Laparoscopic Assisted Percutaneous Anterior Gastropexy for the Management of Acute and Chronic Gastric Volvulus in Infants
Abstract
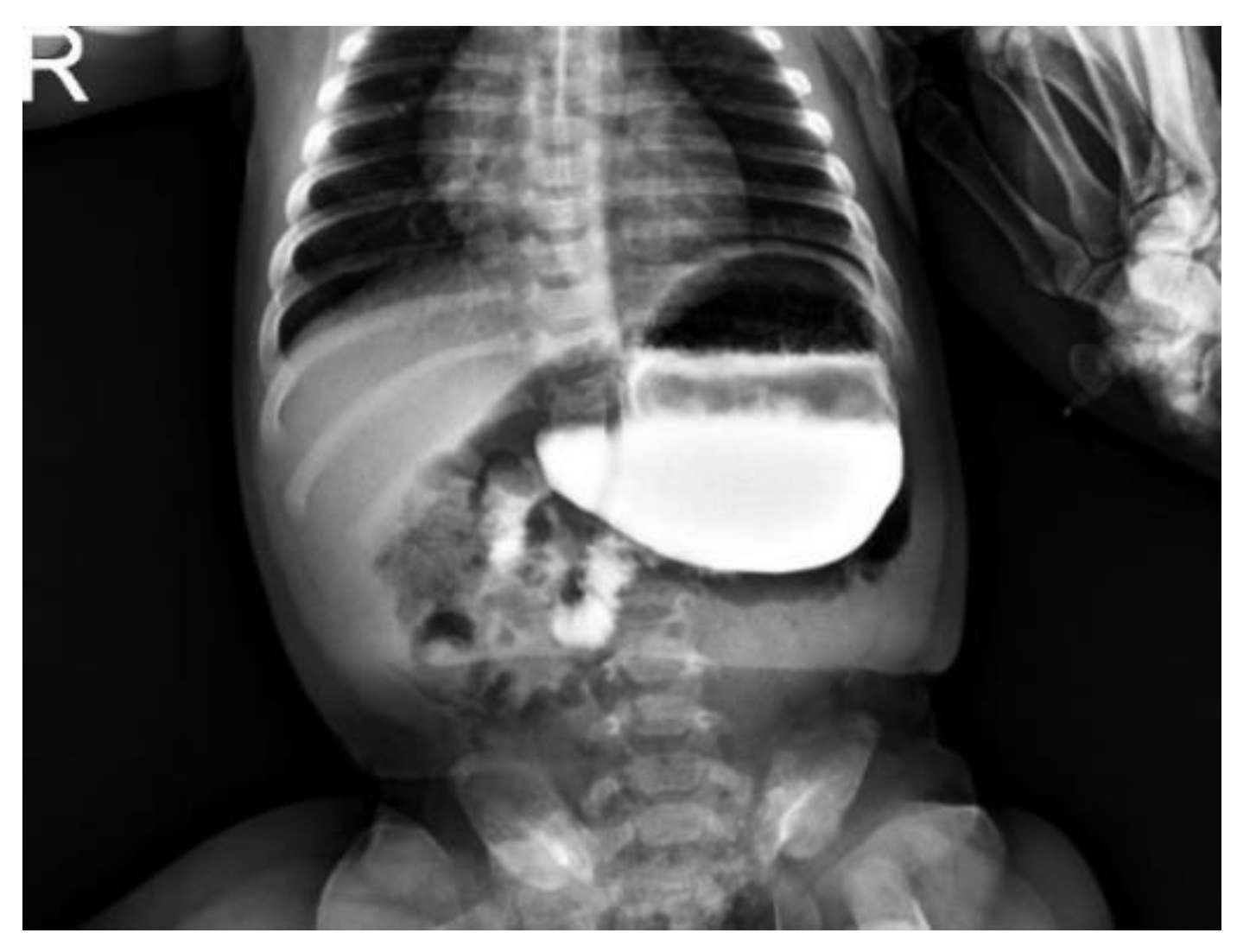
:1. Introduction
2. Material and Methods
3. Results
3.1. Demographics
3.2. Operative Technique
3.3. Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Berti, A. Singolare attorcigliamento dell’esofago col duodeno seguito da rapida morte. Gazz. Med. Ital. 1866, 9, 139–141. [Google Scholar]
- Al-Salem, A. Acute and Chronic Gastric Volvulus in infants and children: Who should be treated surgically? Pediatric Surg. Int. 2007, 23, 1095–1099. [Google Scholar] [CrossRef] [PubMed]
- Singal, A.K.; Patel, R.; Jain, S.; Gavhane, J.; Kadam, N.N. Laparoscopic management of neonatal Gastric Volvulus: A case report and Review of the literature. Eur. J. Pediatric Surg. 2009, 19, 191–193. [Google Scholar] [CrossRef] [PubMed]
- McElreath, D.P.; Olden, K.W.; Aduli, F. Hiccups: A subtle sign in the clinical diagnosis of Gastric Volvulus and a review of the Literature. Dig. Dis. Sci. 2008, 53, 3033–3036. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.; Yamoto, M.; Nomura, A.; Ooyama, K.; Sekioka, A.; Yamada, Y.; Fukumoto, K.; Urushihara, N. Single incision laparoscopic gastropexy for mesentero-axial gastric volvulus. Surg. Case Rep. 2019, 5, 19. [Google Scholar] [CrossRef] [PubMed]
- Cribbs, R.K.; Gow, K.W.; Wulkan, M.L. Gastric Volvulus in Infants and Children. Pediatrics 2008, 122, 752–762. [Google Scholar] [CrossRef] [PubMed]
- Patkowski, D.; Czernik, J.; Chrzan, R.; Jaworski, W.; Apoznański, W. Percutaneous Internal Ring suturing: A simple minimally Invasive technique for inguinal hernia repair in children. J. Laparoendosc. Adv. Surg. Tech. 2006, 16, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Borchardt, M. Zur pathologie and therapie des magen. Arch. Klein. Chir. 1904, 74, 243–260. [Google Scholar]
- Upadhyaya, V.D.; Gangopadhyay, A.N.; Pandey, A.; Kumar, V.; Sharma, S.P.; Gupta, D.K. Acute Gastric Volvulus in neonates—A diagnostic dilemma. Eur. J. Paediatr. Surg. 2008, 18, 188–191. [Google Scholar] [CrossRef] [PubMed]
- Da Costa, K.M.; Saxena, A. Management and outcomes of Gastric Volvulus in children: A systematic review. World J. Pediatrics 2019, 15, 226–234. [Google Scholar] [CrossRef] [PubMed]
- Darani, A.; Mendoza-Sagaon, M.; Reinberg, O. Gastric Volvulus in Children. J. Pediatric Surg. 2005, 40, 855–858. [Google Scholar] [CrossRef] [PubMed]
