Intercultural Differences in the Development of Pediatric Medical Traumatic Stress (PMTS) in Children Following Surgical Hospitalization
Abstract
:1. Introduction
1.1. Pediatric Medical Traumatic Stress (PMTS)—Description of the Phenomenon
1.2. Prevalence of PMTS
1.3. Risk Factors for the Development of Pediatric Medical Traumatic Stress in Children after Hospitalization
1.4. Post-Traumatic Symptoms in Children in Arab Society
1.5. Frequency of Injuries among Arab and Jewish Populations in Israel
1.6. Unique Characteristics of Hospitalized Arab Children
1.7. The Effect of Intercultural Variables on PTSD
1.8. Rationale and Research Hypotheses
2. Method
2.1. Participants
2.2. Measures
- The screening questionnaire (PMTSSQ) [41].
- 2.
- UCLA PTSD Reaction Index for DSM-5 Parent/Caregiver Version for Children Age 6 Years and Younger [42].
- 3.
- Young Child PTSD Checklist (YCPC) [44].
2.3. Procedure
3. Results
3.1. Group Differences
3.2. PTSD Predictors among Arabs and Jews
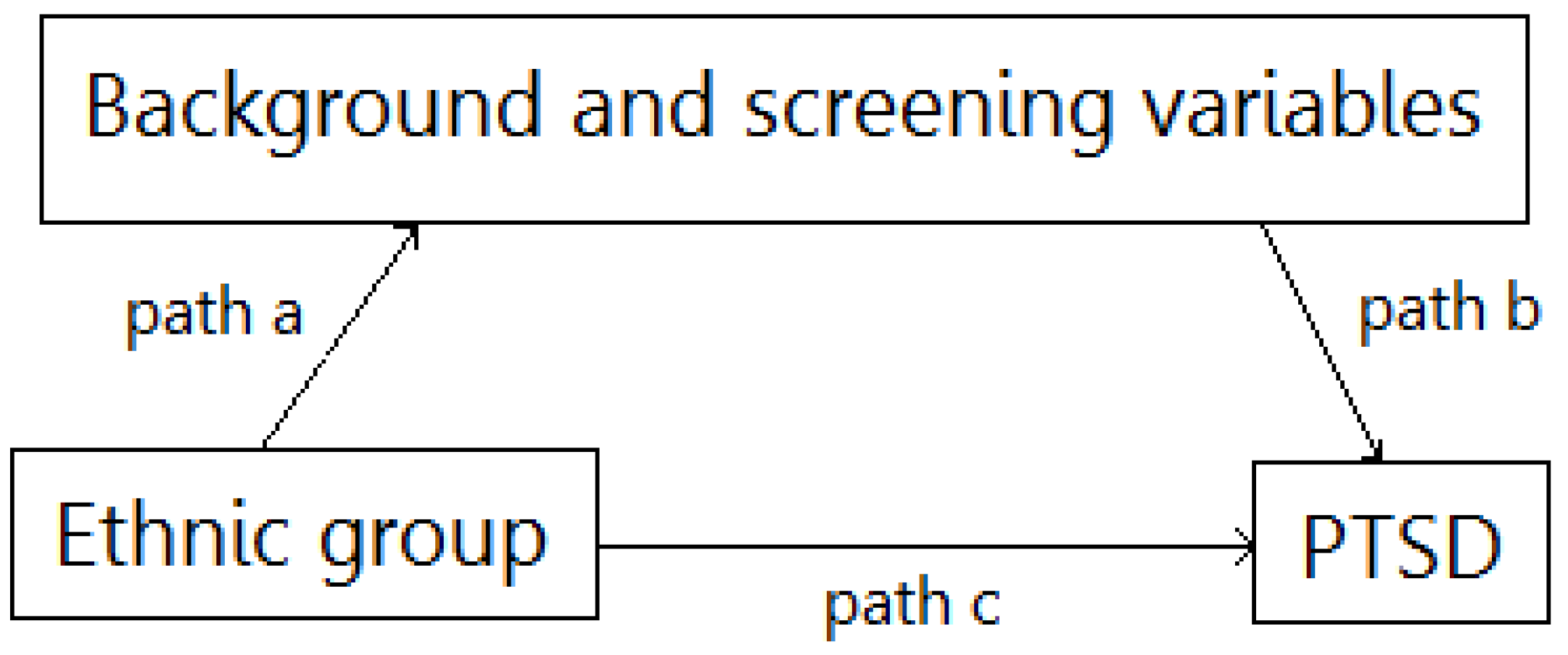
3.3. Mediation Analyses
4. Discussion
The Significance of the Findings and Their Theoretical and Clinical Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Rennick, J.E.; Johnston, C.C.; Dougherty, G.; Platt, R.; Ritchie, J.A. Children’s psychological responses after critical illness and exposure to invasive technology. J. Dev. Behav. Pediatrics 2002, 23, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Shea, T.; Athanasakos, E.; Cleeve, S.; Croft, N.; Gibbs, D. Pediatric Medical Traumatic Stress. J. Child Life Psychosoc. Theory Pract. 2021, 2, 42–54. [Google Scholar] [CrossRef]
- Watson, R.S.; Choong, K.; Colville, G.; Crow, S.; Dervan, L.A.; Hopkins, R.O.; Curley, M.A. Life after critical illness in children—toward an understanding of pediatric post-intensive care syndrome. J. Pediatrics 2018, 198, 16–24. [Google Scholar] [CrossRef]
- Price, J.; Kassam-Adams, N.; Alderfer, M.A.; Christofferson, J.; Kazak, A.E. Systematic review: A reevaluation and update of the integrative (trajectory) model of pediatric medical traumatic stress. J. Pediatric Psychol. 2016, 41, 86–97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Young, A.C.; Paterson, R.S.; Brown, E.A.; Egberts, M.R.; Le Brocque, R.M.; Kenardy, J.A.; Haag, A.C. Topical review: Medical trauma during early childhood. J. Pediatric Psychol. 2021, 46, 739–746. [Google Scholar] [CrossRef]
- Judge, D.; Nadel, S.; Vergnaud, S.; Garralda, E.M. Psychiatric adjustment following meningococcal disease treated on a PICU. Intensive Care Med. 2002, 28, 648–650. [Google Scholar] [CrossRef] [PubMed]
- Forgey, M.; Bursch, B. Assessment and management of pediatric iatrogenic medical trauma. Curr. Psychiatry Rep. 2013, 15, 340. [Google Scholar] [CrossRef]
