Motor Performance in Association with Perceived Loneliness and Social Competence in 11-Year-Old Children Born Very Preterm
Abstract
:1. Introduction
2. Materials and Methods
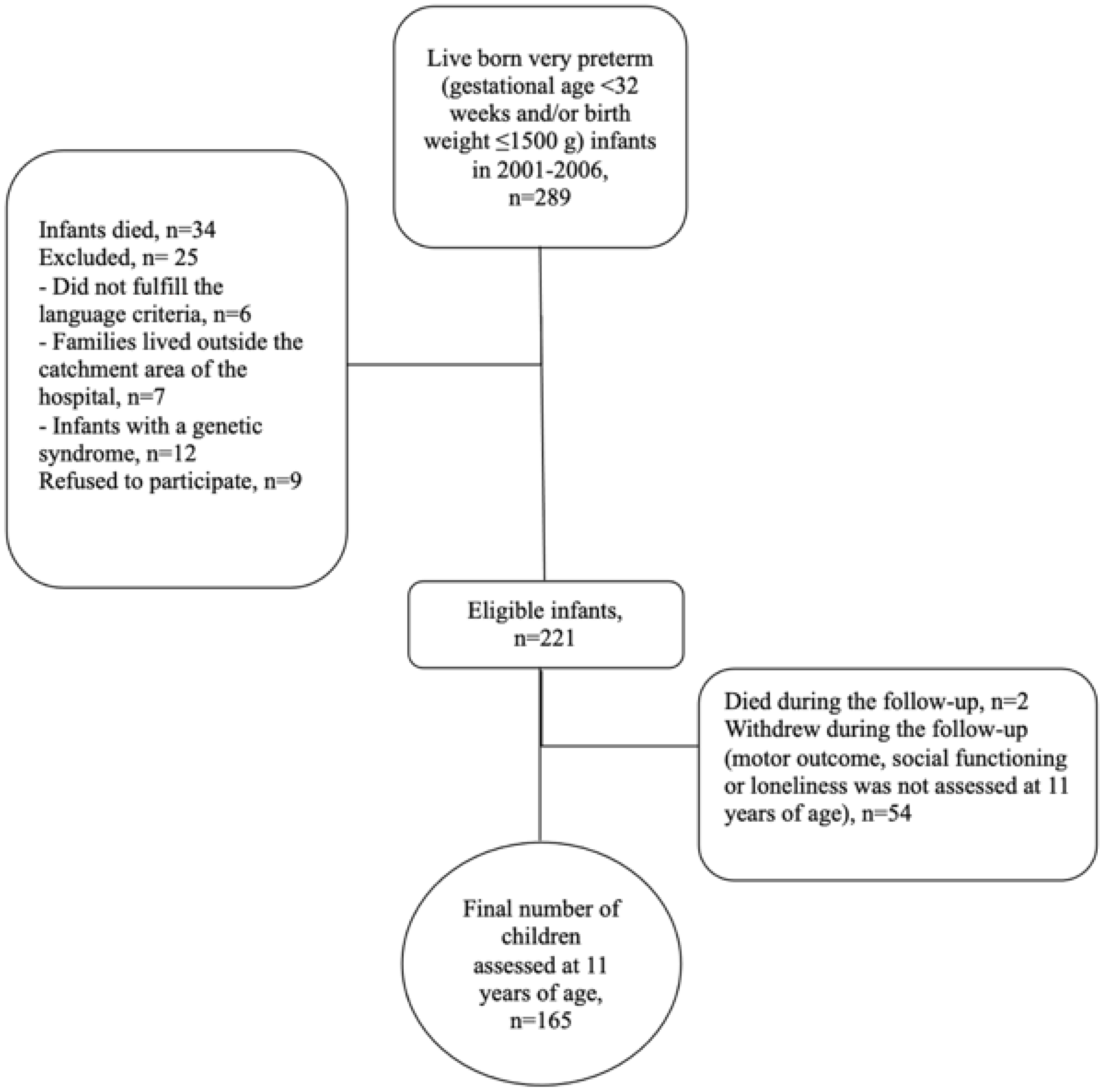
2.1. Participants
2.2. Motor Outcome
2.3. Loneliness at 11 Years of Age
2.4. Social Competence at 11 Years of Age
2.5. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- van der Pal-de Bruin, K.M.; van der Pal, S.M.; Verloove-Vanhorick, S.P.; Walther, F.J. Profiling the Preterm or VLBW Born Adolescent; Implications of the Dutch POPS Cohort Follow-up Studies. Early Hum. Dev. 2015, 91, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Zwicker, J.G.; Missiuna, C.; Harris, S.R.; Boyd, L.A. Developmental Coordination Disorder: A Review and Update. Eur. J. Paediatr. Neurol. 2012, 16, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Edwards, J.; Berube, M.; Erlandson, K.; Haug, S.; Johnstone, H.; Meagher, M.; Sarkodee-Adoo, S.; Zwicker, J.G. Developmental Coordination Disorder in School-Aged Children Born Very Preterm and/or at Very Low Birth Weight: A Systematic Review. J. Dev. Behav. Pediatrics 2011, 32, 678–687. [Google Scholar] [CrossRef] [PubMed]
- de Kieviet, J.F.; Piek, J.P.; Aarnoudse-Moens, C.S.; Oosterlaan, J. Motor Development in Very Preterm and Very Low-Birth-Weight Children From Birth to Adolescence. JAMA 2009, 302, 2235–2242. [Google Scholar] [CrossRef] [PubMed]
- Evensen, K.A.I.; Vik, T.; Helbostad, J.; Indredavik, M.S.; Kulseng, S.; Brubakk, A.M. Motor Skills in Adolescents with Low Birth Weight. Arch. Dis. Child. Fetal Neonatal Ed. 2004, 89, F451–F455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marret, S.; Marchand-Martin, L.; Picaud, J.-C.; Hascoët, J.-M.; Arnaud, C.; Rozé, J.-C.; Truffert, P.; Larroque, B.; Kaminski, M.; Ancel, P.-Y.; et al. Brain Injury in Very Preterm Children and Neurosensory and Cognitive Disabilities during Childhood: The EPIPAGE Cohort Study. PLoS ONE 2013, 8, e62683. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Platt, M.J.; Cans, C.; Johnson, A.; Surman, G.; Topp, M.; Torrioli, M.G.; Krageloh-Mann, I. Trends in Cerebral Palsy among Infants of Very Low Birthweight (<1500 g) or Born Prematurely (<32 Weeks) in 16 European Centres: A Database Study. Lancet 2007, 369, 43–50. [Google Scholar] [CrossRef]
- Sellier, E.; Platt, M.J.; Andersen, G.L.; Krägeloh-Mann, I.; de La Cruz, J.; Cans, C.; Cans, C.; van Bakel, M.; Arnaud, C.; Delobel, M.; et al. Decreasing Prevalence in Cerebral Palsy: A Multi-Site European Population-Based Study, 1980 to 2003. Dev. Med. Child Neurol. 2016, 58, 85–92. [Google Scholar] [CrossRef]
