Optimization of Obstructive Sleep Apnea Management: Novel Decision Support via Unsupervised Machine Learning
Abstract
1. Introduction
2. Literature Review
2.1. OR, PCA, and MCDA in Healthcare
2.2. Novelty and Contributions of the Study
- To develop an objective weighting method within CROWM to extract the relative importance of evaluation criteria for CPAPs.
- To introduce the PCA technique in CROWM for ranking purposes in MCDA problems, enhancing accuracy and objectivity in medical device selection.
- To provide information and enable efficacy comparisons among different CPAP models, assisting healthcare professionals in choosing the most suitable device.
- To construct a support system to evaluate CPAP device performance, considering multiple criteria aligning with clinical guidelines and patient expectations.
3. Methodology
Case Study: Evaluation of CPAP Models
4. The CROWM Method
4.1. Weights of Criteria
4.1.1. The MEREC Method
- Establishment of the decision matrix, expressing the score of each alternative about each criterion analyzed;
- Determination of the normalized decision matrix. The elements of the normalized matrix are denoted by . Below, the first line denotes the set of beneficial criteria, and the second line represents the set of non-beneficial criteria;
- Determination of the overall performance of alternatives []:
- Performance of alternatives by removing each criterion []:
- Calculation of the removal effect of each criterion, through the result of the difference of the modulus sum between the Equations (2) and (3) []:
- Calculation of the weight of the criteria []:
4.1.2. Weight by Factor Loadings
- Calculation of the importance of jth criterion by factor loadings []:
- Calculating weights by factor loadings []:
4.1.3. Calculation of Criteria Weights
4.2. Evaluation of Alternatives
- 1.
- Establishment of a database containing a total of n CPAPs and k evaluation criteria (or variables);
- 2.
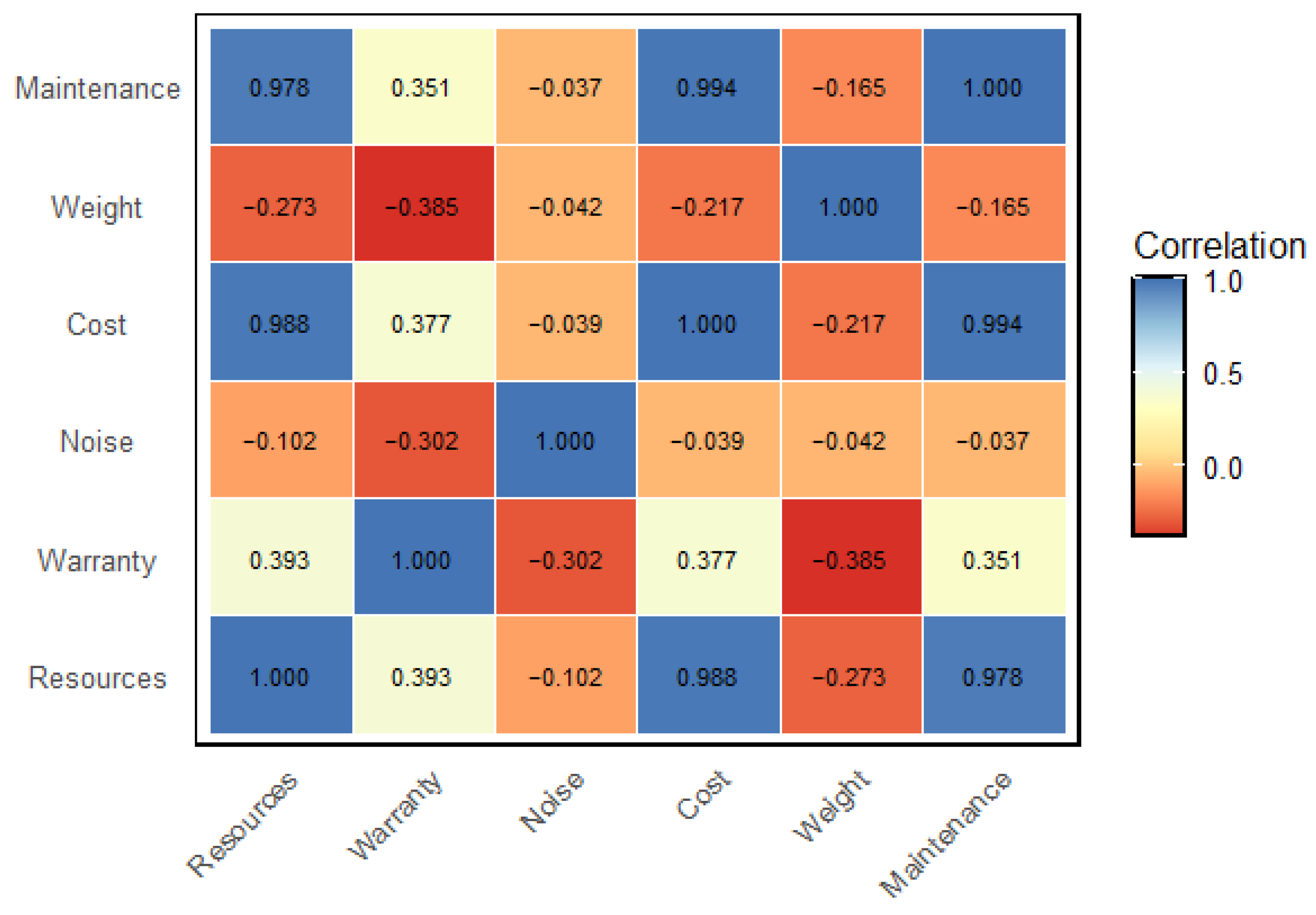
- Determination of the correlation matrix :
- 3.
- Elaboration of the Bartlett sphericity test:
- 4.
- Determination of eigenvalues and their respective shared variances:
- 5.
- Determination of eigenvectors:
- 6.
- Determination of factor scores:
- 7.
- Determination of factors:
- 8.
- Determination of factor loadings and communalities:
- 9.
- Performance evaluation:
4.3. Hypothesis and Limitations
5. Results and Analysis
- Resources: scale from 1 to 7, which represents the number of resources available for each CPAP;
- Warranty (months): warranty period offered for each CPAP, expressed in months;
- Noise (decibels—db): the level of noise produced by CPAP, measured in decibels;
- Cost (real): the monetary cost associated with each CPAP, expressed in real (approximately 5 BRL is equivalent to 1 USD);
- Weight (g): CPAP weight, measured in grams;
- Maintenance: rating from 1 to 7, representing each CPAP’s ease of maintenance.
5.1. Determination of Criteria Weights by CROWM
5.2. Performance Evaluation by CROWM