- Rennick, J.E.; Dougherty, G.; Chambers, C.; Stremler, R.; Childerhose, J.E.; Stack, D.M.; Hutchison, J. Children’s psychological and behavioral responses following pediatric intensive care unit hospitalization: The caring intensively study. BMC Pediatrics 2014, 14, 276. [Google Scholar] [CrossRef] [Green Version]
- Rennick, J.E.; Rashotte, J. Psychological outcomes in children following pediatric intensive care unit hospitalization: A systematic review of the research. J. Child Health Care 2009, 13, 128–149. [Google Scholar] [CrossRef]
- National Child Traumatic Stress Network. Definitions of medical traumatic stress. In Proceedings of the Medical Traumatic Stress Working Group Meeting, Philadelphia, PA, USA, 2003. [Google Scholar]
- Kazak, A.E.; Kassam-Adams, N.; Schneider, S.; Zelikovsky, N.; Alderfer, M.A.; Rourke, M. An integrative model of pediatric medical traumatic stress. J. Pediatric Psychol. 2006, 31, 343–355. [Google Scholar] [CrossRef] [Green Version]
- De Young, A.C.; Kenardy, J.A.; Cobham, V.E.; Kimble, R. Prevalence, comorbidity and course of trauma reactions in young burn-injured children. J. Child Psychol. Psychiatry 2012, 53, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Banh, M.K.; Saxe, G.; Mangione, T.; Horton, N.J. Physician-reported practice of managing childhood posttraumatic stress in pediatric primary care. Gen. Hosp. Psychiatry 2008, 30, 536–545. [Google Scholar] [CrossRef] [PubMed]
- Marsac, M.L.; Kassam-Adams, N.; Hildenbrand, A.K.; Nicholls, E.; Winston, F.K.; Leff, S.S.; Fein, J. Implementing a trauma-informed approach in pediatric health care networks. JAMA Pediatrics 2016, 170, 70–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dueweke, A.R.; Hanson, R.F.; Wallis, E.; Fanguy, E.; Newman, C. Training pediatric primary care residents in trauma-informed care: A feasibility trial. Clin. Pediatrics 2019, 58, 1239–1249. [Google Scholar] [CrossRef]
- Le Brocque, R.M.; Dow, B.L.; McMahon, H.; Crothers, A.L.; Kenardy, J.A.; Williams, T.J.; Long, D.A. The course of posttraumatic stress in children: Examination of symptom trajectories and predictive factors following admission to pediatric intensive care. Pediatric Crit. Care Med. 2020, 21, e399–e406. [Google Scholar] [CrossRef]
- Ari, A.B.; Margalit, D.; Udassin, R.; Benarroch, F. Traumatic stress among school-aged pediatric surgery patients and their parents. Eur. J. Pediatric Surg. 2019, 29, 437–442. [Google Scholar]
- Ari, A.B.; Peri, T.; Margalit, D.; Galili-Weisstub, E.; Udassin, R.; Benarroch, F. Surgical procedures and pediatric medical traumatic stress (PMTS) syndrome: Assessment and future directions. J. Pediatric Surg. 2018, 53, 1526–1531. [Google Scholar] [CrossRef]
