Clinical Differentiation between a Normal Anus, Anterior Anus, Congenital Anal Stenosis, and Perineal Fistula: Definitions and Consequences—The ARM-Net Consortium Consensus
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Terminology and Definitions
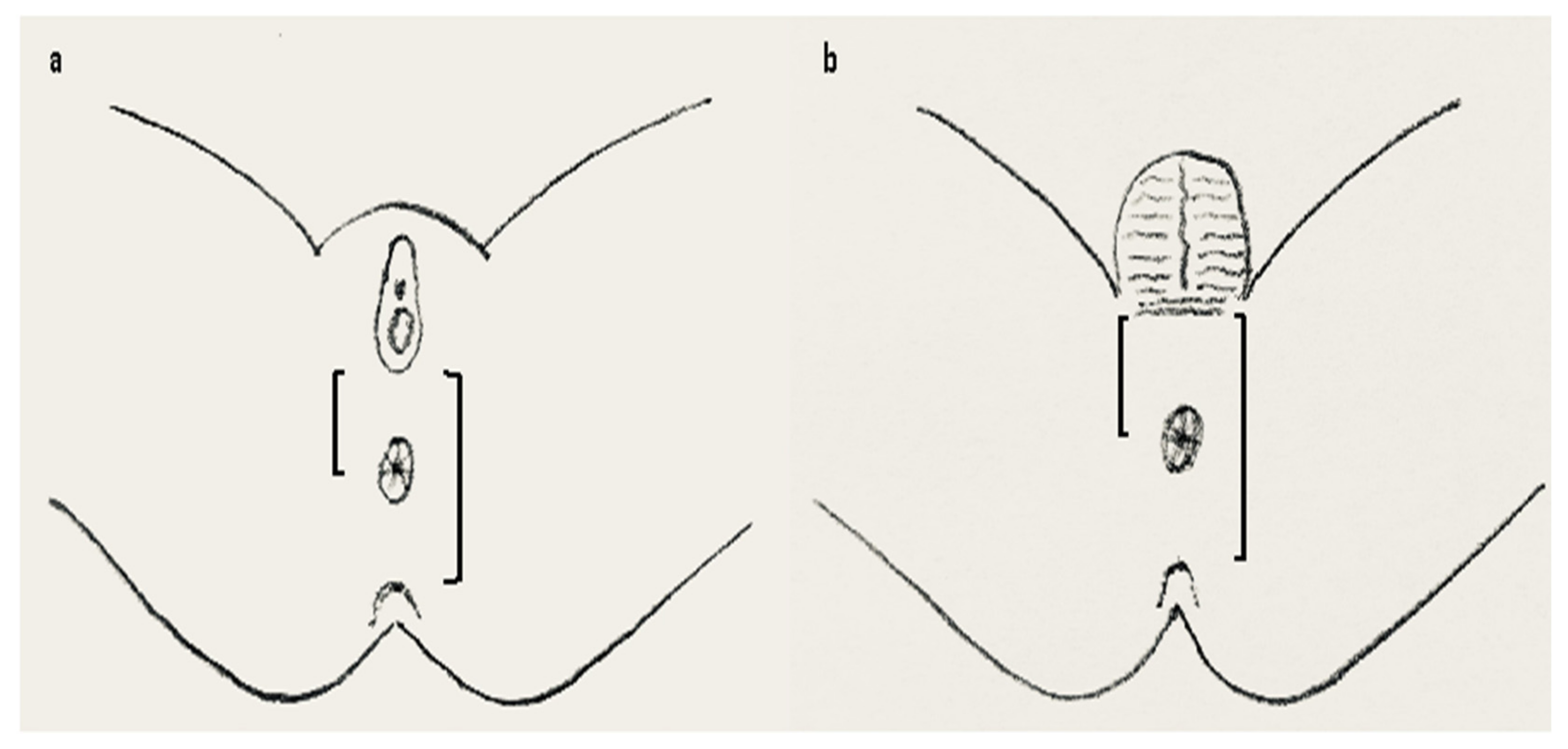
- Normal anus: Lies in a normal position along the perineum between the fourchette (girls) or scrotum (boys) and the coccyx. It is of normal caliber and circumferentially surrounded by the sphincter muscle complex (Figure 1a).
- Anterior anus (AA): Considered a normal anatomic variant and defines an anus that is anteriorly located in the perineum, yet fully surrounded by the sphincter muscle complex [24,25,26,27,28,29], and has a normal caliber [30] (Figure 1b). There is no concomitant ARM (such as rectovaginal H-type fistula, Currarino syndrome, etc.).
- Congenital anal stenosis (CAS): Anus lies in a normal position, completely surrounded by the sphincter muscle complex, but is too narrow. It may be partly covered by a median bar or membrane, usually located at the dentate line [13].
