Virtual and Augmented Reality versus Traditional Methods for Teaching Physiotherapy: A Systematic Review
Abstract
1. Introduction
1.1. Information and Communication Technologies in Education
1.2. Virtual and Augmented Reality
1.3. Virtual and Augmented Reality for Health-Related Adult Education
1.4. New Technologies for Teaching Physiotherapy
1.5. Justification and Objective
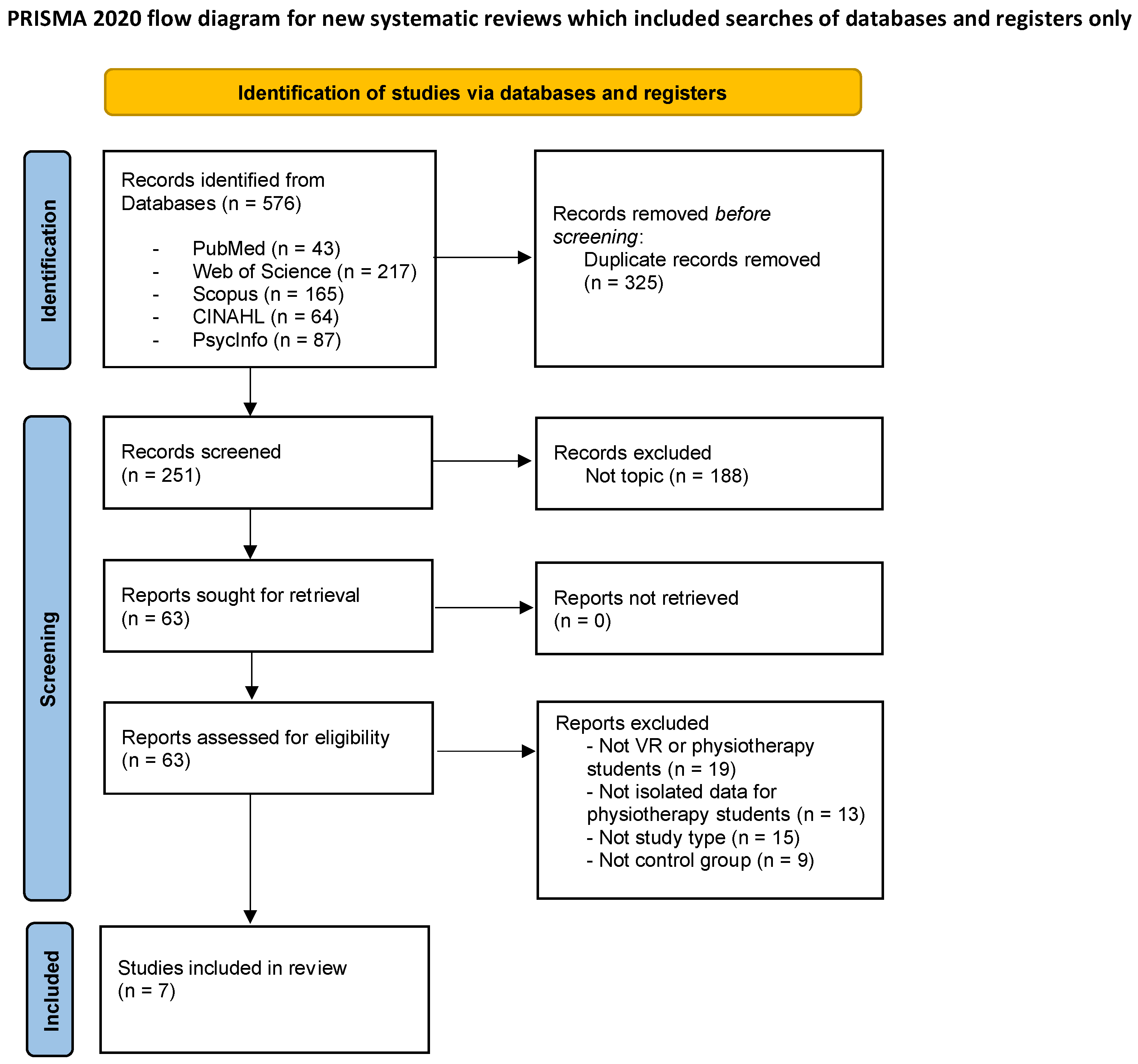
2. Materials and Methods
2.1. Design
2.2. Search Strategy
2.3. Eligibility Criteria
2.4. Selection Process and Data Extraction
2.5. Methodological Quality and Risk of Bias Assessment
3. Results
3.1. Study Types
3.2. Results on Methodological Quality and Risk of Bias
3.3. Participant Characteristics
3.4. VR-AR Systems
3.5. Teaching Content and Duration
3.6. Study Results
3.6.1. Learning Satisfaction
3.6.2. Academic Performance
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McKay, F.H.; Cheng, C.; Wright, A.; Shill, J.; Stephens, H.; Uccellini, M. Evaluating Mobile Phone Applications for Health Behaviour Change: A Systematic Review. J. Telemed. Telecare 2018, 24, 22–30. [Google Scholar] [CrossRef]
- Nicolaou, C.; Matsiola, M.; Kalliris, G. Technology-Enhanced Learning and Teaching Methodologies through Audiovisual Media. Educ. Sci. 2019, 9, 196. [Google Scholar] [CrossRef]
- Delgado, M.; Arrieta, X.; Riveros, V. Uso de Las TIC En Educación, Una Propuesta Para Su Optimización. Omnia Año 2009, 15, 58–77. [Google Scholar]
- Vazquez-Lopez, V.; Huerta-Manzanilla, E.L. Factors Related with Underperformance in Reading Proficiency, the Case of the Programme for International Student Assessment 2018. Eur. J. Investig. Health Psychol. Educ. 2021, 11, 813–828. [Google Scholar] [CrossRef] [PubMed]
- Zaldivar, A.; Tripp, C.; Aguilar, J.A.; Tovar, J.E.; Anguiano, C.E. Using Mobile Technologies to Support Learning in Computer Science Students. IEEE Lat. Am. Trans. 2015, 13, 377–382. [Google Scholar] [CrossRef]
- Arribas, E.; Escobar, I.; Suarez, C.P.; Najera, A.; Beléndez, A. Measurement of the Magnetic Field of Small Magnets with a Smartphone: A Very Economical Laboratory Practice for Introductory Physics Courses. Eur. J. Phys. 2015, 36, 065002. [Google Scholar] [CrossRef]
- Ainsley, B.; Brown, A. The Impact of Informatics on Nursing Education: A Review of the Literature. J. Contin. Educ. Nurs. 2009, 40, 228–232. [Google Scholar] [CrossRef]
- Nicolaou, C.; Kalliris, G. Audiovisual Media Communications in Adult Education: The Case of Cyprus and Greece of Adults as Adult Learners. Eur. J. Investig. Health Psychol. Educ. 2020, 10, 967–994. [Google Scholar] [CrossRef]
- Weiss, P.L.; Kizony, R.; Feintuch, U.; Katz, N. Virtual Reality in Neurorehabilitation. In Textbook of Neural Repair and Rehabilitation; Selzer, M., Cohen, L., Gage, F., Clarke, S., Duncan, P., Eds.; Cambridge University Press: Cambridge, UK, 2006; Volume 51, pp. 182–197. [Google Scholar]
