Association between Time from Dinner to Bedtime and Sleep Quality Indices in the Young Japanese Population: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Study Procedure
2.3. Anthropometric Measurements
2.4. Dietary Assessment
2.5. Self-Reported Questionnaires
2.5.1. Pittsburgh Sleep Quality Index (PSQI)
2.5.2. Morningness–Eveningness Questionnaire (MEQ)
2.5.3. Chalder Fatigue Scale (CFS)
2.5.4. International Physical Activity Questionnaire (IPAQ)
2.6. Statistical Analysis
3. Results
| T1 (n = 88) | T2 (n = 88) | T3 (n = 88) | p Values | ||||
|---|---|---|---|---|---|---|---|
| Age, year | 21.4 | (20.9–21.9) | 21.8 | (21.2–22.4) | 21.1 | (20.7–21.5) | 0.320 |
| Women | 36 | (40.9) | 38 | (43.2) | 41 | (46.6) | 0.746 |
| Living status | |||||||
| Alone | 49 | (55.7) | 55 | (62.5) | 57 | (65.0) | 0.437 |
| Family | 39 | (44.3) | 33 | (37.5) | 31 | (35.2) | |
| Smoking habit | 1 | (1.1) | 4 | (4.5) | 3 | (3.4) | 0.406 |
| Drinking habit | 27 | (30.7) | 25 | (28.4) | 27 | (30.7) | 0.930 |
| Height, cm | 167.0 | (165.2–168.7) | 165.8 | (163.9–167.6) | 166.0 | (164.3–167.7) | 0.566 |
| Weight, kg | 60.9 | (58.7–63.1) | 58.4 | (56.2–60.6) | 60.1 | (58.0–62.2) | 0.261 |
| BMI | 21.8 | (21.3–22.4) | 21.1 | (20.6–21.6) | 21.7 | (21.2–22.3) | 0.137 |
| Breakfast frequency, times/week | 5.1 | (4.6–5.6) | 4.7 | (4.2–5.2) | 4.6 | (4.1–5.1) | 0.317 |
| Breakfast time, h:min | 8:50 | (8:29–9:10) | 8:38 | (8:22–8:55) | 8:47 | (8:30–9:03) | 0.656 |
| Lunch time, h:min | 12:59 | (12:43–13:16) | 12:54 | (12:43–13:06) | 12:39 | (12:29–12:49) | 0.039 |
| Dinner time, h:min | 21:37 | (21:18–21:55) | 20:14 | (20:01–20:26) | 19:12 | (19:00–19:24) | <0.001 |
| Bedtime, h:min | 0:18 | (0:03–0:33) | 0:32 | (0:21–0:44) | 1:07 | (0:55–1:20) | <0.001 |
| Wake time, h:min | 7:41 | (7:22–7:59) | 7:32 | (7:15–7:48) | 7:47 | (7:28–8:07) | 0.463 |
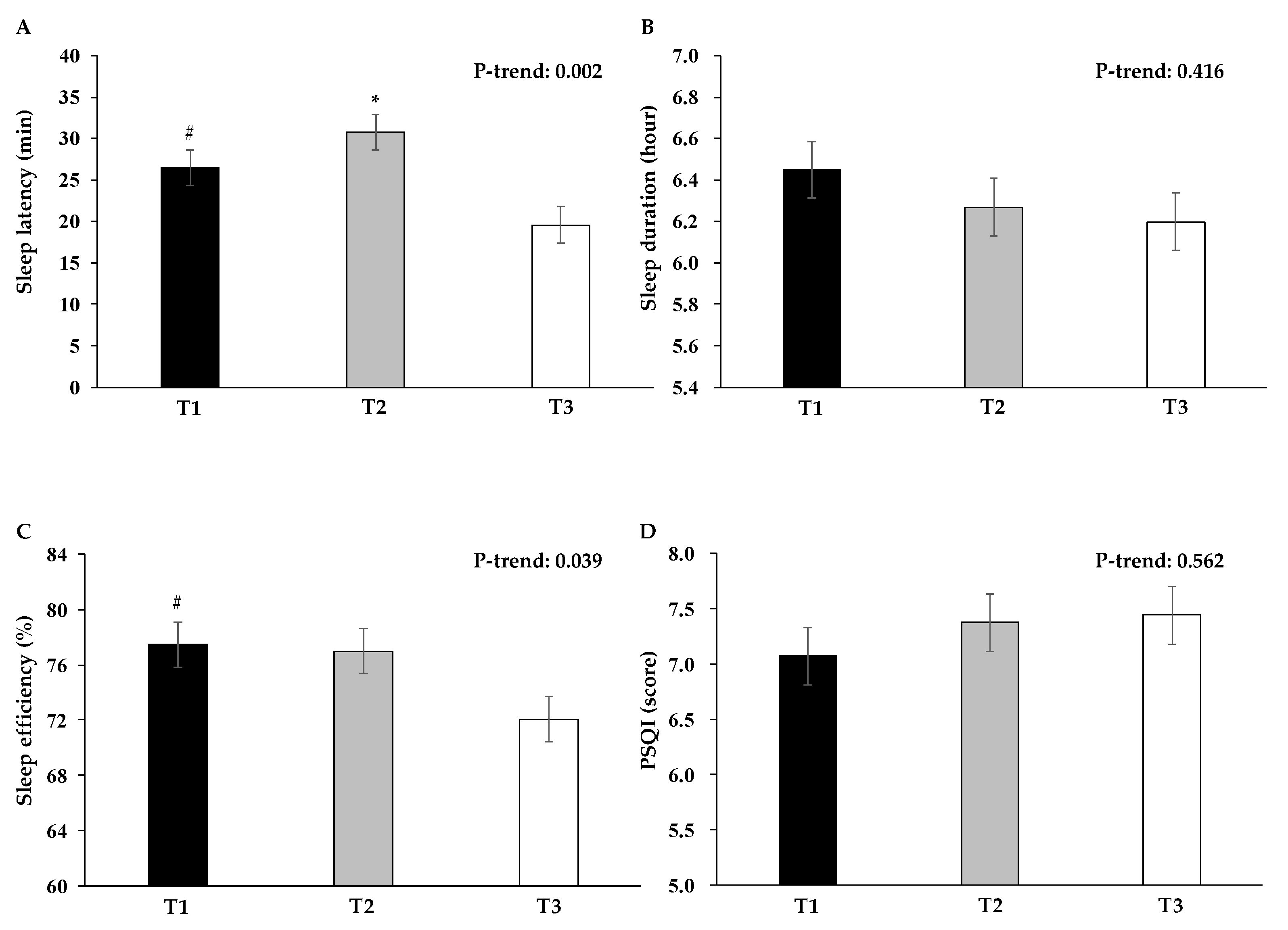
| Sleep latency, min | 25.7 | (21.3–30.1) | 30.0 | (25.0–35.1) | 21.1 | (17.4–24.7) | 0.024 |
| Sleep duration, hour | 6.5 | (6.2–6.7) | 6.3 | (6.1–6.6) | 6.1 | (5.8–6.4) | 0.257 |
| Sleep efficiency, % | 78.1 | (74.1–82.1) | 78.0 | (74.9–81.2) | 70.4 | (66.6–74.1) | 0.003 |
| PSQI, score | 7.0 | (6.4–7.5) | 7.1 | (6.5–7.7) | 7.8 | (7.2–8.4) | 0.147 |
| MEQ, score | 53.7 | (52.0–55.4) | 54.3 | (52.7–55.8) | 52.3 | (50.8–53.8) | 0.126 |
| CFS, score | 15.8 | (14.3–17.3) | 15.1 | (13.8–16.4) | 17.3 | (15.6–19.0) | 0.190 |
| IPAQ, MET-min/week | 2751.5 | (2189.1–3313.9) | 2522.6 | (2049.3–2995.9) | 2930.3 | (2415.5–3445.1) | 0.344 |
| TDB, hour | 2.7 | (2.5–2.9) | 4.3 | (4.2–4.4) | 5.9 | (5.7–6.1) | <0.001 |
| T1 (n = 88) | T2 (n = 88) | T3 (n = 88) | p Values | ||||
|---|---|---|---|---|---|---|---|
| Total | |||||||