- Ben-Ari, A.; Benarroch, F.; Sela, Y.; Margalit, D. Risk factors for the development of medical stress syndrome following surgical intervention. J. Pediatric Surg. 2020, 55, 1685–1690. [Google Scholar] [CrossRef]
- Tillery, R.; Willard, V.W.; Long, A.; Phipps, S. Posttraumatic stress in young children with cancer: Risk factors and comparison with healthy peers. Pediatric Blood Cancer 2019, 66, e27775. [Google Scholar] [CrossRef]
- Haag, A.C.; Landolt, M.A. Young children’s acute stress after a burn injury: Disentangling the role of injury severity and parental acute stress. J. Pediatric Psychol. 2017, 42, 861–870. [Google Scholar] [CrossRef]
- Brown, E.A.; De Young, A.; Kimble, R.; Kenardy, J. Impact of parental acute psychological distress on young child pain-related behavior through differences in parenting behavior during pediatric burn wound care. J. Clin. Psychol. Med. Settings 2019, 26, 516–529. [Google Scholar] [CrossRef] [PubMed]
- Small, L.; Melnyk, B.M. Early predictors of post-hospital adjustment problems in critically Ill young children. Res. Nurs. Health 2006, 29, 622–635. [Google Scholar] [CrossRef] [PubMed]
- De Young, A.C.; Hendrikz, J.; Kenardy, J.A.; Cobham, V.E.; Kimble, R.M. Prospective evaluation of parent distress following pediatric burns and identification of risk factors for young child and parent posttraumatic stress disorder. J. Child Adolesc. Psychopharmacol. 2014, 24, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Stoddard, F.J., Jr.; Sorrentino, E.A.; Ceranoglu, T.A.; Saxe, G.; Murphy, J.M.; Drake, J.E.; Sheridan, R.L. Preliminary evidence for the effects of morphine on posttraumatic stress disorder symptoms in one-to four-year-olds with burns. J. Burn Care Res. 2009, 30, 836–843. [Google Scholar] [CrossRef] [PubMed]
- Graf, A.; Schiestl, C.; Landolt, M.A. Posttraumatic stress and behavior problems in infants and toddlers with burns. J. Pediatric Psychol. 2011, 36, 923–931. [Google Scholar] [CrossRef]
- Assari, S. Family socioeconomic status and exposure to childhood trauma: Racial differences. Children 2020, 7, 57. [Google Scholar] [CrossRef]
- El-Khodary, B.; Samara, M.; Askew, C. Traumatic events and PTSD among Palestinian children and adolescents: The effect of demographic and socioeconomic factors. Front. Psychiatry 2020, 11, 4. [Google Scholar] [CrossRef]
- Afana, A. Problems in Applying Diagnostic Concepts of PTSD and Trauma in the Middle East. Arab J. Psychiatry 2012, 23, 28–34. [Google Scholar]
- Thabet, A.M.; Thabet, S.S.; Vostanis, P. The relationship between war trauma, PTSD, depression, and anxiety among Palestinian children in the Gaza Strip. Health Sci. J. 2016, 10, 1–8. [Google Scholar]
