tobacco Exposure | ||||
|---|---|---|---|---|
| No | Yes | |||
| (n = 22) | (n = 17) | Total (n = 39) | p Value | |
| Birth weight, g (SD) | 1.141 (458) | 1.125 (464) | 1.134 (454) | >0.9 |
| Birth length, cm (SD) | 36.3 (4.9) | 36.6 (4.6) | 36.5 (4.7) | 0.9 |
| Head circumference, cm (SD) | 25.56 (2.87) | 25.48 (3.25) | 25.53 (3.00) | >0.9 |
| Gestational age, wk (SD) | 28.76 (2.64) | 28.40 (2.68) | 28.60 (2.63) | 0.5 |
| Maternal age, yr (SD) | 25.7 (4.9) | 29.8 (6.6) | 27.5 (6.0) | 0.048 |
| Sex | 0.4 | |||
| F | 17 (77%) | 10 (59%) | 27 (69%) | |
| M | 5(23%) | 7(41%) | 12(31%) | |
| Maternal ethnicity | 0.4 | |||
| Black | 5 (23%) | 3 (18%) | 8 (21%) | |
| Black, Native American | 0 (0%) | 1 (5.9%) | 1 (2.6%) | |
| Hispanic | 6 (27%) | 2 (12%) | 8 (21%) | |
| Latino, White | 1 (4.5%) | 0 (0.0%) | 1 (2.6%) | |
| Native American | 1 (4.5%) | 3 (18%) | 4 (10%) | |
| White | 9 (41%) | 7 (41%) | 16 (41%) | |
| White, Native American | 0 (0%) | 1 (5.9%) | 1 (2.6%) | |
| Antenatal steroid, yes | 9 (41%) | 9 (53%) | 18 (46%) | 0.4 |
| Mode of delivery, C-Section | 11 (50%) | 10 (59%) | 21 (54%) | 0.8 |
| Intubated in delivery room, yes | 9 (41%) | 9 (53%) | 18 (46%) | 0.7 |
| Intubated in NICU, yes | 7 (32%) | 4 (24%) | 11 (28%) | 0.7 |
| PDA medical treatment, yes | 9 (41%) | 2 (12%) | 11 (28%) | 0.073 |
| PDA surgical treatment, yes | 1 (4.5%) | 0 (0%) | 1 (2.6%) | >0.9 |
| IVH grade 3 or 4, yes | 2 (9.1%) | 1 (5.9%) | 3 (7.7%) | >0.9 |
| Threshold ROP, yes | 3 (14%) | 1 (5.9%) | 4 (10%) | 0.6 |
| IUGR <10th percentile, yes | 3 (14%) | 0 (0%) | 3 (7.7%) | 0.2 |
| Death or BPD, yes | 15 (38%) | 9 (41%) | 6 (35%) | >0.9 |
| Tobacco Exposure | ||||
|---|---|---|---|---|
| No | Yes | |||
| (n = 22) | (n = 17) | Total (n = 39) | p Value | |
| Maternal diabetes, yes | 3 (14%) | 2 (12%) | 5 (13%) | >0.9 |
| Maternal hypertension, yes | 3 (14%) | 2 (12%) | 5 (13%) | >0.9 |
| Prolonged rupture of membranes (>18h), yes | 4 (18%) | 3 (18%) | 7 (18%) | >0.9 |
| Chorioamnionitis, yes | 10 (45%) | 10 (59%) | 20 (51%) | 0.6 |
| Antepartum hemorrhage, yes | 4 (18%) | 4 (24%) | 8 (21%) | 0.7 |
| Marijuana use, yes | 1 (4.5%) | 1 (5.9%) | 2 (5.1%) | 0.4 |
| Illicit drugs, yes | 0 (0%) | 2 (12%) | 2 (5.1%) | 0.4 |
| Gene | Annotation | Log2-Fold Change | SE | p | Tentative Function |
|---|---|---|---|---|---|
| IL8 | Interleukin 8 | 4.77 | 0.898 | 0.00034 | Neutrophil Chemotaxis |
| S100A9 | S100 Calcium-Binding Protein A9 | 1.72 | 0.339 | 0.000477 | Leukocyte Activation |
| S100A8 | S100 Calcium-Binding Protein A8 | 3.33 | 0.912 | 0.00447 | Leukocyte Activation |
