Carbon Dioxide Reactivity of Brain Tissue Oxygenation after Pediatric Traumatic Brain Injury
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patients
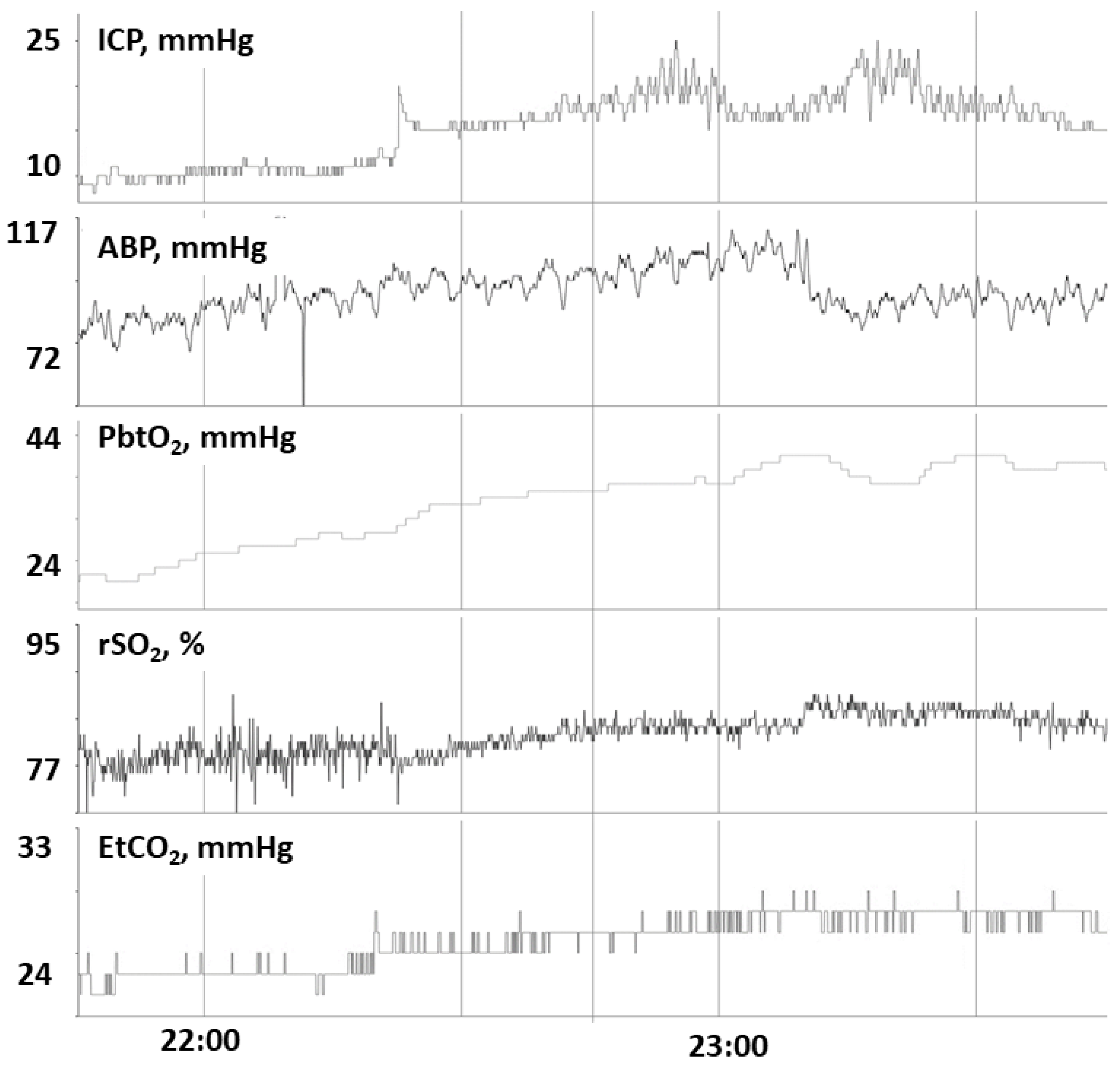
2.3. Physiologic Data
2.4. Pharmacologic Data
2.5. Statistical Analyses
3. Results
3.1. Patient Characteristics
3.2. CO2 Reactivity of PbtO2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hawley, C.A.; Ward, A.B.; Long, J.; Owen, D.W.; Magnay, A.R. Prevalence of traumatic brain injury amongst children admitted to hospital in one health district: A population based study. Injury 2003, 354, 256–260. [Google Scholar] [CrossRef] [Green Version]
- Maas, A.I.R.; Menon, D.K.; Adelson, P.D.; Andelic, N.; Bell, M.J.; Belli, A.; Bragge, P.; Brazinova, A.; Büki, A.; Chesnut, R.M.; et al. Traumatic brain injury: Integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017, 16, 987–1048. [Google Scholar] [CrossRef] [Green Version]
- Kochanek, P.M.; Tasker, R.C.; Carney, N.; Totten, A.M.; Adelson, P.D.; Selden, N.R.; Davis-O’Reilly, C.; Hart, E.L.; Bell, M.J.; Bratton, S.L.; et al. Guidelines for the management of pediatric severe traumatic brain injury, third edition: Update of the brain trauma foundation guidelines. Pediatr. Crit. Care Med. 2019, 20 (Suppl. 1), S1–S82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Appavu, B.; Foldes, S.T.; Adelson, P.D. Clinical trials for pediatric traumatic brain injury: Definition of insanity? J. Neurosurg. Pediatr. 2019, 23, 661–669. [Google Scholar] [CrossRef] [Green Version]
- Figaji, A.A.; Zwane, E.; Thompson, C.; Fieggen, A.G.; Argent, A.C.; Le Roux, P.D.; Peter, J.C. Brain tissue oxygen tension monitoring in pediatric severe traumatic brain injury. Part 1: Relationship with outcome. Child Nerv. Syst. 2009, 25, 1325–1333. [Google Scholar] [CrossRef] [PubMed]
- Rass, V.; Solari, D.; Ianosi, B.; Gaasch, M.; Kofler, M.; Schiefecker, A.J.; Miroz, J.-P.; Morelli, P.; Thomé, C.; Beer, R.; et al. Protocolized Brain Oxygen Optimization in Subarachnoid Hemorrhage. Neurocritical Care 2019, 31, 263–272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chesler, M. Regulation and modulation of pH in the brain. Physiol. Rev. 2003, 83, 1183. [Google Scholar] [CrossRef] [PubMed]