5.3. Advantages and Disadvantages of the CROWM Method
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Benjafield, A.V.; Ayas, N.T.; Eastwood, P.R.; Heinzer, R.; Ip, M.S.M.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pépin, J.-L. Estimation of the Global Prevalence and Burden of Obstructive Sleep Apnoea: A Literature-Based Analysis. Lancet Respir. Med. 2019, 7, 687–698. [Google Scholar] [CrossRef] [PubMed]
- Yasir, M.; Pervaiz, A.; Sankari, A. Cardiovascular Outcomes in Sleep-Disordered Breathing: Are We under-Estimating? Front. Neurol. 2022, 13, 801167. [Google Scholar] [CrossRef] [PubMed]
- McEvoy, R.D.; Antic, N.A.; Heeley, E.; Luo, Y.; Ou, Q.; Zhang, X.; Mediano, O.; Chen, R.; Drager, L.F.; Liu, Z. CPAP for Prevention of Cardiovascular Events in Obstructive Sleep Apnea. N. Engl. J. Med. 2016, 375, 919–931. [Google Scholar] [CrossRef] [PubMed]
- Franklin, K.A.; Lindberg, E. Obstructive Sleep Apnea Is a Common Disorder in the Population—A Review on the Epidemiology of Sleep Apnea. J. Thorac. Dis. 2015, 7, 1311. [Google Scholar] [PubMed]
- Oliver, C.; Li, H.; Biswas, B.; Woodstoke, D.; Blackman, J.; Butters, A.; Drew, C.; Gabb, V.; Harding, S.; Hoyos, C.M. A Systematic Review on Adherence to Continuous Positive Airway Pressure (CPAP) Treatment for Obstructive Sleep Apnoea (OSA) in Individuals with Mild Cognitive Impairment and Alzheimer’s Disease Dementia. Sleep Med. Rev. 2023, 73, 101869. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, M.; da Costa Martha, L.; dos Reis, M.F. Utilização Do Algoritmo Branch and Bound Na Otimização Da Produção de Uma Indústria de Produtos Plásticos. Rev. Trab. Acadêmicos Lusófona 2019, 2, 217–237. [Google Scholar]
- Marsh, K.; IJzerman, M.; Thokala, P.; Baltussen, R.; Boysen, M.; Kaló, Z.; Lönngren, T.; Mussen, F.; Peacock, S.; Watkins, J. Multiple Criteria Decision Analysis for Health Care Decision Making—Emerging Good Practices: Report 2 of the ISPOR MCDA Emerging Good Practices Task Force. Value Health 2016, 19, 125–137. [Google Scholar] [CrossRef] [PubMed]
- Keshavarz-Ghorabaee, M.; Amiri, M.; Zavadskas, E.K.; Turskis, Z.; Antucheviciene, J. Determination of Objective Weights Using a New Method Based on the Removal Effects of Criteria (MEREC). Symmetry 2021, 13, 525. [Google Scholar] [CrossRef]
- Lee, J.; Kang, S.-H.; Rosenberger, J.; Kim, S.B. A Hybrid Approach of Goal Programming for Weapon Systems Selection. Comput. Ind. Eng. 2010, 58, 521–527. [Google Scholar] [CrossRef]
- Moreira, M.Â.L.; Gomes, C.F.S.; Santos, M.; Silva Júnior, A.C.; Costa, I.P. de A. Sensitivity Analysis by the PROMETHEE-GAIA Method: Algorithms Evaluation for COVID-19 Prediction. Procedia Comput. Sci. 2022, 199, 431–438. [Google Scholar] [CrossRef]
- Delesie, L. Bridging the Gap between Clinicians and Health Managers. Eur. J. Oper. Res. 1998, 105, 248–256. [Google Scholar] [CrossRef]
- Dexter, F.; Epstein, R.H.; Marcon, E.; De Matta, R. Strategies to Reduce Delays in Admission into a Postanesthesia Care Unit from Operating Rooms. J. PeriAnesthesia Nurs. 2005, 20, 92–102. [Google Scholar] [CrossRef]