- Trecoci, I.; Morabito, G.; Romano, C.; Salamone, I. Gastric Volvulus in children—A diagnostic problem: Two case reports. J. Med. Case Rep. 2016, 10, 138. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Patkowski, D.; Chrzan, R.; Jaworski, W.; Apoznański, W.; Czernik, J. Percutaneous internal ring suturing for inguinal hernia repair in children under three months of age. Adv. Clin. Exp. Med. 2006, 15, 851–856. [Google Scholar]
- Wolak, P.K.; Patkowski, D. Laparoscopic inguinal hernia repair in children using the percutaneous internal ringsuturing technique—Own experience. Videosurgery Other Miniinvasive Tech. 2014, 9, 53–58. [Google Scholar] [CrossRef] [PubMed]





| Gender | Gestational Age | Age at Surgery (Days) | Weight at Surgery | Presenting Symptoms | Type of Volvulus |
|---|---|---|---|---|---|
| F | 38 + 5 | 102 | 5650 | Vomiting and retching | Organo-axial |
| F | 39 + 0 | 122 | 4840 | Vomiting and retching | Organo-axial |
| F | 38 + 5 | 57 | 4600 | Abdominal distension | Organo-axial |
| M | 39 + 1 | 36 | 3220 | Vomiting and retching | Organo-axial |
| F | 39 + 2 | 6 | 3680 | Vomiting and retching | Organo-axial |
| M | 38 + 2 | 57 | 5280 | Vomiting and retching | Organo-axial |
| M | 38 + 0 | 78 | 6000 | Vomiting and retching | Organo-axial |
| M | 39 + 0 | 43 | 3890 | Vomiting and retching | Organo-axial |
| F | N/A | N/A | N/A | N/A | Organo-axial |
| M | 40 + 4 | 69 | 4980 | Feeding difficulties/failure to thrive | Organo-axial |
| F | N/A | N/A | N/A | N/A | Organo-axial |
| M | N/A | N/A | N/A | N/A | Organo-axial |
| F | N/A | 180 | N/A | N/A | Organo-axial |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iacona, R.V.; Grasso, F.; Grimaldi, S.A.; Lebet, M.; Cacciaguerra, S. Laparoscopic Assisted Percutaneous Anterior Gastropexy for the Management of Acute and Chronic Gastric Volvulus in Infants. Children 2022, 9, 1275. https://doi.org/10.3390/children9091275
Iacona RV, Grasso F, Grimaldi SA, Lebet M, Cacciaguerra S. Laparoscopic Assisted Percutaneous Anterior Gastropexy for the Management of Acute and Chronic Gastric Volvulus in Infants. Children. 2022; 9(9):1275. https://doi.org/10.3390/children9091275
Chicago/Turabian StyleIacona, Roberta Valentina, Francesco Grasso, Silvia Antonia Grimaldi, Massimo Lebet, and Sebastiano Cacciaguerra. 2022. "Laparoscopic Assisted Percutaneous Anterior Gastropexy for the Management of Acute and Chronic Gastric Volvulus in Infants" Children 9, no. 9: 1275. https://doi.org/10.3390/children9091275
APA StyleIacona, R. V., Grasso, F., Grimaldi, S. A., Lebet, M., & Cacciaguerra, S. (2022). Laparoscopic Assisted Percutaneous Anterior Gastropexy for the Management of Acute and Chronic Gastric Volvulus in Infants. Children, 9(9), 1275. https://doi.org/10.3390/children9091275