- Al Jadili, M.; Thabet, A. The relationship Between Post Traumatic Stress Disorder and Coping Strategies among patients with Cancer in Gaza Strip. J. Nurs. Health Stud. 2017, 2, 1–10. [Google Scholar] [CrossRef]
- Abdelaziz, M.T.; Mansour, M. The relationship between PTSD, Anxiety and Depression in Palestinian Children with Cancer and Mental Health of Mothers. J. Psychol. Brain Stud. 2017, 2, 1–9. [Google Scholar]
- Falk, A.; Or, D.; Khalif, A. Child Injuries in Israel: Nation TEREM Report 2020; TEREM Organization; The Ministry of Health: Tel-aviv, Israel, 2020; pp. 76–100. [Google Scholar]
- Baron-Epel, O.; Ivancovsky, M. A socio-ecological model for unintentional injuries in minorities: A case study of Arab Israeli children. Int. J. Inj. Control Saf. Promot. 2015, 22, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Ruglass, L.M.; Morgan-López, A.A.; Saavedra, L.M.; Hien, D.A.; Fitzpatrick, S.; Killeen, T.K.; López-Castro, T. Measurement nonequivalence of the Clinician-Administered PTSD Scale by race/ethnicity: Implications for quantifying posttraumatic stress disorder severity. Psychol. Assess. 2020, 32, 1015. [Google Scholar] [CrossRef] [PubMed]
- Al-Krenawi, A. Mental health practice in Arab countries. Curr. Opin. Psychiatry 2005, 18, 560–564. [Google Scholar] [CrossRef]
- Mohammadzadeh, M.; Awang, H.; Mirzaei, F. Mental health stigma among Middle Eastern adolescents: A protocol for a systematic review. J. Psychiatr. Ment. Health Nurs. 2020, 27, 829–837. [Google Scholar] [CrossRef]
- Ungar, M. Resilience, trauma, context, and culture. Trauma Violence Abuse 2013, 14, 255–266. [Google Scholar] [CrossRef]
- Fasfous, A.F.; Peralta-Ramírez, I.; Pérez-García, M. Symptoms of PTSD among children living in war zones in same cultural context and different situations. J. Muslim Mental Health 2013, 7. [Google Scholar] [CrossRef] [Green Version]
- Noronha, D.O.; Faust, J. Identifying the variables impacting post-burn psychological adjustment: A meta-analysis. J. Pediatric Psychol. 2007, 32, 380–391. [Google Scholar] [CrossRef]
- Ben-Ari, A.; Ben-David, S.; Margalit, D.; Aloni, R.; Benarroch, F. Screening for risk factors for post-surgical traumatic stress in children: The “Pediatric Medical Traumatic Stress Screening Questionnaire (PMTSSQ)”. J. Pediatric Surg. 2022; in press. [Google Scholar]
- Steinberg, A.M.; Brymer, M.J.; Kim, S.; Briggs, E.C.; Ippen, C.G.; Ostrowski, S.A.; Pynoos, R.S. Psychometric properties of the UCLA PTSD reaction index: Part I. J. Trauma. Stress 2013, 26, 10–18. [Google Scholar] [CrossRef]
