Abstract
Childhood overweight and obesity represent a growing public health problem worldwide. Since the 1980s, the global prevalence of overweight and obesity in childhood and adolescence has increased by 47%. The promotion of exercise is an important intervention to reduce the physical damage of obesity. The meta-analysis was conducted in accordance with the general guidelines for the reporting of systematic reviews and meta-analyses (PRISMA). The PubMed, SciELO, ScienceDirect and Google Scholar databases were searched from August to December 2021. The search yielded 722 titles published between 2000 and 2021. After screening the titles and abstracts, 64 duplicate articles were detected, and 27 articles were ultimately included in the systematic review, including 26 articles published in English and one published in Spanish. There was a statistically significant effect of the strength training interventions on the percentage of body fat, Test of 0 i = (p = 0.00, z = 6.92), Test of 0 = (p = 0.00, Q (9) = 42.63). The findings reveal that strength training has a positive impact on the treatment of body fat in children and adolescents with overweight and obesity.
1. Introduction
Childhood overweight and obesity is a global public health problem [1]. It is defined as a condition in which the body carries excessive and unhealthy amounts of body fat, which causes the individual to weigh more than their ideal weight [2]. This complex and multifactorial disease can begin in childhood and may be caused by a genetic-environmental interaction [3].
An imbalance between the energy expended (exercise) and the energy ingested (food) could lead to overweight and obesity. When food intake regularly exceeds calorie expenditure, unused energy is stored in adipose tissue or body fat [4]. Most people who eat and drink more than they use energy will produce adipose tissue to store excess energy [5]. There are many children who have a normal BMI but have a high percentage of body fat and low muscle mass. The promotion of exercise is an important intervention to reduce the physical damage of obesity [6,7].
Since the 1980s, the global prevalence of overweight and obesity in childhood and adolescence has increased by 47%. This trend has been observed in developed countries (where 24% of boys and 23% of girls are overweight or obese) and developing countries (where 13% of boys and girls are overweight or obese). Although the prevalence of childhood overweight and obesity in developed countries may have begun to stabilize, it continues to increase in developing countries, while socioeconomic inequalities in the prevalence of overweight and obesity persist or are expanding in many populations [1].
Childhood obesity has many harmful effects and comorbidities (i.e., associated diseases and disorders) that frequently produce a metabolic syndrome that greatly increases the risk of the individual remaining in an obesogenic state in adolescence and adulthood; 50% of the children who are obese at 6 years remain obese throughout adulthood, and 80% of the children who are obese in adolescence remain obese throughout adulthood [8]. Obesity has serious effects on life expectancy and quality of life, including hyperinsulinemia (high insulin levels), hypertension (high blood pressure) and dyslipidemia (abnormal lipid levels), which can cause heart disease, diabetes, cancer, hypertension and kidney diseases [9].
Strength Training (ST) is a term used to denote a component of sport and physical training that is designed to improve muscle strength, muscle power and muscular endurance, with a wide range of resistive loads, from body weight to weight [10,11]. This type of program can include the use of free weights (bars and dumbbells), weight machines, medicine balls, kettlebells, elastic tubes or a person’s own body weight [12,13].
In the past, strength training was not advisable before the end of sexual maturation due to the lack of hormonal status, especially of testosterone, typical of children and adolescents. It was suspected that strength training caused a negative effect on growth and bone maturation, consequently increasing the predisposition to trauma, especially with respect to the epiphyses, growth cartilages, bones, and bone connective tissue [11,13].
Before puberty and after the age of 70, strength training is not useful from physiological perspective [12]. It is currently possible to verify that the human organism is trainable throughout the life period, although this possibility of training is subject to notable changes that depend on the individual development phase [14].
A meta-analysis conducted in 2018 analyzed the effects of strength training on weight status in children and adolescents with normal weight, overweight and obesity across 24 randomized controlled trials [15]. After examining body mass (kg), BMI, body fat (%), lean mass (kg), skinfolds (mm) and waist circumference (cm), the analysis revealed a significant effect of Strength Training (ST) on body fat, fat-free mass, fat mass and waist circumference but no significant overall effect on body mass and BMI. These findings indicate that ST could play a role in the treatment and prevention of obesity.
However, another meta-analysis conducted in 2013 [16] identified that strength training in children and adolescents with overweight and obesity seems to have very small-to-small effects on body composition and moderate-to-large effects on strength.
The benefits of ST in children and adolescents have been documented, and organizations such as NSCA, UKSCA and AAP (American Academy of Pediatrics) have developed statements in a position of support [10,17,18]. One of these benefits is the positive effect of ST on weight status by reducing body fat, increasing muscle mass and improving the function of nonskeletal muscle tissues; however, the underlying molecular mechanisms of these beneficial effects are largely unknown [19].
Most research on the benefits of exercise on adipose tissue has focused on aerobic exercise [19]. Thus, there is a lack of information on the systemic benefits for body composition of strength exercise beyond improvements in muscle function.
The objective of this study was to perform a systematic meta-analysis to determine the effect of strength training on body fat in children and/or adolescents with overweight or obesity.