- Sahuquillo, J.; Munar, F.; Baguena, M.; Poca, M.A.; Pedraza, S.; Rodríguez-Baeza, A. Evaluation of Cerebrovascular CO2-Reactivity and Autoregulation in Patients with Post-Traumatic Diffuse Brain Swelling (Diffuse Injury III). In Intracranial Pressure and Neuromonitoring in Brain Injury; Marmarou, A., Bullock, R., Eds.; Springer: Vienna, Italy, 1998; pp. 233–236. [Google Scholar] [CrossRef]
- Grande, P.O. Critical Evaluation of the Lund Concept for Treatment of Severe Traumatic Head Injury, 25 Years after Its Introduction. Front. Neurol. 2017, 8, 315. [Google Scholar] [CrossRef] [Green Version]
- Kochanek, P.; Carney, N.; Adelson, P.D.; Ashwal, S.; Bell, M.J.; Bratton, S.; Carson, S.; Chesnut, R.; Ghajar, J.; Goldstein, B.; et al. Guidelines for the acute management of severe traumatic brain injury in infants, children and adolescents–second edition. Pediatr Crit. Care Med. 2012, 13 (Suppl. 1), S1–S82. [Google Scholar] [CrossRef]
- Adelson, P.D.; Pineda, J.; Bell, M.J.; Abend, N.S.; Berger, R.P.; Giza, C.C.; Hotz, G.; Wainwright, M.S. Common data elements for pediatric traumatic brain injury: Recommendations from the working group on demographics and clinical assessment. J. Neurotrauma 2012, 29, 639–653. [Google Scholar] [CrossRef] [Green Version]
- Beers, S.R.; Wisniewski, S.R.; Garcia-Filion, P.; Tian, Y.; Hahner, T.; Berger, R.P.; Bell, M.J.; Adelson, P.D. Validity of a pediatric version of the Glasgow Outcome Scale—Extended. J. Neurotrauma 2012, 29, 1126–1139. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steiner, L.A.; Czosnyka, M.; Piechnik, S.K.; Smielewski, P.; Chatfield, D.; Menon, D.K.; Pickard, J.D. Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Crit. Care Med. 2002, 30, 7338. [Google Scholar] [CrossRef] [PubMed]
- Lewis, P.M.; Czosnyka, M.; Carter, B.G.; Rosenfeld, J.V.; Paul, E.; Singhal, N.; Butt, W. Cerebrovascular pressure reactivity in children with traumatic brain injury. Pediatr. Crit. Care Med. 2015, 16, 739–749. [Google Scholar] [CrossRef] [PubMed]
- Appavu, B.; Temkit, M.; Foldes, S.; Burrows, B.T.; Kuwabara, M.; Jacobson, A.; Adelson, P.D. Association of Outcomes with Model-Based Indices of Cerebral Autoregulation After Pediatric Traumatic Brain Injury. Neurocritical Care 2021, 35, 640–650. [Google Scholar] [CrossRef]
- Asparouhov, T.; Harraker, E.L.; Muthen, B. Dynamic structural equation models: Structural equation modeling. A Multidiscip. J. 2018, 25, 359–388. [Google Scholar] [CrossRef]