| IL1RL1 | Interleukin 1 Receptor Like 1 | −3.41 | 1.1 | 0.0115 | IL-33 Receptor/Inflammatory Signaling |
| CXCL10 | C-X-C Motif Chemokine Ligand 10 | 3.06 | 1.09 | 0.0187 | Peripheral Immune Cell Activation |
| CD44 | CD44 Molecule | 1.7 | 0.614 | 0.02 | Cell–Cell Signaling |
| TNFRSF10C | TNF Receptor Superfamily Member 10c | 1.53 | 0.562 | 0.0212 | Anti-Apoptosis |
| PLAUR | Plasminogen Activator, Urokinase Receptor | 1.78 | 0.676 | 0.0251 | Plasminogen Activation/Extracellular Matrix Degradation |
| IRF7 | Interferon Regulatory Factor 7 | 1.08 | 0.415 | 0.0261 | Anti-viral Immune Response |
| MALT1 | MALT1 Paracaspase | −0.572 | 0.22 | 0.0263 | NF-κB Activation |
| LILRB3 | Leukocyte Immunoglobulin-Like Receptor B3 | 2.04 | 0.795 | 0.0281 | Anti-B Cell Activation |
| HLA-DRB1 | Major Histocompatibility Complex, Class II, DR Beta 1 | 2.74 | 1.14 | 0.0374 | Antigen Presentation |
| HLA-DRB3 | Major Histocompatibility Complex, Class II, DR Beta 3 | 1.78 | 0.746 | 0.0384 | Antigen Presentation |
| HFE | Homeostatic Iron Regulator | −1.25 | 0.529 | 0.0394 | Regulates Iron Absorption |
| TNFSF15 | TNF Superfamily Member 15 | −1.43 | 0.604 | 0.0397 | Endothelial Inflammatory Signaling |
| CD99 | CD99 Molecule | 1.12 | 0.475 | 0.0406 | Leukocyte Migration |
| PTPRC | Protein Tyrosine Phosphatase Receptor Type C | 1.94 | 0.847 | 0.045 | T Cell Activation |
| PTAFR | Platelet-Activating Factor Receptor | −2 | 0.881 | 0.0466 | Receptor for Inflammatory PAF |
| ZBTB16 | Zinc Finger- and BTB Domain-Containing 16 | −2.01 | 0.888 | 0.0469 | Transcription Repression/Myeloid Maturation |
| PLA2G2A | Phospholipase A2 Group IIA | −2.25 | 0.997 | 0.0479 | Phospholipid Metabolism |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Box, D.M.; Makkar, A.; Yu, Z.; Chaaban, H.; Tran, H.H.; Burge, K.Y.; Eckert, J.V. Placental Neutrophil Infiltration Associated with Tobacco Exposure but Not Development of Bronchopulmonary Dysplasia. Children 2022, 9, 381. https://doi.org/10.3390/children9030381
Box DM, Makkar A, Yu Z, Chaaban H, Tran HH, Burge KY, Eckert JV. Placental Neutrophil Infiltration Associated with Tobacco Exposure but Not Development of Bronchopulmonary Dysplasia. Children. 2022; 9(3):381. https://doi.org/10.3390/children9030381
Chicago/Turabian StyleBox, David M., Abhishek Makkar, Zhongxin Yu, Hala Chaaban, Henry H. Tran, Kathryn Y. Burge, and Jeffrey V. Eckert. 2022. "Placental Neutrophil Infiltration Associated with Tobacco Exposure but Not Development of Bronchopulmonary Dysplasia" Children 9, no. 3: 381. https://doi.org/10.3390/children9030381