2. Materials and Methods
2.1. Study Search and Selection Strategies
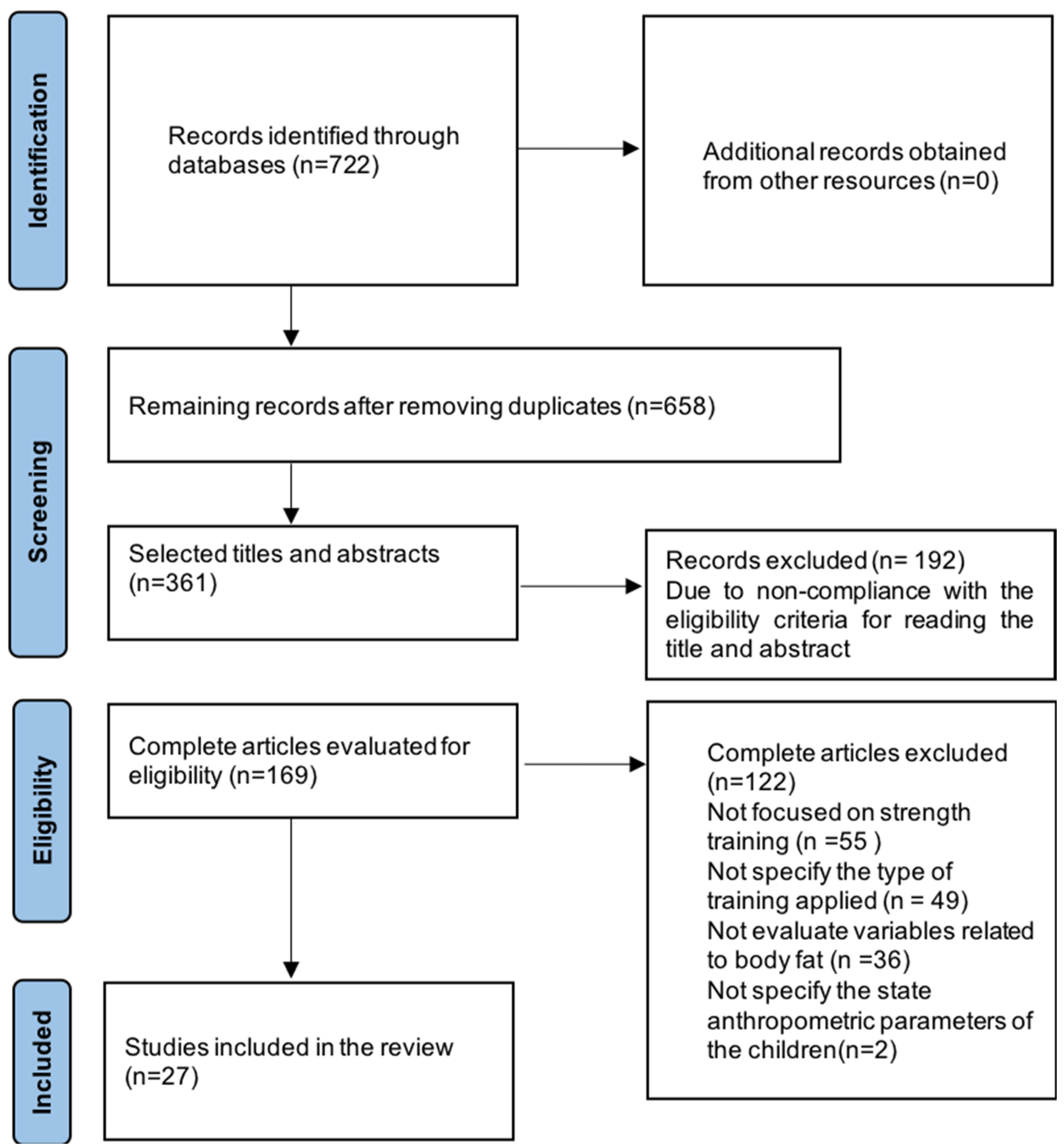
The present meta-analysis was performed in accordance with the general guidelines for the reporting of systematic reviews and meta-analyses (PRISMA) See Figure 1. The PubMed, SciELO, ScienceDirect and Google Scholar databases were systematically searched from August to December 2021. The registration protocol was carried out in the Open Science Framework with the registration number 10.17605/OSF.IO/MNCNBI.
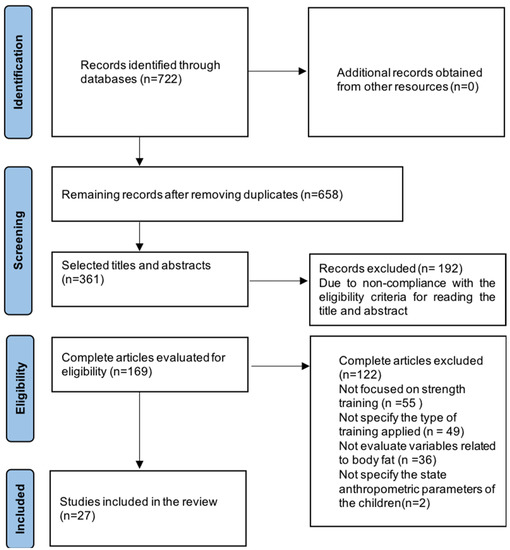
Figure 1.
PRISMA flowchart of systematic search and included studies.
The following keywords were used in English and Spanish. Target population: Youth, youth, child, adolescent, puberty, boys, girls; Strength training: resistance training, muscle strength training, muscle strength program, muscle strength intervention, muscle strength exercise, weight training, strength and conditioning, concurrent training; Weight status: obese, overweight, body composition, waist circumference, fat, body mass, weight, skin fold.
For studies that did not provide access to the complete document or studies that lacked the necessary descriptive statistics, the authors were contacted via email.
2.2. Inclusion and Exclusion Criteria
The inclusion criteria were as follows: (I) participants were aged between 5 and 19 years, (II) body fat was analyzed, (III) randomized controlled trials, (IV) a muscle strength training was implemented and (V) original publications in English or Spanish published from 2000 to 2021.
The exclusion criteria were as follows: (I) the subjects had a pathological condition or disability that affected movement (e.g., cerebral palsy/dyspraxia), (II) the subjects were found to have a behavioral or neuropsychological condition and (III) plyometric, vibratory or neuromuscular training was used, or training specifically for rehabilitation purposes was implemented.
2.3. Data Extraction
The data were extracted using an electronic form and included study characteristics (country, year of publication, sample), characteristics of the participants (age, nutritional status), components of the intervention (duration, type of training), outcome measures (body fat, BMI, waist circumference) and methodological quality. The study was carried out by two researchers, they evaluated the selection of titles and abstracts. Following that, full articles will use the inclusion and exclusion criteria. No automated tools were used in the process.
2.4. Evaluation of Methodological Quality and Risk of Bias
To evaluate the methodological quality and the risk of bias of the included studies, the “Quality assessment tool for quantitative studies” developed by the public health practice project was used [20]. The results of the evaluation led to a general methodological rating of strong, moderate or weak in eight sections: selection bias, study design, confounding factors, blinding, data, collection methods, elimination and dropouts, originality of the treatment and analysis. This evaluation tool has been proven to be valid and reliable. To verify the reliability, this evaluation was carried out in 100% of the included studies, and any disagreement was resolved by discussion between the two authors.
2.5. Data Analysis
The reference data were expressed as numbers, proportions, averages and standard deviations. The meta-analysis was performed with the statistical package Stata/IC14.2 (Texas, USA), and a random effects model was used to examine the decrease or increase in percentage of body fat with 95% confidence intervals (CI). The T 2, H 2 and I 2 statistics were used to evaluate the heterogeneity of the studies; heterogeneity was not determined between the studies if I 2 was less than 50%, and an I 2 value equal to or greater than 50% indicated heterogeneity. A value of H2 equal to 1 means that there is no heterogeneity, and its value increases when heterogeneity between studies increases. To identify publication bias, the effect sample sizes were plotted against standard errors.
