Prolonged Grief Disorder and Symptoms of Anxiety and Depression among Bereaved Family Caregivers in the Context of Palliative Home Care
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Measures
2.3. Statistical Analysis
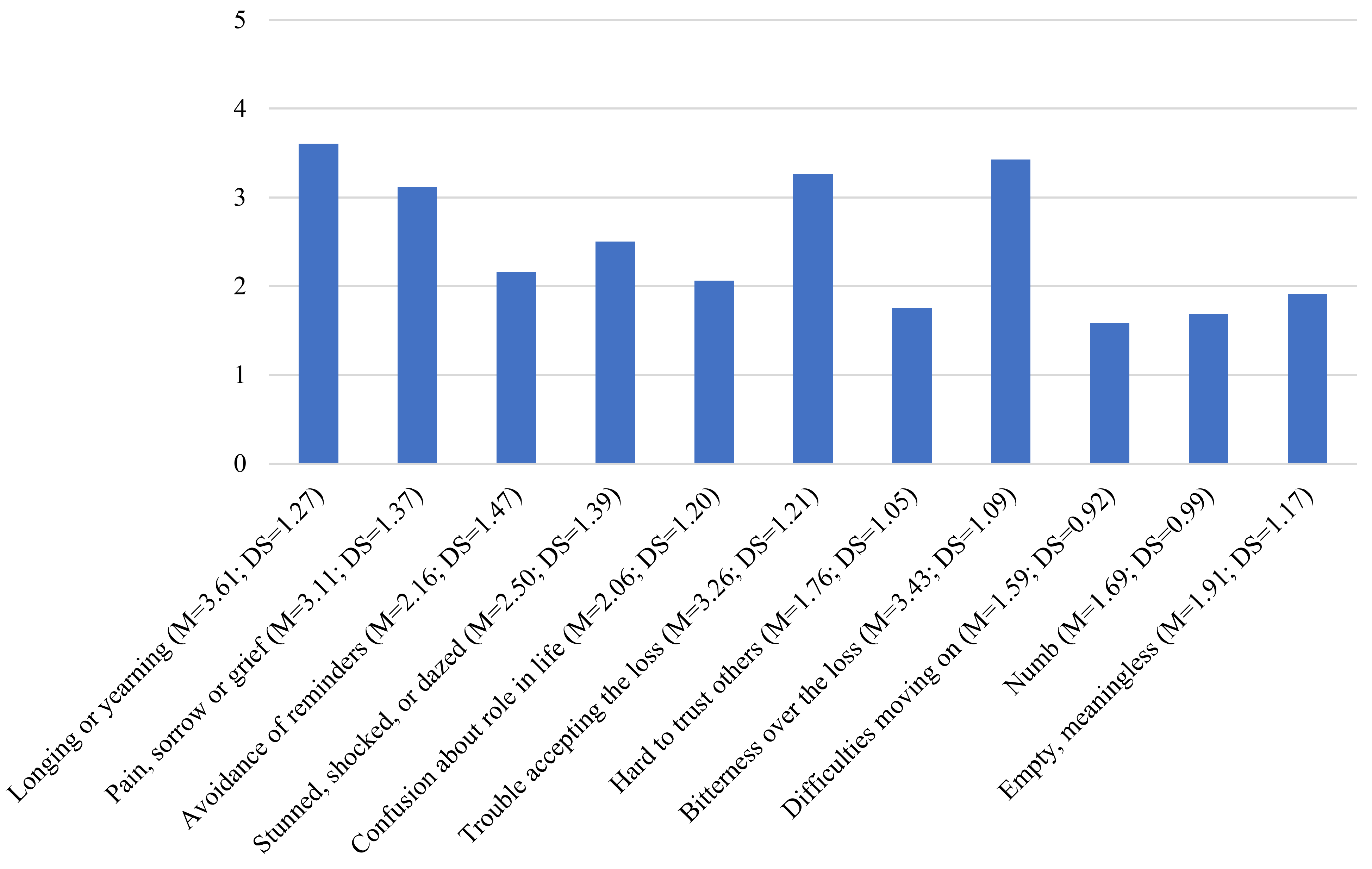
3. Results
3.1. Characteristics of the Sample
3.2. Prevalence of PGD, Depression, and Anxiety
3.3. Comorbidity of PGD, Depression, and Anxiety
3.4. Discriminant Validity of HADS-A, HADS-D, and HADS-TOT Scores
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Holmes, T.H.; Rahe, R.H. The social readjustment rating scale. J. Psychosom. Res. 1967, 11, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Mancini, A.D.; Bonanno, G.A. Predictors and Parameters of Resilience to Loss: Toward an Individual Differences Model. J. Pers. 2009, 77, 1805–1832. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lundorff, M.; Holmgren, H.; Zachariae, R.; Farver-Vestergaard, I.; O’Connor, M. Prevalence of prolonged grief disorder in adult bereavement: A systematic review and meta-analysis. J. Affect. Disord. 2017, 212, 138–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Prigerson, H.G.; Horowitz, M.J.; Jacobs, S.C.; Parkes, C.M.; Aslan, M.; Goodkin, K.; Raphael, B.; Marwit, S.J.; Wortman, C.; Neimeyer, R.A.; et al. Prolonged Grief Disorder: Psychometric Validation of Criteria Proposed for DSM-V and ICD-11. PLoS Med. 2009, 6, e1000121. [Google Scholar] [CrossRef] [Green Version]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; Text Rev.; American Psychiatric Association: Arlington, VA, USA, 2022. [Google Scholar] [CrossRef]
- Zisook, S.; Pies, R.; Simon, N.; Lebowitz, B.; Madowitz, J.; Tal-Young, I.; Shear, M.K. Bereavement, Complicated Grief and DSM Part 1: Depression. J. Clin. Psychiatry 2010, 71, 955. [Google Scholar] [CrossRef] [Green Version]
- Shear, M.K.; Simon, N.; Wall, M.; Zisook, S.; Neimeyer, R.; Duan, N.; Reynolds, C.; Lebowitz, B.; Sung, S.; Ghesquiere, A.; et al. Complicated grief and related bereavement issues for DSM-5. Depress. Anxiety 2011, 28, 103–117. [Google Scholar] [CrossRef] [Green Version]
- Cozza, S.J.; Fisher, J.E.; Mauro, C.; Zhou, J.; Ortiz, C.D.; Skritskaya, N.; Wall, M.M.; Fullerton, C.S.; Ursano, R.J.; Shear, M.K. Performance of DSM-5 Persistent Complex Bereavement Disorder Criteria in a Community Sample of Bereaved Military Family Members. Am. J. Psychiatry 2016, 173, 919–929. [Google Scholar] [CrossRef]
- Guldin, M.B.; Vedsted, P.; Zachariae, R.; Olesen, F.; Jensen, A.B. Complicated grief and need for professional support in family caregivers of cancer patients in palliative care: A longitudinal cohort study. Support Care Cancer 2012, 20, 1679–1685. [Google Scholar] [CrossRef]
