Abstract
Achillea cucullata is a perennial herbaceous plant that has a long history of medical use in many cultures. The present research focuses on the biological activity and therapeutic potential of A. cucullata, namely its antibacterial and anticancer properties. While previous studies have shed light on the cytotoxic and antibacterial capabilities of Achillea cucullata aerial parts, there is still a considerable gap in knowledge concerning the anticancer potential of leaf and flower extracts. A. cucullata’s leaves and flowers were extracted using methanol. The total phenolic and flavonoid contents were evaluated. The antioxidant, cytotoxic, and antibacterial properties were evaluated against both Gram-positive and Gram-negative bacteria. The Gas Chromatography–Mass Spectrometry (GC–MS) analysis of A. cucullata leaf and flower extracts showed numerous amounts of bioactive components, including carvacrol, a TBDMS derivative; 2-Myristynoyl-glycinamide, acetylaminobenzothiazol-2-yl)-2-(adamantan-1-yl); Isolongifolol; (3E,10Z)-Oxacyclotrideca-3,10-diene-2,7-dione; and 3-Heptanone, 5-hydroxy-1,7-diphenyl. The extract has a high level of phenols and flavonoids. Cytotoxicity studies found that A. cucullata leaves and flowers had dose-dependent toxicity against MCF-7 and HepG2 cancer cell lines, with flowers being more effective. Apoptotic genes (caspase-3, 8, 9, and Bax) were upregulated in treated MCF-7 and HepG2 cells, whereas anti-apoptotic genes (Bcl-xL and Bcl-2) were reduced. Antibacterial screening revealed significant activity against both Gram-positive and Gram-negative pathogens. Overall, the research highlights the varied therapeutic potentials of A. cucullata, adding to the knowledge of plant-derived extracts in lowering disease risks. Future research should concentrate on in vivo studies to assess the effectiveness and safety of these substances.
1. Introduction
Compounds derived from medicinal plants provide a wide range of chemical varieties, which is essential for the investigation and development of modern medical treatments [1]. These metabolites are very beneficial to human health and well-being since they have a variety of biological functions, including antibacterial, antioxidant, and anticancer effects [2].
Saudi Arabia has abundant aromatic and therapeutic plants because of its diverse geographical terrain and arid climate; around 30% of these species are rare [3]. Many regions of Saudi Arabia still practice folk medicine, which uses different plant components to treat common diseases [3]. Achillea is a well-known member of the Asteraceae family and is widely distributed in North Africa, Asia, and Southeast Europe. It contains over 100 species of wild-growing plants and has been used since ancient times in the treatment of various diseases and ailments such as stomach pain and spasms, rheumatism, hemorrhoids, pneumonia, allergic rhinitis, and inflammation [4,5,6]. In Saudi Arabia, the Achillea plant is extensively found in the country’s northern areas, namely in the provinces of Tabuk and Arar [7]. Alkamide, phenolic acids, flavonoids, lignans, terpenes, and many other bioactive metabolites were identified from several Achillea plants. Among Achillea species, A. millefolium extracts are the most potent antimicrobial ingredients that have been proven to inhibit the pathogens responsible for skin infections, including Staphylococcus aureus, and also suppress the growth of Pseudomonas aeruginosa [8]. Furthermore, it has been shown that the essential oils derived from the flowers and leaves of A. ageratum have antibacterial properties against S. aureus and Candida albicans strains [9].
As reported in previous studies, the essential oil of Achillea cucullata (Hausskn) Bornm. contains camphor, 1,8-cineole, and isoborneol [10]. The chemical components of A. cucullata’s essential oil were recently documented [11]. However, despite extensive studies on the biological activity of the Achillea species, the biological activity of the A. cucullata extract was not well documented. An earlier investigation found that the methanol extract from A. cucullata’s aerial portions had high antibacterial, anticholinesterase, antidiabetic, and antioxidant effects [12].
Remarkably, the antibacterial, antioxidant, and anticancer activities of A. cucullata leaf and flower extracts have not been well studied. This highlights the potential of A. cucullata in medical research and aligns with the growing interest in plant-based natural products in healthcare. Therefore, the primary objectives of the current study were fourfold: (i) to assess the chemical composition of methanol extracts derived from the leaves and flowers of A. cucullata using the Gas Chromatography–Mass Spectrometry (GC–MS) technique; (ii) to investigate the in vitro anticancer potency of leaves and flowers of A. cucullata in MCF-7 (breast) and HepG2 (liver) cells; and (iii) to dissect the underlying mechanisms using qPCR-based mRNA expression profiling of selected pro- and anti-apoptosis marker genes; and (iv) to determine the antioxidant and antimicrobial activities.