- Zhao, J.; Xu, X.; Jiang, H.; Ding, Y. The Effectiveness of Virtual Reality-Based Technology on Anatomy Teaching: A Meta-Analysis of Randomized Controlled Studies. BMC Med. Educ. 2020, 20, 127. [Google Scholar] [CrossRef]
- Domínguez-Téllez, P.; Moral-Muñoz, J.A.; Salazar, A.; Casado-Fernández, E.; Lucena-Antón, D. Game-Based Virtual Reality Interventions to Improve Upper Limb Motor Function and Quality of Life after Stroke: Systematic Review and Meta-Analysis. Games Health J. 2020, 9, 1–10. [Google Scholar] [CrossRef]
- Henderson, A.; Korner-Bitensky, N.; Levin, M. Virtual Reality in Stroke Rehabilitation: A Systematic Review of Its Effectiveness for Upper Limb Motor Recovery. Top Stroke Rehabil. 2007, 14, 52–61. [Google Scholar] [CrossRef]
- Xiong, J.; Hsiang, E.L.; He, Z.; Zhan, T.; Wu, S.T. Augmented Reality and Virtual Reality Displays: Emerging Technologies and Future Perspectives. Light Sci. Appl. 2021, 10, 216. [Google Scholar] [CrossRef]
- Cordova, D.I.; Lepper, M.R. Intrinsic Motivation and the Process of Learning: Beneficial Effects of Contextualization, Personalization, and Choice. J. Educ. Psychol. 1996, 88, 715–730. [Google Scholar] [CrossRef]
- Merchant, Z.; Goetz, E.T.; Cifuentes, L.; Keeney-Kennicutt, W.; Davis, T.J. Effectiveness of Virtual Reality-Based Instruction on Students’ Learning Outcomes in K-12 and Higher Education: A Meta-Analysis. Comput. Educ. 2014, 70, 29–40. [Google Scholar] [CrossRef]
- Pan, Z.; Cheok, A.D.; Yang, H.; Zhu, J.; Shi, J. Virtual Reality and Mixed Reality for Virtual Learning Environments. Comput. Graph. 2006, 30, 20–28. [Google Scholar] [CrossRef]
- Calvo-Ferrer, J.R.; Belda-Medina, J.R. Análisis de La Satisfacción Del Alumnado de L2 Con Respecto a La Adquisición de Terminología Especializada Por Medio de Videojuegos: Estudio de Caso. Porta Ling. 2015, 24, 179–190. [Google Scholar] [CrossRef]
- Rojas-Sánchez, M.A.; Palos-Sánchez, P.R.; Folgado-Fernández, J.A. Systematic Literature Review and Bibliometric Analysis on Virtual Reality and Education. Educ. Inf. Technol. (Dordr.) 2022, 1–38. [Google Scholar] [CrossRef]
- Christou, C. Virtual Reality in Education. In Affective, Interactive and Cognitive Methods for E-Learning Design: Creating an Optimal Education Experience; Tzanavari, A., Tsapatsoulis, N., Eds.; IGI Global: Hershey, PA, USA, 2010; pp. 228–243. [Google Scholar]
- Cesar Ferreira, F.; Baffa Lourenço, A.; Alves da Cruz, A.J.; Paza, A.H.; Botero, E.R.; Matos Rocha, E. Argumentation in a Virtual Reality Environment: An Approach with Future Physics Teachers. RIED-Rev. Iberoam. De Educ. A Distancia 2021, 24, 179–195. [Google Scholar] [CrossRef]
- Vidal, I.M.G.; López, B.C.; Otero, L.C. New Digital Skills in Students Empowered with the Use of Augmented Reality. Pilot Study. RIED-Rev. Iberoam. De Educ. A Distancia 2021, 24, 137–157. [Google Scholar] [CrossRef]
