Discordance among Belief, Practice, and the Literature in Infection Prevention in the NICU
Abstract
:1. Introduction
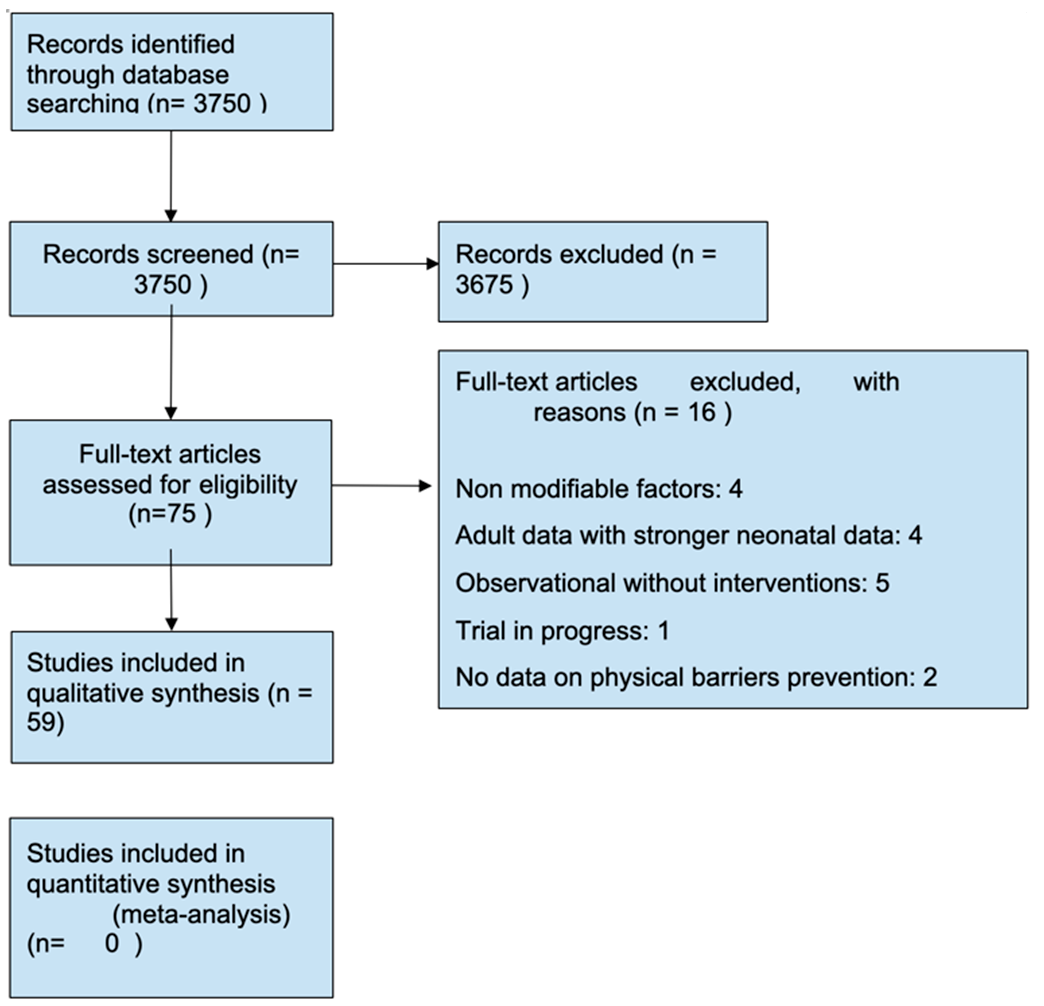
2. Materials and Methods
2.1. Developing the Survey
2.2. Data Collection
- (a)
- Report on practice patterns and practice changing interventions on hand hygiene compliance within the NICU setting.
- (b)
- Association between gloves, gowns, cellphones, accessories, and attire with HAI in the NICU.
- (c)
- Type of water utilized for neonatal bathing and infection risk. Sink disinfection practice and infection risk.
- (d)
- Siblings care policy and visiting restrictions and its impact on HAI.
3. Results
3.1. General Survey Results
3.2. Hand Hygiene, Gowns, and Gloves
3.2.1. Reviewed Literature
- A.
- Hand Hygiene Compliance:
- B.
- Gloves and Gowns:
3.2.2. Survey Results
3.3. Clothing and Attire: White Coats, Ties and Sleeves
3.3.1. Reviewed Literature
3.3.2. Survey Results
3.4. Other Fomites and Accessories
3.4.1. Reviewed Literature
- A.
- Stethoscopes and Cell Phones
- B.
- Rings, Watches, and Artificial Fingernails
3.4.2. Survey Results
3.5. Environment and Facilities
3.5.1. Reviewed Literature
3.5.2. Survey Results
3.6. Siblings and Family Visitation
3.6.1. Reviewed Literature
3.6.2. Survey Results
4. Discussion
- A.
- High certainty of the evidence: The intervention leads to a large reduction/increase in outcome.
- B.
- Moderate certainty of the evidence: The intervention leads to a moderate reduction/increase in outcome.
- C.
- Low certainty of the evidence: The intervention leads to a small reduction/increase in outcome.
- 1.
- High quality prospective cohort study with adequate power or systematic review of these studies.
- 2.
- Lesser quality prospective cohort, retrospective cohort study, or systematic review of these studies.
- 3.
- Case–control study or systematic review of these studies.
- 4.
- Case series.
- 5.
- Expert opinion; case report; clinical examples.
4.1. Physical Barriers: Hand Hygiene, Gowns, and Gloves
- −
- The use of alcohol-based hand hygiene as opposed to soap-based hygiene to improve compliance.
- −
- Structured periodic feedback systems to sustain long term hand hygiene compliance.
- −
- A multimodal approach to spreading awareness and improving compliance for hand hygiene; we recommend incorporating visual reminders and individual feedback.