2. Materials and Methods
2.1. Preparation of Plant Extract
The dried leaves and flowers of A. cucullata extracts were purchased at the Riyadh market in Saudi Arabia. No voucher herbarium deposit is required for the plant. Collection of plant materials was conducted following the guidelines of the International Union for Conservation of Nature (IUCN) policies research involving species at risk of extinction and the Convention on the Trade in Endangered Species of Wild Fauna and Flora. Plant identification was performed by Professor Dr. Mohammed Fasil of King Saud University’s Department of Botany and Microbiology at the College of Science in Riyadh, Saudi Arabia. Following the method outlined by [12], with slight modifications, one hundred grams of leaves and flowers of A. cucullata extracts were macerated for 48 h with sporadic shaking in 1000 milliliters of 80% methanol. Subsequently, the mixture was passed through Whatman No. 1 filter paper, evaporated at 40 °C using a rotary evaporator, and refrigerated at −20 °C to facilitate future usage.
2.2. Determination of Phytochemicals of Extract
The 7890B GC–MS system with a nonpolar DB-5 MS capillary column (30 m length × 0.25 mm internal diameter, phase thickness 0.25 μm) from Agilent Technologies (Santa Clara, CA, USA) was used to analyze the volatile components of methanol extracts from both the leaves and flowers of A. cucullata plants. The autosampler injection system was used to add 0.9 µL of the watery extract that had been diluted with methanol (1 to 9 volume ratio). The identification of the sample components was achieved using GC coupled with a mass-selective detector. It took 73 min of measurement time and a flow rate of 1 mL/min of helium. The oven temperature ranged from 50 to 250 °C, and the split mode ratio was 50. There was a liquid delay of 2 min, an acquisition scan type, a mass range of 40 to 500 g/mol, a scan speed of 1.56 atomic mass units (amu), and the MS source temperature was set to 230 °C. The National Institute of Standards and Technology (NIST) and Willey libraries were the foundation for the component identification process. The components with a matching factor of more than 90% were identified by comparing the components with those located in the computer libraries (Willey and NIST) attached to the GC–MS device.
2.3. Analysis of Total Phenolic Content (TPC) and Total Flavonoid Content (TFC)
The Folin–Ciocalteu method from Wolfe and Liu (2003) [13] with minor changes was used with only minor changes to find the TPC in the extracts. Extracts were diluted to the right concentration, and 0.25 mL portions were mixed with 1.25 mL Folin–Ciocalteu reagent (a mixture of phosphomolybdate and phosphotungstate) which had been ten times diluted with distilled water) and 7.5% NaHCO3. After leaving this mix to sit for 15 min at 45 °C, the absorption was recorded at 765 nm using a spectrophotometer (U2001 UV–vis Spectrophotometer, Hitachi, Japan). Between 20 and 200 µg/mL of gallic acid was used to create a standard curve. The coefficient of determination (R2) of the calibration curves were used to evaluate the linearity of the curve. TPC is expressed as mg gallic acid equivalent per gram of extract ((GAE)/g).
The aluminum chloride (AlCl3) colorimetric method was used to measure the amount of TFC, as described by [14] with minor modifications. In brief, 1.5 mL of methanol was mixed with 0.5 mL (20 mg/mL) of each solution extract. The samples were then mixed with 1.0 M sodium acetate and 0.1 mL of 10% AlCl3. After 2.8 mL of purified water was added, the solutions were left to sit at room temperature. After 30 min, a Hitachi U2001 UV-vis Spectrophotometer (U2001 UV–vis Spectrophotometer, Hitachi, Japan) was used to measure the absorption of the reaction solutions at 415 nm. The same method was used to make the calibration curve for the solutions of quercetin. Vitamin C was used as the positive control. The TFC was presented as quercetin equivalents (QE)/g per gram of extract. Results were shown as the mean ± SD for each experiment that was performed three times.