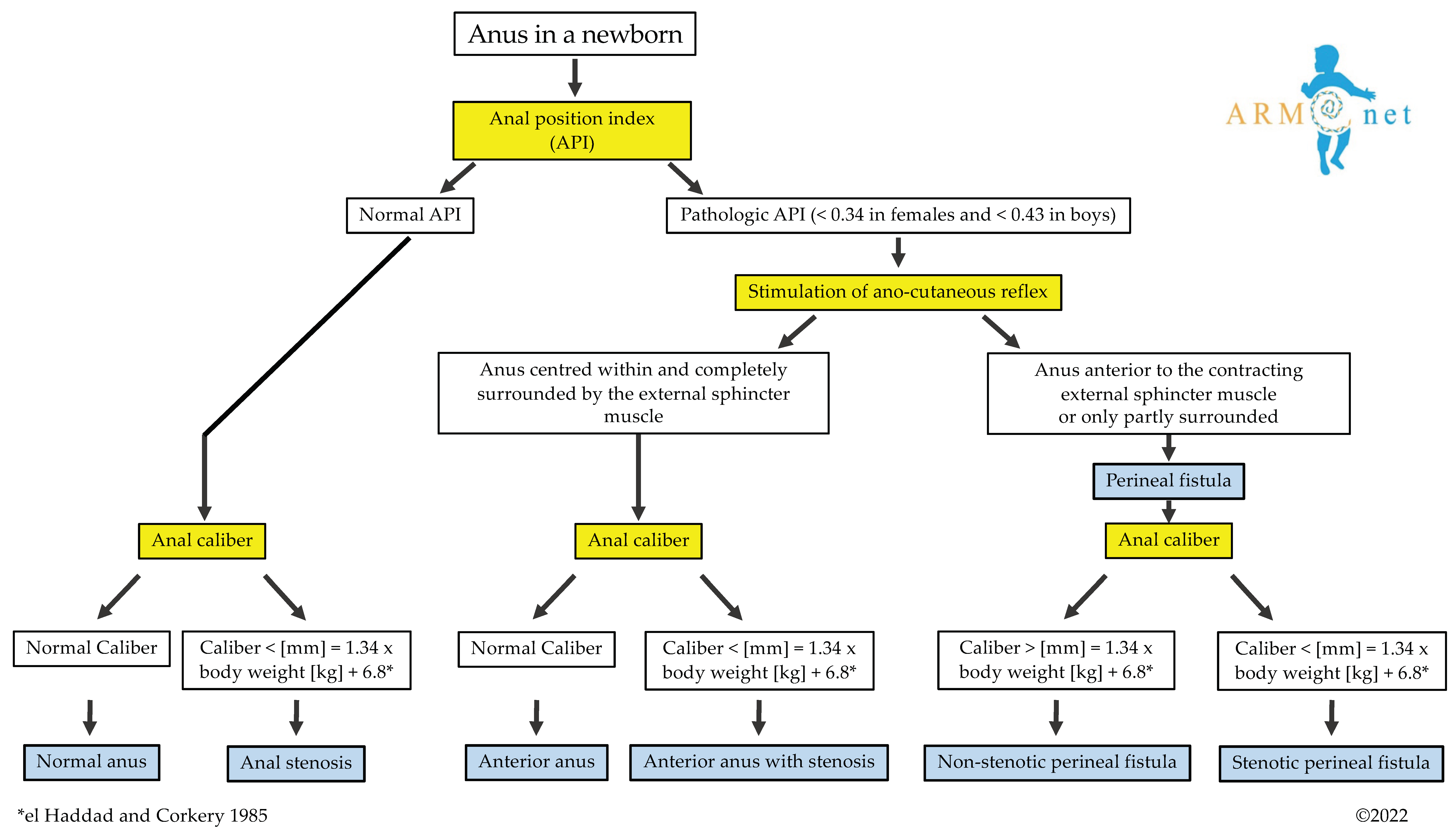
3.1.1. Diagnostic Algorithm
How to Determine Whether the Position of the Anus Is Normal?
How to Determine if the Anal Opening Is Completely Surrounded by the Sphincter Muscle Complex?
How to Determine the Caliber of the Anus in a Newborn?
3.1.2. Further Diagnostic Modalities
3.2. Clinical Aspects
3.2.1. Constipation
3.2.2. Urological and Gynecological Concerns
3.3. Management
Treatment Recommendations for Constipation in Patients with AA, Non-Stenotic PF, or CAS?
3.4. Genetical Concerns
Is Genetic Analysis Warranted in Patients with AA, PF, or CAS?
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Eltayeb, A.A. Delayed presentation of anorectal malformations: The possible associated morbidity and mortality. Pediatr. Surg. Int. 2010, 26, 801–806. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.L.; Gow, K.W.; Penner, J.G.; Blair, G.K.; Murphy, J.J.; Webber, E.M. Presentation of low anorectal malformations beyond the neonatal period. Pediatrics 2000, 105, E68. [Google Scholar] [CrossRef] [PubMed]
- Turowski, C.; Dingemann, J.; Gillick, J. Delayed diagnosis of imperforate anus: An unacceptable morbidity. Pediatr. Surg. Int. 2010, 26, 1083–1086. [Google Scholar] [CrossRef] [PubMed]
- Demirogullari, B.; Ozen, I.O.; Karabulut, R.; Turkyilmaz, Z.; Sonmez, K.; Kale, N.; Basaklar, A.C. Colonic motility and functional assessment of the patients with anorectal malformations according to Krickenbeck consensus. J. Pediatr. Surg. 2008, 43, 1839–1843. [Google Scholar] [CrossRef]
- Grano, C.; Fernandes, M.; Bucci, S.; Aminoff, D.; Lucidi, F.; Violani, C. Self-efficacy beliefs, faecal incontinence and health-related quality of life in patients born with anorectal malformations. Colorectal Dis. 2018, 20, 711–718. [Google Scholar] [CrossRef]
- Rajindrajith, S.; Devanarayana, N.M.; Crispus Perera, B.J.; Benninga, M.A. Childhood constipation as an emerging public health problem. World J. Gastroenterol. 2016, 22, 6864–6875. [Google Scholar] [CrossRef]
- Stenström, P.; Sandelin, H.; Emblem, R.; Björnland, K. Lower urinary tract symptoms in children with anorectal malformations with rectoperineal fistulas. J. Pediatr. Surg. 2016, 51, 1234–1240. [Google Scholar] [CrossRef]
- Stenström, P.; Hambraeus, M.; Arnbjörnsson, E.; Örnö, A.K. Pelvic floor in females with anorectal malformations-findings on perineal ultrasonography and aspects of delivery mode. J. Pediatr. Surg. 2015, 50, 622–629. [Google Scholar] [CrossRef]
- Lindley, R.M.; Shawis, R.N.; Roberts, J.P. Delays in the diagnosis of anorectal malformations are common and significantly increase serious early complications. Acta Paediatr. 2006, 95, 364–368. [Google Scholar] [CrossRef]
- Wilson, B.E.; Etheridge, C.E.; Soundappan, S.V.; Holland, A.J. Delayed diagnosis of anorectal malformations: Are current guidelines sufficient? J. Paediatr. Child Health. 2010, 46, 268–272. [Google Scholar] [CrossRef]
- Haider, N.; Fisher, R. Mortality and morbidity associated with late diagnosis of anorectal malformations in children. Surgeon 2007, 5, 327–330. [Google Scholar] [CrossRef]
- De Blaauw, I.; Midrio, P.; Breech, L.; Bischoff, A.; Dickie, B.; Versteegh, H.P.; Peña, A.; Levitt, M.A. Treatment of adults with unrecognized or inadequately repaired anorectal malformations: 17 cases of rectovestibular and rectoperineal fistulas. J. Pediatr. Adolesc. Gynecol. 2013, 26, 156–160. [Google Scholar] [CrossRef] [PubMed]
- Pakarinen, M.P.; Rintala, R.J. Management and outcome of low anorectal malformations. Pediatr. Surg. Int. 2010, 26, 1057–1063. [Google Scholar] [CrossRef] [PubMed]
- Lawal, T.A. Overview of Anorectal Malformations in Africa. Front. Surg. 2019, 5, 7. [Google Scholar] [CrossRef]
- Vd Merwe, E.; Cox, S.; Numanoglu, A. Anorectal malformations, associated congenital anomalies and their investigation in a South African setting. Pediatr. Surg. Int. 2017, 33, 875–882. [Google Scholar] [CrossRef]
- Aldeiri, B.; Davidson, J.R.; Eaton, S.; Coletta, R.; Cardoso Almeida, A.; Long, A.M.; Knight, M.; Cross, K.M.; Chouikh, T.; Iacobelli, B.D.; et al. Variations in the Detection of Anorectal Anomalies at Birth among European Cities. Eur. J. Pediatr. Surg. 2020, 30, 287–292. [Google Scholar] [CrossRef]
- Jonker, J.E.; Trzpis, M.; Broens, P.M.A. Underdiagnosis of Mild Congenital Anorectal Malformations. J. Pediatr. 2017, 186, 101–104. [Google Scholar] [CrossRef]