- Dyer, E.; Swartzlander, B.J.; Gugliucci, M.R. Using Virtual Reality in Medical Education to Teach Empathy. J. Med. Libr. Assoc. 2018, 106, 498–500. [Google Scholar] [CrossRef]
- Shorey, S.; Ng, E.D. The Use of Virtual Reality Simulation among Nursing Students and Registered Nurses: A Systematic Review. Nurse Educ. Today 2021, 98, 104662. [Google Scholar] [CrossRef]
- Berns, A.; Reyes-Sánchez, S. A Review of Virtual Reality-Based Language Learning Apps. RIED-Rev. Iberoam. De Educ. A Distancia 2021, 24, 159–177. [Google Scholar] [CrossRef]
- Kurul, R.; Ögün, M.N.; Neriman Narin, A.; Avci, Ş.; Yazgan, B. An Alternative Method for Anatomy Training: Immersive Virtual Reality. Anat. Sci. Educ. 2020, 13, 648–656. [Google Scholar] [CrossRef]
- Hurst, K.M. Using Video Podcasting to Enhance the Learning of Clinical Skills: A Qualitative Study of Physiotherapy Students’ Experiences. Nurse Educ. Today 2016, 45, 206–211. [Google Scholar] [CrossRef]
- Hoang, T.; Reinoso, M.; Joukhadar, Z.; Vetere, F.; Kelly, D. Augmented Studio: Projection Mapping on Moving Body for Physiotherapy Education. In Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems, Denver, CO, USA, 6–11 May 2017; Association for Computing Machinery: New York, NY, USA, 2017; pp. 1419–1430. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Scoping reviews (2020 version). In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, Australia, 2020. [Google Scholar]
- Tufanaru, C.; Munn, Z.; Aromataris, E.; Campbell, J.; Hopp, L. Systematic Reviews of Effectiveness. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, Australia, 2020. [Google Scholar]
- Higgins, J.; Savović, J.; Page, M.J.; Sterne, J.A.C. RoB 2: A Revised Cochrane Risk-of-Bias Tool for Randomized Trials. Br. Med. J. 2019, 366, l4898. [Google Scholar]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A Tool for Assessing Risk of Bias in Non-Randomised Studies of Interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Huhn, K.; McGinnis, P.Q.; Wainwright, S.; Deutsch, J.E. A Comparison of 2 Case Delivery Methods: Virtual and Live. J. Phys. Ther. Educ. 2013, 27, 41–48. [Google Scholar] [CrossRef]
- Ulrich, F.; Helms, N.H.; Frandsen, U.P.; Rafn, A.V. Learning Effectiveness of 360° Video: Experiences from a Controlled Experiment in Healthcare Education. Interact. Learn. Environ. 2019, 29, 98–111. [Google Scholar] [CrossRef]
- Ferdous, H.S.; Hoang, T.; Joukhadar, Z.; Reinoso, M.N.; Vetere, F.; Kelly, D.; Remedios, L. “What’s Happening at That Hip?”: Evaluating an On-Body Projection Based Augmented Reality System for Physiotherapy Classroom. In Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems, Glasgow Scotland, UK, 4–9 May 2019; Association for Computing Machinery: New York, NY, USA, 2019; pp. 1–12. [Google Scholar]
- Favolise, M. The Effectiveness of Augmented and Virtual Reality in the Education of Physical Therapy Students. Arch. Phys. Med. Rehabil. 2021, 102, e84. [Google Scholar] [CrossRef]
