Windswept Deformity a Disease or a Symptom? A Systematic Review on the Aetiologies and Hypotheses of Simultaneous Genu Valgum and Varum in Children
Abstract
1. Introduction
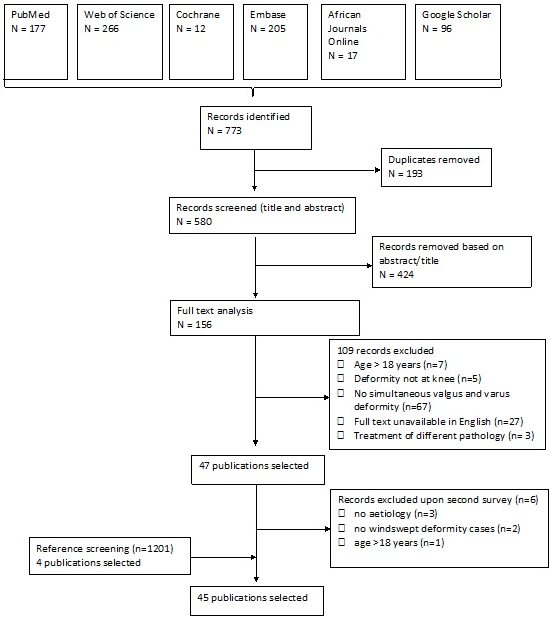
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Sources
2.3. Search Strategies
- 1.
- (windswept deformity) OR (windswept);
- 2.
- (((genu valgum) AND (genu varum)) OR ((genu valgum[MeSH Terms]) AND (genu varum[MeSH Terms]))) OR (combined valgus and varus knee) AND ((humans[Filter]) AND (allchild[Filter])) AND (English[Filter]);
- 3.
- (((((varo-valgum) OR (varovalgum)) OR (genu varo-valgum)) OR (genu varovalgum)) OR (varo-valga)) OR (varovalga).
2.4. Study Selection and Data Extraction
2.5. Level of Evidence and Quality Assessment
3. Results
- Rickets and other metabolic disorders;
- Skeletal dysplasias and other genetic disorders;
- Trauma;
- Descriptive articles without the specific underlying disorder.
| Article | Country of Study | Study Design | Aim of Study | Elaboration of WSD | WSD Aetiology | Level of Evidence (CEBM) and Methodological Quality |
|---|---|---|---|---|---|---|
| Akpede et al. [5] | Nigeria | Prospective cross-sectional | Determine the prevalence of clinical and biochemical rickets. | Two of ten patients who showed biochemical rickets, though not radiologically, did show WSD, suggesting a form of healed rickets. | Rickets, no radiographic evidence of active rickets | IV high |
| Al Kaissi et al. [18] | Austria | Case report | WSD in a patient with Schwartz-Jampel syndrome (SJS). | One patient with SJS, with WSD. | SJS | IV high |
| Al Kaissi et al. [19] | Austria | Case series | Record and discuss WSD in patients with X-linked hypophosphataemic rickets. | In seven patients with hypophosphataemic rickets, the most common angular deformity is WSD. | Hypophosphataemic rickets (from PHEX mutation) | IV moderate |
| Bar-On et al. [20] | Israel | Retrospective case series | Characterise deformities in patients with renal osteodystrophy (ROD). | One out of five patients showed WSD. | ROD | IV high |
| Bar-On et al. [14] | Israel | Retrospective case series | To investigate patients with insensitivity to pain. | One patient developed WSD as a consequence of growth disturbance due to untreated fractures of the growth plate. | Trauma | IV high |
| Bharani et al. [21] | India | Case report | To describe two siblings with sickle cell anaemia, presenting with bilateral lower limb deformities. | Two siblings, both male, 2 and 10 years old with progressive genu valgus on the right, genu varus on the left. | Distal renal tubular acidosis (dRTA) | IV High |
| Bhimma et al. [22] | Natal, South Africa | Case series | To determine the clinical spectrum of rickets among black children. | WSD was found in two patients with vitamin D deficiency and one patient with Ca deficiency in a total population of 37 patients. | Vitamin D and/or Ca deficiency rickets | IV high |
| Dudkiewicz et al. [23] | Israel | Case report | Describe the procedure of bone elongation in hypophosphataemic rickets. | One WSD with right genu valgum/left genu varum. | Hypophosphataemic rickets | IV moderate |
| Eralp et al. [24] | Turkey | Case report | Investigate the result of treatment with fixator-assisted intramedullary nailing in two cases with WSD. | Two patients with WSD, treated for vitamin-D-resistant rickets at younger age. | Vitamin-D-resistant rickets | IV high |
| Gigante et al. [25] | Italy | Case series | Evaluate temporary hemiepiphysiodesis in lower limb deformities in children with renal osteodystrophy (ROD). | One of the seven patients with ROD had WSD. Started as unilateral varus, developed valgus alignment in the contralateral knee. | ROD | IV high |
| Gupta et al. [26] | India | Literature review | Review the different types of nutritional vs. non-nutritional rickets. | Mention of WSD as a skeletal finding in nutritional rickets. It is not mentioned in non-nutritional rickets. | Nutritional rickets | n.a. * |
| Ikegawa [27] | Japan | Literature review | Review of the recent advances and current status of the genetic analysis of skeletal dysplasias. | Describes one WSD case, 17 years old with genu valgum on the left. | Skeletal dysplasia | n.a. * |
| Iyer and Diamond [28] | USA | Literature review | Review the effects of the resurgence of vitamin D deficiency and rickets. | Describes WSD as a possible clinical presentation of rickets. | Vitamin D deficiency rickets | n.a. * |
| Iyer and Diamond [29] | USA | Literature review | Review of the clinical, radiographic and biochemical manifestations of rickets. | Describes WSD as a possible clinical presentation of rickets. | Vitamin D deficiency rickets | n.a. * |
| Kenis et al. [30] | Austria | Case report | To describe the deformities in a patient with dysspondyloen-chondromatosis (DSC). | One patient with WSD with genu valgum of 30° on the right, genu varum of 10° on the left side. Age at start walking: 3 years. | DSC | IV high |
| Kim et al. [31] | Korea | Case series | Investigate the mutation frequency in individuals with multiple epiphyseal dysplasia (MED) and identify radiographic predictors. | Two of the fifty-five patients that identified with a previously reported mutation pathogenic for MED presented with WSD at the knee. One MATN3 and one COMP mutation. | MED | IV moderate |