- Moore, T.; Hennessy, E.M.; Myles, J.; Johnson, S.J.; Draper, E.S.; Costeloe, K.L.; Marlow, N. Neurological and Developmental Outcome in Extremely Preterm Children Born in England in 1995 and 2006: The EPICure Studies. BMJ 2012, 345, e7961. [Google Scholar] [CrossRef] [Green Version]
- Ishii, N.; Kono, Y.; Yonemoto, N.; Kusuda, S.; Fujimura, M.; Neonatal Research Network, J. Outcomes of Infants Born at 22 and 23 Weeks’ Gestation. Pediatrics 2013, 132, 62–71. [Google Scholar] [CrossRef] [Green Version]
- Engel-Yeger, B.; Jarus, T.; Anaby, D.; Law, M. Differences in Patterns of Participation between Youths with Cerebral Palsy and Typically Developing Peers. Am. J. Occup. Ther. 2009, 63, 96–104. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jacobson, D.N.O.; Löwing, K.; Hjalmarsson, E.; Tedroff, K. Exploring Social Participation in Young Adults with Cerebral Palsy. J. Rehabil. Med. 2019, 51, 167–174. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blank, R.; Barnett, A.L.; Cairney, J.; Green, D.; Kirby, A.; Polatajko, H.; Rosenblum, S.; Smits-Engelsman, B.; Sugden, D.; Wilson, P.; et al. International Clinical Practice Recommendations on the Definition, Diagnosis, Assessment, Intervention, and Psychosocial Aspects of Developmental Coordination Disorder. Dev. Med. Child Neurol. 2019, 61, 242–285. [Google Scholar] [CrossRef] [PubMed]
- Uusitalo, K.; Haataja, L.; Nyman, A.; Ripatti, L.; Huhtala, M.; Rautava, P.; Lehtonen, L.; Parkkola, R.; Lahti, K.; Koivisto, M.; et al. Preterm Children’s Developmental Coordination Disorder, Cognition and Quality of Life: A Prospective Cohort Study. BMJ Paediatr. Open 2020, 4, e000633. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Husby, I.M.; Skranes, J.; Olsen, A.; Brubakk, A.-M.; Evensen, K.A.I. Motor Skills at 23 years of Age in Young Adults Born Preterm with Very Low Birth Weight. Early Hum. Dev. 2013, 89, 747–754. [Google Scholar] [CrossRef] [PubMed]
- Setanen, S.; Lehtonen, L.; Parkkola, R.; Aho, K.; Haataja, L. The Motor Profile of Preterm Infants at 11 years of Age. Pediatric Res. 2016, 80, 389–394. [Google Scholar] [CrossRef] [Green Version]
- Blank, R.; Smits-Engelsman, B.; Polatajko, H.; Wilson, P. European Academy for Childhood Disability (EACD): Recommendations on the Definition, Diagnosis and Intervention of Developmental Coordination Disorder (Long Version). Dev. Med. Child Neurol. 2012, 54, 54–93. [Google Scholar] [CrossRef]