- Elhai, J.D.; Layne, C.M.; Steinberg, A.M.; Brymer, M.J.; Briggs, E.C.; Ostrowski, S.A.; Pynoos, R.S. Psychometric properties of the UCLA PTSD reaction index. Part II: Investigating factor structure findings in a national clinic-referred youth sample. J. Trauma. Stress 2013, 26, 10–18. [Google Scholar] [CrossRef]
- Scheeringa, M.S. Young Child PTSD Checklist (YCPC); Tulane University: New Orleans, LA, USA, 2013. [Google Scholar]
- Vasileva, M.; Petermann, F. Mental health needs and therapeutic service utilization of young children in foster care in Germany. Child. Youth Serv. Rev. 2017, 75, 69–76. [Google Scholar] [CrossRef]
- Brislin, R.W. The wording and translation of research instruments. In Field Methods in Cross-Cultural Research; Lonner, W.J., Berry, J.W., Eds.; Sage Publications: Newbury Park, CA, USA, 1986. [Google Scholar]
- Olsson, K.A.; Kenardy, J.A.; De Young, A.C.; Spence, S.H. Predicting children’s post-traumatic stress symptoms following hospitalization for accidental injury: Combining the Child Trauma Screening Questionnaire and heart rate. J. Anxiety Disord. 2008, 22, 1447–1453. [Google Scholar] [CrossRef] [PubMed]
- Proctor, L.J. Children growing up in a violent community: The role of the family. Aggress. Violent Behav. 2006, 11, 558–576. [Google Scholar] [CrossRef]
- Kramer, D.N.; Hertli, M.B.; Landolt, M.A. Evaluation of an early risk screener for PTSD in preschool children after accidental injury. Pediatrics 2013, 132, 945–951. [Google Scholar] [CrossRef]
- Valentine, S.E.; Marques, L.; Wang, Y.; Ahles, E.M.; De Silva, L.D.; Alegría, M. Gender differences in exposure to potentially traumatic events and diagnosis of posttraumatic stress disorder (PTSD) by racial and ethnic group. Gen. Hosp. Psychiatry 2019, 61, 60–68. [Google Scholar] [CrossRef]
- Luckett, T.; Goldstein, D.; Butow, P.N.; Gebski, V.; Aldridge, L.J.; McGrane, J.; King, M.T. Psychological morbidity and quality of life of ethnic minority patients with cancer: A systematic review and meta-analysis. Lancet Oncol. 2011, 12, 1240–1248. [Google Scholar] [CrossRef]
- Marie, M.; SaadAdeen, S.; Battat, M. Anxiety disorders and PTSD in Palestine: A literature review. BMC Psychiatry 2020, 20, 509. [Google Scholar] [CrossRef]
- Popper-Giveon, A.; Keshet, Y.; Liberman, I. Israeli Arabs in health and welfare professions: An ethnic and gender oriented view of representation and employment. Soc. Secur. J. 2015, 97, 95–126. [Google Scholar]
- Central Bureau of Statistics. Live Birth, Deaths, Natural Reproduction, Infant Death and Stillbirths, by Population Group. 2013. Available online: https://www.cbs.gov.il/shnaton61/st06_01.pdf (accessed on 15 January 2022).
- Central Bureau of Statistics. Life Expectancy by Sex, Religion and Population Group; Central Bureau of Statistics: Kathmandu, Nepal, 2013.