- Italian Association of Medical Oncology. I Numeri del Cancro in Italia 2021. 2021. Available online: https://www.aiom.it/wpcontent/uploads/2021/10/2021_NumeriCancro_web.pdf (accessed on 18 October 2022).
- Zordan, R.; Bell, M.; Price, M.; Remedios, C.; Lobb, E.; Hall, C.; Hudson, P. Long-term prevalence and predictors of prolonged grief disorder amongst bereaved cancer caregivers: A cohort study. Palliat. Support Care 2019, 17, 507–514. [Google Scholar] [CrossRef] [Green Version]
- Hudson, P.; Hall, C.; Boughey, A.; Roulston, A. Bereavement support standards and bereavement care pathway for quality palliative care. Palliat. Support Care 2018, 16, 375–387. [Google Scholar] [CrossRef] [Green Version]
- He, L.; Tang, S.; Yu, W.; Xu, W.; Xie, Q.; Wang, J. The prevalence, comorbidity and risks of prolonged grief disorder among bereaved Chinese adults. Psychiatry Res. 2014, 219, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Allen, J.Y.; Haley, W.E.; Small, B.J.; Schonwetter, R.S.; McMillan, S.C. Bereavement among hospice caregivers of cancer patients one year following loss: Predictors of grief, complicated grief, and symptoms of depression. J. Palliat. Med. 2013, 16, 745–751. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coelho, A.; Delalibera, M.; Barbosa, A.; Lawlor, P. Prolonged Grief in Palliative Family Caregivers: A Pilot Study in a Portuguese Sample. Omega 2015, 72, 151–164. [Google Scholar] [CrossRef] [PubMed]
- Tsai, W.I.; Prigerson, H.G.; Li, C.Y.; Chou, W.C.; Kuo, S.C.; Tang, S.T. Longitudinal changes and predictors of prolonged grief for bereaved family caregivers over the first 2 years after the terminally ill cancer patient’s death. Palliat. Med. 2016, 30, 495–503. [Google Scholar] [CrossRef]
- Pearce, C.; Honey, J.R.; Lovick, R.; Creamer, N.Z.; Henry, C.; Langford, A.; Stobert, M.; Barclay, S. ‘A silent epidemic of grief’: A survey of bereavement care provision in the UK and Ireland during the COVID-19 pandemic. BMJ Open 2021, 11, e046872. [Google Scholar] [CrossRef]
- Lenzo, V.; Quattropani, M.C.; Musetti, A.; Zenesini, C.; Freda, M.F.; Lemmo, D.; Vegni, E.; Borghi, L.; Plazzi, G.; Castelnuovo, G.; et al. Resilience Contributes to Low Emotional Impact of the COVID-19 Outbreak Among the General Population in Italy. Front. Psychol. 2020, 11, 576485. [Google Scholar] [CrossRef]
- Lenzo, V.; Quattropani, M.C.; Sardella, A.; Martino, G.; Bonanno, G.A. Depression, Anxiety, and Stress Among Healthcare Workers During the COVID-19 Outbreak and Relationships with Expressive Flexibility and Context Sensitivity. Front. Psychol. 2021, 12, 623033. [Google Scholar] [CrossRef]