- Tareen, F.; Coyle, D.; Aworanti, O.M.; Gillick, J. Delayed diagnosis of anorectal malformation—A persistent problem. Ir. Med. J. 2013, 106, 238–240. [Google Scholar]
- Wilson, B.E.; Holland, A.J. Comment on Turowski et al.: Delayed diagnosis of imperforate anus: An unacceptable morbidity. Pediatr. Surg. Int. 2011, 27, 443–444. [Google Scholar] [CrossRef]
- American Academy of Pediatrics. Committee on Fetus and Newborn. Hospital stay for healthy term newborns. Pediatrics 2010, 125, 405–409. [Google Scholar] [CrossRef]
- El Haddad, M.; Corkery, J.J. The anus in the newborn. Pediatrics 1985, 76, 927–928. [Google Scholar] [CrossRef] [PubMed]
- Tong, W.D.; Ludwig, K.A. Neonatal colon perforation due to anorectal malformations: Can it be avoided? World J. Gastroenterol. 2013, 19, 3915–3917. [Google Scholar] [CrossRef] [PubMed]
- De Blaauw, I.; Wijers, C.H.; Schmiedeke, E.; Holland-Cunz, S.; Gamba, P.; Marcelis, C.L.; Reutter, H.; Aminoff, D.; Schipper, M.; Schwarzer, N.; et al. First results of a European multi-center registry of patients with anorectal malformations. J. Pediatr. Surg. 2013, 48, 2530–2535. [Google Scholar] [CrossRef] [PubMed]
- Herek, O.; Polat, A. Incidence of anterior displacement of the anus and its relationship to constipation in children. Surg. Today 2004, 34, 190–192. [Google Scholar] [CrossRef] [PubMed]
- Iwai, J.; Takahashi, H.; Maie, M.; Ohnuma, N.; Etoh, T.; Tanabe, M.; Aoyagi, H.; Shinbo, K. Diagnosis of anterior perineal anus (APA)—Significance of electromyographic evaluation of the external anal sphincter location. Nihon Heikatsukin Gakkai Zasshi 1988, 24, 193–203. (In Japanese) [Google Scholar] [CrossRef] [PubMed]
- Núñez-Ramos, R.; González-Velasco, M.; Núñez Núñez, R.; Enriquez Zarabozo, E.; Vargas Muñoz, I.; Blesa Sánchez, E. Valoración de la posición del ano en recién nacidos y en niños con estreñimiento crónico. Incidencia del ano anterior ectópico Evaluation of the anal position in newborns and children with chronic constipation. Incidence of anterior ectopic anus. Cir. Pediatr. 2011, 24, 84–89. [Google Scholar] [PubMed]
- Núñez-Ramos, R.; Fabbro, M.A.; González-Velasco, M.; Núñez Núñez, R.; Romanato, B.; Vecchiato, L.; D’Agostino, S.; Blesa Sánchez, E. Determination of the anal position in newborns and in children with chronic constipation: Comparative study in two European healthcare centres. Pediatr. Surg. Int. 2011, 27, 1111–1115. [Google Scholar] [CrossRef]
- Núñez-Ramos, R.; Fabbro, M.A.; González-Velasco, M.; Vargas Muñoz, I.; Núñez Núñez, R. The anal position index and the anal caliber in the newborn: Anterior ectopic anus and constipation. In Constipation in Children: Diagnosis and Treatment; Núñez, R., Fabbro, M.A., Eds.; Nova Science Publishers, Inc.: New York, NY, USA, 2013; pp. 151–165. [Google Scholar]
- Peña, A. Comments on anterior ectopic anus. Pediatr. Surg. Int. 2004, 20, 902. [Google Scholar] [CrossRef]
- Herek, O. Anterior ectopic anus: An accurate definitive term for choice of treatment? Pediatr. Surg. Int. 2001, 17, 501. [Google Scholar] [CrossRef]
- Leape, L.L.; Ramenofsky, M.L. Anterior ectopic anus: A common cause of constipation in children. J. Pediatr. Surg. 1978, 13, 627–630. [Google Scholar] [CrossRef]
- Skandalakis, J.E.; Kingsnorth, A.N.; Colborn, G.L.; Weidman, T.A. Large intestine and anorectum. In Skandalakis’s Surgical Anatomy: The Embryology and Anatomy Basis of Modern Surgery; Skandalakis, J.E., Colborn, G.L., Weidman, T.A., Eds.; Paschalidis Medical Publications: Athens, Greece, 2004; pp. 899–914. [Google Scholar]
- Bar-Maor, J.A.; Eitan, A. Determination of the normal position of the anus (with reference to idiopathic constipation). J. Pediatr. Gastroenterol. Nutr. 1987, 6, 559–561. [Google Scholar] [CrossRef] [PubMed]
- Chan, W.T.; Lee, H.C.; Wang, W.N.; Yeung, C.Y.; Jiang, C.B. Determination of the normal position of the anus in Taiwanese infants. Pediatr. Neonatol. 2009, 50, 158–161. [Google Scholar] [CrossRef]
- Davari, H.A.; Hosseinpour, M. The anal position index: A simple method to define the normal position of the anus in neonate. Acta Paediatr. 2006, 95, 877–880. [Google Scholar] [CrossRef] [PubMed]