- Stippler, M.; Ortiz, V.; Adelson, P.D.; Chang, Y.-F.; Tyler-Kabara, E.C.; Wisniewski, S.R.; Fink, E.L.; Kochanek, P.M.; Brown, S.D.; Bell, M.J. Brain tissue oxygen monitoring after severe traumatic brain injury in children: Relation to outcome and association with other clinical parameters. J. Neurosurg. Pediatr. 2012, 10, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Figaji, A.A.; Zwane, E.; Thompson, C.; Fieggen, A.G.; Argent, A.C.; Le Roux, P.D.; Peter, J.C. Brain tissue oxygen monitoring in pediatric severe traumatic brain injury. Part 2: Relationship with clinical, physiological, and treatment factors. Childs Nerv. Syst. 2009, 25, 1335–1343. [Google Scholar] [CrossRef] [PubMed]
- Okonkwo, D.O.; Shutter, L.; Moore, C.; Temkin, N.R.; Puccio, A.M.; Madden, C.J.; Andaluz, N.; Chesnut, R.; Bullock, M.R.; Grant, G.A.; et al. Brain Oxygen Optimization in Severe Trauamtic Brain Injury Phase II: A Phase II Randomized Trial. Crit. Care Med. 2017, 45, 1907–1914. [Google Scholar] [CrossRef] [PubMed]
- Lochhead, J.J.; Yang, J.; Ronaldson, P.T.; Davis, T.P. Structure, Function, and Regulation of the Blood-Brain Barrier Tight Junction in Central Nervous System Disorders. Front Physiol. 2020, 11, 914. [Google Scholar] [CrossRef]
- Lee, J.H.; Kelly, D.F.; Oertel, M.; McArthur, D.; Glenn, T.; Vespa, P.; Boscardin, W.J.; Martin, N. Carbon dioxide reactivity, pressure autoregulation, and metabolic suppression reactivity after head injury: A transcranial Doppler study. J. Neurosurg. 2001, 95, 222–232. [Google Scholar] [CrossRef] [Green Version]
- Watzman, H.M.; Kurth, C.D.; Montenegro, L.M.; Rome, J.; Steven, J.M.; Nicolson, S.C. Arterial and venous contributions to near-infrared cerebral oximetry. Anesthesiology 2000, 93, 947–953. [Google Scholar] [CrossRef] [PubMed]

| Patient | Sex | Race | Age (Years) | TBI Cause | TBI Mechanism | TBI Type | GCS | GOSE-Peds, 12 Months Post-Injury | Radiographic Neuropathology (CT/MRI) | Neurosurgical Procedures before Monitoring | Sedation | Vasoactive Agents | Hyperosmolar Therapy | PbtO2 Location |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | Hispanic | 12 | MVA (Auto vs. pedestrian) | Closed | DI | 4 | 3 | Diffuse cerebral edema R convexity SDH, Mid-line shift, Cerebellar tonsillar herniation | DC and epidural hematoma evacuation | FNT (1 mcg/hg/h), PRP (50 mcg/kg/min) | None | HTS (bolus) | LF |