| Lambert and Linglart [6] | France | Literature review | To describe the different causes and therapies of genetic and nutritional rickets. | WSD in walking children is a clinical manifestation of rickets. | Rickets | n.a. * |
| McKeand et al. [32] | USA | Case-control study | Describe the natural history of pseudoachondroplasia (PSACH). | WSD in 11/67 cases (16.4%), 8/11 cases (72.7%) needed a corrective operation for WSD. | PSACH | IIIb moderate |
| Muensterer et al. [33] | USA | Literature review | Describe pseudoachondroplasia, and its radiographic features. | In patients with pseudoachondroplasia, WSD typically develops around puberty, when genu varum transforms into WSD due to the progressive joint laxity. | PSACH | n.a.* |
| Nayak et al. [34] | India | Case report | Describe a case of epidermolytic hyperkeratosis (EHK) with rickets. | Epidermolytic hyperkeratosis (EHK) with rickets in a 6-year-old boy showed progressive WSD since age 3. | EHK | V high |
| Nishimura et al. [35] | Germany | Case series | Describe TRPV4 mutations in patients with spondylo-epiphyseal dysplasia (SED) and parastremmatic dysplasia. | A 7-year-old patient with reported low birth weight and length. Onset of walking at age 4. At 7 years she had a short stature (-4SD) and WSD. A TRPV4 mutation was found. | Parastremmatic dysplasia (TRPV4 mutation) | IV moderate |
| Nishimura et al. [36] | Switzerland | Literature review | To describe the different skeletal dysplasia’s related to TRPV4 mutations. | Patients with parastremmatic dysplasia have restricted joints and severe misalignment of the lower limbs (severe genu valgum, genu varum or WSD). | Parastremmatic dysplasia (TRPV4 mutation) | n.a. * |
| Oginni et al. [37] | Nigeria | Prospective case series | Response of oral calcium in Nigerian children with rickets. | Nine out of twenty-six children with underlying Ca-deficiency rickets presented with WSD, they were treated with calcium supplements, with good results. | Calcium-deficiency rickets | IV high |
| Oni and Keswani [38] | Nigeria | Case series | To describe the radiological findings of idiopathic or primary WSD. | Eight WSD patients were found, the onset of clinical and radiological alterations is abrupt, where the disease arises from a formerly normal epiphysis. The radiological features are similar to Blount, and therefore the etiological considerations that apply to Blount may also apply to primary WSD. | Hypotheses: similar to Blount, mechanical pressure, illness | IV moderate |
| Oni et al. [11] | Nigeria | Case series | To describe windswept deformity. | Eight patients with osteochondrosis with abrupt onset in previously healthy children, with formerly normal epiphyses. | Hypothesis: similar to Blount | IV moderate |
| Oyemade [13] | Nigeria | Case series | To describe the correction of primary knee deformities in children with and without rickets. | Rachitic patients WSD 12/47, Non-rachitic patients: WSD 15/67. | Rachitic or idiopathic (Blount) | IV moderate |
| Oyemade [1] | Nigeria | Case series | To clarify aetiological factors in primary deformities of the knee in children. | WSD: peak age male and female 2 years. Rachitic: WSD (12/47). Non-rachitic WSD (15/67). | Rachitic and non-rachitic Blount-like (weight-bearing) | IV moderate |
| Paruk et al. [39] | South Africa | Case report | Describe two cases of primary hyperparathyroidism (PHPT) in adolescence, mimicking rickets. | A 13-year-old male with progressive pain and WSD (right varus, left valgus). Caused by a parathyroid adenoma. | PHPT | IV high |
| Pavone et al. [40] | Italy | Literature review | Review hypophosphataemic rickets. | WSD described as a clinical feature of X-linked hypophosphataemic rickets. | X-linked hypophosphataemic rickets | n.a. * |
| Pettifor et al. [10] | South Africa | Literature review | Presentation of vitamin D deficiency and nutritional rickets in children. | In older children with vitamin D deficiency rickets, WSD may be present. | Vitamin D deficiency rickets and Calcium deficiency rickets | n.a. * |
| Pettifor et al. [41] | South Africa | Case series | Clinical, radiographic and biochemical findings in four children with severe bone deformities resembling rickets. | One out of four children had WSD. | Calcium-deficiency rickets | IV moderate |
| Prakash et al. [42] | India | Prospective cohort | To evaluate the behaviour of lower limb deformities due to rickets. | Five out of one-hundred and seventeen nutritional rickets patients had WSD. Varus deformity being the youngest, valgus and WSD being older. | Nutritional rickets | Iib high |
| Prentice et al. [43] | Gambia | Case-control study | Biochemical profile in Gambian children with rickets of unknown aetiology and normal 25OHD. | One out of thirty-seven patients had WSD. | Calcium-deficiency rickets | IIIb high |
| Shehzad and Shaheen [44] | Pakistan | Case report | Describe a case of epidermolytic hyperkeratosis (EHK) with rickets. | A 13-year old female with WSD, started around the age of 5. Scaling of the skin since birth. | Epidermolytic hyperkeratosis (EHK) with rickets | IV high |