- Kandasamy, G.; Bettany-Saltikov, J.; Cordry, J.; McSherry, R. Use of Vision-Based Augmented Reality to Improve Student Learning of the Spine and Spinal Deformities. An Exploratory Study. S. Afr. J. Physiother. 2021, 77, 1a1579. [Google Scholar] [CrossRef] [PubMed]
- Hartstein, A.J.; Zimney, K.; Verkuyl, M.; Yockey, J.; Berg-Poppe, P. Virtual Reality Instructional Design in Orthopedic Physical Therapy Education: A Randomized Controlled Trial. J. Phys. Ther. Educ. 2022, 36, 176–184. [Google Scholar] [CrossRef]
- Zhao, G.; Fan, M.; Yuan, Y.; Zhao, F.; Huang, H. The Comparison of Teaching Efficiency between Virtual Reality and Traditional Education in Medical Education: A Systematic Review and Meta-Analysis. Ann. Transl. Med. 2021, 9, 252. [Google Scholar] [CrossRef] [PubMed]
- Barteit, S.; Lanfermann, L.; Bärnighausen, T.; Neuhann, F.; Beiersmann, C. Augmented, Mixed, and Virtual Reality-Based Head-Mounted Devices for Medical Education: Systematic Review. JMIR Serious Games 2021, 9, e29080. [Google Scholar] [CrossRef]
- Tursø-Finnich, T.; Overgaard Jensen, R.; Jensen, L.X.; Konge, L.; Thinggaard, E. Virtual Reality Head-Mounted Displays in Medical Education-A Systematic Review. Simul. Healthc. J. Soc. Simul. Healthc. 2022. [Google Scholar] [CrossRef] [PubMed]
- Kyaw, B.M.; Saxena, N.; Posadzki, P.; Vseteckova, J.; Nikolaou, C.K.; George, P.P.; Divakar, U.; Masiello, I.; Kononowicz, A.A.; Zary, N.; et al. Virtual Reality for Health Professions Education: Systematic Review and Meta-Analysis by the Digital Health Education Collaboration. J. Med. Internet Res. 2019, 21, e12959. [Google Scholar] [CrossRef]
- Rickel, J. Intelligent Virtual Agents for Education and Training: Opportunities and Challenges. Conf. Intell. Virtual Agents 2001, 3, 15–22. [Google Scholar]



| Databases | Keywords | Results |
|---|---|---|
| PubMed | (“physical therapy” [Title/Abstract] OR physiotherapy [Title/Abstract]) AND (teaching [Title/Abstract] OR learning [Title/Abstract]) AND (“virtual reality” OR “augmented reality” OR “mixed reality” OR “virtual reality exposure therapy” OR “virtual system”) [Title/Abstract]) | 43 |
| Web of Science | TS = ((“physical therapy” OR physiotherapy) AND (teaching OR learning) AND (“virtual reality” OR “augmented reality” OR “mixed reality” OR “virtual reality exposure therapy” OR “virtual system”)) | 217 |
| Scopus | TS = ((“physical therapy” OR physiotherapy) AND (teaching OR learning) AND (“virtual reality” OR “augmented reality” OR “mixed reality” OR “virtual reality exposure therapy” OR “virtual system”)) | 165 |
| CINAHL | TS = ((“physical therapy” OR physiotherapy) AND (teaching OR learning) AND (“virtual reality” OR “augmented reality” OR “mixed reality” OR “virtual reality exposure therapy” OR “virtual system”)) | 64 |
| PsycInfo | TS = ((“physical therapy” OR physiotherapy) AND (teaching OR learning) AND (“virtual reality” OR “augmented reality” OR “mixed reality” OR “virtual reality exposure therapy” OR “virtual system”)) | 87 |