- Ferrari, F.; Gallo, C.; Pugliese, M.; Guidotti, I.; Gavioli, S.; Coccolini, E.; Zagni, P.; della Casa, E.; Rossi, C.; Lugli, L.; et al. Preterm Birth and Developmental Problems in the Preschool Age. Part I: Minor Motor Problems. J. Matern. Fetal Neonatal Med. 2012, 25, 2154–2159. [Google Scholar] [CrossRef]
- Zwicker, J.G.; Yoon, S.W.; MacKay, M.; Petrie-Thomas, J.; Rogers, M.; Synnes, A.R. Perinatal and Neonatal Predictors of Developmental Coordination Disorder in Very Low Birthweight Children. Arch. Dis. Child. 2013, 98, 118–122. [Google Scholar] [CrossRef] [Green Version]
- Zwicker, J.G.; Harris, S.R.; Klassen, A.F. Quality of Life Domains Affected in Children with Developmental Coordination Disorder: A Systematic Review. Child Care Health Dev. 2013, 39, 562–580. [Google Scholar] [CrossRef]
- Ritchie, K.; Bora, S.; Woodward, L.J. Social Development of Children Born Very Preterm: A Systematic Review. Dev. Med. Child Neurol. 2015, 57, 899–918. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.M.; Champion, P.R.; Woodward, L.J. Social Competence of Preschool Children Born Very Preterm. Early Hum. Dev. 2013, 89, 795–802. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Montagna, A.; Nosarti, C. Socio-Emotional Development Following Very Preterm Birth: Pathways to Psychopathology. Front. Psychol. 2016, 7, 80. [Google Scholar] [CrossRef] [Green Version]
- Pinto-Martin, J.A.; Levy, S.E.; Feldman, J.F.; Lorenz, J.M.; Paneth, N.; Whitaker, A.H. Prevalence of Autism Spectrum Disorder in Adolescents Born Weighing <2000 Grams. Pediatrics 2011, 128, 883–891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ritchie, K.; Bora, S.; Woodward, L.J. Peer Relationship Outcomes of School-Age Children Born Very Preterm. J. Pediatrics 2018, 201, 238–244. [Google Scholar] [CrossRef]
- Linsell, L.; Johnson, S.; Wolke, D.; Morris, J.; Kurinczuk, J.J.; Marlow, N. Trajectories of Behavior, Attention, Social and Emotional Problems from Childhood to Early Adulthood Following Extremely Preterm Birth: A Prospective Cohort Study. Eur. Child Adolesc. Psychiatry 2019, 28, 531–542. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Romano, B. Feeling Lonesome: The Philosophy and Psychology of Loneliness. Philos. Psychol. 2016, 29, 1091–1094. [Google Scholar] [CrossRef]
- Junttila, N.; Vauras, M. Loneliness among School-Aged Children and Their Parents. Scand. J. Psychol. 2009, 50, 211–219. [Google Scholar] [CrossRef]
- Beutel, M.E.; Klein, E.M.; Brähler, E.; Reiner, I.; Jünger, C.; Michal, M.; Wiltink, J.; Wild, P.S.; Münzel, T.; Lackner, K.J.; et al. Loneliness in the General Population: Prevalence, Determinants and Relations to Mental Health. BMC Psychiatry 2017, 17, 97. [Google Scholar] [CrossRef] [Green Version]