3. Results
3.1. Search Results
A total of 722 articles were identified from the PubMed, Science Direct, Scopus, SciELO and Google Scholar databases. In the screening phase, duplicates were eliminated, and the studies were filtered by screening the titles, abstracts and keywords, resulting in 361 references. A total of 169 studies were subjected to full-text analysis, with 55 studies being excluded because they were not focused on strength training, 49 being excluded because they did not specify the type of training applied, 36 being excluded because they did not evaluate variables related to body fat, and 2 being excluded because they did not specify the state anthropometric parameters of the children. Twenty-eight studies met the selection criteria [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48].
3.2. Characteristics of the Studies
Across the 28 included articles, 1834 children and adolescents with overweight or obesity were analyzed, with an average age (years) of 12.5 ± 2.6 (min: 6 max: 19). The average duration (weeks) was 12 ±. 7.3, the average frequency (weekly) was of 3 ± 1.1 days, the average duration (minutes) of 60 ± 10.1 per session, and the average sets per exercise was 3 ± 1.3 with an average of repetitions per exercise of 12 ± 6.6. The studies were conducted in 12 countries: Brazil (10 studies), the United States (4 studies), Australia (3 studies), Canada (2 studies), France (2 studies), Chile (1 study), China (1 study), South Korea (1 study), Spain (1 study), Germany (1 study), Italy (1 study) and Austria (1 study). After the interventions in 92% of the studies, body fat was reduced, the remaining 8% did not present significant results, and the average attendance rate for the studies that measured this variable was 75%. For the studies that provided information, 15% presented a low intensity <50% maximum repetition (MR), 35% medium intensity 50–75% MR, and 50% a high intensity >75%.
3.3. Results of Methodological Quality
The Table 1 show the results of the methodological quality assessment, where the studies obtained a moderate score of 60.7%, a strong score of 35.7% and a weak score of 3.6%.

Table 1.
Quality assessment for quantitative studies.
3.4. Results of the Meta-Analysis
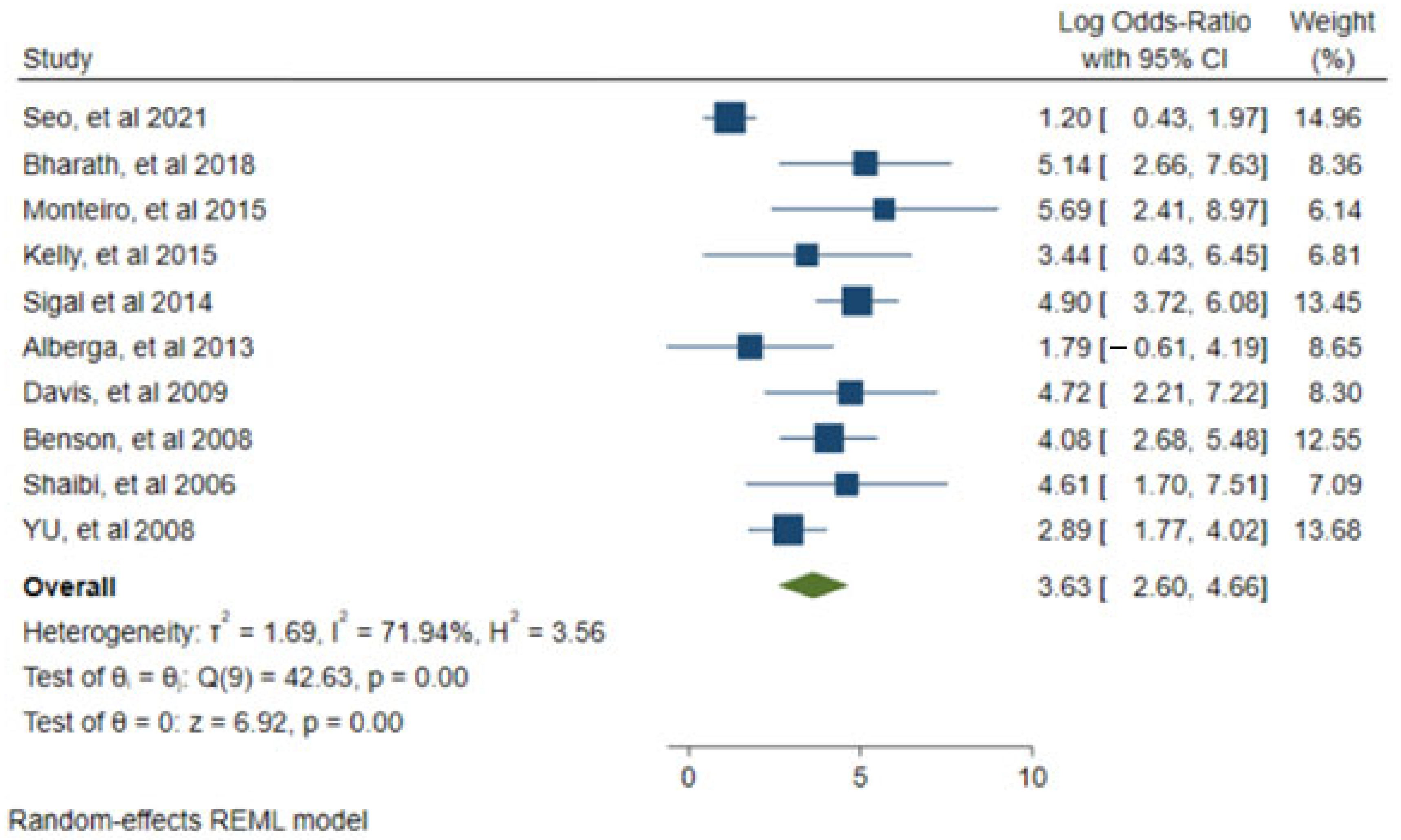
Ten studies reported the necessary statistics to construct the forest plot and funnel plot [21,25,31,32,37,39,44,46,47,48]. Using the random effects model, the results of the percentage of body fat were compared after the interventions with 95% CIs. The results of the meta-analysis revealed that ST is an effective intervention for the treatment of body fat (p = 0.00, z = 6.92), (p = 0.00, Q (9) = 42.63). The heterogeneity parameters of T 2 = 1.69, H 2 = 3.56 and I 2 = 71.94% indicated significant heterogeneity. See Figure 2 and Figure 3.