| Energy, kcal | 2015 | (1907–2123) | 1933 | (1832–2034) | 1873 | (1751–1995) | 0.128 |
| Protein, g | 72.3 | (67.7–76.9) | 71.5 | (67.3–75.7) | 67.8 | (62.4–73.1) | 0.255 |
| Fat, g | 69.8 | (65.1–74.7) | 65.5 | (61.6–69.4) | 63.4 | (59.1–67.6) | 0.107 |
| Carbohydrate, g | 264.9 | (249.6–280.2) | 254.9 | (239.3–270.6) | 249.3 | (231.7–266.8) | 0.171 |
| * Energy-adjusted protein, g | 70.2 | (66.6–73.8) | 71.5 | (67.8–75.2) | 69.4 | (65.6–73.2) | 0.577 |
| * Energy-adjusted fat, g | 67.6 | (64.7–70.5) | 65.7 | (62.9–68.4) | 65.0 | (62.2–67.7) | 0.398 |
| * Energy-adjusted carbohydrate, g | 256.3 | (246.0–266.7) | 255.7 | (245.3–266.1) | 255.3 | (245.9–264.7) | 0.965 |
| Breakfast | |||||||
| Energy, kcal | 372 | (322–422) | 344 | (304–384) | 359 | (310–408) | 0.900 |
| Protein, g | 12.1 | (10.3–14.0) | 11.9 | (10.3–13.5) | 12.3 | (10.3–14.3) | 0.983 |
| Fat, g | 12.6 | (10.5–14.7) | 10.9 | (9.4–12.5) | 11.7 | (9.9–13.5) | 0.740 |
| Carbohydrate, g | 52.0 | (45.0–59.0) | 49.2 | (43.3–55.0) | 50.7 | (43.7–57.7) | 0.921 |
| * Energy-adjusted protein, g | 11.6 | (10.3–12.8) | 12.7 | (11.5–13.9) | 12.0 | (10.7–13.3) | 0.220 |
| * Energy-adjusted fat, g | 12.1 | (10.8–13.4) | 11.8 | (10.7–12.9) | 11.4 | (10.3–12.6) | 0.718 |
| * Energy-adjusted carbohydrate, g | 49.9 | (45.5–54.3) | 52.4 | (48.6–56.2) | 49.7 | (45.5–53.8) | 0.817 |
| Lunch | |||||||
| Energy, kcal | 664 | (622–707) | 655 | (610–700) | 626 | (571–682) | 0.719 |
| Protein, g | 23.9 | (22.4–25.5) | 23.4 | (21.6–25.3) | 21.8 | (19.6–24.0) | 0.260 |
| Fat, g | 21.9 | (20.0–23.7) | 20.8 | (18.9–22.7) | 20.8 | (18.6–22.9) | 0.704 |
| Carbohydrate, g | 89.4 | (82.7–96.0) | 90.1 | (83.7–96.5) | 84.8 | (76.7–92.9) | 0.562 |
| * Energy-adjusted protein, g | 23.8 | (22.8–24.9) | 23.5 | (22.3–24.8) | 21.8 | (20.1–23.5) | 0.050 |
| * Energy-adjusted fat, g | 21.8 | (20.6–23.0) | 20.9 | (19.7–22.1) | 20.7 | (19.2–22.3) | 0.553 |
| * Energy-adjusted carbohydrate, g | 89.1 | (84.9–93.3) | 90.6 | (86.9–94.2) | 84.5 | (79.0–90.0) | 0.291 |
| Dinner | |||||||
| Energy, kcal | 755 | (694–817) | 759 | (707–811) | 753 | (678–828) | 0.926 |
| Protein, g | 30.8 | (28.1–33.4) | 31.7 | (29.2–34.2) | 30.1 | (26.8–33.5) | 0.630 |
| Fat, g | 26.9 | (24.1–29.6) | 28.1 | (25.5–30.7) | 26.6 | (23.7–29.5) | 0.714 |
| Carbohydrate, g | 92.2 | (83.8–100.6) | 88.9 | (81.9–95.9) | 93.0 | (83.1–102.8) | 0.791 |
| * Energy-adjusted protein, g | 31.1 | (29.2–33.1) | 31.6 | (29.4–33.8) | 29.9 | (27.8–32.0) | 0.438 |
| * Energy-adjusted fat, g | 27.2 | (25.3–29.1) | 27.9 | (26.1–29.8) | 26.4 | (24.7–28.1) | 0.507 |
| * Energy-adjusted carbohydrate, g | 93.2 | (87.3–99.2) | 88.8 | (82.8–94.8) | 92.0 | (86.4–97.7) | 0.623 |
| Snacks | |||||||