- Vanhalst, J.; Luyckx, K.; Raes, F.; Goossens, L. Loneliness and Depressive Symptoms: The Mediating and Moderating Role of Uncontrollable Ruminative Thoughts. J. Psychol. 2012, 146, 259–276. [Google Scholar] [CrossRef]
- Lempinen, L.; Junttila, N.; Sourander, A. Loneliness and Friendships among Eight-Year-Old Children: Time-Trends over a 24-Year Period. J. Child Psychol. Psychiatry 2018, 59, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Indredavik, M.S.; Vik, T.; Heyerdahl, S.; Kulseng, S.; Fayers, P.; Brubakk, A.M. Psychiatric Symptoms and Disorders in Adolescents with Low Birth Weight. Arch. Dis. Child. Fetal Neonatal Ed. 2004, 89, 445–450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johnson, S.; Wolke, D. Behavioural Outcomes and Psychopathology during Adolescence. Early Hum. Dev. 2013, 89, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.; Hollis, C.; Kochhar, P.; Hennessy, E.; Wolke, D.; Marlow, N. Autism Spectrum Disorders in Extremely Preterm Children. J. Pediatrics 2010, 156, 525–531. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salomäki, S.; Rautava, P.; Junttila, N.; Huhtala, M.; Leppänen, M.H.; Nyman, A.; Koivisto, M.; Haataja, L.; Lehtonen, L.; Korja, R. Social Functioning Questionnaires of Adolescents Born Preterm Show Average Profiles and Attenuated Sex Differences. Acta Paediatr. 2021, 110, 1490–1497. [Google Scholar] [CrossRef]
- Henderson, S.E.; Sugdan, D.A.; Barnett, A. Movement Assessment Battery for Children (Examiner’s Manual); Pearson Assessment: London, UK, 2007. [Google Scholar]
- Hoza, B.; Bukowski, W.M.; Beery, S. Assessing Peer Network and Dyadic Loneliness. J. Clin. Child Psychol. 2000, 29, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Kaukiainen, A.; Junttila, N.; Kinnunen, R.; Vauras, M. MASK—Monitahoarviointi Sosiaalisesta Kompetenssista; Center of Learning Research, University of Turku: Turku, Finland, 2005. [Google Scholar]
- Junttila, N.; Voeten, M.; Kaukiainen, A.; Vauras, M. Multisource Assessment of Children’s Social Competence. Educ. Psychol. Meas. 2006, 66, 874–895. [Google Scholar] [CrossRef]
- Himmelmann, K.; Hagberg, G.; Beckung, E.; Hagberg, B.; Uvebrant, P. The Changing Panorama of Cerebral Palsy in Sweden. IX. Prevalence and Origin in the Birth-Year Period 1995–1998. Acta Paediatr. 2005, 94, 287–294. [Google Scholar] [CrossRef]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and Reliability of a System to Classify Gross Motor Function in Children with Cerebral Palsy. Dev. Med. Child Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef]