| 2 | M | Hispanic | 3 | Fall from trampoline | Crush | FFT | 6 | 5 | R SDH R to L mid-line shift. Skull base frx | Subdural hematoma evacuation | FNT (1 mcg/kg/h), Dex (0.4 mcg/kg/h) | None | None | LF |
| 3 | M | Asian | 16 | FL | Blast | GLF | 4 | 1 | R scalp hematoma R parietal skull frx R- frontotemporal and parietal SDH R to L mid-line shift R frontal tSAH | DC and subdural hematoma evacuation | FNT (2 mcg/kg/h), Pentobarbital (1 mg/kg/h) | NE | None | RF |
| 4 | M | Hispanic | 11 | MVA (Auto vs. pedestrian) | Closed | DI | 4 | 8 | L parietal scalp hematoma, EDH extending from CCJ to supraclinoid region, tSAH, diffuse cerebral edema, DAI, cerebellar edema and contusion, AO dislocation, T12-L1 frx | Bedside EVD | FNT (1 mcg/kg/h) | Antihypertensives | HTS (bolus) | LF |
| 5 | M | Native American | 15 | MVA (Auto vs. pedestrian) | Closed | DI | 3 | 3 | L frontotemporal and parietal skull fractures, B/L temporal contusions, B/L SDH, diffuse cerebral edema, pneumocephalus, diffuse tSAH at basal cisterns, cerebellar herniation, L to R mid-line shift | DC and epidural hematoma evacuation | FNT (1 mcg/kg/h) | NE | HTS (infusion) | RF |
| 6 | M | Caucasian | 14 | Fall from height | Closed | FFT | 3 | 2 | R temporal bone, occipital condyle and sphenoid sinus frx, cortical contusion on the L mid frontal region of lateral ventricles, SDH | No operation | FNT (2 mcg/kg/h) | NE | HTS (infusion) | RF |
| 7 | M | Caucasian | 15 | MVA (Auto vs. bicycle (w/o helmet)) | Closed | DI | 3 | 7 | L-post scalp hematoma, B/L SDH, tSAH, punctate parenchymal hemorrhages, basal cistern effaced, L- Temporal frx | EVD placement at the OR | DEX (0.6 mcg/kg/h), FNT (1 mcg/kg/h), PRP (0.25 mcg/kg/min) | None | None | LF |
| 8 | M | Caucasian | 14 | MVA (Auto vs. motorcycle (w/o helmet)) | Closed | DI | 4 | 2 | B/L EDH, SDH, effacement of basal cistern, diffuse cerebral edema | DC and epidural hematoma evacuation | DEX (1 mcg/kg/h), PRP (50 mcg/kg/min), FNT (1 mcg/kg/h) | NE | Mannitol, HTS (infusion) | RF |
| 9 | M | Hispanic | 14 | MVA (Auto vs. pedestrian) | Closed | DI | 5 | 5 | L post scalp hematoma, L frontal SDH, IVH, punctate parenchymal hemorrhages | N/A | FNT (1 mcg/kg/h), PRP (50 mcg/kg/min) | EPI, NE | None | LF |
| 10 | F | Caucasian | 17 | MVA (Auto vs. pedestrian) | Closed | DI | 3 | 5 | Scalp hematoma, posterior sutural diastases, pneumocephalus, right sigmoid sinus and superior sagittal sinus thrombus, B/L frontal lobe contusions, tSAH, SDH | DC, evacuation of R frontal contusion | FNT (1 mcg/kg/h), PRP (60 mcg/kg/min) | NE | HTS (infusion), Mannitol | LF |