- −
- The use of non-sterile gloves in addition to hand hygiene during the care of preterm infants and during the RSV season for all infants.
4.2. Attire
- −
- We make a grade C recommendation based on level 3 evidence for prohibition of unsecured ties in the NICU to decrease infection transmission.
- −
- The current level 2 evidence does not support prohibition of white coats or a bare elbow policy to decrease infection transmission in the NICUs. We recommend resource utilization to reinforce other evidence proven interventions.
4.3. Fomites and Accessories
- −
- Disinfecting stethoscopes between patient encounters.
- −
- Instituting policies that regulate the use of cellphones in the NICU. Not enough data exists to recommend prohibiting or restricting their use. However, hygiene is recommended after each use.
4.4. Environment and Facilities
- −
- We make a grade B recommendation based on level 2 evidence in favor of using sterile water for bathing and self-disinfecting sinks in neonatal ICU settings with high rates of tap water pseudomonal colonization.
4.5. Siblings and Family Visitation:
- −
- We make a grade C recommendation based on level 3 evidence for restricting siblings’ access to NICU during RSV seasons.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| nicu infection control |
| nicu infection hand hygiene |
| nicu infection gowning |
| nicu infection family members |
| Nicu family hand hygiene |
| Nicu family hand washing |
| Nicu family infection control |
| NICU hand scrubbing duration |
| Nicu hand hygiene duration |
| Nicu hand hygiene protocol |
| Nicu hand duration |
| Nicu hand hygiene compliance |
| Jewelry infection control |
| Hand hygiene nicu programs |
| Nicu hand hygiene education |
| comparing hand hygiene nicu |
| hand hygiene promotion nicu |
| nicu hand washing promotion |
| nicu hand washing pamphlets |
| nicu hand washing education |
| nicu hand washing comparison |
| nicu hand hygiene comparison |
| ICU infection white coats |
| white coats infection |
| neck ties infection |
| ties infection |
| ties infection clothing |
| rings infection clothing |
| watches infection clothing |
References
- Harrison, W.; Goodman, D. Epidemiologic Trends in Neonatal Intensive Care, 2007–2012. JAMA Pediatr. 2015, 169, 855–862. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fanaroff, A.A.; Stoll, B.J.; Wright, L.L.; Carlo, W.A.; Ehrenkranz, R.A.; Stark, A.R.; Bauer, C.R.; Donovan, E.F.; Korones, S.B.; Laptook, A.R.; et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am. J. Obstet. Gynecol. 2007, 196, 147.e1–147.e8. [Google Scholar] [CrossRef] [PubMed]
- Horbar, J.D.; Carpenter, J.H.; Badger, G.J.; Kenny, M.J.; Soll, R.F.; Morrow, K.A.; Buzas, J.S. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics 2012, 129, 1019–1026. [Google Scholar] [CrossRef] [Green Version]
- Garner, J.S.; Jarvis, W.R.; Emori, T.G.; Horan, T.C.; Hughes, J.M. CDC definitions for nosocomial infections. In APIC Infection Control and Applied Epidemiology: Principles and Practice; Olmsted, R.N., Ed.; Mosby: St. Louis, MI, USA, 1996; p. A-1–20. [Google Scholar]
- Gadallah, M.A.H.; Fotouh, A.M.A.; Habil, I.S.; Imam, S.S.; Wassef, G. Surveillance of health care associated infections in a tertiary hospital neonatal intensive care unit in Egypt: 1-year follow-up. Am. J. Infect. Control 2014, 42, 1207–1211. [Google Scholar] [CrossRef]
- Bolat, F.; Uslu, S.; Bolat, G.; Comert, S.; Can, E.; Bulbul, A.; Nuhoglu, A. Health care associated infections in a neonatal intensive care unitin Turkey. Indian Paediatr. 2012, 49, 951–957. [Google Scholar] [CrossRef]
- Stoll, B.J.; Hansen, N.; Fanaroff, A.A.; Wright, L.L.; Carlo, W.A.; Ehrenkranz, R.A.; Lemons, J.A.; Donovan, E.F.; Stark, A.R.; Tyson, J.E.; et al. Late-onset sepsis in very low birth weight neonates; the experience of the NICHD Neonatal Research Network. Pediatrics 2002, 110, 285–291. [Google Scholar] [CrossRef]
- Boghossian, N.S.; Page, G.P.; Bell, E.F.; Stoll, B.J.; Murray, J.C.; Cotten, C.M.; Shankaran, S.; Walsh, M.C.; Laptook, A.R.; National Institute of Child Health and Human Development Neonatal Research Network; et al. Late-onset sepsis in very low birth weight infants from singleton and multiple-gestation births. J. Pediatr. 2013, 162, 1120–1124.e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gastmeier, P.; Loui, A.; Stamm-Balderjahn, S.; Hansen, S.; Zuschneid, I.; Sohr, D.; Behnke, M.; Obladen, M.; Vonberg, R.-P.; Rüden, H. Outbreaks in neonatal intensive care units-they are not like others. Am. J. Infect. Control 2007, 35, 172–176. [Google Scholar] [CrossRef]