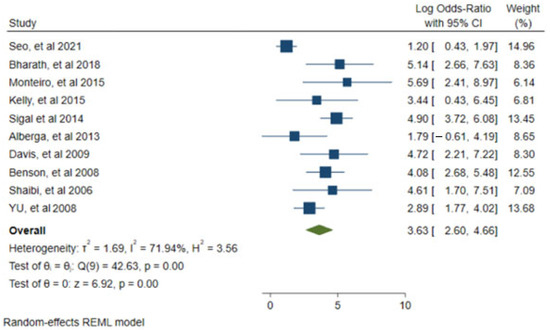
Figure 2.
Forest plot of the random effects model for the meta-analysis between the correlation of reduction or increase in percentage of body fat. Data from: [21,25,31,32,37,39,44,46,47,48].
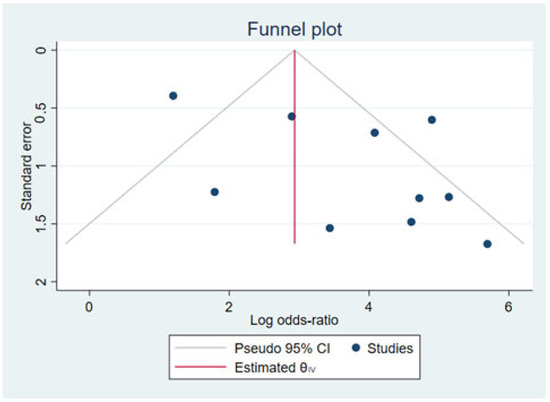
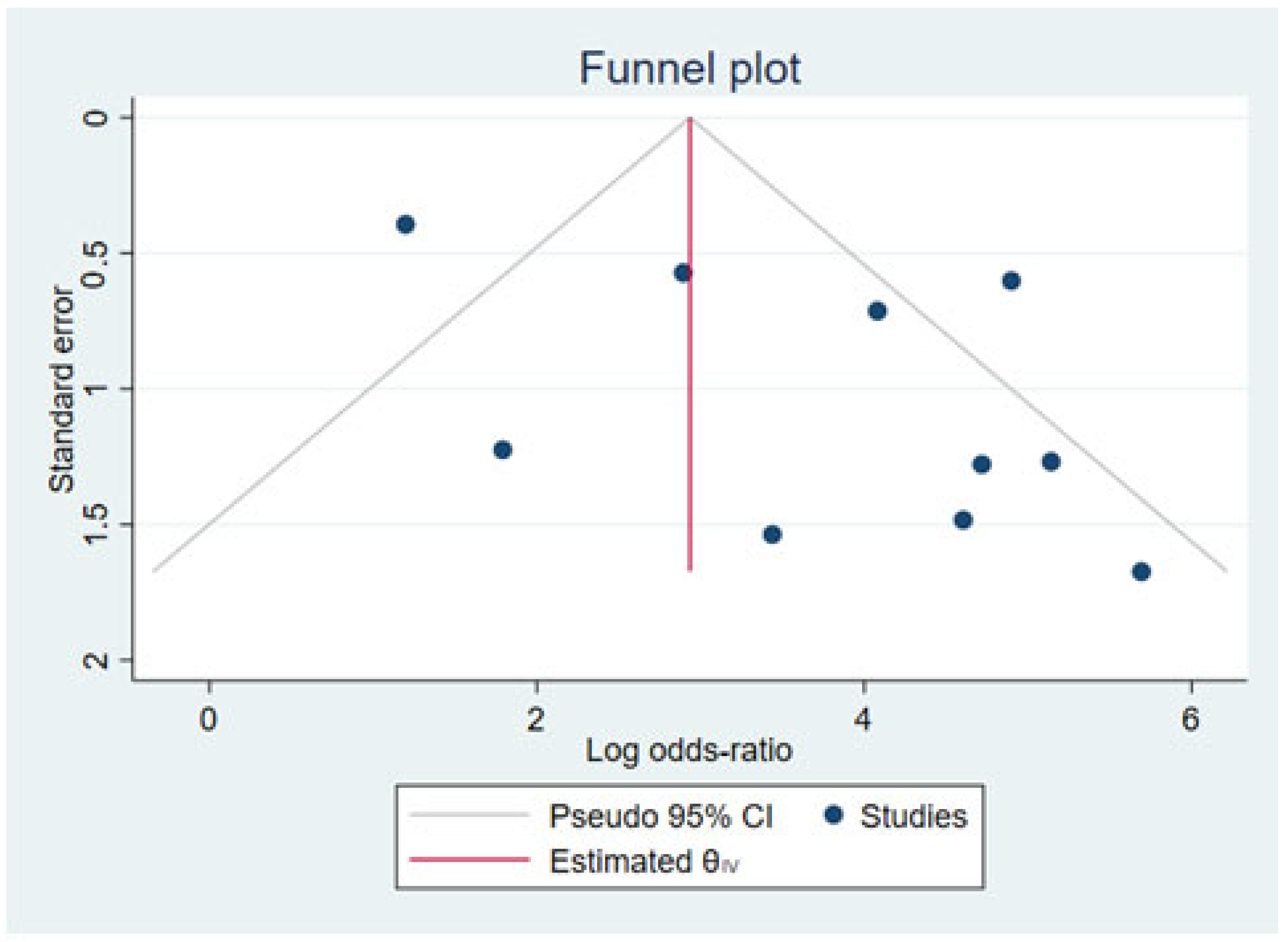
Figure 3.
Funnel plot using sample sizes of the effect against standard errors Data from: [25,31,32,37,44,46,47,49].