- Lenzo, V.; Sardella, A.; Musetti, A.; Freda, M.F.; Lemmo, D.; Vegni, E.; Borghi, L.; Plazzi, G.; Palagini, L.; Castelnuovo, G.; et al. The Relationship Between Resilience and Sleep Quality During the Second Wave of the COVID-19 Pandemic: A Longitudinal Study. Nat. Sci. Sleep 2022, 14, 41. [Google Scholar] [CrossRef]
- Sardella, A.; Lenzo, V.; Basile, G.; Musetti, A.; Franceschini, C.; Quattropani, M.C. Gender and Psychosocial Differences in Psychological Resilience among a Community of Older Adults during the COVID-19 Pandemic. J. Pers. Med. 2022, 12, 1414. [Google Scholar] [CrossRef]
- Wallace, C.L.; Wladkowski, S.P.; Gibson, A.; White, P. Grief during the COVID-19 pandemic: Considerations for palliative care providers. J. Pain Symptom. Manag. 2020, 60, e70–e76. [Google Scholar] [CrossRef]
- Gesi, C.; Carmassi, C.; Cerveri, G.; Carpita, B.; Cremone, I.M.; Dell’Osso, L. Complicated Grief: What to Expect After the Coronavirus Pandemic. Front. Psychiatry 2020, 11, 489. [Google Scholar] [CrossRef] [PubMed]
- Dettmann, L.M.; Adams, S.; Taylor, G. Investigating the prevalence of anxiety and depression during the first COVID-19 lockdown in the United Kingdom: Systematic review and meta-analyses. Br. J. Clin. Psychol. 2022, 61, 757–780. [Google Scholar] [CrossRef]
- Jho, H.J.; Choi, J.Y.; Kwak, K.S.; Chang, Y.J.; Ahn, E.M.; Park, E.J.; Paek, S.J.; Kim, K.M.; Kim, S.H. Prevalence and associated factors of anxiety and depressive symptoms among bereaved family members of cancer patients in Korea: A nation-wide cross-sectional study. Medicine 2016, 95, e3716. [Google Scholar] [CrossRef] [PubMed]
- Simon, N.M.; Shear, K.M.; Thompson, E.H.; Zalta, A.K.; Perlman, C.; Reynolds, C.F.; Frank, E.; Melhem, N.M.; Silowash, R. The prevalence and correlates of psychiatric comorbidity in individuals with complicated grief. Compr. Psychiatry 2007, 48, 395–399. [Google Scholar] [CrossRef] [PubMed]
- Maglia, M.; Tortorici, J.; Lenzo, V.; Aiello, D.; Alì, M.; Aiello, R.; Caponnetto, P. The network that unites a qualitative study on clinical psychological intervention for women with a history of breast cancer and chronic pain. Eur. J. Investig. Health Psychol. Educ. 2022, 12, 619–630. [Google Scholar] [CrossRef] [PubMed]
- Lenzo, V.; Sardella, A.; Musetti, A.; Petralia, M.C.; Grado, I.; Quattropani, M.C. Failures in Reflective Functioning and Reported Symptoms of Anxiety and Depression in Bereaved Individuals: A Study on a Sample of Family Caregivers of Palliative Care Patients. Int. J. Environ. Res. Public Health 2022, 19, 11930. [Google Scholar] [CrossRef]
- World Health Organization. ICD-11. 6B42 Prolonged Grief Disorder. Available online: http://id.who.int/icd/entity/1183832314 (accessed on 15 February 2023).