| Studies (Authors, Year, Country) | Study Design | Participants | Teaching Models | Duration/Content | Outcomes | Results | Methodological Quality (JBI) |
|---|---|---|---|---|---|---|---|
| Huhn et al. 2013. USA [33] | Randomised mixed-methods study | N = 53 graduate students (Doctoral) CG: 27 EG: 26 | CG: Traditional teaching based on large-group discussion EG: Virtual patient simulation through computer software | Six lessons Content: Pathology content and clinical reasoning | Pre-post measurement Health science reasoning test on clinical reasoning; 50-question exam for knowledge acquisition; Objective clinical structured examination to measure the transfer of learning. | There were no significant differences between groups, but EG showed higher results on all objective measures. | 6/13 |
| Ulrich et al. 2019. Denmark [34] | Randomised study | N = 81 graduate students G1: 28 G2: 28 G3: 27 | G1: VR HMD with 360° video (Samsung Gear VR) G2: Conventional videos via laptop G3: Traditional teaching | One lesson Content: The practical task of performing the correct positioning into the supine position | Pre-post measurement Questionnaire on academic performance, user satisfaction, and perception of learning climate. | Academic performance: all treatment groups were equally effective. User satisfaction: 360° video and conventional video were less effective than traditional teaching. Learning climate: only in the student’s emotions, the 360° video surpassed the conventional video. | 7/13 |
| Ferdous et al. 2019. Australia [35] | Randomised crossover study | N = 101 graduate students G1: 24–26 G2: 24–26 G3: 24–26 G4: 24–26 | CG: Traditional teaching EG: AR and projection of anatomical images, virtual pencils to create annotations | Two lessons of 1 h Content: different types of movements of the lower limb musculature | Pre-post measurement Standardised questionnaire type test score. | The results show a statistically significant mean increase in the questionnaire score (22.5%) in the EG with respect to the CG. Z-2.666, p-0.008. | 7/13 |
| Kurul et al. 2020. Turkey [25] | Randomised controlled study | N = 72 undergraduate students CG: 36 EG: 36 | CG: Traditional teaching EG: Immersive VR HMD (Oculus Rift) and “3D Organon Anatomy” software | One lesson of 30 min Content: anatomy and palpation of the cephalic region and neck | Pre-post measurement: Quiz-type questionnaire on anatomy with 15 multiple-choice questions. Likert-type scale on student perception. | Post scores were significantly higher compared to pre-test scores in both EG (p < 0.001) and CG (p < 0.001). The difference between pretest and post-test scores was significantly greater in favour of EG (p < 0.001). | 10/13 |