- Guerriero, F.; Guido, R. Operational Research in the Management of the Operating Theatre: A Survey. Health Care Manag. Sci. 2011, 14, 89–114. [Google Scholar] [CrossRef] [PubMed]
- Rais, A.; Viana, A. Operations Research in Healthcare: A Survey. Int. Trans. Oper. Res. 2011, 18, 1–31. [Google Scholar] [CrossRef]
- Tippong, D.; Petrovic, S.; Akbari, V. A Review of Applications of Operational Research in Healthcare Coordination in Disaster Management. Eur. J. Oper. Res. 2022, 301, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Lamé, G.; Crowe, S.; Komashie, A.; Royston, G. Joining Forces: The Value of Design Partnering with Operational Research to Improve Healthcare Delivery. Des. Sci. 2023, 9, e4. [Google Scholar] [CrossRef]
- Walsh, M.; Kittler, M.G.; Mahal, D. Towards a New Paradigm of Healthcare: Addressing Challenges to Professional Identities through Community Operational Research. Eur. J. Oper. Res. 2018, 268, 1125–1133. [Google Scholar] [CrossRef]
- Le, H.-A.; Hoang, X.-T.; Trieu, Q.-H.; Pham, D.-L.; Le, X.-H. Determining the Best Dressing Parameters for External Cylindrical Grinding Using MABAC Method. Appl. Sci. 2022, 12, 8287. [Google Scholar] [CrossRef]
- Dos Santos, M.; Quintal, R.S.; da Paixão, A.C.; Gomes, C.F.S. Simulation of Operation of an Integrated Information for Emergency Pre-Hospital Care in Rio de Janeiro Municipality. Procedia Comput. Sci. 2015, 55, 931–938. [Google Scholar] [CrossRef]
- Ploskas, N.; Papathanasiou, J. A Decision Support System for Multiple Criteria Alternative Ranking Using TOPSIS and VIKOR in Fuzzy and Nonfuzzy Environments. Fuzzy Sets Syst. 2019, 377, 1–30. [Google Scholar] [CrossRef]
- Zhang, J.; Kou, G.; Peng, Y.; Zhang, Y. Estimating Priorities from Relative Deviations in Pairwise Comparison Matrices. Inf. Sci. 2021, 552, 310–327. [Google Scholar] [CrossRef]
- Favero, L.; Belfiore, P. Data Science for Business and Decision Making; Academic Press: Cambridge, MA, USA, 2019; ISBN 0128112174. [Google Scholar]
- Belton, V.; Stewart, T. Multiple Criteria Decision Analysis: An Integrated Approach; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2002; ISBN 079237505X. [Google Scholar]
- Stević, Ž.; Pamučar, D.; Puška, A.; Chatterjee, P. Sustainable Supplier Selection in Healthcare Industries Using a New MCDM Method: Measurement of Alternatives and Ranking According to COmpromise Solution (MARCOS). Comput. Ind. Eng. 2020, 140, 106231. [Google Scholar] [CrossRef]
- Büyüközkan, G.; Çifçi, G. A Combined Fuzzy AHP and Fuzzy TOPSIS Based Strategic Analysis of Electronic Service Quality in Healthcare Industry. Expert Syst. Appl. 2012, 39, 2341–2354. [Google Scholar] [CrossRef]
- Grigoroudis, E.; Orfanoudaki, E.; Zopounidis, C. Strategic Performance Measurement in a Healthcare Organisation: A Multiple Criteria Approach Based on Balanced Scorecard. Omega 2012, 40, 104–119. [Google Scholar] [CrossRef]