- Genç, A.; Taneli, C.; Tansuğ, N.; Kasirga, E.; Yilmaz, D.; Küçükoğlu, T.; Onağ, A. Evaluation of the location of the anus by a modified technique in the neonate. J. Pediatr. Surg. 2002, 37, 80–82. [Google Scholar] [CrossRef]
- Mohta, A.; Goel, M.R. Determination of anal position index. Indian Pediatr. 2004, 41, 91–92. [Google Scholar]
- Reisner, S.H.; Sivan, Y.; Nitzan, M.; Merlob, P. Determination of anterior displacement of the anus in newborn infants and children. Pediatrics 1984, 73, 216–217. [Google Scholar] [CrossRef]
- Rerksuppaphol, S.; Rerksuppaphol, L. Normal anal position index in Thai newborns. J. Med. Assoc. Thai. 2008, 91, 1839–1844. [Google Scholar]
- Sharma, S.; Perumal, V.; Sharma, K.; Gupta, D.K. Varied parameters and utility of the anal position index: A systematic review and meta-analysis. Pediatr. Surg. Int. 2021, 37, 469–477. [Google Scholar] [CrossRef]
- Alemrajabi, M.; Moradi, M.; Jahangiri, F.; Marzbali, F. Anal position index; can it predict pelvic organ disorders in adults? J. Coloproctol. 2019, 39, 237–241. [Google Scholar] [CrossRef]
- Bornman, M.S.; Chevrier, J.; Rauch, S.; Crause, M.; Obida, M.; Sathyanarayana, S.; Barr, D.B.; Eskenazi, B. Dichlorodiphenyltrichloroethane exposure and anogenital distance in the Venda Health Examination of Mothers, Babies and their Environment (VHEMBE) birth cohort study, South Africa. Andrology 2016, 4, 608–615. [Google Scholar] [CrossRef]
- Patel, J.N.; Kumar, A.; Yadav, P.S.; Chadha, R.; Datta, V.; Roy Choudhury, S. The position of the anal dimple in newborns and infants with anorectal malformations and its correlation with the normal anal position. J. Pediatr. Surg. 2018, 53, 1560–1565. [Google Scholar] [CrossRef] [PubMed]
- Rizk, D.E.; Thomas, L. Relationship between the length of the perineum and position of the anus and vaginal delivery in primigravidae. Int. Urogynecol. J. Pelvic. Floor Dysfunct. 2000, 11, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Torres-Sanchez, L.; Zepeda, M.; Cebrián, M.E.; Belkind-Gerson, J.; Garcia-Hernandez, R.M.; Belkind-Valdovinos, U.; López-Carrillo, L. Dichlorodiphenyldichloroethylene exposure during the first trimester of pregnancy alters the anal position in male infants. Ann. N.Y. Acad. Sci. 2008, 1140, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Tufekci, S.; Yesildag, E. Determination of the Normal Anal Location in Neonates: A Prospective Cross-Sectional Study. Med. Bull Haseki 2021, 59, 330–334. [Google Scholar] [CrossRef]
- Akbiyik, F.; Kutlu, A.O. External genital proportions in pre-pubertal girls: A morphometric reference for female genitoplasty. J. Urol. 2010, 184, 1476–1481. [Google Scholar] [CrossRef]
- Ellibeş Kaya, A.; Doğan, O.; Yassa, M.; Başbuğ, A.; Özcan, C.; Çalışkan, E. Do external female genital measurements affect genital perception and sexual function and orgasm? Turk. J. Obstet. Gynecol. 2020, 17, 175–181. [Google Scholar] [CrossRef]
- Kreklau, A.; Vâz, I.; Oehme, F.; Strub, F.; Brechbühl, R.; Christmann, C.; Günthert, A. Measurements of a ‘normal vulva’ in women aged 15–84: A cross-sectional prospective single-centre study. BJOG 2018, 125, 1656–1661. [Google Scholar] [CrossRef]
- Mixa, V.; Skába, R.; Kraus, J.; Cvachovec, K. Influence of anesthesia on the results of intraoperative diagnostic electromyostimulation in patients with anorectal malformation. J. Pediatr. Surg. 2011, 46, 2135–2139. [Google Scholar] [CrossRef]
- Chatterjee, S.K. Rare/Regional Variants. In Anorectal Malformations in Children. Embriology, Diagnosis, Surgical Treatment, Follow-Up; Holschneider, A.M., Hutson, J.M., Eds.; Springer: Berlin/Heidelberg, Germany, 2006; pp. 252–262. [Google Scholar]
- Holschneider, A.; Hutson, J.; Peña, A.; Beket, E.; Chatterjee, S.; Coran, A.; Davies, M.; Georgeson, K.; Grosfeld, J.; Gupta, D.; et al. Preliminary report on the International Conference for the Development of Standards for the Treatment of Anorectal Malformations. J. Pediatr. Surg. 2005, 40, 1521–1526. [Google Scholar] [CrossRef]
- Bruzeau, A.H.; Moriau, D.; Bahans, C.; Mounayer, C.; Spampinato, G.; Guigonis, V.; Ballouhey, Q.; Fourcade, L. Perineal ultrasound in infants with anteriorly displaced anus: A new decision-making tool for the surgeon? Eur. J. Radiol. 2021, 142, 109854. [Google Scholar] [CrossRef]