| Simsek-Kiper et al. [45] | Turkey | Case series | Report on five patients from 2 unrelated families with SEMDFA (spondyloepimetaphyseal dysplasia Faden-Alkuraya type). | One patient presents with WSD (right genu varum, left genu valgum). | SEMDFA | IV High |
| Smyth [4] | Nigeria | Case report | Describe three cases of windswept deformity. | Three cases of WSD. Two cases with normal development, when suddenly WSD develops. In one case, there is a period of an acute febrile illness (possibly measles) preceding the development of WSD. | Period of epiphyseal instability + stress factor, geographical genetic dysplasia | IV moderate |
| Solagberu [12] | Nigeria | Prospective case series | Determine the varieties of angular deformities of the knee in children, in/around Ilorin, Nigeria. | Ten patients with WSD presented in one year. Age distribution between 2 and 5 years. | One bone diseased, while the other appears to be compensating | IV moderate |
| Teotia et al. [46] | India | Literature review | Report effects of endemic fluoride exposure on metabolic bone disease. | WSD as presentation of bony leg deformity due to high levels of fluoride exposure in drinking water. | Endemic chronic fluoride toxicity | n.a. * |
| Thacher et al. [47] | Nigeria/South Africa | Case report | Three cases of vitamin D-deficiency rickets associated with ichthyosis. | WSD in two patients with ichthyosis and rickets. | Ichthyosis with rickets | IV high |
| Thacher et al. [7] | Nigeria | Literature review | Describe the features of calcium-deficiency rickets. | Bowleg deformity is less specific for active rickets than knock-knee or WSD. | Calcium-deficiency rickets | n.a. * |
| Thacher et al. [9] | Nigeria | Case-control study | Determine whether low dietary calcium intake is associated with rickets in Nigerian children. | Of 123 Nigerian children with rickets: 16 (13%) had WSD. | Calcium-deficiency rickets | IIIb high |
| Thacher et al. [8] | Nigeria | Cohort study | Development of a clinical prediction model for active rickets. | The median age of onset of WSD was 24 months. WSD present in 39 of the 278 cases of active rickets (14%). Children presenting leg deformities over a span of 4 years, 95/736 had WSD (12.9%). | Rickets | IIb moderate |
| Vatanavicharn et al. [48] | USA | Case report | Radiographic patellar finding in a patient with pseudoachondroplasia (COMP mutation). | At age 5, the patient developed WSD (right genu varum, left valgum). | Pseudoachondroplasia (following COMP mutation) | IV high |
| Weiner et al. [49] | USA | Case series | Characterise the typical orthopaedic findings in pseudoachondroplasia. | Angular deformity of knees: genu valgum n = 35 (22%), genu varum n = 89 (56%), WSD n = 35 (22%). Laxity in all patients. | Pseudoachondroplasia (following COMP mutation) | IV moderate |
| Yilmaz et al. [50] | Croatia | Cohort study | Temporary hemi epiphysiodesis for correction of angular deformities in children with skeletal dysplasia. | One patient with metaphyseal dysplasia had WSD and underwent correction for both varus and valgus deformity. | Metaphyseal dysplasia | Iib moderate |
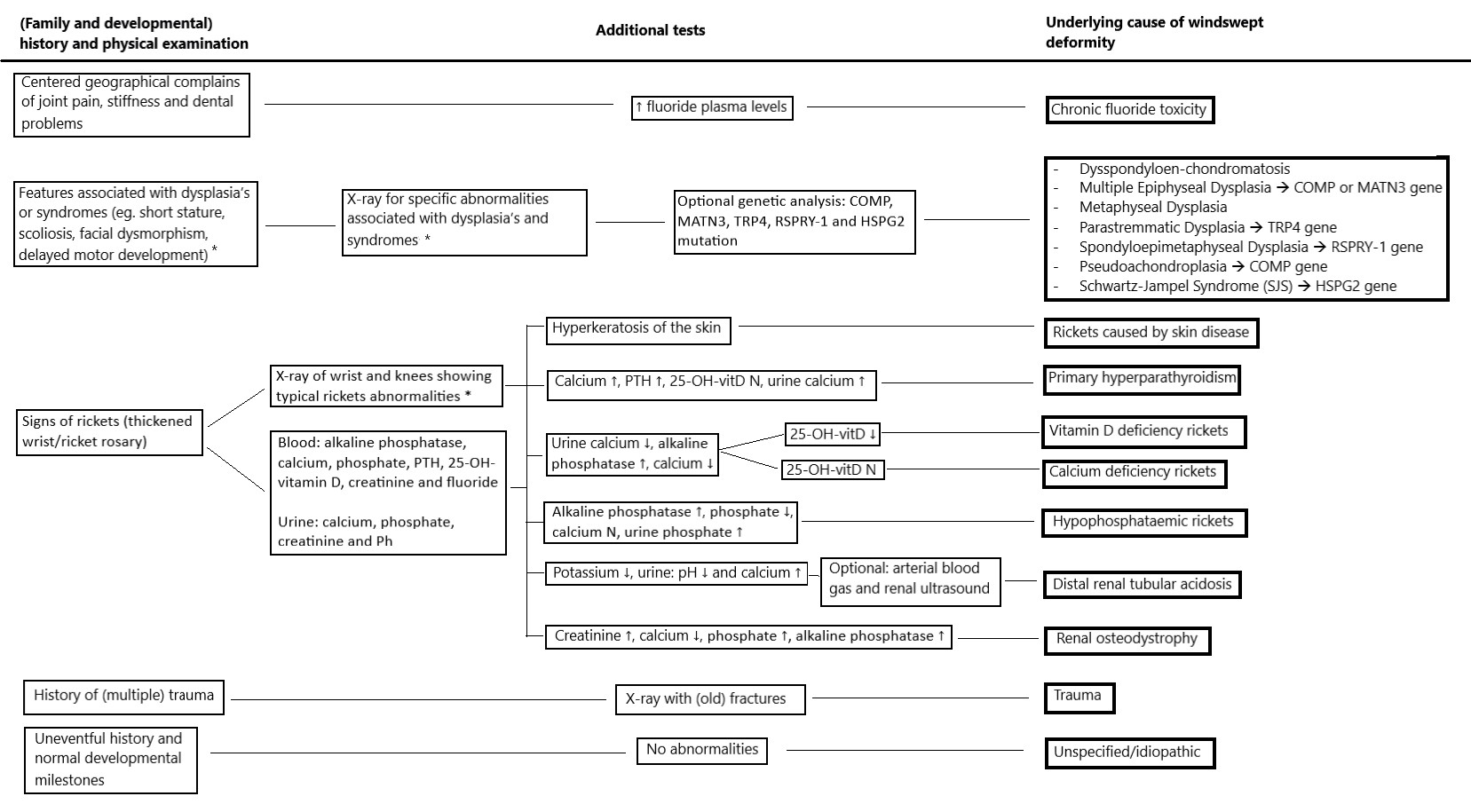
3.1. Rickets and Other Metabolic Disorders
3.2. Skeletal Dysplasia and Other Genetic Disorders
3.3. Trauma
3.4. Descriptive Articles without Specific Underlying Disorder
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Database | Search 1 | Search 2 | Search 3 |
|---|---|---|---|
| Pubmed | (windswept deformity) OR (windswept) | (((genu valgum) AND (genu varum)) OR ((genu valgum[MeSH Terms]) AND (genu varum[MeSH Terms]))) OR (combined valgus and varus knee) AND ((humans[Filter]) AND (allchild[Filter])) AND (english[Filter]) | (((((varo-valgum) OR (varovalgum)) OR (genu varo-valgum)) OR (genu varovalgum)) OR (varo-valga)) OR (varovalga) |
| AJOL | (windswept deformity) OR (windswept) | ((genu valgum) AND (genu varum)) OR (combined valgus and varus knee) | (((((varo-valgum) OR (varo valgum)) OR (genu varo-valgum)) OR (genu varo valgum)) OR (varo-valgo)) OR (varovalga) |
| Cochrane | windswept deformity in Title Abstract Keyword OR windswept in Title Abstract Keyword | ((“genu valgum”):ti,ab,kw OR (“genu valgus”):ti,ab,kw) “AND” ((“genu varum”):ti,ab,kw OR (“genu varus”):ti,ab,kw) | (genu varovalgum) OR (genu varo-valgum) OR (varo-valgum) OR (varovalgum) OR (varovalga) OR (varo-valga) |
| Embase | windswept deformity.mp. OR windswept.mp. | valgus knee/AND varus knee/limit to (human and English language) | varo-valgum.mp. OR genu varo-valgum.mp. |
| G-scholar | knee or genu, “windswept deformity” or windswept, -cerebral, -palsy, -osteoarthritis | combined valgus and varus OR “simultaneous valgus and varus” OR “combined varus and valgus” OR “simultaneous varus and valgus” OR “simultaneous varus and valgus” | genu varovalgum |
| WoS | (windswept deformity OR windswept) | (TS = (genu valgum “and” genu varum) OR (TS = (combined valgus and varus knee “OR” simultaneous valgus and varus))) AND LANGUAGE: (English) | genu varovalgum OR genu varo-valgum OR varovalgum OR varo-valgum OR varo-valga |
Appendix B
| Author | Study Design | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Score | Maximum Score | Percentage | Low/Moderate/High |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Akpede et al. [5] | cross-sectional | Y | Y | Y | Y | N | N | Y | Y | 12 | 16 | 75 | high | |||