2.4. Cell Culture and Cytotoxicity Analysis
Breast cancer (MCF-7) (ATCC HTB-22) and human hepatoma HepG2 (ATCC HB-8065) cell lines were used in this study because they can be used as a functional in vitro model system for testing the lethal qualities of different plant extracts [15,16]. Dulbecco’s Modified Eagle’s Medium with 10% fetal bovine serum, 2 mM glutamine, and a 1% antibiotic solution (100 U/mL of penicillin and 100 μg/mL of streptomycin) was used to grow the cells. The cells were then kept at 37 °C in an atmosphere with 5% CO2 and 95% air. The 3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyl-2H tetrazolium bromide (MTT) assay Report Word (Life Technologies, Eugene, OR, USA) was used to investigate the cytotoxicity of methanol extracts from both the leaves and flowers of A. cucullata on MCF-7 and HepG2 cells. Briefly, 1 × 104 cells were put into each well of a 96-well Corning Costar plate (Corning, Lowell, NY, USA). After that, they were treated with different amounts of A. cucullata flower and leaf extracts (0–400 μg/mL) with cisplatin (30 µg/mL) as the positive control at 37 °C for 48 h while the cells were 80–90% confluency. Ten microliters of MTT (5 mg/mL phosphate buffer salt) solution were added to each well. The plate was then left to sit in the dark for two hours. After that, 100 microliters of dimethyl sulfoxide (DMSO) were added to break up the MTT. A microplate spectrophotometer (BioTek Laboratories, LL, Shoreline, WA, USA) was used to measure the absorbance of each well at 570 nm. 100% of the cells in the negative control, which is the optical density of formazan generated in untreated cells, are viable. To analyze the data and obtain the IC50 value, the mean value was considered [17]. The Virology Research Laboratory (VRG) group, College of Science, King Saud University, Saudi Arabia provided the cell lines. All cell lines were maintained at 37 °C and were mycoplasma-free (LookOut® Mycoplasma qPCR Detection Kitm, Merck, Darmstadt, Germany).
2.5. Expression of Genes
Using rRT-PCR, apoptosis genes (caspase-3, 8, 9, and Bax) and anti-apoptotic genes (Bcl-xL and Bcl-2) were determined. Cells (1 × 104 cells) were grown in a 96-well plate in DMEM with 10% FBS for 24 h at 37 °C. Cells were given the IC50 values provided (100 µL) of each extract for 48 h. After 0.25% trypsin was added to the wells, they were spun at 12,000 rpm for 8 min. The last pellet was mixed with a buffer, and rRT-PCR processing was performed according to the steps we laid out in our most recent work [18].
2.6. Screening for Antibacterial Activity
2.6.1. Disk Diffusion Method
The leaves and flower extracts of A. cucullata were tested for their ability to kill certain Gram-positive and Gram-negative bacteria using the disk-diffusion susceptibility method, following previously described steps [19] with slight modifications. The chosen bacteria represent the Gram-positive strains Staphylococcus aureus (ATCC-29213), Staphylococcus epidermidis (MTCC 12228), and Enterococcus faecalis (ATCC-29212), as well as three Gram-negative strains: Escherichia coli (ATCC-25922), Klebsiella pneumoniae (MTCC-13883), and Pseudomonas aeruginosa (MTCC-27853). These bacteria were swabbed (0.1 mL, 1 × 106 CFU/mL saline) on Mueller Hinton Agar (HMA) medium at 37 °C for 24 h. Ciprofloxacin was used as the positive reference at a concentration of 25 μg/mL. After that, 30 μL of leaves and flower extracts of A. cucullata with different concentrations (500, 1000, and 1500 μg/mL) were put on clean paper disks and left to sit at 37 °C for 24 h. Zones of inhibition diameters were measured in millimeters (mm) [20].
2.6.2. Analysis of Minimum Inhibitory Concentration (MIC) and Minimum Bactericidal Concentration (MBC)
The MIC and MBC of the flower and leaf extracts of A. cucullata were evaluated against certain Gram-positive and Gram-negative bacteria using the 2,3,5-triphenyl tetrazolium chloride (TTC) method, as described by Basri and Sandra (2016) [21], with some changes. TTC staining, a commonly used tetrazolium salt in MIC determination, is a technique that differentiates the mitochondrial activity of cells by observing color changes. Specifically, colorless TTC becomes red when subjected to reducing conditions. This test measures the cellular mitochondrial activity, specifically the contribution of enzymes in the electron transport system to TTC reduction. The red color formation indicates cell viability. This indicator distinguishes between metabolically active and non-active cells based on the enzymatic reduction of 2,3,5-triphenyl tetrazolium (colorless) to 1,3,5-triphenyl formazan (reddish color) in living cells [22,23].
