Behavioral Changes in Preschool- and School-Age Korean Children: A Network Analysis
Abstract
:1. Introduction
- What are the core symptoms in the network of behavioral problem symptoms at 5 and 7 years of age?
- What are the core symptoms of the nonclinical and (sub)clinical groups in the behavioral problem symptom network at 5 and 7 years of age?
- How does the transition of core symptoms between the nonclinical and (sub)clinical groups change from 5 to 7 years of age?
2. Materials and Methods
2.1. Sample
2.2. Measures
CBCL
2.3. Data Analysis
2.3.1. Gaussian Graphical Network Analysis
2.3.2. Network Estimation and Visualization
2.3.3. The Network Comparison Test
2.3.4. Node Predictability
2.3.5. Transition Analysis
3. Results
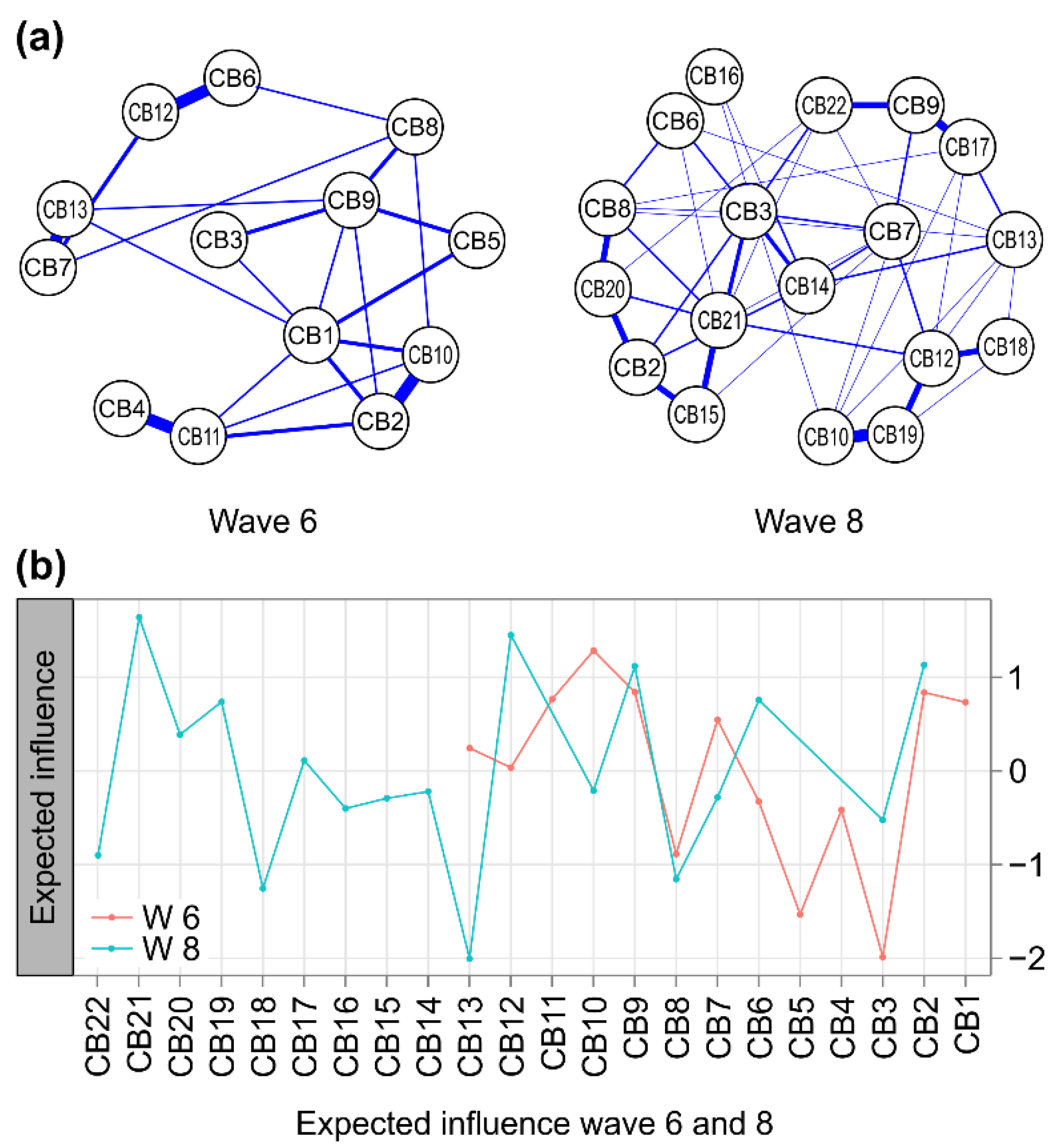
3.1. Network Inference by Age
3.1.1. Sample Characteristics
3.1.2. Network Stability
3.1.3. Replicability: Node Centrality in w6 vs. w8 Networks
3.2. Network Inference According to Clinical Risk
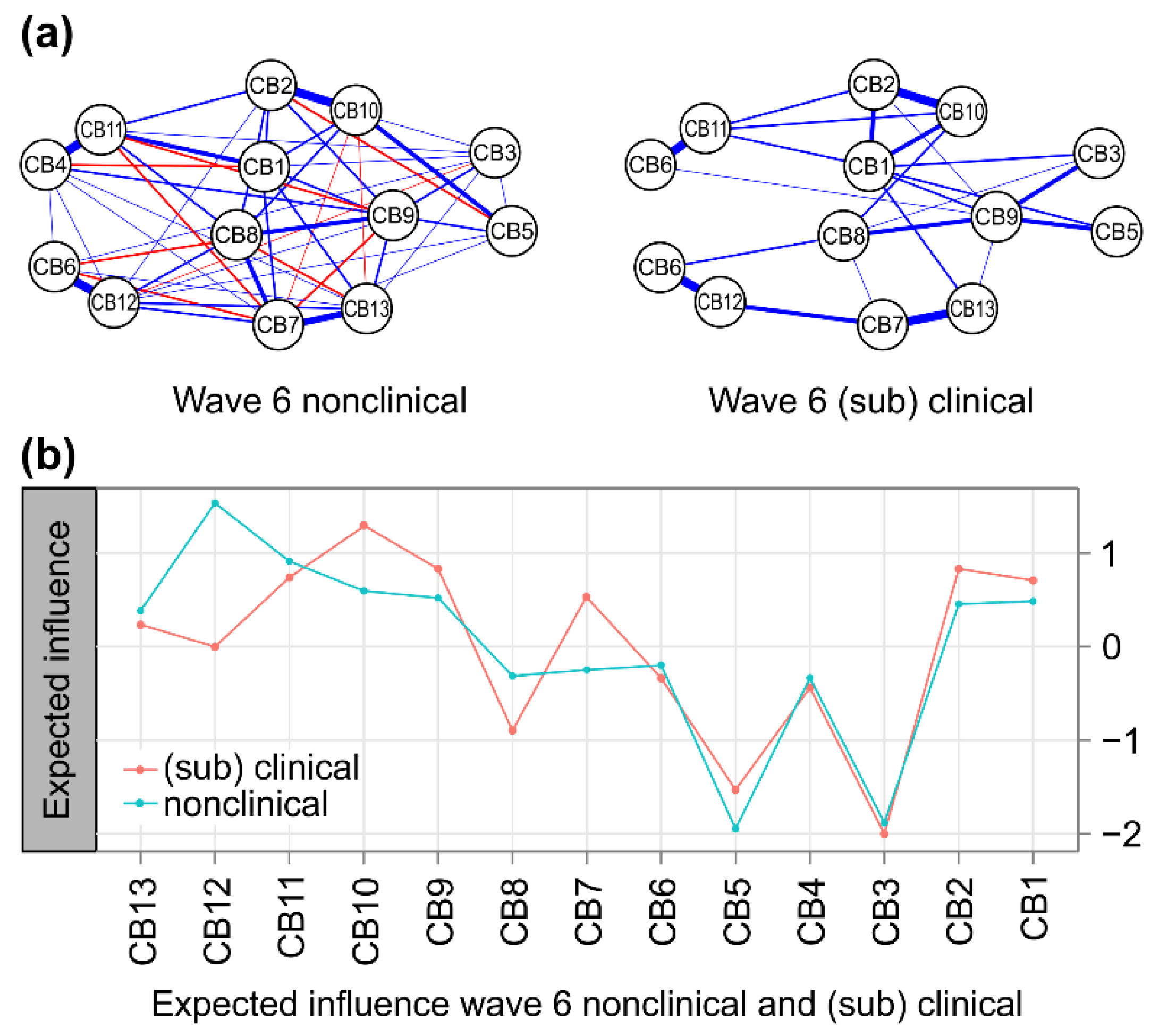
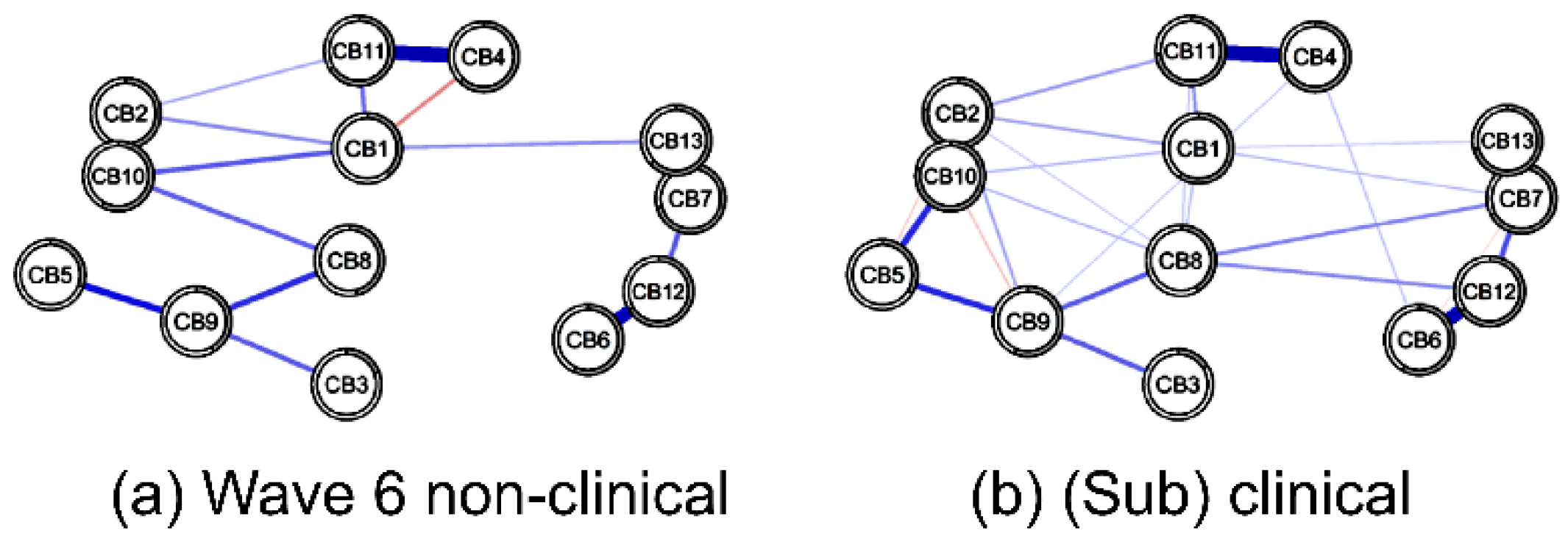
3.2.1. Node Centrality in Nonclinical vs. (Sub)Clinical Networks at w6
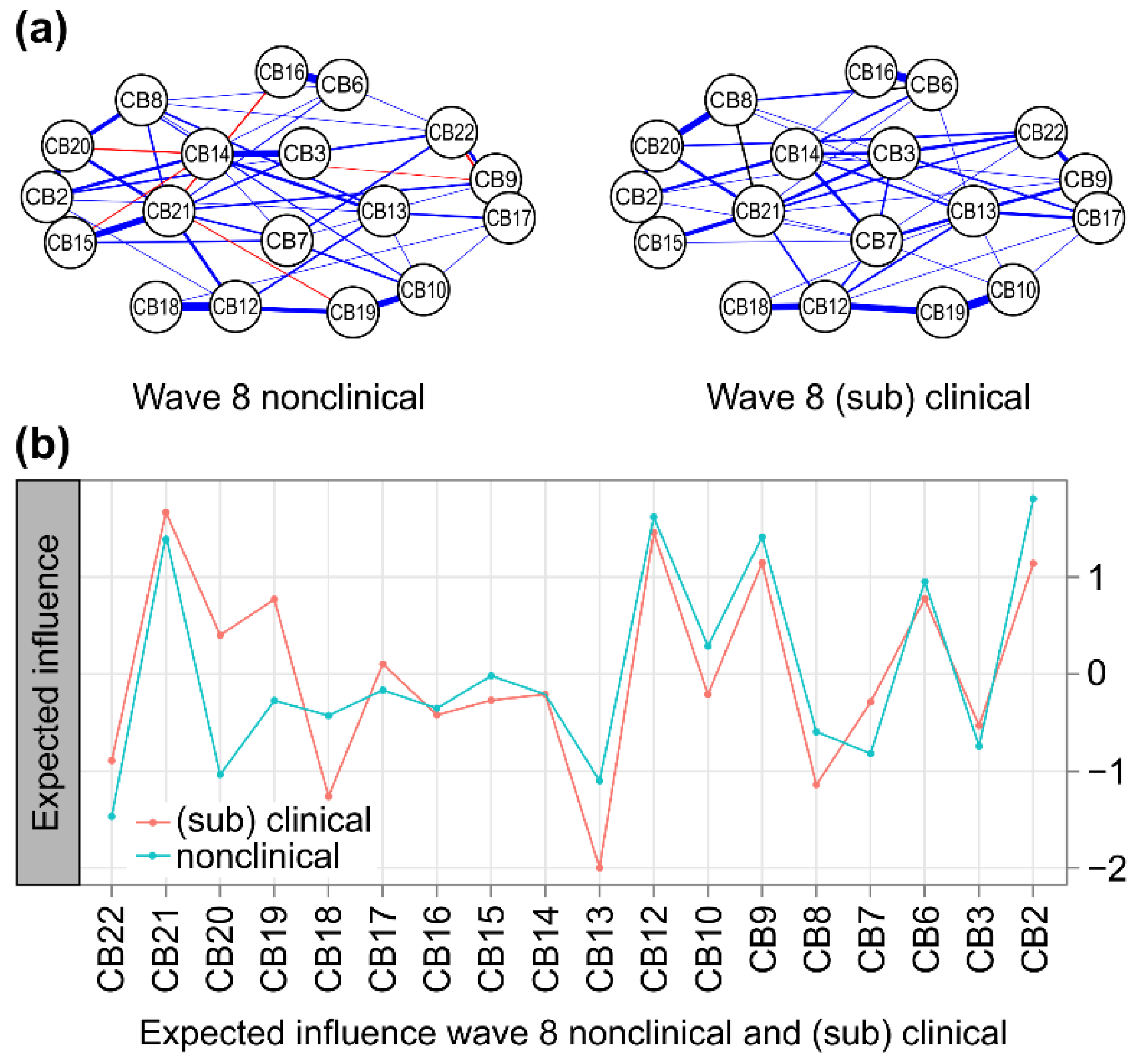
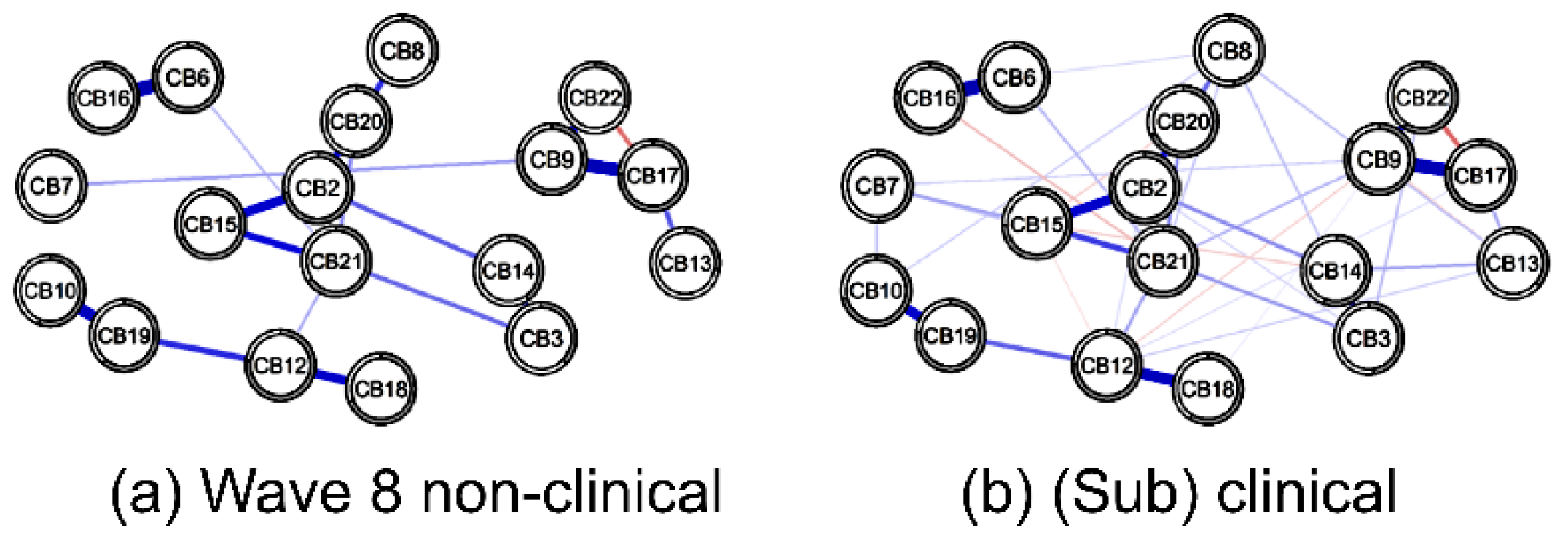
3.2.2. Node Centrality in Nonclinical vs. (Sub)Clinical Networks at Wave 8
3.2.3. Mean Difference of Sub-Factors of CBCL by Groups
3.2.4. Node Predictability
3.2.5. Network Comparison
Nonclinical vs. (Sub)Clinical at w6
Nonclinical vs. (Sub)Clinical at w8
3.3. Group Transition from w6 to w8
4. Discussion
4.1. Stability of the CBCL Behavioral Problem Network
4.2. Core Behavioral Problems in CBCL Networks
4.3. Highly Predictable Behavioral Issues
4.4. Transfer of Core Behavioral Problems
4.5. Limitations and Suggestions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jun, J. Children’s mental health status and its policy implication. Health Welf. Policy Forum 2020, 283, 32–42. [Google Scholar]
- Kim, D.; Lee, K. The influence of early childhood self-concepts and internalization/externalization problem behavior on elementary school adjustment. J. Yeolin Educ. 2021, 29, 239–263. [Google Scholar] [CrossRef]
- Kim, Y.A. Problem behaviors of early childhood and the lower grades of elementary school-the difference in ages and genders. Korea Compr. Infant Child Educ. Support. Soc. 2019, 7, 5–20. [Google Scholar]