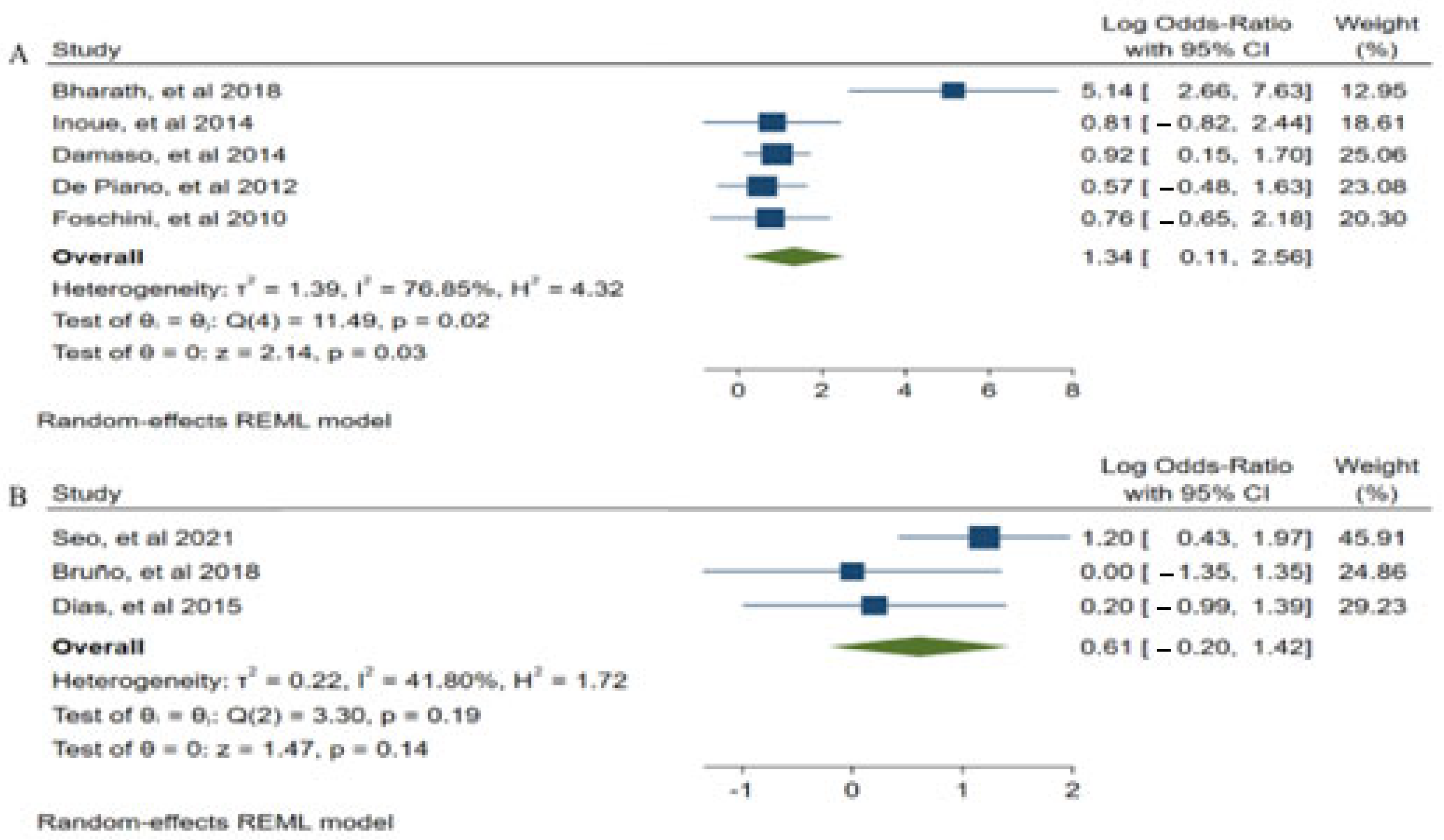
3.5. Subgroup Analysis
In an attempt to determine the causes of heterogeneity in our analysis, subgroup analyzes were performed according to the intensity of the studies (A: High and medium intensities >51% MR, B: Low intensities <50% MR). See Figure 4.
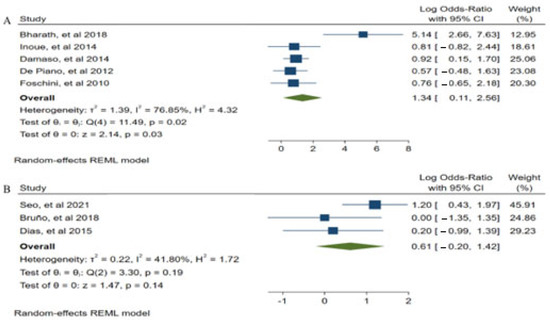
Figure 4.
Subgroup analysis ((A): High and medium intensities > 51% MR, (B): Low intensities < 50% MR) Data from: [21,25,26,30,34,35,41,42].
(A) Five studies were used to construct medium and high intensity subgroup analyzes [25,34,36,41,42], showing that medium and high intensity ST could be an effective intervention for the treatment of body fat loss (p = 0.03, z = 2.14), (p = 0.02, Q (4) = 11.49). (B). Therefore, the studies to construct low intensity subgroup [21,26,30], were not statistically significant for the treatment of body fat (p = 0.14, z = 1.47), (p = 0.19, Q (2) = 3.30).
4. Discussion
According with the position statements of the American Academy of Pediatrics [10], UKSCA [17] and NSCA [18] on youth strength training suggest that it can have a positive impact on body fat, and the significant findings of this meta-analysis for body fat percentage are conclusive, supporting these claims. Regardless of dietary restrictions [50], being more effective at training in the gym [22,24,35,41,42] than home workouts [26,31]. Strength training showed a statistically significant effect on body fat percentage. Although this decrease in fat is expected, it is necessary to investigate in-depth studies considering the individual response to the intensity of strength training.
The training intensities that presented the best benefits for the reduction of body fat were high and medium [22,24,34,42,45], a possible cause may be that these intensities are close to muscle failure > 5 repetitions in reserve, this has been shown to be favorable [14], additionally if it is added to an adequate diet [22,37,51] these results are increased.
In the funnel plot (Figure 3), an asymmetry can be observed, which indicates publication bias. A possible cause is that due to the very specific research topic, there are a limited number of relevant studies; likewise, the existing studies have low sample sizes because the inclusion criteria are only children or adolescents with overweight or obesity.
It has been suggested that training periods of more than 14 weeks are required to observe effects on body fat and increases in lean muscle mass [43]. This suggests that the duration of the intervention for several of the studies may not have been long enough to invoke positive measurable changes.
Although more studies are required to provide a better understanding of the mechanism of a reduction in body fat due to a strength training intervention, it has been reported that a possible cause would be that the ST itself favors the loss of fat through the muscle. The muscle tissue releases Extracellular Vesicles (EVs) that present a potential mechanism through which the beneficial effects of exercise are transmitted to other tissues [52,53]. These EVs contain miR-1 absorbed by adipose tissue, promoting adrenergic signaling and lipolysis in adipose tissue, which favors fat oxidation [19]. Alternatively, it may simply be due to an increase in skeletal muscle mass and the resulting increase in basal metabolic rate [54]. In particular, this has been observed in adolescents [55].
On the other hand, it is also suggested that these changes could be due to increases in total energy expenditure that may have occurred simply when participating in an exercise intervention instead of an increase in metabolically active lean tissue. However, it is important to note that the data of the participants, children and adolescents included in the analysis may have had an impact on the results.