Briefly, various concentrations of the compounds under investigation were diluted twice (1.95 to 800 μg/mL) and added to 100 μL of Mueller Hinton Broth (MHB) on a 96-well plate. Subsequently, 10 µL of bacterial solution was introduced, resulting in a total of 5 × 106 CFU/mL of bacteria in each well. The positive control included 25 μg/mL of ciprofloxacin, whereas the negative control consisted of 0.1% DMSO with MHB. Following a 24 h incubation period at 37 °C, the plates were visually evaluated for bacterial growth. After treatment, each well was filled with 2 mg/mL of TTC (Sigma-Aldrich LTD, Ayrshire, UK) working solution in PBS, and the mixture was let to settle at 37 °C for 20 min. Wells with a colorless solution were considered negative for bacterial growth, but those with a pink appearance similar to the positive control were considered positive for bacterial growth. The MIC in three duplicates was found to be the one that inhibited bacterial growth after the growth of the bacteria. The MBC was the lowest concentration at which an agar subculture could be observed [24].
2.7. Statistical Analysis
The one-way ANOVA menu in SPSS version 28 was used to examine the data, and a significant level was found. It is important to remember that every experiment was carried out in triplicate, and the analysis was performed using the mean ± SD. These statistical tests were used in all sections except the GC–MS system. A “p” value < 0.05 criterion was used to assess statistical significance.
3. Results
3.1. GC–MS Analysis of A. cucullata Flower and Leaf Extracts
The phytochemical components isolated from the flower and leaf extracts of A. cucullata were analyzed using GC–MS. The molecular formula (MF), concentration (peak area percentage), retention time (RT), and concentration of the active principles are shown in (Table 1 and Figure 1). Based on the results, twenty-five distinct phytochemical compounds were discovered. The primary phytochemical components in the leaf extract were determined to be carvacrol, a tert-butyldimethylsilyl (TBDMS) derivative; 2-Myristynoyl-glycinamide; acetylaminobenzothiazol-2-yl)-2-(adamantan-1-yl), while the primary phytochemical components in the the flower extract were Isolongifolol; (3E,10Z)-Oxacyclotrideca-3,10-diene-2,7-dione; and 3-Heptanone, 5-hydroxy-1,7-diphenyl- (10.47%) (Table 2 and Figure 2).

Table 1.
GC–MS analysis of phytochemical compounds identified from the A. cucullata leaf extract.
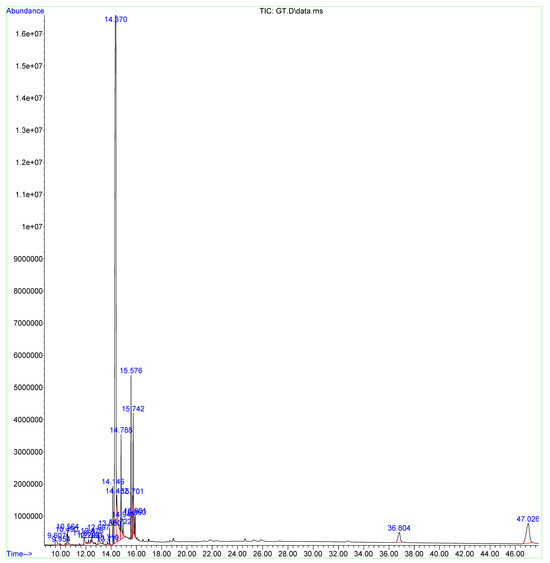
Figure 1.
GC–MS chromatograms of the A. cucullata leaf extract. The GC–MS apparatus was set for 73 min, and methanol extract was used for the study. Every detected peak in the spectrum designates a recognized chemical, and the existence of a sizable peak denotes the extract’s major component.

Table 2.
GC–MS analysis of phytochemical compounds identified from the A. cucullata flower extract.
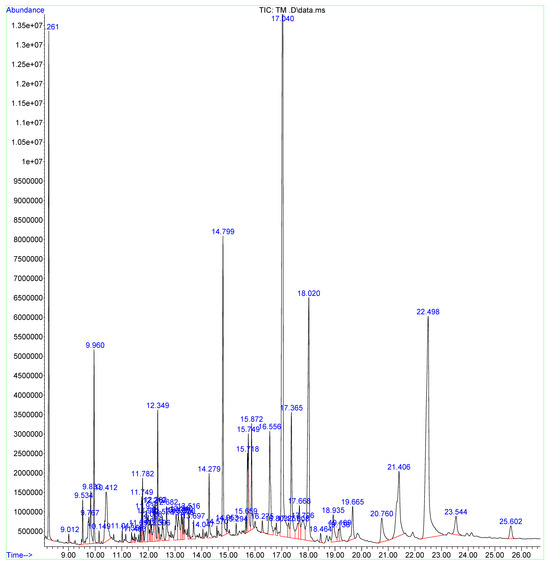
Figure 2.