- Oh, K.J.; Kim, Y.A. The Korean Version of the Child Behavior Checklist (CBCL) for Ages 1.5–5 Manual; Huno: Seoul, Korea, 2008. [Google Scholar]
- Oh, K.; Kim, Y. Manual for the ASEBA School-Age Forms; Huno: Seoul, Korea, 2010. [Google Scholar]
- Biederman, J.; Monuteaux, M.C.; Greene, R.W.; Braaten, E.; Doyle, A.E.; Faraone, S.V. Long-term stability of the Child Behavior Checklist in a clinical sample of youth with attention deficit hyperactivity disorder. J. Clin. Child Psychol. 2001, 30, 492–502. [Google Scholar] [CrossRef] [PubMed]
- Hofstra, M.B.; Verhulst, F.C. Continuity and change of psychopathology from childhood into adulthood: A 14-year follow-up study. J. Am. Acad. Child Adolesc. Psychiatry 2000, 39, 850–858. [Google Scholar] [CrossRef]
- Fischer, M.; Rolf, J.E.; Hasazi, J.E.; Cummings, L. Follow-up of a preschool epidemiological sample: Cross-age continuities and predictions of later adjustment with internalizing and externalizing dimensions of behavior. Child Dev. 1984, 55, 137–150. [Google Scholar] [CrossRef] [PubMed]
- Basten, M.; Tiemeier, H.; Althoff, R.R.; Van De Schoot, R.; Jaddoe, V.W.V.; Hofman, A.; Hudziak, J.J.; Verhulst, F.C.; Van Der Ende, J. The stability of problem behavior across the preschool years: An empirical approach in the general population. J. Abnorm. Child Psychol. 2016, 44, 393–404. [Google Scholar] [CrossRef] [Green Version]
- Scheper, F.Y.; Majdandžić, M.; van de Ven, P.M.; Jansen, L.M.; Doreleijers, T.A.; Schuengel, C.; de Vries, A.L. Temperament traits and psychopathology in young clinically referred children compared to a general population sample. Child Psychiatry Hum. Dev. 2017, 48, 841–850. [Google Scholar] [CrossRef] [Green Version]
- Borsboom, D. Measuring the Mind: Conceptual Issues in Contemporary Psychometrics; Cambridge University Press: Cambridge, UK, 2005. [Google Scholar] [CrossRef]
- Borsboom, D.; Cramer, A.O.; Schmittmann, V.D.; Epskamp, S.; Waldorp, L.J. The small world of psychopathology. PLoS ONE 2011, 6, e27407. [Google Scholar] [CrossRef] [Green Version]
- Boschloo, L.; van Borkulo, C.D.; Rhemtulla, M.; Keyes, K.M.; Borsboom, D.; Schoevers, R.A. The network structure of symptoms of the diagnostic and statistical manual of mental disorders. PLoS ONE 2015, 10, e0137621. [Google Scholar] [CrossRef] [Green Version]
- Boylan, K.R.; Miller, J.L.; Vaillancourt, T.; Szatmari, P. Confirmatory factor structure of anxiety and depression: Evidence of item variance across childhood. Int. J. Methods Psychiatr. Res. 2011, 20, 194–202. [Google Scholar] [CrossRef] [PubMed]