| 11 | F | Native American | 7 | MVA (Auto vs. pedestrian) | Closed | DI | 6 | 4 | B/L frontal, parietal, temporal bone frx, open and depressed, skull base and MF frx, pneumocephalus, EDH, SDH, tSAH | DC and epidural hematoma evacuation | FNT (1 mcg/kg/h), Pentobarbital (2 mg/kg/h) | NE, Vasopressin | HTS (bolus and infusion) | RF |
| 12 | M | Hispanic | 17 | MVA (Auto vs. Pedestrian) | Closed | DI | 5 | 5 | Central midbrain hemorrhage, B/L IVH, R temporal lobe ICH, tSAH, SDH | EVD placement | DEX (0.2 mcg/kg/h), FNT (3 mcg/kg/h), PRP (25 mcg/kg/min) | None | None | RF |
| 13 | M | Hispanic | 20 | MVA (ATV head on head crush (w/o helmet)) | Closed | DI | 7 | 6 | R- frontotemporal scalp hematoma, depressed frx and contusion, R-FPT and occipital ICH, IVH, diffuse cerebral edema, R-to-L midline shift | DC and intraparenchymal hematoma evacuation, partial frontal lobectomy, EVD placement | FNT (3 mcg/kg/h), PRP (25 mcg/kg/min) | None | Mannitol (bolus) HTS (bolus) | RF |
| 14 | M | Caucasian | 14 | MVA (Auto vs. pedestrian) | Closed | DI | 7 | 6 | R parietal scalp hematoma, R-TFP ICH, retroclinoid extradural hematoma, tSAH | DC and hematoma evacuation | FNT (1 mcg/kg/h), PRP (30 mcg/kg/min) | NE | HTS (bolus) | RF |
| Patient | PbtO2 Location | Hemoglobin Concentration (g/dL) | FiO2, sta% | Median PbtO2, mmHg | Median EtCO2, mmHg | Median ABP, mmHg | Median ICP, mmHg | Median rSO2, % | Median PRx |
|---|---|---|---|---|---|---|---|---|---|
| 1 | LF | 10.9 | 70–90 | 10.0 [9.0, 13.0] | 38.0 [33.0, 41.0] | 79.0 [77.0, 81.6] | 14.0 [11.0, 14.0] | 95.0 [93.0, 95.0] | −0.06 [−0.34, 0.12] |
| 2 | LF | 10.6 | 40–50 | 69.0 [65.0, 73.0] | 32.0 [31.0, 32.0] | 93.0 [91.0, 97.0] | 20.0 [17.0, 21.0] | 76.1 [74.2, 77.0] | 0.18 [−0.51, 0.28] |
| 3 | RF | 11.1 | 55–60 | 21.0 [19.0, 24.0] | 33.0 [32.0, 35.0] | 87.0 [83.0, 90.0] | 11.0 [10.0, 15.0] | 77.0 [76.0, 84.4] | −0.40 [−0.73, −0.22] |
| 4 | LF | 13.5 | 50 | 54.0 [47.0, 58.0] | 30.0 [29.0, 32.0] | 92.0 [90.0, 94.0] | 7.0 [7.0, 8.0] | 79.0 [78.0, 80.0] | 0.19 [−0.03, 0.47] |
| 5 | RF | 7.5 | 5–50 | 52.0 [50.0, 64.0] | 38.0 [37.0, 40.0] | 76.8 [73.1, 79.0] | 6.0 [5.0, 7.0] | 75.0 [71.5, 76.7] | 0.29 [0.06, 0.51] |