GC–MS chromatograms of the A. cucullata flower extract. The GC–MS apparatus was set for 73 min, and methanol extract was used for the study. Every detected peak in the spectrum designates a recognized chemical, and the existence of a sizable peak denotes the extract’s major component.
3.2. TPC and TFC of A. cucullata Flower and Leaf Extracts
The TPC and TFC of methanol extracts derived from the leaves and flowers of A. cucullata were measured.
The yield of methanol extracts from the leaves and flowers of A. cucullata was 17% and 19%, respectively, and the results of the Folin–Ciocalteu technique showed that the flower extract had a higher TPC (89.54 ± 1.83 mg GAE/g dry weight of the dry extract; R2 = 0.994) than the leaf extracts (57.34 ± 2.84 mg GAE/g dry weight of the dry extract; R2 = 0.989). On the other hand, the aluminum chloride assay produced TFC values for the flowers (58 ± 2.57 mg QE/g dry weight of the dry extract; R2 = 0.965) and leaves (49 ± 2.47 mg QE/g dry weight of the dry extract; R2 = 0.979).
3.3. Antioxidant Activity
The two distinct techniques of DPPH and ABTS were used to assess the antioxidant potential of the phytochemicals extracted from the leaves and flowers of A. cucullata. The findings were contrasted with conventional antioxidants (vitamin C), as seen in Figure 3. Both the ABTS and DPPH techniques showed better antioxidant activity at higher extract concentrations. In the DPPH technique, the IC50 values of leaves and flowers were 50.19 ± 1.43 and 55.94 ± 2.14 μg/mL, respectively; in the ABTS assay, the IC50values were 66.21 ± 2.42 and 69.21 ± 3.14 μg/mL.
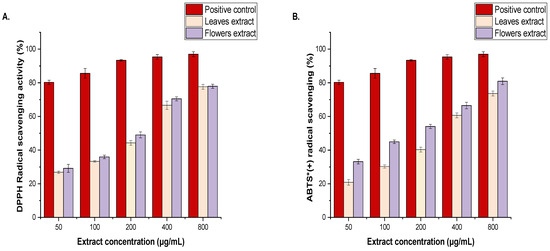
Figure 3.
Antioxidant activity of methanol extracts from the leaves and flowers of A. cucullata plants (A), DPPH reducing power, and (B), ABTS scavenging activity at various concentrations (0–400 μg/mL). The results are the mean values of three replicates. * (+) = radical cation.
3.4. Cell Cytotoxicity
MCF-7 and HepG2 cell proliferation were dose-dependently inhibited by methanol extracts derived from A. cucullata’s leaves and flowers (Figure 4). The extracts from the leaves and flowers of A. cucullata exhibited strong cytotoxic effects on MCF-7 and HepG2 cells compared to the positive control (cisplatin). Cell viability decreases with an increase in extract concentrations. It is interesting to note that the cell viability decreased after 50 μg/mL of A. cucullata leaf extract was added to the culture medium. The viability of MCF-7 was considerably decreased by leaf extract at a concentration of 100 μg/mL, with IC50 values of 65 ± 3.13 μg/mL for MCF-7 and 66.27 ± 2.49% and IC50 values of 45 ± 1.18 μg/mL for HepG2, respectively, compared to the non-treated cells (p = 0.05) (Figure 4A). Similar patterns were seen with the flower extract, which showed IC50 values for MCF-7 and HepG2 cells of 40.35 ± 2.46 and 32.43 ± 3.56 μg/mL, respectively (Figure 4B). Remarkably, against both cell lines, the flower extract exhibited a stronger cytotoxic impact than the leaf extract.
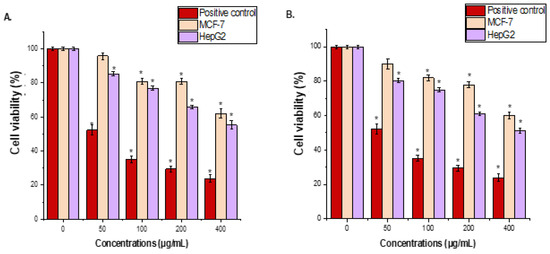
Figure 4.