| Al Kaissi et al. [18] | case report | Y | Y | Y | Y | Y | Y | Y | N | 14 | 16 | 87.5 | high | |||
| Al Kaissi et al. [19] | case series | N | Y | Y | UC | UC | Y | N | UC | Y | NA | 11 | 18 | 61.1 | moderate | |
| Bar-On et al. [20] | case series | Y | UC | UC | Y | UC | Y | Y | Y | Y | NA | 15 | 18 | 83.3 | high | |
| Bar-On et al. [14] | case series | Y | Y | Y | UC | UC | Y | Y | Y | Y | NA | 16 | 18 | 88.9 | high | |
| Bharani et al. [21] | case report | Y | Y | Y | Y | N | NA | N | N | 12 | 14 | 85.7 | high | |||
| Bhimma et al. [22] | case series | Y | Y | Y | UC | UC | Y | N | Y | Y | NA | 14 | 18 | 77.8 | high | |
| Dudkiewicz et al. [23] | case report | N | Y | N | N | N | Y | Y | Y | 8 | 16 | 50 | moderate | |||
| Eralp et al. [24] | case report | Y | N | Y | Y | Y | Y | N | Y | 12 | 16 | 75 | high | |||
| Gigante et al. [25] | case series | Y | Y | UC | Y | UC | N | Y | Y | Y | NA | 14 | 18 | 77,8 | high | |
| Kenis et al. [30] | case report | N | Y | Y | Y | Y | Y | N | Y | 12 | 16 | 75 | high | |||
| Kim et al. [31] | case series | Y | Y | Y | N | UC | Y | Y | NA | N | Y | 13 | 18 | 72.2 | moderate | |
| McKeand et al. [32] | case-control study | Y | UC | Y | Y | Y | N | N | Y | 11 | 16 | 68.75 | moderate | |||
| Nayak et al. [34] | case report | N | Y | Y | Y | Y | Y | N | Y | 12 | 16 | 75 | high | |||
| Nishimura et al. [35] | case series | Y | Y | Y | N | NA | N | N | Y | Y | NA | 10 | 16 | 62.5 | moderate | |
| Oginni et al. [37] | prospective case series | Y | Y | Y | Y | Y | N | N | Y | Y | Y | 16 | 20 | 80 | high | |
| Oni and Keswani [38] | case series | Y | UC | UC | UC | UC | N | Y | NA | Y | NA | 10 | 16 | 62.5 | moderate | |
| Oni et al. [11] | case series | Y | UC | UC | Y | UC | N | Y | NA | N | NA | 9 | 16 | 56.3 | moderate | |
| Oyemade [13] | case series | N | Y | Y | Y | UC | N | Y | Y | Y | NA | 13 | 18 | 72.2 | moderate | |
| Oyemade [1] | case series | Y | Y | Y | Y | UC | N | Y | N | Y | NA | 13 | 18 | 72.2 | moderate | |
| Paruk [39] | case report | Y | Y | Y | Y | Y | Y | Y | Y | 16 | 16 | 100 | high | |||
| Pettifor et al. [41] | case series | N | Y | Y | UC | UC | Y | Y | Y | N | NA | 12 | 18 | 66.7 | moderate | |
| Prakash [42] | prospective cohort | NA | NA | Y | NA | N | Y | Y | Y | Y | Y | Y | 14 | 16 | 87.5 | high |
| Prentice et al. [43] | case-control study | UC | UC | Y | Y | Y | N | Y | Y | 12 | 16 | 75 | high | |||
| Shehzad and Shaheen [44] | case report | Y | Y | Y | Y | Y | Y | N | N | 12 | 16 | 75 | high | |||
| Simsek-Kiper et al. [45] | case series | N | Y | Y | UC | UC | Y | Y | NA | Y | NA | 12 | 16 | 75 | high | |
| Smyth [4] | case report | Y | N | Y | Y | N | N | N | Y | 8 | 16 | 50 | moderate | |||
| Solagberu [12] | prospective case series | Y | UC | Y | Y | UC | N | Y | N | Y | Y | 14 | 20 | 70 | moderate | |
| Thacher et al. [47] | case report | Y | Y | Y | Y | Y | Y | N | Y | 14 | 16 | 87.5 | high | |||
| Thacher et al. [9] | case-control study | Y | Y | Y | Y | Y | N | N | Y | 12 | 16 | 75 | high | |||
| Thacher et al. [8] | cohort study | Y | Y | Y | N | N | N | Y | NA | NA | NA | Y | 10 | 16 | 62.5 | moderate |
| Vatanavicharn et al. [48] | case report | Y | Y | Y | Y | NA | NA | NA | Y | 10 | 10 | 100 | high | |||
| Weiner et al. [49] | case series | N | Y | UC | UC | UC | Y | Y | NA | Y | NA | 11 | 16 | 68.8 | moderate | |
| Yilmaz et al. [50] | cohort study | Y | Y | Y | N | N | Y | Y | Y | Y | UC | Y | 15 | 22 | 68.2 | moderate |
References
- Oyemade, G. Aetiological Factors in Genu Valga, Vara and Varovalga in Nigerian Children. J. Trop. Pediatr. 1975, 21, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Fulford, F.E.; Brown, J.K. Position as a cause of deformity in children with cerebral palsy. Dev. Med. Child Neurol. 1976, 18, 305–314. [Google Scholar] [CrossRef] [PubMed]
- Sharma, L.; Song, J.; Felson, D.T.; Cahue, S.; Shamiyeh, E.; Dunlop, D.D. The Role of Knee Alignment in Disease Progression and Functional Decline in Knee Osteoarthritis. JAMA 2001, 286, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Smyth, E.H. Windswept deformity. J. Bone Jt. Surg. Br. 1980, 62, 166–167. [Google Scholar] [CrossRef] [PubMed]
- Akpede, G.O.; Solomon, E.A.; Jalo, I.; Addy, E.O.; Banwo, A.I.; Omotara, B.A. Nutritional rickets in young Nigerian children in the Sahel savanna. East Afr. Med. J. 2001, 78, 568–575. [Google Scholar] [CrossRef]
- Lambert, A.; Linglart, A. Hypocalcaemic and hypophosphatemic rickets. Best Pract. Res. Clin. Endocrinol. Metab. 2018, 32, 455–476. [Google Scholar] [CrossRef]
- Thacher, T.D. Calcium-deficiency rickets. Endocr. Dev. 2003, 6, 105–125. [Google Scholar]
- Thacher, T.D.; Fischer, P.R.; Pettifor, J. The usefulness of clinical features to identify active rickets. Ann. Trop. Paediatr. 2002, 22, 229–237. [Google Scholar] [CrossRef]
- Thacher, T.D.; Fischer, P.R.; Pettifor, J.M.; Lawson, J.O.; Isichei, C.O.; Chan, G.M. Case-control study of factors associated with nutritional rickets in Nigerian children. J. Pediatr. 2000, 137, 367–373. [Google Scholar] [CrossRef]
- Pettifor, J.M.; Thandrayen, K.; Thacher, T.D. Vitamin D Deficiency and Nutritional Rickets in Children. In Vitamin D; Academic Press: Cambridge, MA, USA, 2018; pp. 179–201. [Google Scholar]