- Unger, S. Social and Structural Determinants and Their Associations with Emergency Department Use and Patient Experience. Master’s Thesis, Ben-Gurion University of the Negev, Beer Sheva, Israel, 2020. [Google Scholar]
- Borkan, J.M.; Morad, M.; Shvarts, S. Universal health care? The views of Negev Bedouin Arabs on health services. Health Policy Plan. 2000, 15, 207–216. [Google Scholar] [CrossRef] [Green Version]
- Haag, A.C.; Landolt, M.A.; Kenardy, J.A.; Schiestl, C.M.; Kimble, R.M.; De Young, A.C. Preventive intervention for trauma reactions in young injured children: Results of a multi-site randomised controlled trial. J. Child Psychol. Psychiatry 2020, 61, 988–997. [Google Scholar] [CrossRef] [PubMed]
- Trickey, D.; Siddaway, A.P.; Meiser-Stedman, R.; Serpell, L.; Field, A.P. A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clin. Psychol. Rev. 2012, 32, 122–138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Young, A.C.; Kenardy, J.A.; Cobham, V.E. Diagnosis of posttraumatic stress disorder in preschool children. J. Clin. Child Adolesc. Psychol. 2011, 40, 375–384. [Google Scholar] [CrossRef] [PubMed]
- Phipps, S.; Long, A.; Hudson, M.; Rai, S.N. Symptoms of post-traumatic stress in children with cancer and their parents: Effects of informant and time from diagnosis. Pediatric Blood Cancer 2005, 45, 952–959. [Google Scholar] [CrossRef] [PubMed]
- Yost, K.J.; Hahn, E.A.; Zaslavsky, A.M.; Ayanian, J.Z.; West, D.W. Predictors of health-related quality of life in patients with colorectal cancer. Health Qual. Life Outcomes 2008, 6, 66. [Google Scholar] [CrossRef] [Green Version]
- Kagawa-Singer, M.; Valdez Dadia, A.; Yu, M.C.; Surbone, A. Cancer, culture, and health disparities: Time to chart a new course? CA A Cancer J. Clin. 2010, 60, 12–39. [Google Scholar] [CrossRef]
| Jews (n = 151) | Arabs (n = 102) | Group Differences | |
|---|---|---|---|
| Age of child (years, M [SD]) | 2.89 (1.52) | 3.12 (1.60) | t(250) = −1.15 |
| SES (difficulties, n [%]) | 32 (22.4%) | 47 (46.1%) | χ 2(1) = 15.31 *** |
| Previous trauma (M [SD]) | 1.17 (0.61) | 1.63 (1.35) | t(129.01) = 3.20 ** |
| Emergency surgery (n, %) | 48 (31.8%) | 30 (29.4%) | χ2(1) = 0.16 |
| Hospitalization duration (days, M [SD]) | 2.78 (2.39) | 7.56 (7.65) | t(114.50) = 6.10 *** |
| Child’s previous functioning ^ (M [SD]) | 1.43 (0.51) | 1.92 (1.25) | t(123.67) = 3.71 *** |
| Parental previous functioning ^ (M [SD]) | 1.55 (0.70) | 2.08 (1.25) | t(143.21) = 3.92 *** |
| Child’s anxiety level (M [SD]) | 2.07 (1.01) | 2.76 (1.58) | t(156.72) = 3.93 *** |
| Parental perception of severity (M [SD]) | 2.53 (1.07) | 2.79 (1.41) | t(176.18) = 1.59 |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. PTSD | - | ||||||||
| 2. Age of child | −0.04 | - | |||||||
| 3. SES | 0.30 ** | 0.05 | - | ||||||
| 4. Previous trauma | 0.62 *** | 0.02 | 0.33 ** | - | |||||
| 5. Surgery type | 0.68 *** | −0.07 | 0.14 | 0.44 *** | - | ||||
| 6. Hospitalization duration | 0.69 *** | −0.06 | 0.20 * | 0.39 *** | 0.49 *** | - | |||
| 7. Child’s previous functioning | 0.68 *** | 0.06 | 0.34 *** | 0.50 *** | 0.41 *** | 0.48 *** | - | ||
| 8. Parental previous functioning | 0.72 *** | 0.03 | 0.42 *** | 0.62 *** | 0.51 *** | 0.50 *** | 0.89 *** | - | |