- De Luca, M.L.; Tineri, M.; Zaccarello, G.; Grossi, G.; Altomonte, A.; Slavic, E.; Palummieri, A.; Greco, R. Adattamento e validazione del questionario “PG-13” Prolonged Grief nel contesto italiano. Riv. It. Cur. Pall. 2015, 17, 84–92. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The Hospital Anxiety and Depression Scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [Green Version]
- Zigmond, A.S.; Snaith, R.P. (Eds.) The Hospital Anxiety and Depression Scale with the Irritability Depression-Anxiety Scale and the Leads Situational Anxiety Scale Manual; GL Assessment Ltd.: London, UK, 1994. [Google Scholar]
- Brennan, C.; Worrall-Davies, A.; McMillan, D.; Gilbody, S.; House, A. The Hospital Anxiety and Depression Scale: A diagnostic meta-analysis of case-finding ability. J. Psychosom. Res. 2010, 69, 371–378. [Google Scholar] [CrossRef]
- Wu, Y.; Levis, B.; Sun, Y.; He, C.; Krishnan, A.; Neupane, D.; Bhandari, P.M.; Negeri, Z.; Benedetti, A.; Thombs, B.D. Accuracy of the Hospital Anxiety and Depression Scale Depression subscale (HADS-D) to screen for major depression: Systematic review and individual participant data meta-analysis. BMJ 2021, 373, n972. [Google Scholar] [CrossRef]
- Denning, M.; Goh, E.T.; Tan, B.; Kanneganti, A.; Almonte, M.; Scott, A.; Martin, G.; Clarke, J.; Sounderajah, V.; Markar, S.; et al. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the COVID-19 pandemic: A multinational cross-sectional study. PLoS ONE 2021, 16, e0238666. [Google Scholar] [CrossRef] [PubMed]
- Iani, L.; Lauriola, M.; Costantini, M. A confirmatory bifactor analysis of the hospital anxiety and depression scale in an Italian community sample. Health Qual. Life Outcomes 2014, 12, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mandrekar, J.N. Receiver operating characteristic curve in diagnostic test assessment. J. Thorac. Oncol. 2010, 5, 1315–1316. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Youden, W.J. Index for rating diagnostic tests. Cancer 1950, 3, 32–35. [Google Scholar] [CrossRef]
- Bonanno, G.A. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? Am. Psychol. 2004, 59, 20–28. [Google Scholar] [CrossRef] [Green Version]
- Lenzo, V.; Sardella, A.; Grazia, V.; Corsano, P.; Quattropani, M.C.; Franceschini, C.; Musetti, A. Fear of COVID-19 and future orientation: Different profiles in dealing with the pandemic and associations with loneliness and posttraumatic growth. Psychol. Trauma 2022. [Google Scholar] [CrossRef]
- Boelen, P.A.; Prigerson, H.G. The influence of symptoms of prolonged grief disorder, depression, and anxiety on quality of life among bereaved adults. Eur. Arch. Psychiatry Clin. Neurosci. 2007, 257, 444–452. [Google Scholar] [CrossRef]
- Stroebe, M.; Schut, H.; Stroebe, W. Health outcomes of bereavement. Lancet 2007, 370, 1960–1973. [Google Scholar] [CrossRef]
- Lingiardi, V.; McWilliams, N. (Eds.) Psychodynamic Diagnostic Manual: PDM-2; Guilford Publications: New York, NY, USA, 2017. [Google Scholar]
- Treml, J.; Kaiser, J.; Plexnies, A.; Kersting, A. Assessing prolonged grief disorder: A systematic review of assessment instruments. J. Affect. Disord. 2020, 274, 420–434. [Google Scholar] [CrossRef]
- Prigerson, H.G.; Boelen, P.A.; Xu, J.; Smith, K.V.; Maciejewski, P.K. Validation of the new DSM-5-TR criteria for prolonged grief disorder and the PG-13-Revised (PG-13-R) scale. World Psychiatry 2021, 20, 96–106. [Google Scholar] [CrossRef]