- Oni, O.O.; Keswani, H.; Aganga, M.O. Windswept deformity. Arch. Dis. Child 1983, 58, 541–543. [Google Scholar] [CrossRef][Green Version]
- Solagberu, B.A. Angular Deformities of the Knee in Children. Niger. J. Surg. Res. 2000, 2, 62–67. [Google Scholar] [CrossRef]
- Oyemade, G.A. The correction of primary knee deformities in children. Int. Orthop. 1981, 5, 241–245. [Google Scholar] [CrossRef] [PubMed]
- Bar-On, E.; Weigl, D.; Parvari, R.; Katz, K.; Weitz, R.; Steinberg, T. Congenital insensitivity to pain. Orthopaedic manifestations. J. Bone Jt. Surg. Br. 2002, 84, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Persson-Bunke, M.; Hägglund, G.; Lauge-Pedersen, H. Windswept hip deformity in children with cerebral palsy. J. Pediatr. Orthop. B 2006, 15, 335–338. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Qureshi, R.; Mattis, P.; Lisy, K.; et al. Chapter 7: Systematic reviews of etiology and risk in: Aromataris E. In Joanna Briggs Institute Reviewer’s Manual; Munn, Z., Ed.; The Joanna Briggs Institute: Adelaide, Australia, 2017; Available online: https://reviewersmanual.joannabriggs.org/ (accessed on 14 January 2022).
- Al Kaissi, A.; Ganger, R.; Klaushofer, K.; Grill, F. Windswept deformity in a patient with Schwartz-Jampel syndrome. Swiss Med. Wkly. 2012, 142, w13519. [Google Scholar]
- Al Kaissi, A.; Farr, S.; Ganger, R.; Klaushofer, K.; Grill, F. Windswept lower limb deformities in patients with hypophosphataemic rickets. Swiss Med. Wkly. 2013, 143, w13904. [Google Scholar]
- Bar-On, E.; Horesh, Z.; Katz, K.; Weigl, D.M.; Becker, T.; Cleper, R.; Krause, I.; Davidovits, M. Correction of Lower Limb Deformities in Children With Renal Osteodystrophy by the Ilizarov Method. J. Pediatr. Orthop. 2008, 28, 747–751. [Google Scholar] [CrossRef]
- Bharani, A.; Manchanda, R.; Singh, R.K.; Prashant, S. Distal renal tubular acidosis in sickle cell anemia. Saudi J. Kidney Dis. Transplant. 2018, 29, 1000–1004. [Google Scholar] [CrossRef]
- Bhimma, R.; Pettifor, J.; Coovadia, H.M.; Moodley, M.; Adhikari, M. Rickets in black children beyond infancy in Natal. S. Afr. Med. J. 1995, 85, 668–672. [Google Scholar]
- Dudkiewicz, I.; Schindler, A.; Ganel, A. Elongation of long bones for short stature in patients with hypophosphatemic rickets. Isr. Med. Assoc. J. 2003, 5, 66–67. [Google Scholar] [PubMed]
- Eralp, L.; Kocaoglu, M.; Çakmak, M.; Ozden, V.E. A correction of windswept deformity by fixator assisted nailing. J. Bone Jt. Surgery. Br. Vol. 2004, 86, 1065–1068. [Google Scholar] [CrossRef]
- Gigante, C.; Borgo, A.; Corradin, M. Correction of lower limb deformities in children with renal osteodystrophy by guided growth technique. J. Child. Orthop. 2017, 11, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Sinha, R.; Banerjee, S. Nutritional Verses Non Nutritional Rickets; The Institute of Child Health Calcutta: Kolkata, India, 2013; Volume 13, pp. 19–26. [Google Scholar]
- Ikegawa, S. Genetic analysis of skeletal dysplasia: Recent advances and perspectives in the post-genome-sequence era. J. Hum. Genet. 2006, 51, 581–586. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Iyer, P.; Diamond, F.B., Jr. Shedding Light on Hypovitaminosis D and Rickets. Adv. Pediatr. 2007, 54, 115–133. [Google Scholar] [CrossRef] [PubMed]
- Iyer, P.; Diamond, F. Detecting Disorders of Vitamin D Deficiency in Children: An Update. Adv. Pediatr. 2013, 60, 89–106. [Google Scholar] [CrossRef] [PubMed]
- Kenis, V.; Baindurashvili, A.; Melchenko, E.; Ganger, R.; Grill, F.; Al Kaissi, A. Spinal and extraspinal deformities in a patient with dysspondyloenchondromatosis. Ger. Med. Sci. 2013, 11, Doc06. [Google Scholar]
- Kim, O.H.; Park, H.; Seong, M.W.; Cho, T.J.; Nishimura, G.; Superti-Furga, A.; Unger, S.; Ikegawa, S.; Choi, I.H.; Song, H.R.; et al. Revisit of multiple epiphyseal dysplasia: Ethnic difference in genotypes and comparison of radiographic features linked to the COMP and MATN3 genes. Am. J. Med. Genet. A 2011, 155, 2669–2680. [Google Scholar] [CrossRef]
- McKeand, J.; Rotta, J.; Hecht, J.T. Natural history study of pseudoachondroplasia. Am. J. Med. Genet. 1996, 63, 406–410. [Google Scholar] [CrossRef]
- Muensterer, O.J.; Berdon, W.E.; Lachman, R.S.; Done, S.L. Pseudoachondroplasia and the seven Ovitz siblings who survived Auschwitz. Pediatr. Radiol. 2012, 42, 475–480. [Google Scholar] [CrossRef]
- Nayak, S.; Behera, S.K.; Acharjya, B.; Sahu, A.; Mishra, D. Epidermolytic hyperkeratosis with rickets. Indian J. Dermatol. Venereol. Leprol. 2006, 72, 139–142. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, G.; Dai, J.; Lausch, E.; Unger, S.; Megarbané, A.; Kitoh, H.; Kim, O.H.; Cho, T.-J.; Bedeschi, F.; Benedicenti, F.; et al. Spondylo-epiphyseal dysplasia, Maroteaux type (pseudo-Morquio syndrome type 2), and parastremmatic dysplasia are caused by TRPV4 mutations. Am. J. Med Genet. Part A 2010, 152, 1443–1449. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, G.; Lausch, E.; Savarirayan, R.; Shiba, M.; Spranger, J.; Zabel, B.; Ikegawa, S.; Superti-Furga, A.; Unger, S. TRPV4-associated skeletal dysplasias. Am. J. Med. Genet. Part C Semin. Med. Genet. 2012, 160, 190–204. [Google Scholar] [CrossRef] [PubMed]