- Cummings, C.M.; Caporino, N.E.; Kendall, P.C. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychol. Bull. 2014, 140, 816. [Google Scholar] [CrossRef] [PubMed]
- Nuijten, M.B.; Deserno, M.K.; Cramer, A.O.J.; Borsboom, D. Mental disorders as complex networks. Clin. Neuropsychiatry 2016, 13, 68–76. [Google Scholar]
- Stringaris, A.; Maughan, B.; Copeland, W.S.; Costello, E.J.; Angold, A. Irritable mood as a symptom of depression in youth: Prevalence, developmental, and clinical correlates in the Great Smoky Mountains Study. J. Am. Acad. Child Adolesc. Psychiatry 2013, 52, 831–840. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rouquette, A.; Pingault, J.B.; Fried, E.I.; Orri, M.; Falissard, B.; Kossakowski, J.J.; Vitaro, F.; Tremblay, R.; Cote, S.M.; Borsboom, D. Emotional and behavioral symptom network structure in elementary school girls and association with anxiety disorders and depression in adolescence and early adulthood: A network analysis. JAMA Psychiatry 2018, 75, 1173–1181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bergman, L.R.; Magnusson, D. A person-oriented approach in research on developmental psychopathology. Dev. Psychopathol. 1997, 9, 291–319. [Google Scholar] [CrossRef]
- Bergman, L.R.; Trost, K. The person-oriented versus the variable-oriented approach: Are they complementary, opposites, or exploring different worlds? Merrill-Palmer Q. 2006, 52, 601–632. [Google Scholar] [CrossRef]
- Denham, S.A.; Workman, E.; Cole, P.M.; Weissbrod, C.; Kendziora, K.T.; ZAHN–WAXLER, C.A.R.O.L.Y.N. Prediction of externalizing behavior problems from early to middle childhood: The role of parental socialization and emotion expression. Dev. Psychopathol. 2000, 12, 23–45. [Google Scholar] [CrossRef]
- Panel Study of Korean Children. Available online: https://panel.kicce.re.kr/pskc/module/rawDataManage/index.do?menu_idx=56 (accessed on 8 May 2020).
- Korean Statistical Information Service. Available online: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1L9H002&conn_path=I3 (accessed on 10 January 2022).
- Epskamp, S.; Borsboom, D.; Fried, E.I. Estimating psychological networks and their accuracy: A tutorial paper. Behav. Res. Methods 2018, 50, 195–212. [Google Scholar] [CrossRef] [Green Version]