| Energy, kcal | 223 | (180–266) | 175 | (141–209) | 135 | (108–162) | 0.013 |
| Protein, g | 5.5 | (4.2–6.7) | 4.4 | (3.3–5.6) | 3.5 | (2.3–4.8) | 0.017 |
| Fat, g | 8.4 | (6.4–10.4) | 5.7 | (4.5–6.9) | 4.3 | (3.2–5.4) | 0.003 |
| Carbohydrate, g | 31.3 | (25.4–37.3) | 26.8 | (21.1–32.4) | 20.9 | (16.5–25.3) | 0.042 |
| * Energy-adjusted protein, g | 4.5 | (3.6–5.4) | 4.6 | (3.7–5.4) | 4.4 | (3.3–5.4) | 0.476 |
| * Energy-adjusted fat, g | 6.7 | (5.7–7.6) | 5.9 | (5.1–6.7) | 5.6 | (4.8–6.5) | 0.305 |
| * Energy-adjusted carbohydrate, g | 25.2 | (22.2–28.3) | 27.5 | (24.3–30.7) | 25.6 | (22.4–28.8) | 0.656 |
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Saner, N.J.; Lee, M.J.; Pitchford, N.W.; Kuang, J.; Roach, G.D.; Garnham, A.; Stokes, T.; Phillips, S.M.; Bishop, D.J.; Bartlett, J.D. The effect of sleep restriction, with or without high-intensity interval exercise, on myofibrillar protein synthesis in healthy young men. J. Physiol. 2020, 598, 1523–1536. [Google Scholar] [CrossRef]
- Nedeltcheva, A.V.; Kilkus, J.M.; Imperial, J.; Schoeller, D.A.; Penev, P.D. Insufficient sleep undermines dietary efforts to reduce adiposity. Ann. Intern. Med. 2010, 153, 435–441. [Google Scholar] [CrossRef]
- Sexton, C.E.; Storsve, A.B.; Walhovd, K.B.; Johansen-Berg, H.; Fjell, A.M. Poor sleep quality is associated with increased cortical atrophy in community-dwelling adults. Neurology 2014, 83, 967–973. [Google Scholar] [CrossRef] [PubMed]
- Arendt, J.; Skene, D.J. Melatonin as a chronobiotic. Sleep Med. Rev. 2005, 9, 25–39. [Google Scholar] [CrossRef] [PubMed]
- Sapede, D.; Cau, E. The pineal gland from development to function. Curr. Top. Dev. Biol. 2013, 106, 171–215. [Google Scholar] [CrossRef] [PubMed]
- Chauffard-Alboucq, F.A.; Leathwood, P.D.; Dormond, C.A. Changes in plasma amino acid and subjective sleepiness ratings in humans after consuming L-tryptophan/maltodextrin mixes. Amino. Acids 1991, 1, 37–45. [Google Scholar] [CrossRef]
- Voderholzer, U.; Hornyak, M.; Thiel, B.; Huwig-Poppe, C.; Kiemen, A.; Konig, A.; Backhaus, J.; Riemann, D.; Berger, M.; Hohagen, F. Impact of experimentally induced serotonin deficiency by tryptophan depletion on sleep EEG in healthy subjects. Neuropsychopharmacology 1998, 18, 112–124. [Google Scholar] [CrossRef]
- George, C.F.; Millar, T.W.; Hanly, P.J.; Kryger, M.H. The effect of L-tryptophan on daytime sleep latency in normals: Correlation with blood levels. Sleep 1989, 12, 345–353. [Google Scholar] [CrossRef]
- Yasuda, J.; Yoshizaki, T.; Yamamoto, K.; Yoshino, M.; Ota, M.; Kawahara, T.; Kamei, A. Association of Frequency of Milk or Dairy Product Consumption with Subjective Sleep Quality during Training Periods in Japanese Elite Athletes: A Cross-Sectional Study. J. Nutr. Sci. Vitaminol. 2019, 65, 177–183. [Google Scholar] [CrossRef]