- Oginni, L.M.; Sharp, C.A.; Badru, O.S.; Risteli, J.; Davie, M.W.J.; Worsfold, M.; Fischer, P.R. Radiological and biochemical resolution of nutritional rickets with calcium. Arch. Dis. Child. 2003, 88, 812–817. [Google Scholar] [CrossRef][Green Version]
- Oni, O.O.; Keswani, H. Idiopathic or primary windswept deformity: The etiological significance of the radiological findings. J. Pediatr. Orthop. 1984, 4, 293–296. [Google Scholar] [CrossRef]
- Paruk, I.M.; Pirie, F.J.; Motala, A.A. Rickets mimicker: A report of two cases of primary hyperparathyroidism in adolescence. J. Endocrinol. Metab. Diabetes S. Afr. 2018, 24, 1–5. [Google Scholar] [CrossRef][Green Version]
- Pavone, V.; Testa, G.; Iachino, S.G.; Evola, F.R.; Avondo, S.; Sessa, G. Hypophosphatemic rickets: Etiology, clinical features and treatment. Eur. J. Orthop. Surg. Traumatol. 2014, 25, 221–226. [Google Scholar] [CrossRef]
- Pettifor, J.; Ross, F.; Travers, R.; Glorieux, F.; Deluca, H. Dietary calcium deficiency: A syndrome associated with bone deformities and elevated serum 1,25-Dihyroxyvitamin D concentrations. Metab. Bone Dis. Relat. Res. 1981, 2, 301–305. [Google Scholar] [CrossRef]
- Prakash, J.; Mehtani, A.; Sud, A.; Reddy, B.K. Is surgery always indicated in rachitic coronal knee deformities? Our experience in 198 knees. J. Orthop. Surg. 2017, 25, 2309499017693532. [Google Scholar] [CrossRef]
- Prentice, A.; Ceesay, M.; Nigdikar, S.; Allen, S.; Pettifor, J. FGF23 is elevated in Gambian children with rickets. Bone 2008, 42, 788–797. [Google Scholar] [CrossRef]
- Shehzad, A.; Shaheen, S. Epidermolytic hyperkeratosis (bullous ichthyosiform erythroderma) with rickets: A case report. J. Pak. Assoc. Dermatol. 2008, 18, 182–186. [Google Scholar]
- Simsek-Kiper, P.O.; Taskiran, E.Z.; Kosukcu, C.; Urel-Demir, G.; Akgun-Dogan, O.; Yilmaz, G.; Alikasifoglu, M. Further delineation of spondyloepimetaphyseal dysplasia Faden-Alkuraya type: A RSPRY1-associated spondylo-epi-metaphyseal dysplasia with cono-brachydactyly and craniosynostosis. Am. J. Med. Genet. A 2018, 176, 2009–2016. [Google Scholar] [CrossRef] [PubMed]
- Teotia, M.; Teotia, S.P.; Singh, K.P. Endemic chronic fluoride toxicity and dietary calcium deficiency interaction syndromes of metabolic bone disease and deformities in India: Year 2000. Indian J. Pediatr. 1998, 65, 371–381. [Google Scholar] [CrossRef] [PubMed]
- Thacher, T.D.; Fischer, P.R.; Pettifor, J.M.; Darmstadt, G.L. Nutritional Rickets in Ichthyosis and Response to Calcipotriene. Pediatrics 2004, 114, e119–e123. [Google Scholar] [CrossRef] [PubMed]
- Vatanavicharn, N.; Lachman, R.S.; Rimoin, D.L. Multilayered patella: Similar radiographic findings in pseudoachondroplasia and recessive multiple epiphyseal dysplasia. Am. J. Med. Genet. A 2008, 146, 1682–1686. [Google Scholar] [CrossRef]
- Weiner, D.S.; Guirguis, J.; Makowski, M.; Testa, S.; Shauver, L.; Morgan, D. Orthopaedic manifestations of pseudoachondroplasia. J. Child. Orthop. 2019, 13, 409–416. [Google Scholar] [CrossRef]
- Yilmaz, G.; Oto, M.; Thabet, A.M.; Rogers, K.J.; Anticevic, D.; Thacker, M.M.; Mackenzie, W.G. Correction of lower extremity angular deformities in skeletal dysplasia with hemiepiphysiodesis: A preliminary report. J. Pediatr. Orthop. 2014, 34, 336–345. [Google Scholar] [CrossRef]
- Pettifor, J.M.; Ross, P.; Moodley, G.; Shuenyane, E. Calcium deficiency in rural black children in South Africa—A comparison between rural and urban communities. Am. J. Clin. Nutr. 1979, 32, 2477–2483. [Google Scholar] [CrossRef]
- Jagtap, V.S.; Sarathi, V.; Lila, A.R.; Bandgar, T.; Menon, P.; Shah, N.S. Hypophosphatemic rickets. Indian J. Endocrinol. Metab. 2012, 16, 177–182. [Google Scholar] [CrossRef]
- Rice, A.S.; Crane, J.S. Epidermolytic Hyperkeratosis. In StatPearls; StatPearls Publishing LLC.: Treasure Island, FL, USA, 2020. [Google Scholar]
- Milstone, L.M.; Ellison, A.F.; Insogna, K.L. Serum Parathyroid Hormone Level Is Elevated in Some Patients With Disorders of Keratinization. Arch. Dermatol. 1992, 128, 926–930. [Google Scholar] [CrossRef]
| Author | Country of Study | WSD Cases | Male | Female | Suggested Aetiology or Hypothesis | Ethnicity | Onset Age (Months) | Onset Valgus | Onset Varus | Valgus Right | Valgus Left |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Akpede et al. [5] | Nigeria | 2 | - | - | Biochemical rickets | African | - | - | - | - | - |
| Al Kaissi et al. [49] | Austria | 1 | 1 | 0 | Schwarz-Jampel Syndrome (SJS) | - | - | - | - | - | 1 |
| Al Kaissi et al. [19] | Austria | 7 | 7 | 0 | X-linked hypophosphataemic rickets | - | 14–18 | - | - | - | - |
| Bar-On et al. [20] | Israel | 1 | 1 | 0 | Renal osteodystrophy (ROD) | - | - | 1 | - | 1 | - |
| Bar-On et al. [14] | Israel | 1 | 0 | 1 | Congenital insensitivity to pain (trauma) | Middle-East | - | - | - | 1 | - |
| Bharani et al. [21] | India | 2 | 2 | 0 | Distal renal tubular acidosis (dRTA) | Asian | 36 | - | - | 2 | - |
| Bhimma et al. [22] | South Africa | 3 | - | - | Vitamin D and/or Ca deficiency rickets | African | - | - | - | - | - |
| Dudkiewicz et al. [23] | Israel | 1 | 1 | 0 | Hypophosphataemic rickets | - | - | - | - | 1 | - |
| Eralp et al. [24] | Turkey | 2 | 1 | 1 | Vitamin D-resistant rickets | - | - | - | - | 2 | - |
| Gigante et al. [25] | Italy | 1 | 1 | 0 | Renal osteodystrophy (ROD) | - | - | - | 1 | 1 | - |