- Touwen, B.C.L. The Examination of the Child with Minor Neurological Dysfunction; Heinemann Medical Books: London, UK, 1979. [Google Scholar]
- Setänen, S.; Haataja, L.; Parkkola, R.; Lind, A.; Lehtonen, L. Predictive Value of Neonatal Brain MRI on the Neurodevelopmental Outcome of Preterm Infants by 5 Years of Age. Acta Paediatr. 2013, 102, 492–497. [Google Scholar] [CrossRef]
- Uusitalo, K.; Haataja, L.; Nyman, A.; Lehtonen, T.; Setänen, S.; PIPARI Study Group. Hammersmith Infant Neurological Examination and Long-Term Cognitive Outcome in Children Born Very Preterm. Dev. Med. Child Neurol. 2021, 63, 947–953. [Google Scholar] [CrossRef] [PubMed]
- Poulsen, A.A.; Ziviani, J.M.; Cuskelly, M.; Smith, R. Boys with Developmental Coordination Disorder: Loneliness and Team Sports Participation. Am. J. Occup. Ther. 2007, 61, 451–462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Omer, S.; Jijon, A.M.; Leonard, H.C. Research Review: Internalising Symptoms in Developmental Coordination Disorder: A Systematic Review and Meta-Analysis. J. Child Psychol. Psychiatry 2019, 60, 606–621. [Google Scholar] [CrossRef] [PubMed]
| Study Children, n = 165 | Drop-Outs, n = 56 | p-Value | |
|---|---|---|---|
| Gestational age, mean (SD) [minimum, maximum], week | 29.0 (2.7) [23 + 0, 35 + 6] | 29.0 (2.8) [23 + 5, 35 + 1] | 1.0 |
| Birth weight, mean (SD) [minimum, maximum], grams | 1128.7 (315.9) [400.0, 2120.0] | 1181.3 (369.5) [565.0, 1970.0] | 0.3 |
| Birth weight z-score, mean (SD) [minimum, maximum] | −1.4 (1.5) [−4.9, 3.4] | −1.3 (1.3) [−3.9, 2.0] | 0.6 |
| Small for gestational age (<−2 SD), n (%) | 54 (32.7) | 14 (25.0) | 0.3 |
| Male, n (%) | 92 (55.8) | 33 (58.9) | 0.7 |
| Cesarean delivery, n (%) | 97 (58.8) | 37 (66.1) | 0.3 |
| Multiple birth, n (%) | 58 (35.2) | 9 (16.1) | 0.007 |
| Bronchopulmonary dysplasia, n (%) | 20 (12.1) | 8 (14.3) | 0.7 |
| Operated necrotizing enterocolitis, n (%) | 6/162 (3.7) | 4/55 (7.3) | 0.3 |
| Sepsis, n (%) | 30 (18.2) | 7 (12.5) | 0.3 |
| Laser-treated retinopathy of prematurity, n (%) | 4/154 (2.6) | 4/53 (7.5) | 0.2 |
| Major brain pathologies in magnetic resonance imaging at term age * n (%) | 39/160 (24.4) | 17/55 (30.9) | 0.3 |
| Mother’s education > 12 years, n (%) | 67/155 (43.2) | 18/50 (36.0) | 0.4 |
| Father’s education > 12 years, n (%) | 39/154 (25.3) | 9/48 (18.8) | 0.4 |
| Children with CP, n = 6 | Children with DCD, n = 18 | |
|---|---|---|
Gross Motor Function Classification System