- Abdel-Basset, M.; Manogaran, G.; Gamal, A.; Smarandache, F. A Group Decision Making Framework Based on Neutrosophic TOPSIS Approach for Smart Medical Device Selection. J. Med. Syst. 2019, 43, 38. [Google Scholar] [CrossRef] [PubMed]
- Nagurney, A.; Masoumi, A.H.; Yu, M. Supply Chain Network Operations Management of a Blood Banking System with Cost and Risk Minimization. Comput. Manag. Sci. 2012, 9, 205–231. [Google Scholar] [CrossRef]
- Wang, H.; Luo, P.; Wu, Y. Research on the Location Decision-Making Method of Emergency Medical Facilities Based on WSR. Sci. Rep. 2023, 13, 18011. [Google Scholar] [CrossRef] [PubMed]
- Beheshtinia, M.A.; Bahrami, F.; Fathi, M.; Asadi, S. Evaluating and Prioritizing the Healthcare Waste Disposal Center Locations Using a Hybrid Multi-Criteria Decision-Making Method. Sci. Rep. 2023, 13, 15130. [Google Scholar] [CrossRef] [PubMed]
- KhanMohammadi, E.; Talaie, H.; Azizi, M. A Healthcare Service Quality Assessment Model Using a Fuzzy Best–Worst Method with Application to Hospitals with in-Patient Services. Healthc. Anal. 2023, 4, 100241. [Google Scholar] [CrossRef]
- Eriş, M.B.; Sezer, E.D.G.; Ocak, Z. Prioritization of the Factors Affecting the Performance of Clinical Laboratories Using the AHP and ANP Techniques. Netw. Model. Anal. Health Inform. Bioinform. 2022, 12, 5. [Google Scholar] [CrossRef]
- Costa, I.P.A.; Maêda, S.M.D.N.; Teixeira, L.F.H.S.B.; Gomes, C.F.S.; Santos, M.D. Choosing a Hospital Assistance Ship to Fight the Covid-19 Pandemic. Rev. Saude Publica 2020, 54, 79. [Google Scholar] [CrossRef] [PubMed]
- Li, X.D.; Tai, J.; Xu, Z.F.; Peng, X.X.; Feng, G.S.; Zhang, Y.M.; Zhang, J.; Guo, Y.L.; Wu, Y.X.; Shi, J.; et al. The Validity and Reliability of Simplified Chinese Version of the Pediatric Sleep Questionnaire for Screening Children with Obstructive Sleep Apnea Syndrome in Beijing. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi = Chin. J. Otorhinolaryngol. Head Neck Surg. 2016, 51, 812–818. [Google Scholar]
- Chen, M.; Shi, F.; Wu, H.; Cheng, L.; He, P.; Jin, Q.; Huang, J. Impact of Obstructive Sleep Apnea on Health-Related Quality of Life in Patients with Partial Laryngectomy for Laryngeal Cancer. Ear Nose Throat J. 2022, 01455613231178955. [Google Scholar] [CrossRef]
- Celik, Y.; Yapici-Eser, H.; Balcan, B.; Peker, Y. Association of Excessive Daytime Sleepiness with the Zung Self-Rated Depression Subscales in Adults with Coronary Artery Disease and Obstructive Sleep Apnea. Diagnostics 2021, 11, 1176. [Google Scholar] [CrossRef] [PubMed]
- Dugger, Z.; Halverson, G.; McCrory, B.; Claudio, D. Principal Component Analysis in MCDM: An Exercise in Pilot Selection. Expert Syst. Appl. 2022, 188, 115984. [Google Scholar] [CrossRef]
- Guo, Z.; Zhang, Y. The Third-Party Logistics Performance Evaluation Based on the AHP-PCA Model. In Proceedings of the 2010 International Conference on E-Product E-Service and E-Entertainment, Henan, China, 7–9 November 2010; pp. 1–4. [Google Scholar]
- Creswell, J.W.; Creswell, J.D. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches; Sage Publications: London, UK, 2017; ISBN 1506386717. [Google Scholar]