- Al-Haifi, A.A.; AlMajed, H.T.; Al-Hazzaa, H.M.; Musaiger, A.O.; Arab, M.A.; Hasan, R.A. Relative Contribution of Obesity, Sedentary Behaviors and Dietary Habits to Sleep Duration Among Kuwaiti Adolescents. Glob. J. Health Sci. 2016, 8, 107–117. [Google Scholar] [CrossRef]
- Yamamura, S.; Morishima, H.; Kumano-go, T.; Suganuma, N.; Matsumoto, H.; Adachi, H.; Sigedo, Y.; Mikami, A.; Kai, T.; Masuyama, A.; et al. The effect of Lactobacillus helveticus fermented milk on sleep and health perception in elderly subjects. Eur. J. Clin. Nutr. 2009, 63, 100–105. [Google Scholar] [CrossRef]
- Wurtman, R.J.; Wurtman, J.J.; Regan, M.M.; McDermott, J.M.; Tsay, R.H.; Breu, J.J. Effects of normal meals rich in carbohydrates or proteins on plasma tryptophan and tyrosine ratios. Am. J. Clin. Nutr. 2003, 77, 128–132. [Google Scholar] [CrossRef]
- Lyons, P.M.; Truswell, A.S. Serotonin precursor influenced by type of carbohydrate meal in healthy adults. Am. J. Clin. Nutr. 1988, 47, 433–439. [Google Scholar] [CrossRef]
- Afaghi, A.; O’Connor, H.; Chow, C.M. High-glycemic-index carbohydrate meals shorten sleep onset. Am. J. Clin. Nutr. 2007, 85, 426–430. [Google Scholar] [CrossRef]
- Iao, S.I.; Jansen, E.; Shedden, K.; O’Brien, L.M.; Chervin, R.D.; Knutson, K.L.; Dunietz, G.L. Associations between bedtime eating or drinking, sleep duration and wake after sleep onset: Findings from the American time use survey. Br. J. Nutr. 2021, 127, 1–10. [Google Scholar] [CrossRef]
- Mollayeva, T.; Thurairajah, P.; Burton, K.; Mollayeva, S.; Shapiro, C.M.; Colantonio, A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med. Rev. 2016, 25, 52–73. [Google Scholar] [CrossRef]
- Ohayon, M.; Wickwire, E.M.; Hirshkowitz, M.; Albert, S.M.; Avidan, A.; Daly, F.J.; Dauvilliers, Y.; Ferri, R.; Fung, C.; Gozal, D.; et al. National Sleep Foundation’s sleep quality recommendations: First report. Sleep Health 2017, 3, 6–19. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Doi, Y.; Minowa, M.; Uchiyama, M.; Okawa, M.; Kim, K.; Shibui, K.; Kamei, Y. Psychometric assessment of subjective sleep quality using the Japanese version of the Pittsburgh Sleep Quality Index (PSQI-J) in psychiatric disordered and control subjects. Psychiatry Res. 2000, 97, 165–172. [Google Scholar] [CrossRef]
- Horne, J.A.; Ostberg, O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int. J. Chronobiol. 1976, 4, 97–110. [Google Scholar]
- Chalder, T.; Berelowitz, G.; Pawlikowska, T.; Watts, L.; Wessely, S.; Wright, D.; Wallace, E.P. Development of a fatigue scale. J. Psychosom. Res. 1993, 37, 147–153. [Google Scholar] [CrossRef]