- Sardella, A.; Lenzo, V.; Basile, G.; Martino, G.; Quattropani, M.C. Emotion regulation strategies and difficulties in older adults: A systematic review. Clin. Gerontol. 2022, 1–22. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | n (%) | M | SD |
|---|---|---|---|
| Age (in years) | 43.50 | 14.04 | |
| Gender | |||
| Male | 36 (22.9) | ||
| Female | 121 (77.1) | ||
| Education | |||
| Primary or middle school diploma | 34 (21.7) | ||
| High school diploma | 66 (42) | ||
| Graduate | 57 (36.3) | ||
| Relation with the deceased loved one | |||
| Son or daughter | 82 (52.3) | ||
| Nephew | 32 (20.4) | ||
| Spouse | 15 (9.5) | ||
| Other (for example, brother-in-law) | 28 (17.8) | ||
| Main caregiver | |||
| Yes | 90 (57.3) | ||
| No | 67 (42.7) | ||
| Work before the loss | |||
| Yes | 76 (48.4) | ||
| No | 81 (51.6) | ||
| Work after the loss | |||
| Yes | 63 (40.1) | ||
| No | 94 (59.9) | ||
| Time since the loss (years) | 3.59 | 4.92 |
| I.D. | Age | Gender | Education | Kinship | Main Caregiver | Work before the Loss | Work after the Loss | Time | PG-13 | HADS-A | HADS-D | HADS-TOT |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 73 | F | Middle school | Spouse | Yes | No | No | 1 | 39 | 14 | 13 | 27 |
| 2 | 51 | F | High school | Daughter | Yes | No | Yes | 1 | 42 | 11 | 8 | 19 |
| 3 | 24 | F | High school | Daughter | Yes | Yes | Yes | 1 | 46 | 7 | 12 | 19 |
| 4 | 35 | F | Graduate | Daughter | Yes | No | No | 1 | 53 | 14 | 14 | 28 |
| 5 | 75 | F | Middle school | Spouse | No | No | No | 2 | 51 | 19 | 18 | 37 |
| 6 | 49 | F | Middle school | Daughter | Yes | No | Yes | 2 | 48 | 13 | 15 | 28 |
| 7 | 57 | F | High school | Daughter | Yes | Yes | Yes | 2 | 40 | 7 | 7 | 14 |
| Variable | Min | Max | M | SD | 1. 1. PG-13 | 2. HADS-A | 3. HADS-D |
|---|---|---|---|---|---|---|---|
| 1. PG-13 | 11 | 53 | 27.08 | 8.84 | |||
| 2. HADS-A | 0 | 19 | 7.34 | 4.11 | 0.37 ** | ||
| 3. HADS-D | 0 | 18 | 6.22 | 3.56 | 0.54 ** | 0.61 ** | |
| 4. HADS-TOT | 1 | 37 | 13.57 | 6.74 | 0.50 ** | 0.91 ** | 0.89 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sardella, A.; Musetti, A.; Caponnetto, P.; Quattropani, M.C.; Lenzo, V. Prolonged Grief Disorder and Symptoms of Anxiety and Depression among Bereaved Family Caregivers in the Context of Palliative Home Care. Eur. J. Investig. Health Psychol. Educ. 2023, 13, 490-500. https://doi.org/10.3390/ejihpe13020037
Sardella A, Musetti A, Caponnetto P, Quattropani MC, Lenzo V. Prolonged Grief Disorder and Symptoms of Anxiety and Depression among Bereaved Family Caregivers in the Context of Palliative Home Care. European Journal of Investigation in Health, Psychology and Education. 2023; 13(2):490-500. https://doi.org/10.3390/ejihpe13020037
Chicago/Turabian StyleSardella, Alberto, Alessandro Musetti, Pasquale Caponnetto, Maria C. Quattropani, and Vittorio Lenzo. 2023. "Prolonged Grief Disorder and Symptoms of Anxiety and Depression among Bereaved Family Caregivers in the Context of Palliative Home Care" European Journal of Investigation in Health, Psychology and Education 13, no. 2: 490-500. https://doi.org/10.3390/ejihpe13020037
APA StyleSardella, A., Musetti, A., Caponnetto, P., Quattropani, M. C., & Lenzo, V. (2023). Prolonged Grief Disorder and Symptoms of Anxiety and Depression among Bereaved Family Caregivers in the Context of Palliative Home Care. European Journal of Investigation in Health, Psychology and Education, 13(2), 490-500. https://doi.org/10.3390/ejihpe13020037