- Scheithauer, S.; Oude-Aost, J.; Heimann, K.; Haefner, H.; Schwanz, T.; Waitschies, B.; Kampf, G.; Orlikowsky, T.; Lemmen, S.W. Hand hygiene in pediatric and neonatal intensive care unit patients: Daily opportunities and indication- and profession-specific analyses of compliance. Am. J. Infect. Control 2011, 39, 732–737. [Google Scholar] [CrossRef]
- Larson, E.L.; Albrecht, S.; O’Keefe, M. Hand hygiene behavior in a pediatric emergency department and a pediatric intensive care unit: Comparison of use of 2 dispenser systems. Am. J. Crit. Care 2005, 14, 304–311. [Google Scholar] [CrossRef]
- Harbarth, S.; Pittet, D.; Grady, L.; Goldmann, D.A. Compliance with hand hygiene practice in pediatric intensive care. Pediatr. Crit. Care Med. 2001, 2, 311–314. [Google Scholar] [CrossRef] [PubMed]
- Adams-Chapman, I.; Stoll, B.J. Prevention of nosocomial infections in the neonatal intensive care unit. Curr. Opin. Pediatr. 2002, 14, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Ramasethu, J. Prevention and treatment of neonatal nosocomial infections. Matern. Health Neonatol. Perinatol. 2017, 3, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alsubaie, S.; bin Maither, A.; Alalmaei, W.; Al-Shammari, A.D.; Tashkandi, M.; Somily, A.M.; Alaska, A.; Bin Saeed, A.A. Determinants of hand hygiene noncompliance in intensive care units. Am. J. Infect. Control 2013, 41, 131–135. [Google Scholar] [CrossRef]
- Graham, P.L., III. Simple Strategies to Reduce Healthcare Associated Infections in the Neonatal Intensive Care Unit: Line, Tube, and Hand Hygiene. Clin. Perinatol. 2010, 37, 645–653. [Google Scholar] [CrossRef] [PubMed]
- Stahmeyer, J.T.; Lutze, B.; Von Lengerke, T.; Chaberny, I.F.; Krauth, C. Hand hygiene in intensive care units: A matter of time? J. Hosp. Infect. 2017, 95, 338–343. [Google Scholar] [CrossRef]
- Kurtz, S.L. Identification of low, high, and super gelers and barriers to hand hygiene among intensive care unit nurses. Am. J. Infect. Control 2017, 45, 839–843. [Google Scholar] [CrossRef]
- Kramer, A.; Pittet, D.; Klasinc, R.; Krebs, S.; Koburger, T.; Fusch, C.; Assadian, O. Shortening the Application Time of Alcohol-Based Hand Rubs to 15 Seconds May Improve the Frequency of Hand Antisepsis Actions in a Neonatal Intensive Care Unit. Infect. Control Hosp. Epidemiol. 2017, 38, 1430–1434. [Google Scholar] [CrossRef]
- Cohen, B.; Saiman, L.; Cimiotti, J.; Larson, E. Factors associated with hand hygiene practices in two neonatal intensive care units. Pediatr. Infect. Dis. J. 2003, 22, 494–499. [Google Scholar] [CrossRef] [Green Version]
- Brown, S.M.; Lubimova, A.V.; Khrustalyeva, N.M.; Shulaeva, S.V.; Tekhova, I.; Zueva, L.P.; Goldmann, D.; O’Rourke, E.J. Use of an alcohol-based hand rub and quality improvement interventions to improve hand hygiene in a Russian neonatal intensive care unit. Infect. Control Hosp. Epidemiol. 2003, 24, 172–179. [Google Scholar] [CrossRef]
- Girou, E.; Loyeau, S.; Legrand, P.; Oppein, F.; Brun-Buisson, C. Efficacy of handrubbing with alcohol based solution versus standard handwashing with antiseptic soap: Randomised clinical trial. BMJ 2002, 325, 362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sharma, V.; Dutta, S.; Taneja, N.; Narang, A. Comparing Hand-hygiene Measures in a Neonatal ICU: A Randomized Cross-over Trial. Indian Pediatr. 2013, 50, 917–921. [Google Scholar] [CrossRef] [PubMed]
- Sakamoto, F.; Yamada, H.; Suzuki, C.; Sugiura, H.; Tokuda, Y. Increased use of alcohol-based hand sanitizers and successful eradication of methicillin-resistant Staphylococcus aureus from a neonatal intensive care unit: A multivariate time series analysis. Am. J. Infect. Control. 2010, 38, 529–534. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Larson, E.L.; Cimiotti, J.; Haas, J.; Parides, M.; Nesin, M.; Della-Latta, P.; Saiman, L. Effect of Antiseptic Handwashing vs Alcohol Sanitizer on Health Care–Associated Infections in Neonatal Intensive Care Units. Arch. Pediatr. Adolesc. Med. 2005, 159, 377. [Google Scholar] [CrossRef] [Green Version]
- Miranda-Novales, M.G.; Sobreyra-Oropeza, M.; Rosenthal, V.D.; Higuera, F.; Armas-Ruiz, A.; Pérez-Serrato, I.; Torres-Hernández, H.; Zamudio-Lugo, I.; Flores-Ruiz, E.M.; Campuzano, R.; et al. Impact of the International Nosocomial Infection Control Consortium (INICC) Multidimensional Hand Hygiene Approach During 3 Years in 6 Hospitals in 3 Mexican Cities. J. Patient Saf. 2019, 15, 49–54. [Google Scholar] [CrossRef]
- Wetzker, W.; Bunte-Schönberger, K.; Walter, J.; Pilarski, G.; Gastmeier, P.; Reichardt, C. Compliance with hand hygiene: Reference data from the national hand hygiene campaign in Germany. J. Hosp. Infect. 2016, 92, 328–331. [Google Scholar] [CrossRef]