- Tanaka, M.; Fukuda, S.; Mizuno, K.; Imai-Matsumura, K.; Jodoi, T.; Kawatani, J.; Takano, M.; Miike, T.; Tomoda, A.; Watanabe, Y. Reliability and validity of the Japanese version of the Chalder Fatigue Scale among youth in Japan. Psychol. Rep. 2008, 103, 682–690. [Google Scholar] [CrossRef]
- Craig, C.L.; Marshall, A.L.; Sjostrom, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef]
- Murase, N.; Katsumura, T.; Ueda, C.; Inoue, S.; Shimomitsu, T. Validity and reliability of Japanese version of International Physical Activity Questionnaire. J. Health Welf. Stat. 2002, 49, 1–9. [Google Scholar]
- Sujarwoto, S. Sleep Disturbance in Indonesia: How Much Does Smoking Contribute? Behav. Sleep Med. 2020, 18, 760–773. [Google Scholar] [CrossRef]
- Zhu, H.; Xu, H.; Chen, R.; Liu, S.; Xia, Y.; Fu, Y.; Li, X.; Qian, Y.; Zou, J.; Yi, H.; et al. Smoking, obstructive sleep apnea syndrome and their combined effects on metabolic parameters: Evidence from a large cross-sectional study. Sci. Rep. 2017, 7, 8851. [Google Scholar] [CrossRef]
- Mehari, A.; Weir, N.A.; Gillum, R.F. Gender and the association of smoking with sleep quantity and quality in American adults. Women Health 2014, 54, 1–14. [Google Scholar] [CrossRef]
- McNamara, J.P.; Wang, J.; Holiday, D.B.; Warren, J.Y.; Paradoa, M.; Balkhi, A.M.; Fernandez-Baca, J.; McCrae, C.S. Sleep disturbances associated with cigarette smoking. Psychol. Health Med. 2014, 19, 410–419. [Google Scholar] [CrossRef]
- Patrick, M.E.; Griffin, J.; Huntley, E.D.; Maggs, J.L. Energy Drinks and Binge Drinking Predict College Students’ Sleep Quantity, Quality, and Tiredness. Behav. Sleep Med. 2018, 16, 92–105. [Google Scholar] [CrossRef]
- Fucito, L.M.; Bold, K.W.; Van Reen, E.; Redeker, N.S.; O’Malley, S.S.; Hanrahan, T.H.; DeMartini, K.S. Reciprocal variations in sleep and drinking over time among heavy-drinking young adults. J. Abnorm. Psychol. 2018, 127, 92–103. [Google Scholar] [CrossRef]
- Ehlers, C.L.; Wills, D.; Gilder, D.A. A history of binge drinking during adolescence is associated with poorer sleep quality in young adult Mexican Americans and American Indians. Psychopharmacology 2018, 235, 1775–1782. [Google Scholar] [CrossRef]
- Popovici, I.; French, M.T. Binge drinking and sleep problems among young adults. Drug Alcohol. Depend 2013, 132, 207–215. [Google Scholar] [CrossRef]
- Nunez, P.; Perillan, C.; Arguelles, J.; Diaz, E. Comparison of sleep and chronotype between senior and undergraduate university students. Chronobiol. Int. 2019, 36, 1626–1637. [Google Scholar] [CrossRef]
- Fong, T.C.; Chan, J.S.; Chan, C.L.; Ho, R.T.; Ziea, E.T.; Wong, V.C.; Ng, B.F.; Ng, S.M. Psychometric properties of the Chalder Fatigue Scale revisited: An exploratory structural equation modeling approach. Qual. Life Res. 2015, 24, 2273–2278. [Google Scholar] [CrossRef]