- Fruchterman, T.M.; Reingold, E.M. Graph drawing by force-directed placement. Softw. Pract. Exper. 1991, 21, 1129–1164. [Google Scholar] [CrossRef]
- Jones, P.J.; Mair, P.; McNally, R.J. Visualizing psychological networks: A tutorial in R. Front. Psychol. 2018, 9, 1742. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Borkulo, C.D.; van Bork, R.; Boschloo, L.; Kossakowski, J.J.; Tio, P.; Schoevers, R.A.; Borsboom, D.; Waldorp, L.J. Comparing network structures on three aspects: A permutation test. Psychol. Methods, 2022; Advance online publication. [Google Scholar] [CrossRef]
- Haslbeck, J.M.; Waldorp, L.J. How well do network models predict observations? On the importance of predictability in network models. Behav. Res. Methods 2018, 50, 853–861. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Phillips, R.D.; Wilson, S.M.; Sun, D.; VA Mid-Atlantic MIRECC Workgroup; Morey, R. Posttraumatic stress disorder symptom network analysis in U.S. military veterans: Examining the impact of combat exposure. Front. Psychiatry 2018, 9, 608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Beard, C.; Millner, A.J.; Forgeard, M.J.; Fried, E.I.; Hsu, K.J.; Treadway, M.T.; Leonard, C.V.; Björgvinsson, T. Network analysis of depression and anxiety symptom relationships in a psychiatric sample. Psychol. Med. 2016, 46, 3359–3369. [Google Scholar] [CrossRef] [Green Version]
- Kim, K.M.; Kim, H.; Kim, D.; Kim, J.W. The analysis of network structure among the depressive symptoms in a clinical sample of children and adolescents. Asian J. Psychiatr. 2021, 62, 102748. [Google Scholar] [CrossRef]
- Armour, C.; Fried, E.I.; Deserno, M.K.; Tsai, J.; Pietrzak, R.H. A network analysis of DSM-5 posttraumatic stress disorder symptoms and correlates in US military veterans. J. Anxiety Disord. 2017, 45, 49–59. [Google Scholar] [CrossRef]
- Hansen, M.; Armour, C.; McGlinchey, E.; Ross, J.; Ravn, S.L.; Andersen, T.E.; Lindekilde, N.; Elmose, M.; Karsberg, S.; Fried, E. Investigating centrality in PTSD symptoms across diagnostic systems using network analysis. Eur. J. Psychotraumatol. 2021, 12 (Suppl. S1), 1866412. [Google Scholar] [CrossRef]
- Hardy, A.; O’Driscoll, C.; Steel, C.; Van Der Gaag, M.; Van Den Berg, D. A network analysis of post-traumatic stress and psychosis symptoms. Psychol. Med. 2021, 51, 2485–2492. [Google Scholar] [CrossRef]