| Ikegawa [27] | Japan | 1 | 1 | 0 | Pseudoachondroplasia | Asian | - | - | - | - | 1 |
| Kenis et al. [30] | Austria | 1 | 1 | 0 | Dysspondyloenchondromatosis (DSC) | Caucasian | - | - | - | 1 | - |
| Kim et al. [31] | Korea | 2 | 2 | 0 | Multiple epiphyseal dysplasia (MED) | Asian | - | - | - | - | - |
| McKeand et al. [32] | USA | 11 | - | - | Pseudoachondroplasia | Caucasian | - | - | - | - | - |
| Nayak et al. [34] | India | 1 | 1 | 0 | Rickets (epidermolytic hyperkeratosis) | - | 36 | - | - | - | - |
| Nishimura et al. [35] | Germany | 1 | 0 | 1 | Parastremmatic dysplasia (with TRPV4 mutation) | African | - | - | - | - | 1 |
| Oginni et al. [37] | Nigeria | 9 | - | - | Ca deficiency rickets | African | - | - | - | - | - |
| Oni and Keswani [38] | Nigeria | 8 | 3 | 5 | Similar to Blount mechanical pressure + illness | African | 6–24 | 1 | 1 | 2 | - |
| Oyemade [1] | Nigeria | 28 | 18 | 10 | Rickets (12) or non-rachitic (15) (3 hypotheses: weight-bearing, dietetic, genetic) | African | 12–108 | - | - | - | - |
| Paruk et al. [39] | South Africa | 1 | 1 | 0 | Primary hyperparathyroidism | African | 150 | - | - | - | 1 |
| Pettifor et al. [41] | South Africa | 1 | 0 | 1 | Ca deficiency rickets | African | - | - | - | 1 | - |
| Prakash et al. [42] | India | 5 | - | - | Nutritional rickets | Asian | 48–120 | - | - | - | - |
| Prentice et al. [43] | Gambia | 1 | - | - | Ca deficiency rickets | African | - | - | - | - | - |
| Shehzad and Shaheen [44] | Pakistan | 1 | 0 | 1 | Rickets (epidermolytic hyperkeratosis) | Asian | 60 | - | - | - | - |
| Simsek-Kiper et al. [45] | Turkey | 1 | 1 | 0 | Spondyloepimetaphyseal dysplasia Faden-Alkuraya type (SEMDFA) | Caucasian | 36–48 | - | - | - | 1 |
| Smyth [4] | Nigeria | 3 | 2 | 1 | Period of epiphyseal instability + stress factor, geographical genetics | African | 24–54 | 3 | - | 1 | 1 |
| Solagberu [12] | Nigeria | 10 | - | - | Compensation for 1 diseased bone | African | 24–60 | - | - | - | - |
| Thacher et al. [47] | Nigeria/South Africa | 2 | 1 | 1 | Ichthyosis with rickets | African | - | - | - | - | - |
| Thacher et al. [8] | Nigeria | 39 | - | - | Rickets | African | - | - | - | - | - |
| Vatanavicharn et al. [48] | USA | 1 | 0 | 1 | Pseudoachondroplasia | Caucasian | 60 | - | - | - | 1 |
| Weiner et al. [49] | USA | 35 | - | - | Pseudoachondroplasia | Caucasian | - | - | - | 1 | - |
| Yilmaz et al. [50] | Croatia | 1 | 0 | 1 | Metaphyseal dysplasia | Caucasian | - | - | - | - | 1 |
| Total | 184 | 45 | 24 | African n = 108 Asian n = 11 Caucasian n = 50 Middle-east n = 1 Missing ethnicity n = 14 | 5 | 2 | 14 | 8 |
| Aetiology Group | Specific Aetiology | Family History | History | Physical Exam | Laboratory Findings | X-Ray | Articles |
|---|---|---|---|---|---|---|---|
| Rickets | Vitamin D deficiency rickets* | Generally uneventful | Decreased exposure to sunlight | Thickened wrists and ankles, rickety rosarymuscle weakness | Alkaline phosphatase ↑ Phosphate ↓/N/↑ Calcium ↓ 25-OH-vitD ↓ 1.25-di-OH-vit D ↓/N/↑ PTH ↑ Urine: Ca ↓ | Widening of the growth plate and abnormal configuration of the metaphysis:
Anterior rib ends: rachitic rosary | Bhimma et al. [22], Thacher [7], Iyer et al. [28,29], Gupta et al. [26], Prakash et al. [42] |
| Calcium deficiency rickets* | Generally uneventful | Low-calcium diet | Thickened wrists and ankles, rickety rosary | Alkaline phosphatase ↑ Phosphate ↓ Calcium ↓ 25-OH-vitD N 1.25-di-OH-vit D ↑ PTH ↑ Urine: Ca ↓ | See above | Bhimma et al. [22], Oginni et al. [37], Prentice et al. [43], Pettifor et al. [41], Gupta et al. [26] | |
| Hypophosphataemic rickets | X-linked (PHEX mutation) or autosomal dominant (FGF23 mutation) transmission | Delayed walking, muscular weakness, bone pain, failure to thrive, tooth abscesses | Thickened wrists and ankles, rickety rosary, dental abnormalities | Alkaline phosphatase ↑ Phosphate ↓ Calcium N 25-OH-vitD N 1.25-di-OH-vitD N/↓ PTH N/↑ FGF23 ↑Urine: phosphate ↑ Genetic testing: PHEX mutation | See above | Bhimma et al. [22], Al-Kaissi et al. [19], Dudkiewicz et al. [23], Pavone et al. [40], Eralp et al. [24], Gupta et al. [26], Prakash et al. [42] | |
| Skin disease (Epidermolytic hyperkeratosis or Ichthyosis) | Consanguinity and familial inheritance may occur | Bright red blisters after birth. Development of hyperkeratotic plaques | Generalised dry skin, hyperkeratotic and cobble-stone plaques. Rib beading, widening of wrists and ankles | Alkaline phosphatase ↑ Phosphate ↓ Calcium ↓ 25-OH-vitD ↓ PTH ↑ Skin biopsy: hyperkeratosis | See above | Shehzad and Shaheen [44], Nayak et al. [34], Thacher [47] | |
| Other metabolic | Primary hyperparathyroidism | Generally uneventful | Progressive pain, normal developmental milestones | No abnormalities | Alkaline phosphatase ↑ Phosphate ↓ Calcium ↑ PTH ↑ 25-OH-vitD N 1.25-di-OH-vitD ↑ Urine: Ca ↑ | See above and a sestamibi scan: increased focal uptake of the parathyroid glands | Paruk et al. [39] |
| Chronic fluoride toxicity | Affected family members, centred geographic distribution of fluoride levels | Mild: generalised bone and joint painmoderate: stiffness and rigiditySevere: flexion deformities at hips and knees | Stiff and rigid spine and joints, flexion deformity hips, knees and elbows, hypo-mineralisation of tooth enamel | Alkaline phosphatase ↑ Phosphate N Calcium N 25-OHD N1-25(OH)2D ↑ PTH ↑ Plasma fluoride ↑ | Osteosclerosis, periosteal bone formation, calcifications of interosseus membrane, rickets-like metaphyses | Teotia et al. [46] | |