- Park, H.; Suh, B. Association between sleep quality and physical activity according to gender and shift work. J. Sleep Res. 2020, 29, e12924. [Google Scholar] [CrossRef]
- Willett, W.C.; Howe, G.R.; Kushi, L.H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 1997, 65, 1220S–1228S; discussion 1229S–1231S. [Google Scholar] [CrossRef]
- Fagerland, M.W. t-tests, non-parametric tests, and large studies--A paradox of statistical practice? BMC Med. Res. Methodol. 2012, 12, 78. [Google Scholar] [CrossRef]
- Lopes, T.; Borba, M.E.; Lopes, R.; Fisberg, R.M.; Lemos Paim, S.; Vasconcelos Teodoro, V.; Zalcman Zimberg, I.; Crispim, C.A. Eating Late Negatively Affects Sleep Pattern and Apnea Severity in Individuals With Sleep Apnea. J. Clin. Sleep Med. 2019, 15, 383–392. [Google Scholar] [CrossRef]
- Chung, N.; Bin, Y.S.; Cistulli, P.A.; Chow, C.M. Does the Proximity of Meals to Bedtime Influence the Sleep of Young Adults? A Cross-Sectional Survey of University Students. Int. J. Environ. Res. Public Health 2020, 17, 2677. [Google Scholar] [CrossRef]
- Chen, C.Y.; Asakawa, A.; Fujimiya, M.; Lee, S.D.; Inui, A. Ghrelin gene products and the regulation of food intake and gut motility. Pharmacol. Rev. 2009, 61, 430–481. [Google Scholar] [CrossRef] [PubMed]
- Weikel, J.C.; Wichniak, A.; Ising, M.; Brunner, H.; Friess, E.; Held, K.; Mathias, S.; Schmid, D.A.; Uhr, M.; Steiger, A. Ghrelin promotes slow-wave sleep in humans. Am. J. Physiol. Endocrinol. Metab. 2003, 284, E407–E415. [Google Scholar] [CrossRef]
- Kluge, M.; Schussler, P.; Bleninger, P.; Kleyer, S.; Uhr, M.; Weikel, J.C.; Yassouridis, A.; Zuber, V.; Steiger, A. Ghrelin alone or co-administered with GHRH or CRH increases non-REM sleep and decreases REM sleep in young males. Psychoneuroendocrinology 2008, 33, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Kluge, M.; Gazea, M.; Schussler, P.; Genzel, L.; Dresler, M.; Kleyer, S.; Uhr, M.; Yassouridis, A.; Steiger, A. Ghrelin increases slow wave sleep and stage 2 sleep and decreases stage 1 sleep and REM sleep in elderly men but does not affect sleep in elderly women. Psychoneuroendocrinology 2010, 35, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Gibbons, C.; Caudwell, P.; Finlayson, G.; Webb, D.L.; Hellstrom, P.M.; Naslund, E.; Blundell, J.E. Comparison of postprandial profiles of ghrelin, active GLP-1, and total PYY to meals varying in fat and carbohydrate and their association with hunger and the phases of satiety. J. Clin. Endocrinol. Metab. 2013, 98, E847–E855. [Google Scholar] [CrossRef]
- Smotek, M.; Farkova, E.; Mankova, D.; Koprivova, J. Evening and night exposure to screens of media devices and its association with subjectively perceived sleep: Should “light hygiene” be given more attention? Sleep Health 2020, 6, 498–505. [Google Scholar] [CrossRef]