- Bertrand, J.W.M.; Fransoo, J.C. Operations Management Research Methodologies Using Quantitative Modeling. Int. J. Oper. Prod. Manag. 2002, 22, 241–264. [Google Scholar] [CrossRef]
- Checkland, P.B.; Haynes, M.G. Varieties of Systems Thinking: The Case of Soft Systems Methodology. In Management Control Theory; Routledge: London, UK, 2019; pp. 151–160. [Google Scholar]
- SlideModel CATWOE Analysis Slide Template. Available online: https://slidemodel.com/free-powerpoint-templates/free-catwoe-analysis-slide-template-for-powerpoint/ (accessed on 6 March 2024).
- Ecer, F.; Pamucar, D. A Novel LOPCOW-DOBI Multi-criteria Sustainability Performance Assessment Methodology: An Application in Developing Country Banking Sector. Omega 2022, 112, 102690. [Google Scholar] [CrossRef]
- Zhang, H.; Yang, L.; Li, M. A Novel Comprehensive Model of Suitability Analysis for Matching Area in Underwater Geomagnetic Aided Inertial Navigation. Math. Probl. Eng. 2019, 2019, 9740812. [Google Scholar] [CrossRef]
- Mishra, R.; Mishra, O.N. A Hybrid PCA-AHP-Multi-Grade Fuzzy Approach to Assess Marketing-Based Flexibility. Mark. Intell. Plan. 2018, 36, 213–229. [Google Scholar] [CrossRef]
- Diaby, V.; Sanogo, V.; Moussa, K.R. ELICIT: An Alternative Imprecise Weight Elicitation Technique for Use in Multi-Criteria Decision Analysis for Healthcare. Expert Rev. Pharmacoeconomics Outcomes Res. 2016, 16, 141–147. [Google Scholar] [CrossRef][Green Version]
- Zhou, J.-L.; Xu, Q.-Q.; Zhang, X.-Y. Water Resources and Sustainability Assessment Based on Group AHP-PCA Method: A Case Study in the Jinsha River Basin. Water 2018, 10, 1880. [Google Scholar] [CrossRef]
- Liu, X.; Han, Y.; Qiu, H.; Zheng, Z. Threat Evaluation in Air Defense Based on Improved KPCA-TOPSIS. In Proceedings of the 2018 IEEE CSAA Guidance, Navigation and Control Conference, CGNCC 2018, Xiamen, China, 10–12 August 2018; Institute of Electrical and Electronics Engineers Inc.: New York, NY, USA; National University of Defense Technology, College of Mechatronics Engineering and Automation: Changsha, China, 2018. [Google Scholar]
- Lin, C.L.; Shih, Y.H.; Tzeng, G.H.; Yu, H.C. A Service Selection Model for Digital Music Service Platforms Using a Hybrid MCDM Approach. Appl. Soft Comput. 2016, 48, 385–403. [Google Scholar] [CrossRef]
- Abonyi, J.; Czvetkó, T.; Kosztyán, Z.T.; Héberger, K. Factor Analysis, Sparse PCA, and Sum of Ranking Differences-Based Improvements of the Promethee-GAIA Multicriteria Decision Support Technique. PLoS ONE 2022, 17, e0264277. [Google Scholar] [CrossRef] [PubMed]
- Roulet, C.-A.; Flourentzou, F.; Labben, H.H.; Santamouris, M.; Koronaki, I.; Dascalaki, E.; Richalet, V. ORME: A Multicriteria Rating Methodology for Buildings. Build. Environ. 2002, 37, 579–586. [Google Scholar] [CrossRef]
- Li, Q.; Lu, C.; Zhao, H. Risk Assessment of Floor Water Inrush Based on TOPSIS Combined Weighting Model: A Case Study in a Coal Mine, China. Earth Sci. Inform. 2023, 16, 565–578. [Google Scholar] [CrossRef]