- Rescorla, L.A.; Genaro, B.; Ivanova, M.Y.; International ASEBA Consortium. International comparisons of emotionally reactive problems in preschoolers: CBCL/1½–5 Findings from 21 Societies. J. Clin. Child Adolesc. Psychol. 2020, 49, 773–786. [Google Scholar] [CrossRef]
- Ivanova, M.Y.; Achenbach, T.M.; Rescorla, L.A.; Harder, V.S.; Ang, R.P.; Bilenberg, N.; Bjarnadottir, G.; Capron, C.; De Pauw, S.S.; Dias, P.; et al. Preschool psychopathology reported by parents in 23 societies: Testing the seven-syndrome model of the child behavior checklist for ages 1.5–5. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 1215–1224. [Google Scholar] [CrossRef]
- Fried, E.I.; van Borkulo, C.D.; Cramer, A.O.; Boschloo, L.; Schoevers, R.A.; Borsboom, D. Mental disorders as networks of problems: A review of recent insights. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ebesutani, C.; Bernstein, A.; Nakamura, B.J.; Chorpita, B.F.; Higa-McMillan, C.K.; Weisz, J.R. Concurrent validity of the Child Behavior Checklist DSM-oriented scales: Correspondence with DSM diagnoses and comparison to syndrome scales. J. Psychopathol. Behav. Assess. 2010, 32, 373–384. [Google Scholar] [CrossRef] [Green Version]
- Cramer, A.O.; Waldorp, L.J.; Van Der Maas, H.L.; Borsboom, D. Comorbidity: A network perspective. Behav. Brain Sci. 2010, 33, 137–150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McElroy, E.; Fearon, P.; Belsky, J.; Fonagy, P.; Patalay, P. Networks of depression and anxiety symptoms across development. J. Am. Acad. Child Adolesc. Psychiatry 2018, 57, 964–973. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Costello, E.; Mustillo, S.; Erkanli, A.; Keeler, G.; Angold, A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch. Gen. Psychiatry 2003, 60, 837–844. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wichstrøm, L.; Belsky, J.; Steinsbekk, S. Homotypic and heterotypic continuity of symptoms of psychiatric disorders from age 4 to 10 years: A dynamic panel model. J. Child Psychol. Psychiatry 2017, 58, 1239–1247. [Google Scholar] [CrossRef]
- Baek, S.Y. Difference analysis on K-CBCL’s special checklist and DSM diagnostic scale for child behavioral problems in the elementary, middle and high school levels. J. Humanit. Soc. Sci. 2016, 21, 345–360. [Google Scholar]
- Walsh, K.; McLaughlin, K.A.; Hamilton, A.; Keyes, K.M. Trauma exposure, incident psychiatric disorders, and disorder transitions in a longitudinal population representative sample. J. Psychiatr. Res. 2017, 92, 212–218. [Google Scholar] [CrossRef]