| Distal renal tubular acidosis | Familial inheritance | Sickle cell disease, failure to thrive, polyuria, polydipsia | Low weight/height, frontal bossing, wrist widening (signs of rickets) | ABG: Metabolic acidosis Potassium ↓ Chloride ↑ Urine: pH↓, calcium ↑ Renal ultrasound: nephrocalcinosis | Osteopenia, angular deformities and signs of rickets | Bharani et al. [21] | |
| Renal Osteodystrophy | Familial inheritance may occur | Bone pain, muscle weakness | Significant growth retardation | Alkaline phosphatase ↑ Phosphate ↑ Calcium ↓ Creatinine ↑ PTH ↑ | Widening and elongation of the growth plates and cupping of the metaphysis and signs of rickets | Bar-On et al. [20], Gigante et al. [25] | |
| Dysplasia’s and syndromes | Dysspondyloen-chondromatosis | Generally uneventful | Delays in motor development | Neonatal dwarfism, unequal limb length, flat midface with frontal prominence and progressive kyphoscoliosis | No abnormalities | Aniosospondyly and enchondroma-like lesions in the metaphyseal and diaphyseal portions of the long tubular bones | Kenis et al. [30] |
| Multiple Epiphyseal Dysplasia | Familial inheritance may occur | Joint pain, scoliosis, deformities hands, feet, knees and hips | Muscular hypotonia, ligamentous hyperlaxity, abnormal gait, angular deformities at hips and knees | Genetic testing: COMP or MATN3 mutations | COMP: small and round femoral head, MATN3: crescent-shaped femoral head | Kim et al. [31] | |
| Metaphyseal Dysplasia | Consanguinity and familial inheritance may occur | Mental, physical and height development are usually normal | Angular deformities of the knees, palpable widening of the distal femur and clavicles | no abnormalities | Erlenmeyer flask deformity | Yilmaz et al. [50] | |
| Parastremmatic Dysplasia | Generally uneventful | Normal mental milestones, motor development may be slightly delayed, short stature | Windswept and flexural deformity of the legs, scoliosis, platyspondyly | Genetic testing: TRP4 mutation | Flaky metaphyses with wide zones of radiolucencies and flocky calcifications, disorganised epiphyseal ossifications, severe platyspondyly | Nishimura et al. [35,36] | |
| Spondyloepimetaphyseal Dysplasia Faden-Alkuraya type | Parental consanguinity, autosomal recessive inheritance | Difficulty walking, short stature, delayed motor and mental development | Short stature, hypertelorism, brachycephaly, short nose with depressed nasal bridge, tented upper lip, proptosis | Genetic testing: RSPRY-1 mutation | Mild spondylar dysplasia, epi-metaphyseal dysplasia of long bones (flat and irregular epi- and metaphyseal flaring) | Siimsek-kiper et al. [45] | |
| Pseudoachondroplasia | Autosomal dominant inheritance | Normal birthweight and length, At around 2-4yr of age short stature and disproportionately short limbs appear | Short stature, disproportionately short limbs, short and stubby fingers, increased joint laxity, waddling gait | Genetic testing: COMP mutation | Irregular or fragmented epiphyses, flaring, widening or trumpeting of the metaphyses, anterior beaking of vertebrae | Muensterer et al. [33], Vatanavicharn et al. [27], Weiner et al. [49], McKeand et al. [32] | |
| Schwartz-Jampel Syndrome (SJS) | Parental consanguinity and familial inheritance | Normal gestation with severe muscle stiffness at birth | Dysmorphic facial features, trismus | Genetic: HSPG2 gene mutation | Kyphoscoliosis, platyspondyly with coronal clefts in vertebrae, inferior femoral and superior tibial epiphyses look enlarged and distorted | Al-Kaissi et al. [48] | |
| Trauma | Trauma | Generally uneventful | History of fractures | Abnormal gait, signs of bruises and evidence of (old) fractures | Non specific | Evidence of (old) fractures | Bar-On et al. [14] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jansen, N.J.; Dockx, R.B.M.; Witlox, A.M.; Straetemans, S.; Staal, H.M. Windswept Deformity a Disease or a Symptom? A Systematic Review on the Aetiologies and Hypotheses of Simultaneous Genu Valgum and Varum in Children. Children 2022, 9, 703. https://doi.org/10.3390/children9050703
Jansen NJ, Dockx RBM, Witlox AM, Straetemans S, Staal HM. Windswept Deformity a Disease or a Symptom? A Systematic Review on the Aetiologies and Hypotheses of Simultaneous Genu Valgum and Varum in Children. Children. 2022; 9(5):703. https://doi.org/10.3390/children9050703
Chicago/Turabian StyleJansen, Niels J., Romy B. M. Dockx, Adhiambo M. Witlox, Saartje Straetemans, and Heleen M. Staal. 2022. "Windswept Deformity a Disease or a Symptom? A Systematic Review on the Aetiologies and Hypotheses of Simultaneous Genu Valgum and Varum in Children" Children 9, no. 5: 703. https://doi.org/10.3390/children9050703
APA StyleJansen, N. J., Dockx, R. B. M., Witlox, A. M., Straetemans, S., & Staal, H. M. (2022). Windswept Deformity a Disease or a Symptom? A Systematic Review on the Aetiologies and Hypotheses of Simultaneous Genu Valgum and Varum in Children. Children, 9(5), 703. https://doi.org/10.3390/children9050703