- Hajiagha, S.H.R.; Mahdiraji, H.A.; Hashemi, S.S. Total Area Based on Orthogonal Vectors (TAOV) as a Novel Method of Multi-Criteria Decision Aid. Technol. Econ. Dev. Econ. 2018, 24, 1679–1694. [Google Scholar] [CrossRef]
- Xianjun, Z.; Fangxiong, X.; Ningling, M.; Di, D.; Xianzhong, Z.; Wenting, H. Effectiveness Evaluation of Humanware Service in Novel Decision System. In Proceedings of the 2020 IEEE International Conference on Networking, Sensing and Control, ICNSC 2020, Nanjing, China, 30 October–2 November 2020. [Google Scholar]
- Curran, M.; Lazzarini, G.; Baumgart, L.; Gabel, V.; Blockeel, J.; Epple, R.; Stolze, M.; Schader, C. Representative Farm-Based Sustainability Assessment of the Organic Sector in Switzerland Using the SMART-Farm Tool. Front. Sustain. Food Syst. 2020, 4, 554362. [Google Scholar] [CrossRef]
- Mittal, P. A Multi-Criterion Decision Analysis Based on PCA for Analyzing the Digital Technology Skills in the Effectiveness of Government Services. In Proceedings of the 2020 International Conference on Decision Aid Sciences and Application (DASA), Sakheer, Bahrain, 8–9 November 2020; pp. 490–494. [Google Scholar]
- Stankovic, J.J.; Jankovic-Milic, V.; Marjanovic, I.; Janjic, J. An Integrated Approach of PCA and PROMETHEE in Spatial Assessment of Circular Economy Indicators. Waste Manag. 2021, 128, 154–166. [Google Scholar] [CrossRef]
- Bartlett, M.S. A Note on the Multiplying Factors for Various χ2 Approximations. J. R. Stat. Society. Ser. B (Methodol.) 1954, 16, 296–298. [Google Scholar] [CrossRef]
- Ruscio, J.; Roche, B. Determining the Number of Factors to Retain in an Exploratory Factor Analysis Using Comparison Data of Known Factorial Structure. Psychol. Assess. 2012, 24, 282. [Google Scholar] [CrossRef]
- Fávero, L.P.; Belfiore, P. Manual de Análise de Dados: Estatística e Modelagem Multivariada Com Excel®, SPSS® e Stata®; Elsevier: São Paulo, Brasil, 2017; ISBN 8535285059. [Google Scholar]
- Yazdani, M.; Zarate, P.; Kazimieras Zavadskas, E.; Turskis, Z. A Combined Compromise Solution (CoCoSo) Method for Multi-Criteria Decision-Making Problems. Manag. Decis. 2019, 57, 2501–2519. [Google Scholar] [CrossRef]
- dos Santos, M.; Costa, I.P.d.A.; Gomes, C.F.S. Multicriteria Decision-Making in the Selection of Warships: A New Approach to the AHP Method. Int. J. Anal. Hierarchy Process 2021, 13, 147–169. [Google Scholar] [CrossRef]
- Spearman, C. The Proof and Measurement of Association between Two Things. In Studies in Individual Differences: The Search for Intelligence; Jenkins, J.J., Paterson, D.G., Eds.; Appleton-Century-Crofts: Norwalk, CA, USA, 1961; pp. 45–58. [Google Scholar]
- Mukaka, M.M. A Guide to Appropriate Use of Correlation Coefficient in Medical Research. Malawi Med. J. 2012, 24, 69–71. [Google Scholar]




| Method | Objective Weights | Techniques | Communality Assessment | Advantages and Disadvantages | PCA Tests | Non-Beneficial Criteria in PCA | Alternative Evaluation |