- Pessoa-silva, C.L.; Posfay-barbe, K.; Pfister, R.; Touveneau, S.; Perneger, T.V.; Pittet, D. Healthcare workers caring for critically ill neonates attitudes and perceptions toward hand hygiene among healthcare workers caring for critically Ill Neonates. Infect. Control Hosp. Epidemiol. 2005, 26, 305–311. [Google Scholar] [CrossRef]
- Bloom, B.T.; Craddock, A.; Delmore, P.M.; Kurlinski, J.P.; Voelker, M.; Landfish, N.; Rodriguez-Pierce, M.; Swanton, D.; Rossi, J.; Ehlen, J.; et al. Reducing Acquired Infections in the NICU: Observing and Implementing Meaningful Differences in Process Between High and Low Acquired Infection Rate Centers. J. Perinatol. 2003, 23, 489–492. [Google Scholar] [CrossRef] [Green Version]
- Lam, B.C.; Lee, J.; Lau, Y. Hand Hygiene Practices in a Neonatal Intensive Care Unit: A Multimodal Intervention and Impact on Nosocomial Infection. Pediatrics 2004, 114, e565–e571. [Google Scholar] [CrossRef] [Green Version]
- Danchaivijitr, S.; Pichiensatian, W.; Apisarnthanarak, A.; Kachintorn, K.; Cherdrungsi, R. Strategies to improve hand hygiene practices in two university hospitals. J. Med. Assoc. Thai. 2005, 88 (Suppl. 1), S155–S160. [Google Scholar]
- Pessoa-Silva, C.L.; Hugonnet, S.; Pfister, R.; Pfister, R.; Touveneau, S.; Dharan, S.; Posfay-Barbe, K.; Pittet, D. Reduction of Health Care–Associated Infection Risk in Neonates by Successful Hand Hygiene Promotion Carmem. Pediatrics 2007, 120, e382–e390. [Google Scholar] [CrossRef] [PubMed]
- van den Hoogen, A.; Brouwer, A.J.; Verboon-Maciolek, M.A.; Gerards, L.J.; Fleer, A.; Krediet, T.G. Improvement of Adherence to Hand Hygiene Practice Using a Multimodal Intervention Program in a Neonatal Intensive Care. J. Nurs. Care Qual. 2011, 26, 22–29. [Google Scholar] [CrossRef] [PubMed]
- Helder, O.K.; Weggelaar, A.M.; Waarsenburg, D.C.; Looman, C.W.; van Goudoever, J.B.; Brug, J.; Kornelisse, R.F. Computer screen saver hand hygiene information curbs a negative trend in hand hygiene behavior. Am. J. Infect. Control 2012, 40, 951–954. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mukerji, A.; Narciso, J.; Moore, C.; McGeer, A.; Kelly, E.; Shah, V. An observational study of the hand hygiene initiative: A comparison of preintervention and postintervention outcomes. BMJ Open 2013, 3, e003018. [Google Scholar] [CrossRef] [Green Version]
- Rosenthal, V.D.; Pawar, M.; Leblebicioglu, H.; Navoa-Ng, J.A.; Villamil-Gómez, W.; Armas-Ruiz, A.; Cuéllar, L.E.; Medeiros, E.A.; Mitrev, Z.; Gikas, A.; et al. Impact of the International Nosocomial Infection Control Consortium (INICC) Multidimensional Hand Hygiene Approach over 13 Years in 51 Cities of 19 Limited-Resource Countries from Latin America, Asia, the Middle East, and Europe. Infect. Control Hosp. Epidemiol. 2013, 34, 415–423. [Google Scholar] [CrossRef] [Green Version]
- Song, X.; Stockwell, D.C.; Floyd, T.; Short, B.L.; Singh, N. Improving hand hygiene compliance in health care workers: Strategies and impact on patient outcomes. Am. J. Infect. Control 2013, 41, e101–e105. [Google Scholar] [CrossRef]
- Chhapola, V.; Brar, R. Impact of an educational intervention on hand hygiene compliance and infection rate in a developing country neonatal intensive care unit. Int. J. Nurs. Pract. 2015, 21, 486–492. [Google Scholar] [CrossRef]
- Sadeghi-Moghaddam, P.; Arjmandnia, M.; Shokrollahi, M.; Aghaali, M. Does training improve compliance with hand hygiene and decrease infections in the neonatal intensive care unit? A prospective study. J. Neonatal-Perinat. Med. 2015, 8, 221–225. [Google Scholar] [CrossRef]
- Joshi, S.; Amatya, P.; Poudel, B.; Yadav, S.A. Handwashing Practices in Neonatal Intensive Care Unit, Paediatric Intensive Care Unit and Neonatal Nurseries in Patan Hospital. J. Nepal Health Res. Counc. 2017, 15, 56–60. [Google Scholar] [CrossRef] [Green Version]
- Hoang, D.; Khawar, N.; George, M.; Gad, A.; Sy, F.; Narula, P. Video didactic at the point of care impacts hand hygiene compliance in the neonatal intensive care unit (NICU). J. Healthc. Risk Manag. 2018, 37, 9–15. [Google Scholar] [CrossRef]
- Picheansathian, W.; Pearson, A.; Suchaxaya, P. The effectiveness of a promotion programme on hand hygiene compliance and nosocomial infections in a neonatal intensive care unit. Int. J. Nurs. Pract. 2008, 14, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Sharek, P.J.; Benitz, W.E.; Abel, N.J.; Freeburn, M.J.; Mayer, M.L.; Bergman, D.A. Effect of an Evidence-Based Hand Washing Policy on Hand Washing Rates and False-Positive Coagulase Negative Staphylococcus Blood and Cerebrospinal Fluid Culture Rates in a Level III NICU. J. Perinatol. 2002, 22, 137–143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raskind, C.H.; Worley, S.; Vinski, J.; Goldfarb, J. Hand Hygiene Compliance Rates After an Educational Intervention in a Neonatal Intensive. Infect. Control Hosp. Epidemiol. 2007, 28, 1096–1098. [Google Scholar] [CrossRef] [PubMed]