- Benedek, E.P. Children and Psychic Trauma: A Brief Review of Contemporary Thinking, in Post-Traumatic Stress Disorder in Children; Eth, S., Pynoos, R.S., Eds.; American Psychiatric Publishing: Washington, DC, USA, 1985; pp. 1–16. [Google Scholar]
- Meiser-Stedman, R.; Smith, P.; Glucksman, E.; Yule, W.; Dalgleish, T. The posttraumatic stress disorder diagnosis in preschool-and elementary school-age children exposed to motor vehicle accidents. Am. J. Psychiatry 2008, 165, 1326–1337. [Google Scholar] [CrossRef] [Green Version]
- Scheeringa, M.S. Developmental considerations for diagnosing PTSD and acute stress disorder in preschool and school-age children. Am. J. Psychiatry 2008, 165, 1237–1239. [Google Scholar] [CrossRef]
- Zarrella, I.; Russolillo, L.A.; Caviglia, G.; Perrella, R. Continuity and discontinuity between psychopathology of childhood and adulthood: A review on retrospective and prospective studies. Res. Psychother. Psychopathol. Process Outcome 2017, 20, 248. [Google Scholar] [CrossRef] [PubMed]
- Groh, A.M.; Roisman, G.I.; van IJzendoorn, M.H.; Bakermans-Kranenburg, M.J.; Fearon, R. The significance of insecure and disorganized attachment for children’s internalizing symptoms: A meta-analytic study. Child Dev. 2012, 83, 591–610. [Google Scholar] [CrossRef] [PubMed]
- Madigan, S.; Atkinson, L.; Laurin, K.; Benoit, D. Attachment and internalizing behavior in early childhood: A meta-analysis. Dev. Psychol. 2013, 49, 672–689. [Google Scholar] [CrossRef] [Green Version]
- Fearon, R.; Bakermans-Kranenburg, M.J.; van IJzendoorn, M.H.; Lapsley, A.; Roisman, G.I. The significance of insecure attachment and disorganization in the development of children s externalizing behavior: A meta-analytic study. Child Dev. 2010, 81, 435–456. [Google Scholar] [CrossRef] [PubMed]
- Mun, S.Y.; Kang, J.H. The effect of children’s academic stress on problem behavior: The moderating effect of friendship quality. Korean J. Couns. 2013, 14, 3323–3339. [Google Scholar] [CrossRef]
- Hofstra, M.B.; Van Der Ende, J.A.N.; Verhulst, F.C. Child and adolescent problems predict DSM-IV disorders in adulthood: A 14-year follow-up of a Dutch epidemiological sample. J. Am. Acad. Child Adolesc. Psychiatry 2002, 41, 182–189. [Google Scholar] [CrossRef]
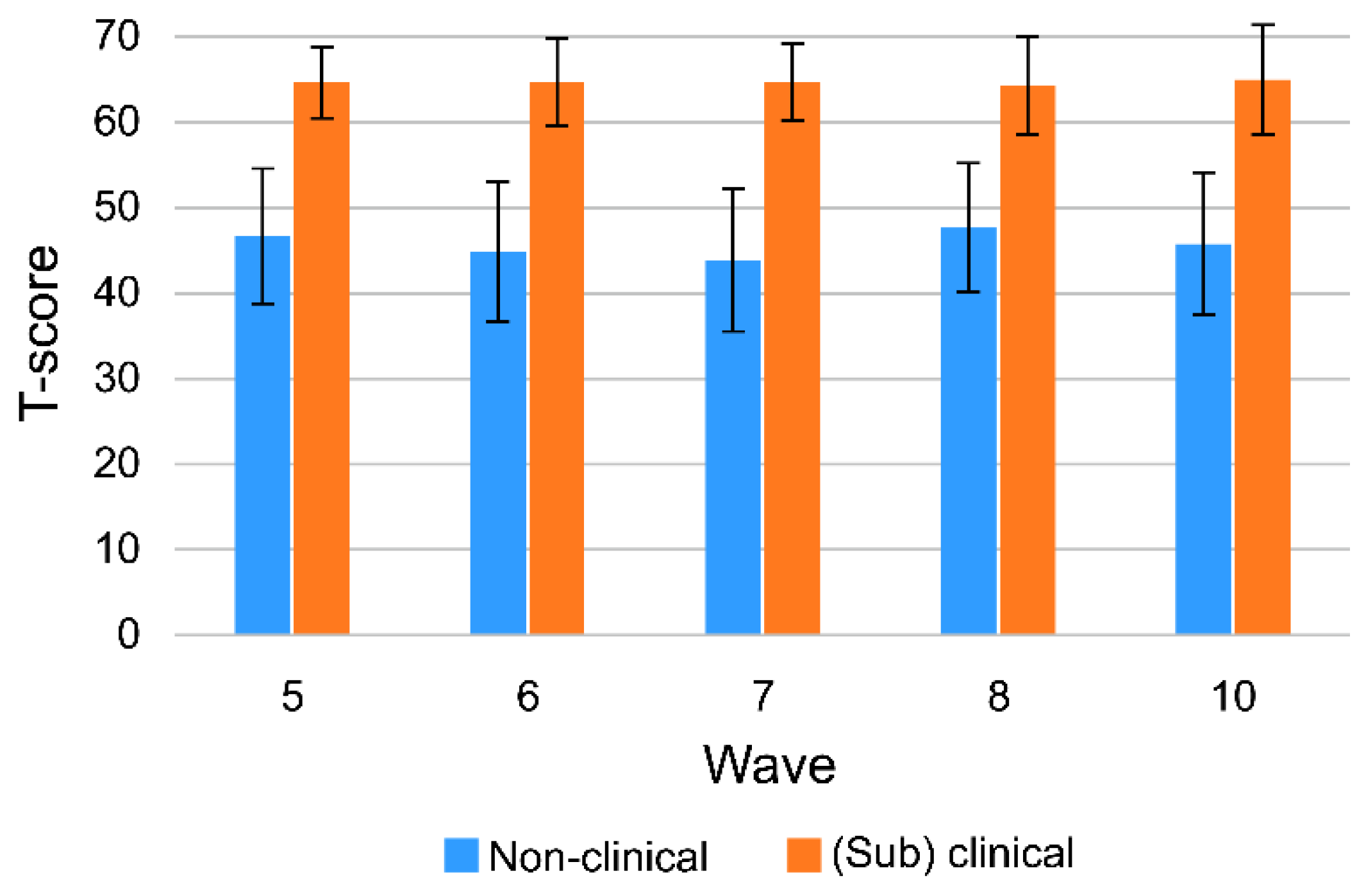

| M | SD | n | % | Missing (%) | |
|---|---|---|---|---|---|