| 6 | RF | 10.2 | 35–80 | 39.0 [37.0, 44.0] | 32.0 [31.0, 36.0] | 109.0 [100.0, 111.0] | 11.0 [10.0, 12.0] | 71.4 [70.1, 73.0] | 0.25 [0.02, 0.48] |
| 7 | LF | 11.4 | 45–60 | 27.0 [25.0, 28.0] | 33.0 [32.0, 34.0] | 91.0 [84.0, 98.0] | 6.0 [5.0, 8.0] | 69.0 [64.8, 71.0] | −0.11 [−0.30, 0.07] |
| 8 | RF | 11.6 | 50–65 | 7.0 [5.0, 10.0] | 37.0 [35.0, 39.0] | 78.0 [75.0, 82.0] | 15.0 [14.0, 16.0] | 91.0 [89.0, 92.0] | 0.07 [−0.21, 0.35] |
| 9 | LF | 6.2 | 40–60 | 21.1 [14.5, 27.1] | 28.0 [27.0, 29.0] | 76.0 [73.0, 78.0] | 7.0 [7.0, 10.0] | 82.0 [81.0, 84.0] | 0.67 [0.54, 0.82] |
| 10 | LF | 9.0 | 30–95 | 14.2 [12.6, 18.6] | 32.0 [31.0, 33.0] | 81.0 [76.0, 83.5] | 12.0 [10.0, 13.0] | 95.0 [94.0, 95.0] | −0.06 [−0.30, 0.18] |
| 11 | RF | 9.8 | 60–85 | 26.0 [25.0, 28.0] | 33.0 [32.0, 34.0] | 100.0 [960, 103.0] | 11.0 [7.0, 14.0] | 33.0 [70.0, 75.4] | 0.07 [−0.29, 0.40] |
| 12 | LF | 11 | 40–50 | 76.6 [74.9, 78.9] | 36.0 [34.0, 39.0] | 75.0 [68.0, 80.0] | 16.0 [9.0, 19.0] | 71.8 [70.0, 73.1] | −0.02 [−0.22, 0.20] |
| 13 | RF | 15.9 | 30–100 | 36.0 [32.0, 38.0] | 33.0 [33.0, 34.0] | 93.0 [91.0, 99.0] | 14.0 [12.1, 15.0] | 74.8 [73.0, 75.9] | 0.15 [−0.01, 0.29] |
| 14 | RF | 16.2 | 40–50 | 8.5 [6.9, 9.1] | 37.0 [33.0, 38.0] | 81.0 [78.0, 87.7] | 23.0 [22.0, 24.0] | 95.0 [95.0, 95.0] | 0.13 [−0.05, 0.31] |
| Patient | PbtO2 to EtCO2 [SRC (95% CI)] | PbtO2 to ICP [SRC (95% CI)] | PbtO2 to ABP [SRC (95% CI)] | PbtO2 to rSO2 [SRC (95% CI)] |
|---|---|---|---|---|
| 1 | 0.06 (0.05, 0.08) | 0.30 (0.28, 0.31) | 0.06 (0.05, 0.08) | 0.24 (0.22, 0.25) |
| 2 | −0.06 (−0.07, −0.05) | 0.04 (0.03, 0.06) | 0.14 (0.13, 0.15) | 0.24 (0.22, 0.25) |
| 3 | 0.20 (0.19, 0.22) | −0.04 (−0.05, −0.02) | 0.23 (0.21, 0.24) | −0.35 (−0.36, −0.33) |
| 4 | 0.26 (0.24, 0.27) | 0.14 (0.12, 0.15) | 0.48 (0.47, 0.49) | −0.24 (−0.25, −0.22) |
| 5 | 0.18 (0.17, 0.20) | 0.49 (0.48, 0.50) | 0.21, (0.20, 0.22) | 0.37 (0.36, 0.38) |
| 6 | 0.83 (0.82, 0.83) | 0.57 (0.56, 0.59) | 0.53 (0.52, 0.55) | 0.39 (0.37, 0.41) |
| 7 | 0.64 (0.63, 0.64) | −0.54 (−0.55, −0.53) | 0.38 (0.37, 0.39) | −0.44 (−0.45, −0.42) |
| 8 | 0.14 (0.12, 0.15) | 0.14 (0.13, 0.16) | 0.63 (0.62, 0.63) | −0.33 (−0.34, −0.32) |
| 9 | −0.44 (−0.45, −0.42) | −0.25 (−0.26, −0.24) | 0.66 (0.65, 0.67) | 0.20 (0.19, 0.21) |
| 10 | −0.45 (−0.46, −0.43) | −0.40 (−0.41, −0.39) | 0.46 (0.45, 0.47) | 0.26 (0.25, 0.28) |