|---|---|---|---|---|---|---|---|
| CROWM | X | PCA and MEREC | X | Removes DM evaluation/Bias-free. | X | X | X |
| PCA-AHP [44] | PCA and AHP | Considers the evaluation of the DM/Enables bias in the process. | X | X | |||
| PCA-AHP-MFA [45] | PCA and AHP | Considers the evaluation of the DM/Enables bias in the process. | X | X | |||
| AHP-PCA-GP [9] | PCA, AHP, and Goal Programming (GP) | Considers the evaluation of the DM/Enables bias in the process. | X | ||||
| AHP-PCA [38] | PCA and AHP | Considers the evaluation of the DM/Enables bias in the process. | X | ||||
| ELICIT [46] | PCA and Monte Carlo | Considers the evaluation of the DM/Enables bias in the process. | |||||
| Group AHP-PCA [47] | PCA and AHP | Considers the evaluation of the DM/Enables bias in the process. | X | ||||
| KPCA-TOPSIS [48] | X | PCA and TOPSIS | Removes DM evaluation/Bias-free. | X | |||
| PCA—VIKOR, ANP, DEMATEL [49] | PCA and VIKOR | Considers the evaluation of the DM/Enables bias in the process. | X | X | |||
| P-SPCA, P-PFA and P-SRD [50] | X | PCA and PROMETHEE-GAIA | Removes DM evaluation/Bias-free. | X | X | ||
| ORME [51] | PCA, ELECTRE III, and IV | Considers the evaluation of the DM/Enables bias in the process. | X | ||||
| WIRI [52] | X | PCA, CRITIC and TOPSIS | Removes DM evaluation/Bias-free. | X | |||
| TAOV [53] | PCA | Considers the evaluation of the DM/Enables bias in the process. | X | ||||
| PCA-TOPSIS [54] | X | PCA and TOPSIS | Removes DM evaluation/Bias-free. | X | |||
| SMART-PCA [55] | PCA | Considers the evaluation of the DM/Enables bias in the process. | X | ||||
| AHP-PCA and Communalities [56] | PCA and AHP | Considers the evaluation of the DM/Enables bias in the process. | X | ||||
| PCA-PROMETHEE [57] | X | PCA and PROMETHEE | Removes DM evaluation/Bias-free. | X | X |
| CPAPs\Criterion | Resources | Warranty | Noise | Cost | Weight | Maintenance | |
|---|---|---|---|---|---|---|---|
| CP1 | S10 AutoSet | 5 | 24 | −26 | −5200 | −1248 | 5.3 |
| CP2 | AirSense 10 Elite | 3 | 24 | −26 | −3500 | −1248 | 3.6 |
| CP3 | CPAP XT-I | 3 | 12 | −30 | −3800 | −1800 | 4 |
| CP4 | AirMini AutoSet | 7 | 24 | −30 | −7000 | −300 | 7 |
| CP5 | SleepStyle | 6 | 24 | −28 | −6000 | −1700 | 6 |
| CP6 | VPAP Aircurve 10 VAauto | 6 | 24 | −28 | −6600 | −1300 | 6.4 |
| CP7 | SleepLive | 3 | 3 | −32 | −3673 | −1500 | 3.7 |
| CP8 | Dreamstation | 4 | 3 | −26 | −4123 | −1300 | 4 |
| CP9 | Ecostar | 2 | 24 | −29 | −2400 | −800 | 2 |
| Weights | |||
|---|---|---|---|
| Criteria | MEREC | Factor Loadings | CROWM |
| Resources | 0.168 | 0.196 | 0.182 |
| Warranty | 0.383 | 0.153 | 0.268 |
| Noise | 0.030 | 0.110 | 0.070 |
| Cost | 0.119 | 0.199 | 0.159 |
| Weight | 0.108 | 0.140 | 0.124 |
| Maintenance | 0.193 | 0.201 | 0.197 |
| PC1 | PC2 | PC3 | PC4 | PC5 | PC6 | |
|---|---|---|---|---|---|---|
| Eigenvalues | 3.281 | 1.208 | 1.020 | 0.475 | 0.013 | 0.004 |
| Shared variance | 0.547 | 0.201 | 0.17 | 0.079 | 0.002 | 0.001 |
| Cumulative shared variance | 54.70% | 74.80% | 91.80% | 99.70% | 99.90% | 100.00% |