- Janota, J.; Šebková, S.; Višňovská, M.; Kudláčková, J.; Hamplová, D.; Zach, J. Hand hygiene with alcohol hand rub and gloves reduces the incidence of late onset sepsis in preterm neonates. Acta Paediatr. 2014, 103, 1053–1056. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, D.A.; Blackman, A.; Conaway, M.R.; Sinkin, R.A. Nonsterile Glove Use in Addition to Hand Hygiene to Prevent Late-Onset Infection in Preterm Infants. JAMA Pediatr. 2014, 168, 909. [Google Scholar] [CrossRef]
- Yin, J.; Schweizer, M.L.; Herwaldt, L.A.; Pottinger, J.M.; Perencevich, E.N. Benefits of Universal Gloving on Hospital-Acquired Infections in Acute Care Pediatric Units. Pediatrics 2013, 131, e1515–e1520. [Google Scholar] [CrossRef] [Green Version]
- Cloney, D.L.; Donowitz, L.G. Overgown use for infection control in nurseries and neonatal intensive care units. Am. J. Dis. Child. 1986, 140, 680–683. [Google Scholar] [CrossRef]
- Yu, V.Y.H. Neonatal sepsis and infection control policies in Australia. J. Paediatr. Child Health 1990, 26, 252–256. [Google Scholar] [CrossRef]
- Pelke, S.; Ching, D.; Easa, D.; Melish, M.E. Gowning Does Not Affect Colonization or Infection Rates in a Neonatal Intensive Care Unit. Arch. Pediatr. Adolesc. Med. 1994, 148, 1016–1020. [Google Scholar] [CrossRef]
- Tan, S.G.; Lim, S.H.; Malathi, I. Does routine gowning reduce nosocomial infection and mortality rates in a neonatal nursery? A Singapore experience. Int. J. Nurs. Prac. 1995, 1, 52–58. [Google Scholar] [CrossRef]
- Rutala, W.A.; Weber, D.J. A Review of Single-Use and Reusable Gowns and Drapes in Health Care. Infect. Control Hosp. Epidemiol. 2001, 22, 248–257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Webster, J.; Pritchard, M.A. Gowning by attendants and visitors in newborn nurseries for prevention of neonatal morbidity and mortality. In Cochrane Database of Systematic Reviews; Webster, J., Ed.; John Wiley & Sons, Ltd.: Chichester, UK, 2003; p. CD003670. [Google Scholar]
- Ebell, M.H. Gowning in newborn and special-care nurseries. Am. Fam. Physician 2004, 70, 83. [Google Scholar] [PubMed]
- Garvin, K.W.; Lipira, L.; Neradilek, M.; Fox, A.; Ali, F.; Pottinger, P.S. Attitudes regarding the safety of health care provider attire. Am. J. Infect. Control 2014, 42, 1219–1222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Treakle, A.M.; Thom, K.A.; Furuno, J.P.; Strauss, S.M.; Harris, A.D.; Perencevich, E.N. Bacterial contamination of health care workers’ white coats. Am. J. Infect. Control 2009, 37, 101–105. [Google Scholar] [CrossRef] [Green Version]
- BANU, A.; ANAND, M.; NAGI, N. White Coats as a Vehicle for Bacterial Dissemination. J. Clin. Diagnostic. Res. 2012, 6, 1381–1384. [Google Scholar] [CrossRef]
- Weber, R.L.; Khan, P.D.; Fader, R.C.; Weber, R.A.; Child, J.A. Prospective study on the effect of shirt sleeves and ties on the transmission of bacteria to patients. J. Hosp. Infect. 2012, 80, 252–254. [Google Scholar] [CrossRef]
- Willis-Owen, C.A.; Subramanian, P.; Kumari, P.; Houlihan-Burne, D. Effects of “bare below the elbows” policy on hand contamination of 92 hospital doctors in a district general hospital. J. Hosp. Infect. 2010, 75, 116–119. [Google Scholar] [CrossRef]
- Eveillard, M.; Joly-Guillou, M.L. Bare below the elbows and quality of hand washing: A randomised comparison study. J. Hosp. Infect. 2007, 74, 86–88. [Google Scholar]
- Haun, N.; Hooper-Lane, C.; Safdar, N. Healthcare Personnel Attire and Devices as Fomites: A Systematic Review. Infect. Control Hosp. Epidemiol. 2016, 37, 1367–1373. [Google Scholar] [CrossRef]
- Youngster, I.; Berkovitch, M.; Heyman, E.; Lazarovitch, Z.; Goldman, M. The stethoscope as a vector of infectious diseases in the paediatric division. Acta Paediatr. 2008, 97, 1253–1255. [Google Scholar] [CrossRef]
- Beckstrom, A.C.; Cleman, P.E.; Cassis-Ghavami, F.L.; Kamitsuka, M.D. Surveillance study of bacterial contamination of the parent’s cell phone in the NICU and the effectiveness of an anti-microbial gel in reducing transmission to the hands. J. Perinatol. 2013, 33, 960–963. [Google Scholar] [CrossRef] [PubMed]