| Monthly age | 50.99 | 1.21 | |||
| Boys | 671 | 50.7 | 0.0 | ||
| Father with a college degree or higher | 961 | 72.6 | 1.0 | ||
| Mother with a college degree or higher | 935 | 70.7 | 0.5 | ||
| Households with above-average income in 2012 [23] | 697 | 52.7 | 1.1 |
| Node Label | Norms | w6 | w8 | ||||
|---|---|---|---|---|---|---|---|
| Nonclinical | (Sub)Clinical | Nonclinical | (Sub)Clinical | ||||
| (n = 1177) | (n = 146) | (n = 1152) | (n = 171) | ||||
| M (SD) | t (g) | M (SD) | t (g) | ||||
| CB1 | Emotionally reactive | 51.64 (3.10) | 62.81 (7.49) | −17.82 *** (2.91) | |||
| CB2 | Anxious/depressed | 52.22 (3.72) | 62.86 (7.09) | −17.83 *** (2.52) | 52.41 (3.86) | 62.13 (6.78) | −18.32 *** (2.24) |
| CB3 | Somatic complaints | 52.56 (4.38) | 59.49 (7.40) | −11.08 *** (1.44) | 52.35 (3.81) | 60.05 (6.86) | −14.34 *** (1.78) |
| CB4 | Withdrawn | 52.21 (3.89) | 61.66 (6.51) | −17.17 *** (2.22) | |||
| CB5 | Sleep problems | 51.47 (3.50) | 58.47 (6.94) | −12.01 *** (1.74) | |||
| CB6 | Attention problems | 51.85 (3.68) | 59.32 (6.61) | −13.39 *** (1.82) | 52.32 (3.91) | 58.75 (7.73) | −10.68 *** (1.40) |
| CB7 | Aggressive behaviors | 51.43 (3.03) | 61.79 (5.48) | −22.43 *** (3.06) | 52.61 (3.79) | 62.75 (5.90) | −21.83 *** (2.46) |
| CB8 | Other Problems | 51.55 (3.05) | 63.23 (5.68) | −24.40 *** (3.40) | 52.76 (4.25) | 61.96 (6.90) | −16.97 *** (1.97) |
| CB9 | DSM affective problems | 51.50 (3.20) | 61.01 (6.71) | −16.89 *** (2.54) | 51.60 (3.07) | 60.06 (7.18) | −15.21 *** (2.20) |
| CB10 | DSM anxiety problems | 51.71 (3.33) | 61.53 (7.50) | −15.64 *** (2.45) | 53.85 (4.34) | 61.57 (6.42) | −15.21 *** (1.66) |
| CB11 | DSM pervasive developmental problems | 51.96 (3.79) | 62.62 (7.47) | −16.96 *** (2.45) | |||
| CB12 | DSM attention-deficit/hyper-activity problems | 52.20 (3.82) | 60.77 (6.77) | −15.00 *** (2.02) | 52.39 (3.72) | 63.19 (5.76) | −23.77 *** (2.43) |
| CB13 | DSM oppositional defiant problems | 51.63 (3.32) | 60.93 (6.39) | −17.30 *** (2.46) | 52.88 (4.46) | 62.25 (6.82) | −17.42 *** (1.94) |
| CB14 | Withdrawn/depressed | 51.75 (3.54) | 60.17 (6.99) | −15.46 *** (2.03) | |||
| CB15 | Rule-breaking behavior | 52.80 (4.40) | 62.47 (8.58) | −14.46 *** (1.88) | |||
| CB16 | Social problems | 52.26 (4.42) | 57.26 (8.15) | −7.85 *** (0.99) | |||
| CB17 | Thought problems | 51.79 (3.36) | 60.38 (7.55) | −14.66 *** (2.07) | |||