- Shimura, A.; Sugiura, K.; Inoue, M.; Misaki, S.; Tanimoto, Y.; Oshima, A.; Tanaka, T.; Yokoi, K.; Inoue, T. Which sleep hygiene factors are important? comprehensive assessment of lifestyle habits and job environment on sleep among office workers. Sleep Health 2020, 6, 288–298. [Google Scholar] [CrossRef]
- Matuzaki, L.; Santos-Silva, R.; Marqueze, E.C.; de Castro Moreno, C.R.; Tufik, S.; Bittencourt, L. Temporal sleep patterns in adults using actigraph. Sleep Sci. 2014, 7, 152–157. [Google Scholar] [CrossRef]
- Kim, Y.; Park, I.; Kang, M. Convergent validity of the international physical activity questionnaire (IPAQ): Meta-analysis. Public Health Nutr. 2013, 16, 440–452. [Google Scholar] [CrossRef]
- Kitazawa, M.; Yoshimura, M.; Hitokoto, H.; Sato-Fujimoto, Y.; Murata, M.; Negishi, K.; Mimura, M.; Tsubota, K.; Kishimoto, T. Survey of the effects of internet usage on the happiness of Japanese university students. Health Qual. Life Outcomes 2019, 17, 151. [Google Scholar] [CrossRef]
- Toyama, N.; Ekuni, D.; Taniguchi-Tabata, A.; Yoneda, T.; Kataoka, K.; Yokoi, A.; Uchida, Y.; Fukuhara, D.; Saho, H.; Monirul, I.M.; et al. Associations between sleep bruxism, sleep quality, and exposure to secondhand smoke in Japanese young adults: A cross-sectional study. Sleep Med. 2020, 68, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Zeron-Rugerio, M.F.; Longo-Silva, G.; Hernaez, A.; Ortega-Regules, A.E.; Cambras, T.; Izquierdo-Pulido, M. The Elapsed Time between Dinner and the Midpoint of Sleep is Associated with Adiposity in Young Women. Nutrients 2020, 12, 410. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yasuda, J.; Kishi, N.; Fujita, S. Association between Time from Dinner to Bedtime and Sleep Quality Indices in the Young Japanese Population: A Cross-Sectional Study. Dietetics 2023, 2, 140-149. https://doi.org/10.3390/dietetics2020011
Yasuda J, Kishi N, Fujita S. Association between Time from Dinner to Bedtime and Sleep Quality Indices in the Young Japanese Population: A Cross-Sectional Study. Dietetics. 2023; 2(2):140-149. https://doi.org/10.3390/dietetics2020011
Chicago/Turabian StyleYasuda, Jun, Nanami Kishi, and Satoshi Fujita. 2023. "Association between Time from Dinner to Bedtime and Sleep Quality Indices in the Young Japanese Population: A Cross-Sectional Study" Dietetics 2, no. 2: 140-149. https://doi.org/10.3390/dietetics2020011
APA StyleYasuda, J., Kishi, N., & Fujita, S. (2023). Association between Time from Dinner to Bedtime and Sleep Quality Indices in the Young Japanese Population: A Cross-Sectional Study. Dietetics, 2(2), 140-149. https://doi.org/10.3390/dietetics2020011