- Orsi, G.B.; Natale, F.; D’Ettorre, G.; Protano, C.; Vullo, V.; De Curtis, M. Mobile phone microbial contamination among neonatal unit healthcare workers. Infect. Control Hosp. Epidemiol. 2015, 36, 487–488. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heyba, M.; Ismaiel, M.; Alotaibi, A.; Mahmoud, M.; Baqer, H.; Safar, A.; Al-Sweih, N.; Al-Taiar, A. Microbiological contamination of mobile phones of clinicians in intensive care units and neonatal care units in public hospitals in Kuwait. BMC Infect. Dis. 2011, 15, 434. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Flaherty, N.; Fenelon, L. The stethoscope and healthcare-associated infection: A snake in the grass or innocent bystander? J. Hosp. Infect. 2015, 91, 1–7. [Google Scholar] [CrossRef]
- Khodavaisy, S.; Nabili, M.; Davari, B.; Vahedi, M. Evaluation of bacterial and fungal contamination in the health care workers’ hands and rings in the intensive care unit. J. Prev. Med. Hyg. 2011, 52, 215–218. [Google Scholar]
- Kennedy, A.M.; Elward, A.M.; Fraser, V.J. Survey of Knowledge, Beliefs, and Practices of Neonatal Intensive Care Unit Healthcare Workers Regarding Nosocomial Infections, Central Venous Catheter Care, and Hand Infection Control and Hospital Epidemiology Survey of Knowledge, Beliefs, and Practices. Infect. Control Hosp. Epidemiol. 2004, 25, 747–752. [Google Scholar] [CrossRef] [Green Version]
- Rogers, E.; Alderdice, F.; McCall, E.; Jenkins, J.; Craig, S. Reducing nosocomial infections in neonatal intensive care. J. Matern.-Fetal Neonatal Med. 2010, 23, 1039–1046. [Google Scholar] [CrossRef]
- Li, Q.-F.; Xu, H.; Ni, X.-P.; Lin, R.; Jin, H.; Wei, L.-Y.; Liu, D.; Shen, L.-H.; Zha, J.; Xu, X.-F.; et al. Impact of relocation and environmental cleaning on reducing the incidence of healthcare-associated infection in NICU. World J. Pediatr. 2017, 13, 217–221. [Google Scholar] [CrossRef]
- Cohen, R.; Babushkin, F.; Shimoni, Z.; Cohen, S.; Litig, E.; Shapiro, M.; Adler, A.; Paikin, S. Water faucets as a source of Pseudomonas aeruginosa infection and colonization in neonatal and adult intensive care unit patients. Am. J. Infect. Control 2017, 45, 206–209. [Google Scholar] [CrossRef]
- Fusch, C.; Pogorzelski, D.; Main, C.; Meyer, C.-L.; El Helou, S.; Mertz, D. Self-disinfecting sink drains reduce the Pseudomonas aeruginosa bioburden in a neonatal intensive care unit. Acta Paediatr. 2015, 104, e344–e349. [Google Scholar] [CrossRef]
- Parry, G.J. Relationship between probable nosocomial bacteraemia and organisational and structural factors in UK neonatal intensive care units. Qual. Saf. Health Care 2005, 14, 264–269. [Google Scholar] [PubMed] [Green Version]
- Tan, S.; Clarkson, M.; Sharkey, D. Variation in Visiting and Isolation Policies in Neonatal Units. Pediatr. Infect. Dis. J. 2017, 37, e20–e22. [Google Scholar] [CrossRef] [PubMed]
- Aiello, A.E.; Cimiotti, J.; Della-Latta, P.; Larson, E.L.; Mailman, J.L. A comparison of the bacteria found on the hands of “homemakers” and neonatal intensive care unit nurses. J. Hosp. Infect. 2003, 54, 310–315. [Google Scholar] [CrossRef]
- Wittrock, B.; Lavin, M.A.; Pierry, D.; Thomson, R.; Wurtz, R. Parents as a Vector for Nosocomial Infection in the Neonatal Intensive Care Unit. Infect. Control Hosp. Epidemiol. 2001, 22, 472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peluso, A.M.; Harnish, B.A.; Miller, N.S.; Cooper, E.R.; Fujii, A.M. Effect of young sibling visitation on respiratory syncytial virus activity in a NICU. J. Perinatol. 2015, 35, 627–630. [Google Scholar] [CrossRef]
- Horikoshi, Y.; Okazaki, K.; Miyokawa, S.; Kinoshita, K.; Higuchi, H.; Suwa, J.; Aizawa, Y.; Fukuoka, K. Sibling visits and viral infection in the neonatal intensive care unit. Pediatr. Int. 2018, 60, 153–156. [Google Scholar] [CrossRef]
- Schünemann, H.J.; Vist, G.E.; Higgins, J.P.T.; Santesso, N.; Deeks, J.J.; Glasziou, P.; Akl, E.A.; Guyatt, G.H. Chapter 15, Interpreting results and drawing conclusions. In Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (Updated February 2021); Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2021; Available online: www.training.cochrane.org/handbook (accessed on 2 February 2022).
- Burns, P.B.; Rohrich, R.J.; Chung, K.C. The levels of evidence and their role in evidence-based medicine. Plast. Reconstr. Surg. 2011, 128, 305–310. [Google Scholar] [CrossRef] [Green Version]
| Domain | Description |
|---|---|
| Demographic data | NICU size, presence of trainees, academic affiliation, years of experience |
| Physical barriers | Hand hygiene, gloving and gowns |
| Attire | White coat, neck ties, jewelry, bare elbows |
| Mobile phones | Regulation of use and practice policy |
| Environment | Visitors, parents’ hand hygiene, toy sharing |
| Facility | Sterile water use, self-disinfecting sinks |