- Casson Masselin, M.; Moriau, D.; Bahans, C.; Spampinato, G.; Guigonis, V.; Ballouhey, Q.; Fourcade, L. Transperineal ultrasound to assess anal positioning in female neonates. Med. Ultrason. 2021, 23, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Haber, H.P.; Warmann, S.W.; Fuchs, J. Transperineal sonography of the anal sphincter complex in neonates and infants: Differentiation of anteriorly displaced anus from low-type imperforate anus with perineal fistula. Ultraschall Med. 2008, 29, 383–387. [Google Scholar] [CrossRef] [PubMed]
- Kerremans, R.P.; Pennickx, F.M.; Beckers, J.P. Functional evaluation of ectopic anus and its surgical consequences. Am. J. Dis. Child. 1974, 128, 811–814. [Google Scholar] [CrossRef] [PubMed]
- Schuster, T.; Joppich, I.; Schneider, K.; Jobst, G. A computerised vector manometry study of the so-called ectopic anus. Pediatr. Surg. Int. 2000, 16, 8–14. [Google Scholar] [CrossRef]
- Keshtgar, A.S.; Athanasakos, E.; Clayden, G.S.; Ward, H.C. Evaluation of outcome of anorectal anomaly in childhood: The role of anorectal manometry and endosonography. Pediatr. Surg. Int. 2008, 24, 885–892. [Google Scholar] [CrossRef] [PubMed]
- Kashyap, P.; Bates, N. Magnetic resonance imaging anatomy of the anal canal. Australas. Radiol. 2004, 48, 443–449. [Google Scholar] [CrossRef]
- Schäfer, A.; Enck, P.; Fürst, G.; Kahn, T.; Frieling, T.; Lübke, H.J. Anatomy of the anal sphincters. Comparison of anal endosonography to magnetic resonance imaging. Dis. Colon. Rectum. 1994, 37, 777–781. [Google Scholar] [CrossRef]
- AbouZeid, A.A.; Mohammad, S.A.; Khairy, K.T. MRI anatomy of anteriorly displaced anus: What obstructs defecation? Pediatr. Radiol. 2014, 44, 831–838. [Google Scholar] [CrossRef]
- Thambidorai, C.R.; Raghu, R.; Zulfiqar, A. Magnetic resonance imaging in anterior ectopic anus. Pediatr. Surg. Int. 2008, 24, 161–165. [Google Scholar] [CrossRef]
- Antonov, N.K.; Ruzal-Shapiro, C.B.; Morel, K.D.; Millar, W.S.; Kashyap, S.; Lauren, C.T.; Garzon, M.C. Feed and Wrap MRI Technique in Infants. Clin. Pediatr. 2017, 56, 1095–1103. [Google Scholar] [CrossRef]
- De Souza, N.M.; Ward, H.C.; Williams, A.D.; Battin, M.; Harris, D.N.; McIver, D.K. Transanal MR imaging after repair of anorectal anomalies in children: Appearances in pull-through versus posterior sagittal reconstructions. AJR Am. J. Roentgenol. 1999, 173, 723–728. [Google Scholar] [CrossRef] [PubMed]
- Piloni, V.; Fioravanti, P.; Spazzafumo, L.; Rossi, B. Measurement of the anorectal angle by defecography for the diagnosis of fecal incontinence. Int. J. Colorectal Dis. 1999, 14, 131–135. [Google Scholar] [CrossRef]
- Bill, A.H., Jr.; Johnson, R.J.; Foster, R.A. Anteriorly placed rectal opening in the perineum ectopic anus; a report of 30 cases. Ann. Surg. 1958, 147, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Esposito, G.; Ascione, G.; Tamburrini, O.; Settimi, A. Antéposition de l’anus. Cause de constipation chez l’enfant [Anteposition of the anus. A cause of constipation in children]. Chir. Pediatr. 1985, 26, 279–281. [Google Scholar] [PubMed]
- Fukunaga, K.; Kimura, K.; Lawrence, J.P.; Soper, R.T.; Phearman, L.A.; Loening-Baucke, V. Anteriorly located anus: Is constipation caused by abnormal location of the anus? J. Pediatr. Surg. 1996, 31, 245–246. [Google Scholar] [CrossRef]
- Hendren, W.H. Constipation caused by anterior location of the anus and its surgical correction. J. Pediatr. Surg. 1978, 13, 505–512. [Google Scholar] [CrossRef]
- Ishitani, M.B.; Rodgers, B.M. Anteriorly displaced anus: An under-recognized cause of chronic constipation. Pediatr. Surg. Int. 1991, 6, 217–220. [Google Scholar] [CrossRef]
- Tuggle, D.W.; Perkins, T.A.; Tunell, W.P.; Smith, E.I. Operative treatment of anterior ectopic anus: The efficacy and influence of age on results. J. Pediatr. Surg. 1990, 25, 996–997; discussion 997–998. [Google Scholar] [CrossRef]
- Upadhyaya, P. Mid-anal sphincteric malformation, cause of constipation in anterior perineal anus. J. Pediatr. Surg. 1984, 19, 183–186. [Google Scholar] [CrossRef]
- Duci, M.; Fascetti-Leon, F.; Bogana, G.; Gamba, P.; Midrio, P. Conservative management of anterior located anus: A medium-long term follow up. J. Pediatr. Surg. 2021, 56, 2277–2280. [Google Scholar] [CrossRef]
- Rerksuppaphol, S.; Rerksuppaphol, L. Anterior displacement of anus: A common association with constipation in infancy. Asian Biomed. 2010, 4, 595–601. [Google Scholar] [CrossRef]