| CPAPs | PC1 | PC2 | PC3 |
|---|---|---|---|
| CP1 | 0.479 | 0.776 | −0.724 |
| CP2 | −0.493 | 1.348 | −0.449 |
| CP3 | −0.800 | −0.919 | −0.333 |
| CP4 | 1.622 | −0.168 | 1.719 |
| CP5 | 0.776 | −0.365 | −0.987 |
| CP6 | 1.060 | −0.186 | −0.395 |
| CP7 | −1.008 | −1.690 | 0.671 |
| CP8 | −0.525 | −0.090 | −0.869 |
| CP9 | −1.113 | 1.294 | 1.368 |
| Factor Loadings | Communalities | |||||
|---|---|---|---|---|---|---|
| Criteria | PC1 | PC2 | PC3 | PC1 | PC2 | PC3 |
| Resources | 0.978 | −0.156 | −0.069 | 0.956 | 0.024 | 0.005 |
| Warranty | 0.558 | 0.646 | 0.109 | 0.311 | 0.417 | 0.012 |
| Noise | 0.143 | 0.690 | −0.643 | 0.020 | 0.476 | 0.413 |
| Cost | −0.970 | 0.223 | 0.075 | 0.942 | 0.050 | 0.006 |
| Weight | 0.370 | 0.419 | 0.756 | 0.137 | 0.175 | 0.572 |
| Maintenance | 0.957 | −0.256 | −0.114 | 0.915 | 0.065 | 0.013 |
| Ranking | CROWM | PCA | CoCoSo | Gaussian AHP | ||||
|---|---|---|---|---|---|---|---|---|
| 1º | CP4 | 1.134 | CP4 | 1.145 | CP4 | 2.722 | CP4 | 0.208 |
| 2º | CP6 | 0.564 | CP6 | 0.475 | CP1 | 2.704 | CP9 | 0.119 |
| 3º | CP1 | 0.362 | CP1 | 0.295 | CP6 | 2.679 | CP6 | 0.115 |
| 4º | CP5 | 0.294 | CP5 | 0.183 | CP5 | 2.61 | CP1 | 0.112 |
| 5º | CP2 | −0.087 | CP2 | −0.074 | CP2 | 2.51 | CP5 | 0.109 |
| 6º | CP9 | −0.278 | CP9 | −0.115 | CP9 | 2.009 | CP2 | 0.105 |
| 7º | CP8 | −0.428 | CP8 | −0.453 | CP8 | 1.837 | CP3 | 0.080 |
| 8º | CP3 | −0.696 | CP3 | −0.679 | CP3 | 1.778 | CP8 | 0.079 |
| 9º | CP7 | −0.863 | CP7 | −0.778 | CP7 | 1.316 | CP7 | 0.072 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Araújo Costa, A.P.; Terra, A.V.; de Souza Rocha Junior, C.; de Araújo Costa, I.P.; Moreira, M.Â.L.; dos Santos, M.; Gomes, C.F.S.; da Silva, A.S. Optimization of Obstructive Sleep Apnea Management: Novel Decision Support via Unsupervised Machine Learning. Informatics 2024, 11, 22. https://doi.org/10.3390/informatics11020022
de Araújo Costa AP, Terra AV, de Souza Rocha Junior C, de Araújo Costa IP, Moreira MÂL, dos Santos M, Gomes CFS, da Silva AS. Optimization of Obstructive Sleep Apnea Management: Novel Decision Support via Unsupervised Machine Learning. Informatics. 2024; 11(2):22. https://doi.org/10.3390/informatics11020022
Chicago/Turabian Stylede Araújo Costa, Arthur Pinheiro, Adilson Vilarinho Terra, Claudio de Souza Rocha Junior, Igor Pinheiro de Araújo Costa, Miguel Ângelo Lellis Moreira, Marcos dos Santos, Carlos Francisco Simões Gomes, and Antonio Sergio da Silva. 2024. "Optimization of Obstructive Sleep Apnea Management: Novel Decision Support via Unsupervised Machine Learning" Informatics 11, no. 2: 22. https://doi.org/10.3390/informatics11020022
APA Stylede Araújo Costa, A. P., Terra, A. V., de Souza Rocha Junior, C., de Araújo Costa, I. P., Moreira, M. Â. L., dos Santos, M., Gomes, C. F. S., & da Silva, A. S. (2024). Optimization of Obstructive Sleep Apnea Management: Novel Decision Support via Unsupervised Machine Learning. Informatics, 11(2), 22. https://doi.org/10.3390/informatics11020022