There are limitations in this study, that must be taken present into account when explain the results. First, the included studies used several different types of exercise intervention (exclusive strength training or strength training plus aerobic training) with great variability within the study interventions with respect to the number of participants (ranging from 18 to 304 participants). The duration varied from 6 to 52 weeks, the frequency varied from 2 to 5 times per week, and the programs also included a mixture of a series of 1 to 4 per exercise and repetitions with a range of 4 to 25 with low intensities, medium or high according to the 1MR, with different methodologies such as undulating periodization, training of a progressive nature with an increase in the number of sets, repetitions and resistance; in circuit, with linear periodization or with daily undulating periodization, circuit training; and with training at home or in the gym, added to the fact that the age of entry was not measured.
For the results, there were a variety of different measurement methods; for example, the percentage of body fat was measured by DEXA, BodPod, bioelectrical impedance, skinfolds and magnetic resonance. In the analysis, not all studies reported data to allow an exhaustive investigation, so limited conclusions can be drawn based on this level of additional analysis.
5. Conclusions
The results of this systematic review confirm that ST could be an effective intervention for the treatment of body fat percentage in the first 14 weeks of intervention with better long-term results (>36 weeks), in turn, high and medium intensities are beneficial for reducing body fat percentage. However, a more in-depth research is needed on ST intensities and their effect at the individual level in children and adolescents, these findings can be used to develop new methods for the treatment of childhood obesity.
Author Contributions
Conceptualization, L.D.M.-H., J.A.-R. and E.R.-M.; Formal analysis, L.D.M.-H., R.B.-G., M.d.C.C.-M., J.R.-V., and O.R.F.-C.; Writing—original draft preparation, L.D.M.-H., and O.R.F.-C.; Writing—review and editing, J.A.-R., L.M.-C., R.C.J.-S., and N.d.S.C.-C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
This study was supported by a scholarship awarded by the National Council of Science and Technology of Mexico (CONACYT) No. CVU: 1077876 to LDM-H. The authors thank Itze Noriega Muro for reviews of this work.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bleich, S.N.; Vercammen, K.A.; Zatz, L.Y.; Frelier, J.M.; Ebbeling, C.B.; Peeters, A. Interventions to prevent global childhood overweight and obesity: A systematic review. Lancet Diabetes Endocrinol. 2018, 6, 332–346. [Google Scholar] [CrossRef]
- Tsatsoulis, A.; Paschou, S.A. Metabolically Healthy Obesity: Criteria, Epidemiology, Controversies, and Consequences. Curr. Obes. Rep. 2020, 9, 109–120. [Google Scholar] [CrossRef] [PubMed]
- Ceballos, J.J.; Pérez, R.; Flores, J.A.; Vargas-Sánchez, J.; Ortega-Gutiérrez, G.; Madriz-Prado, R.; Hernández-Moreno, A. Obesidad Una Pandemia Del Siglo 21. Rev. Sanid. Mil. 2018, 72, 332–338. [Google Scholar]
- Löffler, M.C.; Betz, M.J.; Blondin, D.P.; Augustin, R.; Sharma, A.K.; Tseng, Y.-H.; Scheele, C.; Zimdahl, H.; Mark, M.; Hennige, A.M.; et al. Challenges in tackling energy expenditure as obesity therapy: From preclinical models to clinical application. Mol. Metab. 2021, 51, 101237. [Google Scholar] [CrossRef]
- Stanhope, K.L.; Goran, M.I.; Bosy-Westphal, A.; King, J.C.; Schmidt, L.A.; Schwarz, J.M.; Stice, E.; Sylvetsky, A.C.; Turnbaugh, P.J.; Bray, G.A.; et al. Pathways and mechanisms linking dietary components to cardiometabolic disease: Thinking beyond calories. Obes. Rev. 2018, 19, 1205–1235. [Google Scholar] [CrossRef]
- Yuksel, H.S.; Şahin, F.N.; Maksimovic, N.; Drid, P.; Bianco, A. School-based intervention programs for preventing obesity and promoting physical activity and fitness: A systematic review. Int. J. Environ. Res. Public Health 2020, 17, 347. [Google Scholar] [CrossRef]
- Bray, I.; Slater, A.; Lewis-Smith, H.; Bird, E.; Sabey, A. Promoting positive body image and tackling overweight/obesity in children and adolescents: A combined health psychology and public health approach. Prev. Med. 2018, 116, 219–221. [Google Scholar] [CrossRef]
- Raimann, T. Obesidad y sus complicaciones. Rev. Médica Clínica Las Condes 2011, 22, 20–26. [Google Scholar] [CrossRef][Green Version]
- Han, J.C.; Lawlor, D.A.; Kimm, S.Y.S. Childhood obesity. Lancet 2010, 375, 1737–1748. [Google Scholar] [CrossRef]
- Stricker, P.R.; Faigenbaum, A.D.; McCambridge, T.M. Resistance training for children and adolescents. Pediatrics 2020, 145, e20201011. [Google Scholar] [CrossRef]
- Ramsay, J.A.; Blimkie, C.; Smith, K.; Garner, S.; Macdougall, D.; Sale, D. Strength training effects in prepubescent boys. Med. Sci. Sports Exerc. 1990, 22, 25–27. [Google Scholar] [CrossRef] [PubMed]
- Faigenbaum, A.D.; McFarland, J.E. Resistance training for kids: Right from the Start. ACSM’s Health Fit. J. 2016, 20, 16–22. [Google Scholar] [CrossRef]
- Pitton, P.M. Prepubescent strength training: The effects of resistance training on strength gains in prepubescent children. Natl. Strength Cond. Assoc. J. 1992, 14, 55–57. [Google Scholar] [CrossRef]
- Gregory, H.; Travis, T. Essentials of Strength Training and Conditioning, 4th ed.; Human Kinetics: Champaign, IL, USA, 2015; Available online: https://cutt.ly/XF704KY (accessed on 1 February 2022).