- Kyrklund, K.; Pakarinen, M.P.; Taskinen, S.; Rintala, R.J. Bowel function and lower urinary tract symptoms in females with anterior anus treated conservatively: Controlled outcomes into adulthood. J. Pediatr. Surg. 2015, 50, 1168–1173. [Google Scholar] [CrossRef] [PubMed]
- Rintala, R.J. Congenital Anorectal Malformations. In Pediatric Surgery, 2nd ed.; Burge, D.M., Griffiths, M.D., Steinbrecher, H.A., Wheeler, R.A., Eds.; CRC Press: Boca Raton, FL, USA, 2005; pp. 155–166. [Google Scholar]
- Kyrklund, K.; Pakarinen, M.P.; Rintala, R.J. Manometric findings in relation to functional outcomes in different types of anorectal malformations. J. Pediatr. Surg. 2017, 52, 563–568. [Google Scholar] [CrossRef] [PubMed]
- Krantz, K.E.; Atkinson, J.P. Pediatric and adolescent gynecology. I. Fundamental considerations. Gross anatomy. Ann. N.Y. Acad. Sci. 1967, 142, 551–575. [Google Scholar] [CrossRef]
- Breech, L. Gynecologic concerns in patients with anorectal malformations. Semin. Pediatr. Surg. 2010, 19, 139–145. [Google Scholar] [CrossRef]
- Ness, W. Obstetric anal sphincter injury: Causes, effects and management. Nurs. Times 2017, 113, 28–32. [Google Scholar]
- Halleran, D.R.; Coyle, D.; Kulaylat, A.N.; Ahmad, H.; Langer, J.C.; Gasior, A.C.; Diefenbach, K.A.; Wood, R.J.; Levitt, M.A. The cutback revisited—The posterior rectal advancement anoplasty for certain anorectal malformations with rectoperineal fistula. J. Pediatr. Surg. 2021, S0022-3468, 845–849. [Google Scholar] [CrossRef]
- Abeyaratne, M. Posterior transposition of anterior ectopic anus. J. Pediatr. Surg. 1991, 26, 725–727. [Google Scholar] [CrossRef]
- Shah, A.J.; Bhattacharjee, N.; Patel, D.N.; Ganatra, J.R. Anal shift: Preliminary results. J. Pediatr. Surg. 2003, 38, 196–198. [Google Scholar] [CrossRef]
- Rawat, J.; Singh, S.; Pant, N. Anorectal Malformations in Adolescent Females: A Retrospective Study. J. Indian Assoc. Pediatr. Surg. 2018, 23, 57–60. [Google Scholar] [CrossRef]
- Suomalainen, A.; Wester, T.; Koivusalo, A.; Rintala, R.J.; Pakarinen, M.P. Congenital funnel anus in children: Associated anomalies, surgical management and outcome. Pediatr. Surg. Int. 2007, 23, 1167–1170. [Google Scholar] [CrossRef] [PubMed]
- Jenetzky, E.; Reckin, S.; Schmiedeke, E.; Schmidt, D.; Schwarzer, N.; Grasshoff-Derr, S.; Zwink, N.; Bartels, E.; Rissmann, A.; Leonhardt, J.; et al. Practice of dilatation after surgical correction in anorectal malformations. Pediatr. Surg. Int. 2012, 28, 1095–1099. [Google Scholar] [CrossRef] [PubMed]
- Schmiedeke, E.; Busch, M.; Stamatopoulos, E.; Lorenz, C. Multidisciplinary behavioural treatment of fecal incontinence and constipation after correction of anorectal malformation. World J. Pediatr. 2008, 4, 206–210. [Google Scholar] [CrossRef] [PubMed]
- Falcone, R.A., Jr.; Levitt, M.A.; Peña, A.; Bates, M. Increased heritability of certain types of anorectal malformations. J. Pediatr. Surg. 2007, 42, 124–127; discussion 127–128. [Google Scholar] [CrossRef] [PubMed]
- Mahalik, S.K.; Mahajan, J.K.; Sodhi, K.S.; Garge, S.; Vaiphei, K.; Rao, K.L. Rare association in a female DSD case of phallus, accessory phallic urethra, perineal lipoma and anterior ectopic anus. J. Pediatr. Urol. 2013, 9, e39–e42. [Google Scholar] [CrossRef][Green Version]
- Amornfa, J.; Taecholarn, C.; Khaoroptham, S. Currarino syndrome: Report of two cases and review of the literature. J. Med. Assoc. Thai. 2005, 88, 1697–1702. [Google Scholar]
- Meroni, G. X-Linked Opitz G/BBB Syndrome. In GeneReviews®; Adam, M.P., Ardinger, H.H., Pagon, R.A., Wallace, S.E., Bean, L.J.H., Mirzaa, G., Amemiya, A., Eds.; University of Washington: Seattle, WA, USA, 2004; pp. 1993–2021. [Google Scholar]
- Anoop, P.; Sasidharan, C.K. Baller-Gerold syndrome. Indian J. Pediatr. 2002, 69, 1097–1098. [Google Scholar] [CrossRef]
- Savarirayan, R.; Tomlinson, P.; Thompson, E. Baller-Gerold syndrome associated with congenital portal venous malformation. J. Med. Genet. 1998, 35, 767–769. [Google Scholar] [CrossRef]
- Wakhlu, A.K.; Wakhlu, A.; Tandon, R.K.; Kureel, S.N. Congenital megalourethra. J. Pediatr. Surg. 1996, 31, 441–443. [Google Scholar] [CrossRef]
- Goh, D.W.; Davey, R.B.; Dewan, P.A. Bladder, urethral, and vaginal duplication. J. Pediatr. Surg. 1995, 30, 125–126. [Google Scholar] [CrossRef]