| Favolise 2021. USA [36] | Cohort longitudinal study | N = 297 graduate students (Doctoral) CG: 162 EG: 135 | CG: Traditional teaching EG: Visible Body through VR and AR software | N/A Content: Gross anatomy | Post measurement Exams for knowledge acquisition on osteology and cadaver dissection. Survey about self-efficacy. | Positive results were found for the EG group on knowledge acquisition of cadaver dissection, and student’s self-efficacy. | 2/11 |
| Kandasamy et al. 2021. United Kingdom [37] | Crossover longitudinal study | N = 74 undergraduate students CG: 37 EG: 37 | CG: Traditional teaching EG: Active learning using an AR mobile application | Two weeks Content: Anatomy of spine, and spine pathologies | Post measurement Structured questionnaire about level of understanding and engagement. | Significant results were found for the EG group on level of understanding and engagement. | 6/9 |
| Hartstein et al. 2022. USA [38] | Randomised controlled study | N = 59 graduate students (1st year) | CG: Traditional standardised patient instruction EG: Immersive VR learning experience with Oculus Quest 2 | One lesson Content: simulation of a patient encounter to enhance clinical decision-making skills | Pre-post measurement Clinical decision-making tool Metacognitive Awareness Inventory Diagnostic accuracy and efficiency Engagement Musculoskeletal objective structured clinical examination | Non-significant differences were found between groups for the clinical decision-making tool, metacognitive awareness inventory, diagnostic accuracy. Only the results for engagement are significant for the EG. | 10/13 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lucena-Anton, D.; Fernandez-Lopez, J.C.; Pacheco-Serrano, A.I.; Garcia-Munoz, C.; Moral-Munoz, J.A. Virtual and Augmented Reality versus Traditional Methods for Teaching Physiotherapy: A Systematic Review. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 1780-1792. https://doi.org/10.3390/ejihpe12120125
Lucena-Anton D, Fernandez-Lopez JC, Pacheco-Serrano AI, Garcia-Munoz C, Moral-Munoz JA. Virtual and Augmented Reality versus Traditional Methods for Teaching Physiotherapy: A Systematic Review. European Journal of Investigation in Health, Psychology and Education. 2022; 12(12):1780-1792. https://doi.org/10.3390/ejihpe12120125
Chicago/Turabian StyleLucena-Anton, David, Juan Carlos Fernandez-Lopez, Ana I. Pacheco-Serrano, Cristina Garcia-Munoz, and Jose A. Moral-Munoz. 2022. "Virtual and Augmented Reality versus Traditional Methods for Teaching Physiotherapy: A Systematic Review" European Journal of Investigation in Health, Psychology and Education 12, no. 12: 1780-1792. https://doi.org/10.3390/ejihpe12120125
APA StyleLucena-Anton, D., Fernandez-Lopez, J. C., Pacheco-Serrano, A. I., Garcia-Munoz, C., & Moral-Munoz, J. A. (2022). Virtual and Augmented Reality versus Traditional Methods for Teaching Physiotherapy: A Systematic Review. European Journal of Investigation in Health, Psychology and Education, 12(12), 1780-1792. https://doi.org/10.3390/ejihpe12120125