| CB18 | DSM somatic problems | 52.52 (4.01) | 61.14 (6.76) | −16.25 *** (1.93) | |||
| CB19 | DSM conduct problems | 51.98 (3.86) | 60.47 (7.32) | −14.89 *** (1.90) | |||
| CB20 | Obsessive–compulsive symptom | 52.75 (4.32) | 60.78 (7.36) | −13.94 *** (1.67) | |||
| CB21 | Posttraumatic stress problems | 51.98 (3.28) | 62.49 (6.15) | −21.89 *** (2.79) | |||
| CB22 | Sluggish cognitive tempo | 51.17 (3.33) | 58.32 (8.44) | −10.94 *** (1.65) | |||
| Mean Edge Weight | 0.088 | 0.176 | 0.089 | 0.134 | |||
| T-Score M (SD) | |||||
|---|---|---|---|---|---|
| Class | w6 | (sub)clinical | (sub)clinical | nonclinical | nonclinical |
| w8 | (sub)clinical | nonclinical | (sub)clinical | nonclinical | |
| n (%) | 73 (5.00) | 73 (5.00) | 98 (7.41) | 1079 (81.56) | |
| w6 | CB1 | 62.58 (7.47) | 63.04 (7.56) | 53.59 (4.25) | 51.46 (2.92) |
| CB2 | 62.85 (7.25) | 62.88 (6.98) | 53.99 (4.38) | 52.06 (3.62) | |
| CB7 | 62.21 (5.54) | 61.38 (5.44) | 53.50 (4.21) | 51.24 (2.82) | |
| CB9 | 61.59 (7.30) | 60.44 (6.06) | 52.79 (4.11) | 51.39 (3.08) | |
| CB10 | 60.95 (8.06) | 62.12 (6.90) | 53.08 (4.43) | 51.58 (3.18) | |
| CB11 | 62.37 (7.83) | 62.86 (7.14) | 53.89 (5.54) | 51.79 (3.55) | |
| w8 | CB2 | 63.45 (7.63) | 55.45 (4.84) | 61.14 (5.91) | 52.20 (3.70) |
| CB6 | 59.70 (8.72) | 52.42 (3.99) | 58.05 (6.87) | 52.31 (3.90) | |
| CB9 | 61.38 (8.84) | 52.79 (4.11) | 59.08 (5.48) | 51.52 (2.97) | |
| CB12 | 64.15 (6.15) | 54.99 (4.92) | 62.47 (5.38) | 52.21 (3.56) | |
| CB19 | 60.82 (8.17) | 54.23 (5.20) | 60.21 (6.64) | 51.82 (3.71) | |
| CB21 | 63.22 (7.26) | 54.01 (4.39) | 61.94 (5.13) | 51.85 (3.15) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goh, E.-K.; Jeon, H.J. Behavioral Changes in Preschool- and School-Age Korean Children: A Network Analysis. Children 2022, 9, 677. https://doi.org/10.3390/children9050677
Goh E-K, Jeon HJ. Behavioral Changes in Preschool- and School-Age Korean Children: A Network Analysis. Children. 2022; 9(5):677. https://doi.org/10.3390/children9050677
Chicago/Turabian StyleGoh, Eun-Kyoung, and Hyo Jeong Jeon. 2022. "Behavioral Changes in Preschool- and School-Age Korean Children: A Network Analysis" Children 9, no. 5: 677. https://doi.org/10.3390/children9050677
APA StyleGoh, E.-K., & Jeon, H. J. (2022). Behavioral Changes in Preschool- and School-Age Korean Children: A Network Analysis. Children, 9(5), 677. https://doi.org/10.3390/children9050677