- Lall, M.; Thakur, S.; Puri, R.; Verma, I.; Mukerji, M.; Jha, P. A 54 Mb 11qter duplication and 0.9 Mb 1q44 deletion in a child with laryngomalacia and agenesis of corpus callosum. Mol. Cytogenet. 2011, 21, 19. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.P.; Lin, H.M.; Leung, C.; Lin, S.P.; Su, Y.N.; Su, J.W.; Chen, Y.T.; Wang, W. Partial monosomy 9p (9p22.2-->pter) and partial trisomy 18q (18q21.32-->qter) in a female infant with anorectal malformations. Genet. Couns. 2012, 23, 201–206. [Google Scholar] [PubMed]
- Colombo, M.; Maestri, L.; Lambiase, R.; Magni, L.A. La politelia come spia di altre malformazioni congenite: Un esempio clinico [Polythelia as a sign of other congenital malformations: A clinical example]. Pediatr. Med. Chir. 1994, 16, 399–400. [Google Scholar]
- Branski, D.; Gale, R.; Gross-Kieselstein, E.; Abrahamov, A. Propionic acidemia and anorectal anomalies in three siblings. Am. J. Dis. Child. 1977, 131, 1379–1381. [Google Scholar] [CrossRef] [PubMed]
- Maegawa, G.H.; Chitayat, D.; Blaser, S.; Whyte, H.; Thomas, M.; Kim, P.; Kim, J.; Taylor, G.; McNamara, P.J. Duodenal and biliary atresia associated with facial, thyroid and auditory apparatus abnormalities: A new mandibulofacial dysostosis syndrome? Clin. Dysmorphol. 2006, 15, 191–196. [Google Scholar] [CrossRef]
- Verloes, A.; Le Merrer, M.; Davin, J.C.; Wittamer, P.; Abrassart, C.; Bricteux, G.; Briard, M.L. The orocraniodigital syndrome of Juberg and Hayward. J. Med. Genet. 1992, 29, 262–265. [Google Scholar] [CrossRef]
- James, P.A.; McGaughran, J. A severe case of oculo-ectodermal syndrome? Clin. Dysmorphol. 2002, 11, 179–182. [Google Scholar] [CrossRef]
- Chamaria, K.; Shetty, R. Ectopic anus with barrel gun perineum rare type of anorectal anomaly. J Radiol Case Rep. 2013, 7, 31–36. [Google Scholar] [CrossRef]
- Ottolenghi, A.; Sulpasso, M.; Bianchi, S.; Bettili, G.; Salloum, A.; Liber, H. Ectopic anus in childhood. Eur. J. Pediatr. Surg. 1994, 4, 145–150. [Google Scholar] [CrossRef]
- Pandey, A.; Pandey, P.; Singh, S.P.; Agarwal, S.; Gupta, V.; Verma, R. Histology with immunohistochemistry of the fistula region in female anorectal malformation: Can it be used for neo-anus reconstruction? J. Paediatr. Child Health. 2018, 54, 177–182. [Google Scholar] [CrossRef]
- Petrino, R.A.; Golladay, E.S.; Mollitt, D.L.; Butler, H. Surgically correctable fecal incontinence. South Med. J. 1985, 78, 130–133. [Google Scholar] [CrossRef] [PubMed]
- Rex, D.K.; Lappas, J.C.; Popp, B. Association of anterior ectopic anus and partial absence of levator musculature in a woman with impaired defecation. Report of a case. Dis. Colon. Rectum. 1990, 33, 974–976. [Google Scholar] [CrossRef] [PubMed]
- Tesař, M.; Vávra, P.; Richter, V.; Ihnát, P. Anus perinei ventralis in adulthood—Case report. Rozhl. Chir. 2020, 99, 552–555. [Google Scholar]
- Upadhyaya, V.D.; Bharti, L.K.; Mishra, A.; Yousuf, M.; Mishra, P.; Kumar, B. Constipation after surgery for anorectal malformations: Unrecognised problem until it is a problem. Afr. J. Paediatr. Surg. 2021, 18, 67–71. [Google Scholar] [CrossRef]
- Yeung, C.K.; Lund, L. Laparoscopic cecostomy for anterior ectopic anus with constipation: A new and technical proposal. Eur. J. Pediatr. Surg. 2000, 10, 276–277. [Google Scholar] [CrossRef] [PubMed]
- Ruttenstock, E.M.; Zani, A.; Huber-Zeyringer, A.; Höllwarth, M.E. Pre- and postoperative rectal manometric assessment of patients with anorectal malformations: Should we preserve the fistula? Dis. Colon. Rectum. 2013, 56, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Swan, S.H.; Sathyanarayana, S.; Barrett, E.S.; Janssen, S.; Liu, F.; Nguyen, R.H.; Redmon, J.B.; TIDES Study Team. First trimester phthalate exposure and anogenital distance in newborns. Hum. Reprod. 2015, 30, 963–972. [Google Scholar] [CrossRef] [PubMed]
- Zarean, M.; Keikha, M.; Feizi, A.; Kazemitabaee, M.; Kelishadi, R. The role of exposure to phthalates in variations of anogenital distance: A systematic review and meta-analysis. Environ. Pollut. 2019, 247, 172–179. [Google Scholar] [CrossRef]
- Romano-Riquer, S.P.; Hernández-Avila, M.; Gladen, B.C.; Cupul-Uicab, L.A.; Longnecker, M.P. Reliability and determinants of anogenital distance and penis dimensions in male newborns from Chiapas, Mexico. Paediatr. Perinat. Epidemiol. 2007, 21, 219–228. [Google Scholar] [CrossRef]