| Hand hygiene efforts | Methods to promote compliance and ensure long-term adoption of hand hygiene |
| Survey Question * | 0–20 (n = 57) | 21–40 (n = 119) | 41–80 (n = 143) | 81+ (n = 45) | p-Value |
|---|---|---|---|---|---|
| Hand hygiene policy | 57 (100.00%) | 118 (99.16%) | 143 (100.00%) | 45 (100.00%) | 0.5591 |
| Non-sterile gloves policy | 19 (33.33%) | 57 (47.90%) | 76 (53.15%) | 18 (40.00%) | 0.0613 |
| Non-sterile gowns policy | 1 (1.75%) | 10 (8.40%) | 3 (2.10%) | 0 (0.00%) | 0.0159 |
| Patient-dedicated stethoscope | 1 (1.75%) | 1 (0.84%) | 1 (0.70%) | 0 (0.00%) | 0.8000 |
| Sterile gloves for <28 weeks GA | 0 (0.00%) | 1 (0.84%) | 0 (0.00%) | 0 (0.00%) | 0.5591 |
| Bare below elbows | 0 (0.00%) | 0 (0.00%) | 1 (0.70%) | 0 (0.00%) | 0.6708 |
| No white coat policy | 29 (50.88%) | 74 (62.18%) | 94 (65.73%) | 24 (53.33%) | 0.1748 |
| No unsecured neck ties policy | 21 (36.84%) | 44 (36.97%) | 53 (37.06%) | 11 (24.44%) | 0.4379 |
| No jewelry policy | 40 (70.18%) | 83 (69.75%) | 102 (71.33%) | 33 (73.33%) | 0.9721 |
| Bare bones (short sleeves) policy | 37 (64.91%) | 82 (68.91%) | 101 (70.63%) | 29 (64.44%) | 0.8038 |
| Pre-Examination stethoscope disinfection policy | 30 (52.63%) | 55 (46.22%) | 61 (42.66%) | 19 (42.22%) | 0.6037 |
| None of the above 5 policies | 8 (14.04%) | 10 (8.40%) | 9 (6.29%) | 5 (11.11%) | 0.3351 |
| Young relatives’ access restricted policy | 52 (91.23%) | 96 (80.67%) | 117 (81.82%) | 35 (77.78%) | 0.2607 |
| Parents perform hand hygiene policy | 42 (73.68%) | 91 (76.47%) | 108 (75.52%) | 28 (62.22%) | 0.2855 |
| Sharing of toys/utensils is prohibited policy | 36 (63.16%) | 67 (56.30%) | 77 (53.85%) | 22 (48.89%) | 0.5051 |
| No environmental policies in place | 3 (5.26%) | 7 (5.88%) | 9 (6.29%) | 1 (2.22%) | 0.7664 |
| Sterile water used for bathing policy | 1 (1.75%) | 8 (6.72%) | 20 (13.99%) | 7 (15.56%) | 0.0196 |
| Self-disinfecting sink drain policy | 1 (1.75%) | 6 (5.04%) | 4 (2.80%) | 2 (4.44%) | 0.6499 |
| Do not know facility policies | 26 (45.61%) | 47 (39.50%) | 79 (55.24%) | 26 (57.78%) | 0.0424 |
| No facility policies (prior 3 rows) | 30 (52.63%) | 60 (50.42%) | 43 (30.07%) | 11 (24.44%) | 0.0002 |
| Increasing accessibility to alcohol based hand rubs | 55 (96.49%) | 118 (99.16%) | 140 (97.90%) | 43 (95.56%) | 0.4682 |
| Installing/increasing posters/reminders around NICU | 7 (64.91%) | 97 (81.51%) | 112 (78.32%) | 36 (80.00%) | 0.0901 |
| Reducing alcohol application time < 30 s | 5 (8.77%) | 21 (17.65%) | 19 (13.29%) | 7 (15.56%) | 0.4421 |
| Clustering of nursing procedures | 46 (80.70%) | 85 (71.43%) | 93 (65.03%) | 29 (64.44%) | 0.1404 |
| No compliance policies (prior 4 rows) | 1 (1.75%) | 1 (0.84%) | 1 (0.70%) | 1 (2.22%) | 0.7937 |
| Periodic performance feedback to promote adoption | 26 (45.61%) | 75 (63.03%) | 84 (58.74%) | 28 (62.22%) | 0.1602 |
| Periodic audit reports to promote adoption | 15 (26.32%) | 70 (58.82%) | 84 (58.74%) | 30 (66.67%) | < 0.0001 |
| Periodic hand hygiene course to promote adoption | 16 (28.07%) | 38 (31.93%) | 36 (25.17%) | 16 (35.56%) | 0.4811 |
| Courses during grand rounds to promote adoption | 9 (15.79%) | 22 (18.49%) | 22 (15.38%) | 9 (20.00%) | 0.8505 |
| None of the above to promote adoption (prior 4 rows) | 17 (29.82%) | 20 (16.81%) | 26 (18.18%) | 5 (11.11%) | 0.0837 |
| Other methods to promote adoption | 2 (3.51%) | 4 (3.36%) | 6 (4.20%) | 1 (2.22%) | 0.9370 |
| Surgical scrubbing for all is best policy | 23 (40.35%) | 42 (35.29%) | 41 (28.67%) | 10 (22.22%) | 0.1623 |
| Alcohol based hand rubs is best policy | 3 (5.26%) | 18 (15.13%) | 41 (28.67%) | 10 (22.22%) | 0.0009 |
| Soap based hand washing is best policy | 26 (45.61%) | 55 (46.22%) | 61 (42.66%) | 22 (48.89%) | 0.8799 |
| Other things are best policy | 6 (10.53%) | 9 (7.56%) | 9 (6.29%) | 5 (11.11%) | 0.6395 |
| Country | Intervention | Measured Outcome | Results |
|---|---|---|---|
| US (2002) [29] | Posters, Feedback | Compliance | 47% to 85% |
| China (2004) [30] | Posters, Feedback | Infection rate | 17 to 9 per 100 admission |
| Thailand (2005) [31] | Multilevel | Compliance | 35% to 50% |
| Switzerland (2007) [32] | Posters, Feedback | Compliance | 42% to 55% |
| Netherlands (2011) [33] | Multimodal | Compliance | 23% to 50% |
| Netherlands (2012) [34] | Screensavers | Compliance | 63% to 71% |
| Canada (2013) [35] | Multimodal | Compliance | 50 to76% |
| LMICs (2013) [36] | Multimodal | Compliance | 48% to 71% |
| USA (2013) [37] | Failure mode effectiveness | Compliance | 50% to 84% |
| India (2015) [38] | Posters, Feedback | Sepsis rate | 96 to 47 per 1000 patient days |