| 2 (33) 3 (50) 1 (17) | |
| Boys, n (%) | 4 (67) | 17 (94) |
| Full-scale intelligence quotient < 70, n (%) | 2 (33) | 7 (39) |
| Severe hearing impairment, n (%) | 0 (0) | 1 (6) |
| Outcome Variable | Movement ABC-2 Children with CP n = 6 | Movement ABC-2 Children with DCD, n = 18 | Movement ABC-2 Children Typical Motor Development, n = 141 |
|---|---|---|---|
| PNDLS | |||
| Social loneliness | r = −0.6, p = 0.2 | r = 0.3, p = 0.3 c | r = −0.1, p = 0.4 c |
| Emotional loneliness | r = 0.4, p = 0.5 a | r = −0.3, p = 0.2 a | r = 0.0, p = 0.6 e |
| MASCS | |||
| Co-operation skills | r = 0.2, p = 0.7 | r = −0.2, p = 0.4 b | r = 0.0, p = 0.7 d |
| Empathy | r = −0.3, p = 0.5 | r = −0.3, p = 0.3 | r = 0.1, p = 0.5 a |
| Impulsivity | r = 0.5, p = 0.3 | r = 0.06, p = 0.8 | r = 0.0, p = 0.6 b |
| Disruptiveness | r = 0.4, p = 0.4 | r = −0.2, p = 0.4 | r = −0.1, p = 0.4 c |
| Outcome Variable | Children with CP, n = 6 Mean (SD) | Children with DCD, n = 18 Mean (SD) | Children with Typical Motor Development, n = 141 Mean (SD) | p-Value |
|---|---|---|---|---|
| PNDL | ||||
| Social loneliness | 9.0 (1.5) | 8.9 (2.7) c | 7.8 (2.3) c | 0.1 |
| Emotional loneliness | 8.8 (1.9) a | 8.6 (3.0) a | 7.6 (2.4) e | 0.2 |
| MASCS | ||||
| Cooperation skills | 10.9 (1.6) | 10.3 (1.5) b | 10.1 (1.3) d | 0.3 |
| Empathy | 6.4 (0.8) | 5.8 (0.9) | 6.0 (0.8) a | 0.3 |
| Impulsivity | 2.9 (1.0) | 4.5 (1.0) | 4.1 (1.1)b | 0.008 * |
| Disruptiveness | 2.9 (0.4) | 3.9 (0.2) | 3.7 (0.1)c | 0.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Helin, M.; Karukivi, M.; Haataja, L.; Rautava, P.; Junttila, N.; Salomäki, S.; Lehtonen, L.; Setänen, S., on behalf of the PIPARI Study Group. Motor Performance in Association with Perceived Loneliness and Social Competence in 11-Year-Old Children Born Very Preterm. Children 2022, 9, 660. https://doi.org/10.3390/children9050660
Helin M, Karukivi M, Haataja L, Rautava P, Junttila N, Salomäki S, Lehtonen L, Setänen S on behalf of the PIPARI Study Group. Motor Performance in Association with Perceived Loneliness and Social Competence in 11-Year-Old Children Born Very Preterm. Children. 2022; 9(5):660. https://doi.org/10.3390/children9050660
Chicago/Turabian StyleHelin, Minttu, Max Karukivi, Leena Haataja, Päivi Rautava, Niina Junttila, Susanna Salomäki, Liisa Lehtonen, and Sirkku Setänen on behalf of the PIPARI Study Group. 2022. "Motor Performance in Association with Perceived Loneliness and Social Competence in 11-Year-Old Children Born Very Preterm" Children 9, no. 5: 660. https://doi.org/10.3390/children9050660