- Salazar-Martinez, E.; Romano-Riquer, P.; Yanez-Marquez, E.; Longnecker, M.P.; Hernandez-Avila, M. Anogenital distance in human male and female newborns: A descriptive, cross-sectional study. Environ. Health. 2004, 3, 8. [Google Scholar] [CrossRef]


| Study | Age Group | Country | N | Mean Values of API | Anterior Displacement -2 SD | ||
|---|---|---|---|---|---|---|---|
| Male (SD) (n) | Female (SD) (n) | Male | Female | ||||
| 1. Reisner et al., 1984 [38] | Newborn | Israel | 200 | 0.58 (0.06) (100) | 0.44 (0.05) (100) | <0.46 | <0.34 |
| 4-18 months | 30 | 0.56 (0.4) (15) | 0.40 (0.06) (15) | <0.28 | |||
| 2. Bar-Maor and Eitan 1987 [33] | 3 days–12 years | Israel | 104 | 0.56 (0.10 *) (74) | 0.39 (0.09) (30) | <0.36 | <0.21 |
| Constipated 3d-12y | 34 | 0.58 (0.09) (23) | 0.4 (0.07) (11) | <0.4 | <0.26 | ||
| 3. Genç et al., 2002 [36] | Newborn | Turkey | 60 | 0.53 (0.05) (26) | 0.46 (0.08) (34) | <0.43 | <0.30 |
| 4. Mohta and Goel 2004 [37] | Newborn–3 years | India | 387 | 0.43 (0.05) (300) | 0.37 (0.06) (87) | <0.33 | <0.25 |
| 5. Herek and Polat 2004 [24] | Newborn–10 years | Turkey | 357 | 0.51 (0.08) (191) | 0.36 (0.08) (166) | <0.35 | <0.20 |
| 6. Rerksuppaphol et al., 2008 [39] | Newborn | Thailand | 403 | 0.51 (0.07) (203) | 0.38 (0.08) (200) | <0.37 | <0.22 |
| 7. Davari and Hosseinpour 2006 [35] | Newborn | Iran | 400 | 0.54 (0.07) (200) | 0.45 ** (0.08) (200) | <0.40 | <0.29 |
| 8. Patel et al., 2018 [43] | Newborn and infants | India | 65 | 0.53 (0.07) (31) | 0.36 (0.07) (34) | <0.39 | <0.22 |
| 9. Chan et al., 2009 [34] | Neonates | Taiwan | 200 | 0.54 (0.03) (100) | 0.40 (0.04) (100) | <0.48 | <0.32 |
| 5–19 months | 30 | 0.53 (0.02) (15) | 0.39 (0.06) (15) | <0.49 | <0.27 | ||
| 10. Núñez-Ramos et al., 2011 [27] | Newborn | Spain | 529 | 0.53 (0.06) (262) | 0.40 (0.05) (267) | <0.41 | <0.30 |
| Older constipated patients | 64 | 0.47 (0.10) (26) | 0.36 (0.10) (38) | <0.27 | <0.16 | ||
| 11. Núñez-Ramos et al., 2011 [27] | Newborn | Italy | 483 | 0.51 (0.06) (237) | 0.39 (0.08) (246) | <0.39 | <0.23 |
| 12. Torres-Sanchez et al., 2008 [45] | Newborn–Infants | Mexico | 71 | 0.6 (0.07) (37) | 0.5 (0.07) (34) | <0.46 | <0.36 |
| Sharma et al., 2021 [40] | overall mean of all studies: | 0.51 (0.04) | 0.40 (0.03) | <0.43 | <0.34 | ||
| 13. Rizk and Thomas 2000 [44] | Adult women | UAE | 212 | 0.49 (0.12) (212) | <0.25 | ||
| 14. Bornman et al., 2016 [42] | Newborn | South Africa | 659 | 0.58 (0.59) (336) *** | 0.46 (0.61) (323) *** | <0.46 | <0.33 |
| 15. Alemrajabi et al., 2019 [41] | Adults | Iran | 63 | 0.53 (0.11) (48) | 0.45 (0.16) (15) | <0.31 | <0.13 |
| 16. Tufekci and Yesildag 2021 [46] | Neonates | Turkey | 405 | 0.52 (0.05) (230) | 0.39 (0.4) (175) | <0.42 **** | <0.31 **** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amerstorfer, E.E.; Schmiedeke, E.; Samuk, I.; Sloots, C.E.J.; van Rooij, I.A.L.M.; Jenetzky, E.; Midrio, P.; ARM-Net Consortium. Clinical Differentiation between a Normal Anus, Anterior Anus, Congenital Anal Stenosis, and Perineal Fistula: Definitions and Consequences—The ARM-Net Consortium Consensus. Children 2022, 9, 831. https://doi.org/10.3390/children9060831
Amerstorfer EE, Schmiedeke E, Samuk I, Sloots CEJ, van Rooij IALM, Jenetzky E, Midrio P, ARM-Net Consortium. Clinical Differentiation between a Normal Anus, Anterior Anus, Congenital Anal Stenosis, and Perineal Fistula: Definitions and Consequences—The ARM-Net Consortium Consensus. Children. 2022; 9(6):831. https://doi.org/10.3390/children9060831
Chicago/Turabian StyleAmerstorfer, Eva E., Eberhard Schmiedeke, Inbal Samuk, Cornelius E. J. Sloots, Iris A. L. M. van Rooij, Ekkehart Jenetzky, Paola Midrio, and ARM-Net Consortium. 2022. "Clinical Differentiation between a Normal Anus, Anterior Anus, Congenital Anal Stenosis, and Perineal Fistula: Definitions and Consequences—The ARM-Net Consortium Consensus" Children 9, no. 6: 831. https://doi.org/10.3390/children9060831
APA StyleAmerstorfer, E. E., Schmiedeke, E., Samuk, I., Sloots, C. E. J., van Rooij, I. A. L. M., Jenetzky, E., Midrio, P., & ARM-Net Consortium. (2022). Clinical Differentiation between a Normal Anus, Anterior Anus, Congenital Anal Stenosis, and Perineal Fistula: Definitions and Consequences—The ARM-Net Consortium Consensus. Children, 9(6), 831. https://doi.org/10.3390/children9060831