- Collins, H.; Booth, J.N.; Duncan, A.; Fawkner, S. The effect of resistance training interventions on fundamental movement skills in youth: A meta-analysis. Sport Med. Open 2018, 5, 17. [Google Scholar] [CrossRef]
- Schranz, N.; Tomkinson, G.; Olds, T. What is the effect of resistance training on the strength, body composition and psychosocial status of overweight and obese children and adolescents? A systematic review and meta-analysis. Sport Med. 2013, 43, 893–907. [Google Scholar] [CrossRef]
- Lloyd, R.S.; Faigenbaum, A.D.; Myer, G.D.; Stone, M.; Oliver, J.; Jeffreys, I.; Pierce, K. UKSCA Position Statement: Youth Resistance Training. Prof. Strength Cond. 2012, 26, 26–39. [Google Scholar]
- Icheli, L.; Itka, M.; Owland, T. Youth Resistance Training: Updated Position Statement Paper from the National Strength and Conditioning Association. J. Strength Cond. Res. 2009, 23, 60–79. [Google Scholar] [CrossRef]
- Vechetti, I.J.; Peck, B.D.; Wen, Y.; Walton, R.G.; Valentino, T.R.; Alimov, A.P.; Dungan, C.M.; Van Pelt, D.W.; von Walden, F.; Alkner, B.; et al. Mechanical overload-induced muscle-derived extracellular vesicles promote adipose tissue lipolysis. FASEB J. 2021, 35, e21644. [Google Scholar] [CrossRef]
- National Collaborating Centre for Methods and Tools. Quality assessment tool for quantitative studies. Worldviews Evid. Based Nurs. 2004, 1, 176–184. [Google Scholar]
- Seo, Y.-G.; Lim, H.; Kim, Y.; Ju, Y.-S.; Choi, Y.-J.; Lee, H.-J.; Jang, H.B.; Park, S.I.; Park, K.H. Effects of circuit training or a nutritional intervention on body mass index and other cardiometabolic outcomes in children and adolescents with overweight or obesity. PLoS ONE 2021, 16, e0245875. [Google Scholar] [CrossRef]
- Miguet, M.; Fearnbach, N.S.; Metz, L.; Khammassi, M.; Julian, V.; Cardenoux, C.; Pereira, B.; Boirie, Y.; Duclos, M.; Thivel, D. Effect of HIIT versus MICT on body composition and energy intake in dietary restrained and unrestrained adolescents with obesity. Appl. Physiol. Nutr. Metab. 2020, 45, 437–445. [Google Scholar] [CrossRef] [PubMed]
- Horsak, B.; Schwab, C.; Baca, A.; Greber-Platzer, S.; Kreissl, A.; Nehrer, S.; Keilani, M.; Crevenna, R.; Kranzl, A.; Wondrasch, B. Effects of a lower extremity exercise program on gait biomechanics and clinical outcomes in children and adolescents with obesity: A randomized controlled trial. Gait Posture 2019, 70, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Branco, B.H.M.; Carvalho, I.Z.; de Oliveira, H.G.; Fanhani, A.P.; Dos Santos, M.C.M.; de Oliveira, L.P.; Nelson Nardo, J. Effects of 2 types of resistance training models on obese adolescents’ body composition, cardiometabolic risk, and physical fitness. J. Strength Cond. Res. 2020, 34, 2672–2682. [Google Scholar] [CrossRef]
- Bharath, L.P.; Choi, W.W.; Cho, J.-M.; Skobodzinski, A.A.; Wong, A.; Sweeney, T.E.; Park, S.-Y. Combined resistance and aerobic exercise training reduces insulin resistance and central adiposity in adolescent girls who are obese: Randomized clinical trial. Eur. J. Appl. Physiol. 2018, 118, 1653–1660. [Google Scholar] [CrossRef]
- Bruñó, A.; Escobar, P.; Cebolla, A.; Álvarez-Pitti, J.; Guixeres, J.; Lurbe, E.; Baños, R.; Lisón, J.F. Home-Exercise Childhood Obesity Intervention: A Randomized Clinical Trial Comparing Print Versus Web-Based (Move It) Platforms. J. Pediatr. Nurs. 2018, 42, e79–e84. [Google Scholar] [CrossRef]
- Fiorilli, G.; Iuliano, E.; Aquino, G.; Campanella, E.; Tsopani, D.; Di Costanzo, A.; Calcagno, G.; di Cagno, A. Different consecutive training protocols to design an intervention program for overweight youth: A controlled study. Diabetes Metab. Syndr. Obes. Targets Ther. 2017, 10, 37–45. [Google Scholar] [CrossRef]
- Rey, O.; Vallier, J.M.; Nicol, C.; Mercier, C.S.; Maïano, C. Effects of combined vigorous interval training program and diet on body composition, physical fitness, and physical self-perceptions among obese adolescent boys and girls. Pediatric Exerc. Sci. 2017, 29, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Crouter, S.E.; Salas, C.; Wiecha, J. Effects of an afterschool community center physical activity program on fitness and body composition in obese youth. J. Sports Sci. 2017, 35, 1034–1040. [Google Scholar] [CrossRef]
- Dias, I.; Farinatti, P.; De Souza, M.G.; Manhanini, D.P.; Balthazar, E.; Dantas, D.L.; de Andrade Pinto, E.H.; Bouskela, E.; Kraemer-Aguiar, L.G. Effects of Resistance Training on Obese Adolescents. Med. Sci. Sports Exerc. 2015, 47, 2636–2644. [Google Scholar] [CrossRef]
- Kelly, L.A.; Loza, A.; Lin, X.; Schroeder, E.T.; Hughes, A.; Kirk, A.; Knowles, A.-M. The effect of a home-based strength training program on type 2 diabetes risk in obese Latino boys. J. Pediatr. Endocrinol. Metab. 2015, 28, 315–322. [Google Scholar] [CrossRef]
- Monteiro, P.A.; Chen, K.Y.; Lira, F.S.; Saraiva, B.T.C.; Antunes, B.M.; Campos, E.Z.; Freitas, I.F., Jr. Concurrent and aerobic exercise training promote similar benefits in body composition and metabolic profiles in obese adolescents. Lipids Health Dis. 2015, 14, 153. [Google Scholar] [CrossRef] [PubMed]
- Antunes, B.; Christofaro, D.; Monteiro, P.; Silveira, L.S.; Fernandes, R.A.; Mota, J.; Júnior, I.F.F. Effect of concurrent training on gender-specific biochemical variables and adiposity in obese adolescents. Arch. Endocrinol. Metab. 2015, 59, 303–309. [Google Scholar] [CrossRef] [PubMed]