| 11 | −0.65 (−0.66, −0.65) | −0.58 (−0.59, −0.57) | 0.03 (0.02, 0.05) | −0.48 (−0.49, −0.47) |
| 12 | 0.09 (0.08, 0.11) | −0.03 (−0.04, −0.01) | 0.42 (0.41, 0.43) | 0.08 (0.06, 0.09) |
| 13 | 0.59 (0.58, 0.60) | 0.16 (0.15, 0.18) | 0.67 (0.67, 0.68) | −0.21 (−0.23, −0.20) |
| 14 | −0.45 (−0.47, −0.44) | −0.23 (−0.24, 0.22) | 0.48 (0.46, 0.49) | −0.12 (−0.14, −0.11) |
| Grouped Analysis | 0.05 (0.04, 0.06) | 0.02 (0.02, 0.03) | 0.36 (0.35, 0.36) | 0.02 (0.01, 0.02) |
| CO2 Reactivity of PbtO2 | PbtO2 to EtCO2 [SRC (95% CI)] | PbtO2 to rSO2 [SRC (95% CI)] | PbtO2 to ICP [SRC (95% CI)] | PbtO2 to ABP [SRC (95% CI)] |
|---|---|---|---|---|
| Intact | 0.44 (0.44, 0.45) | −0.08 (−0.09, −0.08) | 0.22 (0.21, 0.23) | 0.38 (0.38, 0.39) |
| Impaired | −0.38 (−0.39, −0.37) | 0.15 (0.14, 0.16) | −0.28 (−0.29, −0.28) | 0.31 (0.31, 0.32) |
| CO2 Reactivity to PbtO2 | Intact CO2 Reactivity of PbtO2, Median [IQR] | Impaired CO2 Reactivity of PbtO2, Median [IQR] | p-Value |
|---|---|---|---|
| PbtO2 | 36.0 [21.0, 52.0] | 21.1 [14.2, 26.0] | 0.0000 |
| ICP | 11.0 [7.0, 14.0] | 12.0 [11.0, 20.0] | 0.0000 |
| PRx | 0.07 [−0.06, 0.19] | 0.13 [0.07, 0.18] | 0.0134 |
| ABP | 87.0 [78.0, 92.0] | 81.0 [81.0, 93.0] | 0.0000 |
| EtCO2 | 33.0 [33.0, 37.0] | 32.0 [32.0, 33.0] | 0.0000 |
| rSO2 | 75.0 [71.8, 79.0] | 82.0 [76.1, 95.0] | 0.0000 |
| GOSE-Peds, 12 months post-injury | 3.0 [2.0, 6.0] | 5.0 [5.0, 5.0] | 0.0000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hanalioglu, D.; Oh, A.; Temkit, M.; Adelson, P.D.; Appavu, B. Carbon Dioxide Reactivity of Brain Tissue Oxygenation after Pediatric Traumatic Brain Injury. Children 2022, 9, 409. https://doi.org/10.3390/children9030409
Hanalioglu D, Oh A, Temkit M, Adelson PD, Appavu B. Carbon Dioxide Reactivity of Brain Tissue Oxygenation after Pediatric Traumatic Brain Injury. Children. 2022; 9(3):409. https://doi.org/10.3390/children9030409
Chicago/Turabian StyleHanalioglu, Damla, Ann Oh, M’Hamed Temkit, P. David Adelson, and Brian Appavu. 2022. "Carbon Dioxide Reactivity of Brain Tissue Oxygenation after Pediatric Traumatic Brain Injury" Children 9, no. 3: 409. https://doi.org/10.3390/children9030409
APA StyleHanalioglu, D., Oh, A., Temkit, M., Adelson, P. D., & Appavu, B. (2022). Carbon Dioxide Reactivity of Brain Tissue Oxygenation after Pediatric Traumatic Brain Injury. Children, 9(3), 409. https://doi.org/10.3390/children9030409