| Iran (2015) [39] | Multimodal | Compliance | 30% to 70% |
| Nepal (2017) [40] | Over basin video | Compliance | 9% to 68% |
| US (2018) [41] | Over basin video | Compliance | 42% to 72% |
| Mexico (2019) [26] | Multimodal | Compliance | 45% to 79% |
| Compliance Interventions (n = 364) | ||
| Intervention | Institution Utilization | Support |
| Increasing basin accessibility | 97% | 98.5% |
| Posters and reminders | 77% | 86.1% |
| Alcohol application < 30 s | 14% | 40% |
| Clustering of nursing procedures | 69% | 88% |
| Sustainability interventions (n = 364) | ||
| Performance feedback | 58% | 84% |
| Emailed audit reports | 54% | 78% |
| Mandatory courses | 29% | 49% |
| Grand rounds presentations | 17% | 39% |
| None of the above | 18% | n/a |
| Survey Question * | 0–5 (n = 98) | 6–10 (n = 35) | 11–20 (n = 67) | 20+ (n = 164) | p-Value |
|---|---|---|---|---|---|
| Opinion on effect of hand hygiene | 5.00 (0.00) | 5.00 (0.00) | 4.96 (0.27) | 4.99 (0.11) | 0.1940 |
| Opinion on non-sterile gloves | 3.73 (1.04) | 3.69 (0.96) | 3.52 (1.12) | 3.38 (1.02) | 0.0522 |
| Opinion on non-sterile gowns | 2.67 (0.88) | 2.66 (0.59) | 2.49 (0.89) | 2.16 (0.86) | <0.0001 |
| Opinion on no white coat in NICU | 4.47 (0.79) | 4.40 (0.69) | 4.33 (0.84) | 3.92 (1.09) | <0.0001 |
| Opinion on no unsecured neck ties | 4.14 (0.95) | 4.00 (0.87) | 4.00 (0.85) | 3.71 (0.99) | 0.0027 |
| Opinion on no jewelry in NICU | 4.03 (0.99) | 3.94 (1.00) | 4.42 (0.82) | 4.29 (0.90) | 0.0105 |
| Opinion of bare elbows in NICU | 4.27 (0.86) | 4.29 (0.83) | 4.19 (0.94) | 4.30 (0.86) | 0.8532 |
| Opinion of pre-examination stethoscope disinfection | 4.27 (0.86) | 4.11 (0.90) | 4.15 (0.93) | 4.26 (0.87) | 0.6911 |
| Opinion of limiting Young relatives’ access to NICU | 4.43 (0.81) | 4.34 (0.91) | 4.22 (1.03) | 4.26 (0.98) | 0.4597 |
| Opinion of parents performing hand hygiene | 4.60 (0.67) | 4.34 (0.80) | 4.64 (0.64) | 4.52 (0.69) | 0.1614 |
| Opinion of not allowing shared toys or utensils | 4.31 (0.88) | 3.97 (0.89) | 4.39 (0.85) | 4.26 (0.83) | 0.1253 |
| Opinion of sterile water being used for baths | 2.97 (0.95) | 3.09 (0.85) | 2.82 (0.85) | 2.91 (0.79) | 0.4692 |
| Opinion of self-disinfecting sink drains in NICU | 3.34 (0.73) | 3.26 (0.66) | 3.21 (0.57) | 3.23 (0.67) | 0.5783 |
| Opinion of increasing accessibility to alcohol based hand rubs | 4.92 (0.28) | 4.86 (0.43) | 4.91 (0.29) | 4.78 (0.52) | 0.0378 |
| Opinion of installing/increasing posters/reminders around NICU | 4.26 (0.80) | 4.37 (0.77) | 4.54 (0.64) | 4.24 (0.85) | 0.0588 |
| Opinion of reducing alcohol application time below 30 s | 3.51 (0.82) | 3.60 (0.88) | 3.64 (0.85) | 3.38 (0.81) | 0.1161 |
| Opinion of clustering of nursing procedures to reduce patient contacts | 4.40 (0.74) | 4.20 (0.76) | 4.30 (0.84) | 4.17 (0.87) | 0.1705 |
| Opinion of periodic performance feedback w/face to face interaction | 4.16 (0.74) | 4.31 (0.68) | 4.45 (0.68) | 4.26 (0.83) | 0.1296 |
| Opinion of distributing periodic audit reports | 4.05 (0.83) | 4.17 (0.75) | 4.22 (0.78) | 4.09 (0.80) | 0.5375 |
| Opinion of effectiveness of periodic mandatory hand hygiene courses | 3.30 (1.07) | 3.51 (0.98) | 3.66 (1.05) | 3.60 (0.97) | 0.0696 |
| Opinion of hand hygiene presentations during grand rounds | 3.27 (1.05) | 3.31 (1.11) | 3.45 (0.97) | 3.28 (0.99) | 0.6674 |
| Policy | Institutional Utilization (n = 364) | Support (n = 364) |
|---|---|---|
| No white coat | 60% | 79% |
| No unsecured ties | 35% | 64% |
| No jewelry | 70% | 80% |
| Bare elbows | 68% | 80% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alslaim, H.S.; Chan, J.; Saleem-Rasheed, F.; Ibrahim, Y.; Karabon, P.; Novotny, N. Discordance among Belief, Practice, and the Literature in Infection Prevention in the NICU. Children 2022, 9, 492. https://doi.org/10.3390/children9040492
Alslaim HS, Chan J, Saleem-Rasheed F, Ibrahim Y, Karabon P, Novotny N. Discordance among Belief, Practice, and the Literature in Infection Prevention in the NICU. Children. 2022; 9(4):492. https://doi.org/10.3390/children9040492
Chicago/Turabian StyleAlslaim, Hossam S., Jonathan Chan, Fozia Saleem-Rasheed, Yousef Ibrahim, Patrick Karabon, and Nathan Novotny. 2022. "Discordance among Belief, Practice, and the Literature in Infection Prevention in the NICU" Children 9, no. 4: 492. https://doi.org/10.3390/children9040492
APA StyleAlslaim, H. S., Chan, J., Saleem-Rasheed, F., Ibrahim, Y., Karabon, P., & Novotny, N. (2022). Discordance among Belief, Practice, and the Literature in Infection Prevention in the NICU. Children, 9(4), 492. https://doi.org/10.3390/children9040492