- Inoue, D.S.; De Mello, M.T.; Foschini, D.; Lira, F.S.; Ganen, A.D.P.; Campos, R.M.D.S.; Sanches, P.D.L.; Silva, P.L.; Corgosinho, F.C.; Rossi, F.E.; et al. Linear and undulating periodized strength plus aerobic training promote similar benefits and lead to improvement of insulin resistance on obese adolescents. J. Diabetes Complicat. 2015, 29, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Dâmaso, A.R.; Da Silveira, R.M.; Caranti, D.A.; De Piano, A.; Fisberg, M.; Foschini, D.; Sanches, P.D.L.; Tock, L.; Lederman, H.M.; Tufik, S.; et al. Aerobic plus resistance training was more effective in improving the visceral adiposity, metabolic profile and inflammatory markers than aerobic training in obese adolescents. J. Sports Sci. 2014, 32, 1435–1445. [Google Scholar] [CrossRef]
- Ackel-D’Elia, C.; Carnier, J.; Bueno, C.R.; Campos, R.S.; Sanches, P.L.; Clemente, A.G.; Tufik, S.; de Mello, M.T.; Dâmaso, A.R. Effects of different physical exercises on leptin concentration in obese adolescents. Int. J. Sports Med. 2014, 35, 164–171. [Google Scholar] [CrossRef][Green Version]
- Sigal, R.J.; Alberga, A.S.; Goldfield, G.S.; Prud’Homme, D.; Hadjiyannakis, S.; Gougeon, R.; Phillips, P.; Tulloch, H.; Malcolm, J.; Doucette, S.; et al. Effects of aerobic training, resistance training, or both on percentage body fat and cardiometabolic risk markers in obese adolescents: The healthy eating aerobic and resistance training in youth randomized clinical trial. JAMA Pediatr. 2014, 168, 1006–1014. [Google Scholar] [CrossRef]
- Vásquez, F.; Díaz, E.; Lera, L.; Meza, J.; Salas, I.; Rojas Moncada, P.; Atalah Samur, E.; Burrows, R. Efecto residual del ejercicio de fuerza muscular en la prevención secundaria de la obesidad infantil. Nutr. Hosp. 2013, 28, 333–339. [Google Scholar] [CrossRef]
- Alberga, A.S.; Farnesi, B.C.; Lafleche, A.; Legault, L.; Komorowski, J. The effects of resistance exercise training on body composition and strength in obese prepubertal children. Physician Sportsmed. 2013, 41, 103–109. [Google Scholar] [CrossRef]
- Antunes, B.d.M.; Monteiro, P.A.; Silveira, L.S.; Cayres, S.U.; da Silva, C.B.; Junior, I.F.F. Effect of concurrent training on risk factors and hepatic steatosis in obese adolescents. Rev. Paul. Pediatr. 2013, 31, 371–376. [Google Scholar] [CrossRef]
- De Piano, A.; De Mello, M.T.; Sanches, P.D.L.; da Silva, P.L.; Campos, R.M.; Carnier, J.; Corgosinho, F.; Foschini, D.; Masquio, D.L.; Tock, L.; et al. Long-term effects of aerobic plus resistance training on the adipokines and neuropeptides in nonalcoholic fatty liver disease obese adolescents. Eur. J. Gastroenterol. Hepatol. 2012, 24, 1313–1324. [Google Scholar] [CrossRef]
- Foschini, D.; Arajo, R.C.; Bacurau, R.; De Piano, A.; De Almeida, S.S.; Carnier, J.; Rosa, T.D.; De Mello, M.T.; Tufik, S.; Dâmaso, A.R. Treatment of obese adolescents: The influence of periodization models and ACE genotype. Obesity 2010, 18, 766–772. [Google Scholar] [CrossRef] [PubMed]
- McGuigan, M.R.; Tatasciore, M.; Newton, R.U.; Pettigrew, S. Eight weeks of resistance training can significantly alter body composition in children who are overweight or obese. J. Strength Cond. Res. 2009, 23, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Davis, J.N.; Kelly, L.A.; Lane, C.J.; Ventura, E.E.; Byrd-Williams, C.E.; Alexandar, K.A.; Azen, S.P.; Chou, C.-P.; Spruijt-Metz, D.; Weigensberg, M.J.; et al. Randomized control trial to improve adiposity and insulin resistance in overweight Latino adolescents. Obesity 2009, 17, 1542–1548. [Google Scholar] [CrossRef] [PubMed]
- Sgro, M.; McGuigan, M.R.; Pettigrew, S.; Newton, R.U. The effect of duration of resistance training interventions in children who are overweight or obese. J. Strength Cond. Res. 2009, 23, 1263–1270. [Google Scholar] [CrossRef]
- Benson, A.C.; Torode, M.E.; Singh, M.A. The effect of high-intensity progressive resistance training on adiposity in children: A randomized controlled trial. Int. J. Obes. 2008, 32, 1016–1027. [Google Scholar] [CrossRef]
- Shaibi, G.Q.; Cruz, M.L.; Ball, G.D.C.; Weigensberg, M.J.; Salem, G.J.; Crespo, N.C.; Goran, M.I. Effects of resistance training on insulin sensitivity in overweight Latino adolescent males. Med. Sci. Sports Exerc. 2006, 38, 1208–1215. [Google Scholar] [CrossRef]
- Yu, C.C.; Sung, R.Y.; Hau, K.T.; Lam, P.K.; Nelson, E.A.; So, R.C. The effect of diet and strength training on obese children’s physical self-concept. J Sports Med Phys Fitness. 2008, 48, 76–82. [Google Scholar]
- Alberga, A.S.; Sigal, R.J.; Kenny, G.P. A review of resistance exercise training in obese adolescents. Physician Sportsmed. 2011, 39, 50–63. [Google Scholar] [CrossRef]
- Strasser, B.; Schobersberger, W. Evidence for resistance training as a treatment therapy in obesity. J. Obes. 2011, 2011, 482564. [Google Scholar] [CrossRef]
- Elly, C.; Urnett, N.; Ewton, M. Effects of strength training on body composition and bone mineral content in children who are obese. Strength Cond. 2005, 25, 396–403. [Google Scholar]
- Valentino, T.; Mobley, C.B.; McCarthy, J.J. The role of extracellular vesicles in skeletal muscle and systematic adaptation to exercise. J. Physiol. 2021, 599, 845–861. [Google Scholar] [CrossRef]
- Gutin, B.; Barbeau, P.; Owens, S.; Lemmon, C.R.; Bauman, M.; Allison, J.; Kang, H.-S.; Litaker, M.S. Effects of exercise intensity on cardiovascular fitness, total body composition, and visceral adiposity of obese adolescents. Am. J. Clin. Nutr. 2002, 75, 818–826. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.J.; Eather, N.; Morgan, P.J.; Plotnikoff, R.C.; Faigenbaum, A.D.; Lubans, D.R. The health benefits of muscular fitness for children and adolescents: A systematic review and meta-analysis. Sports Med. 2014, 44, 1209–1223. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, R.S.; Faigenbaum, A.D.; Stone, M.H.; Oliver, J.L.; Jeffreys, I.; Moody, J.A.; Brewer, C.; Pierce, K.C.; McCambridge, T.M.; Howard, R.; et al. Position statement on youth resistance training: The 2014 International Consensus. Br. J. Sports Med. 2014, 48, 498–505. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).