| 9. Child’s anxiety level | 0.71 *** | −0.10 | 0.34 *** | 0.49 *** | 0.56 *** | 0.52 *** | 0.75 *** | 0.76 *** | - |
| 10. Parental severity perception | 0.79 *** | −0.09 | 0.31 ** | 0.54 *** | 0.60 *** | 0.62 *** | 0.81 *** | 0.78 *** | 0.87 *** |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. PTSD | - | ||||||||
| 2. Age of child | 0.03 | - | |||||||
| 3. SES | 0.14 | 0.00 | - | ||||||
| 4. Previous trauma | 0.15 | 0.07 | 0.07 | - | |||||
| 5. Surgery type | 0.25 ** | −0.07 | 0.01 | 0.04 | - | ||||
| 6. Hospitalization duration | 0.35 *** | −0.09 | 0.06 | −0.05 | 0.18 * | - | |||
| 7. Child’s previous functioning | 0.17 * | 0.17 * | 0.13 | 0.21 * | −0.05 | 0.00 | - | ||
| 8. Parental previous functioning | 0.16 | 0.01 | 0.25 ** | 0.02 | −0.01 | 0.08 | 0.09 | - | |
| 9. Child’s anxiety level | 0.14 | −0.12 | 0.06 | 0.05 | 0.32 *** | 0.16 | 0.18 * | 0.02 | - |
| 10. Parental severity perception | 0.26 *** | −0.12 | 0.16 | 0.21 ** | 0.38 *** | 0.20 * | 0.22 ** | 0.03 | 0.29 *** |
| Mediator | Path a | Path b | Path c | Indirect Effect (Bootstrapping) | ||||
|---|---|---|---|---|---|---|---|---|
| B (SE) | t | B (SE) | z | B (SE) | z | B (SE) | 95% CI | |
| SES | ||||||||
| Previous trauma | −0.45 (0.12) | −3.64 *** | 0.90 (0.17) | 5.29 *** | −0.80 (0.41) | −1.92 * | −0.41 (0.17) | −0.78; −0.14 |
| Surgery type | ||||||||
| Hospitalization duration | −4.79 (0.67) | −7.15 *** | 0.30 (0.005) | 5.72 *** | 0.25 (0.49) | 0.51 | −1.43 (0.40) | −2.38; −0.82 |
| Child’s previous functioning | −0.48 (0.11) | −4.27 *** | 1.30 (0.22) | 5.95 *** | −0.33 (0.46) | −0.73 | −0.63 (0.21) | −1.10; −0.28 |
| Parental previous functioning | −0.53 (0.12) | −4.35 *** | 1.25 (0.20) | 6.28 *** | −0.44 (0.45) | −0.99 | −0.67 (0.21) | −1.14; −0.31 |
| Child’s anxiety level | −0.69 (0.16) | −4.26 *** | 1.18 (0.20) | 5.97 *** | −0.20 (0.47) | −0.43 | −0.82 (0.26) | −1.42; −0.40 |
| Parental severity perception | −0.26 (0.16) | −1.68 | 1.47 (0.22) | 6.72 *** | −0.91 (0.46) | −1.96 * | −0.39 (0.26) | −0.99; 0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Masalha, B.; Ben-David, S.; Benarroch, F.; Ben-ari, A. Intercultural Differences in the Development of Pediatric Medical Traumatic Stress (PMTS) in Children Following Surgical Hospitalization. Children 2022, 9, 526. https://doi.org/10.3390/children9040526
Masalha B, Ben-David S, Benarroch F, Ben-ari A. Intercultural Differences in the Development of Pediatric Medical Traumatic Stress (PMTS) in Children Following Surgical Hospitalization. Children. 2022; 9(4):526. https://doi.org/10.3390/children9040526
Chicago/Turabian StyleMasalha, Bushra, Shiri Ben-David, Fortu Benarroch, and Amichai Ben-ari. 2022. "Intercultural Differences in the Development of Pediatric Medical Traumatic Stress (PMTS) in Children Following Surgical Hospitalization" Children 9, no. 4: 526. https://doi.org/10.3390/children9040526
APA StyleMasalha, B., Ben-David, S., Benarroch, F., & Ben-ari, A. (2022). Intercultural Differences in the Development of Pediatric Medical Traumatic Stress (PMTS) in Children Following Surgical Hospitalization. Children, 9(4), 526. https://doi.org/10.3390/children9040526