The effect of A. cucullata’s leaves (A) and flowers (B) extracts on the viability of MCF-7 and HepG2 cells was determined using the MTT assay. Cells were treated with A. cucullata’s leaf and flower extracts (0–400 μg/mL) for 24 h. The mean ± SD is presented from three independent experiments (* = p < 0.05 compared to non-treated cells (negative control)).
3.5. Apoptotic Analysis
The effects of methanol extracts derived from A. cucullata’s leaves and flowers on apoptotic populations (caspase-3, 8, 9, and Bax) and anti-apoptotic genes (Bcl-xL and Bcl-2) activity are demonstrated in Figure 5. A noticeable increase in caspase-3, 8, 9, and Bax activity was observed when the MCF-7 and HepG2 cells were treated with 65 μg/mL of A. cucullata’s leaf and (40 μg/mL) of flower extract compared to the control cells (p < 0.05). Conversely, the expression of anti-apoptotic genes (Bcl-xL and Bcl-2) was lower than in the untreated control (p < 0.05).
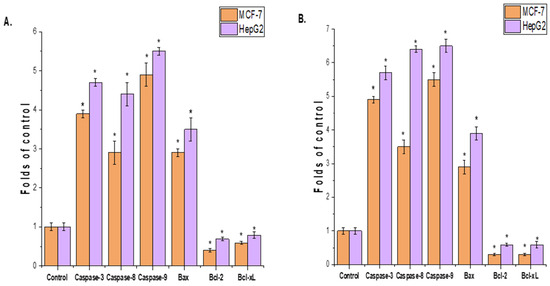
Figure 5.
Effect of methanol extracts of A. cucullata’s leaves (A) and flowers (B) on MCF-7 and HepG2 cell lines. Methanol extracts derived from A. cucullata’s leaves and flowers significantly stimulate the activity of a percentage of the apoptotic population (caspase-3, 8, 9, and Bax) after 24 h of incubation. The results are represented as the mean ± SD of three independent experiments (* = p < 0.05 compared to non-treated cells (control)).
3.6. Antibacterial Effects of Bioactive Compounds
A. cucullata flower and leaf extracts showed antibacterial activity against both Gram-positive and Gram-negative bacteria using the disk diffusion technique; MIC values for the flower extract varied from 3.12 ± 0.00 to 12.50 ± 0.00 μg/mL and for the leaf extract from 4.68 ± 2.21 to 25 ± 0.00 μg/mL (Table 3 and Table 4). A. cucullata flower extract was most effective against S. epidermidis (MTCC 12228) among all the strains, with a MIC of 12 ± 0.00 μg/mL. Conversely, weaker antibacterial effects were observed against E. faecalis (ATCC-29212) with MIC values of (25 ± 0.00 μg/mL) when tested with A. cucullata leaf extract.

Table 3.
The inhibitory zone (mm), MIC (μg/mL), and MBC (μg/mL) of A. cucullata leaf extract.

Table 4.
The inhibitory zone (mm), MIC (μg/mL), and MBC (μg/mL) of the A. cucullata flower extract.
4. Discussion
The use of traditional medicine in Saudi Arabia that is based on the pharmacological properties of medicinal plants is becoming more common. It shows a close relationship to natural remedies, health, food, and traditional healing practices that are accepted by a particular community [25]. An ethnopharmacological survey targeting the use of medicinal plants belonging to Saudi citizens showed that 80% of the interviewees have used herbal medicine for medications. It was reported in another study that 20% and 70% of the interviewed people use herbal medicine for chronic and acute conditions, respectively [26]. Our results show that the GC–MS analysis of A. cucullata leaf and flower extracts found several chemicals representing various bioactive chemical groups. A. cucullata leaf extract contains twenty-five distinct phytochemical compounds. It was found that carvacrol, a derivative of TBDMS, the main phytochemical component in the leaf extract, accounted for 68.16%. Next in order was 2-Myristynoyl-glycinamide (6.47%), as shown in Table 1 and Figure 1. The A. cucullata flower extract was found to contain thirty-four distinct phytochemical compounds. Of these, isolongifolol (24.35%) was the most abundant, followed by (3E,10Z)-Oxacyclotrideca-3,10-diene-2,7-dione (18.72%) (Table 2 and Figure 2). Many of these substances have already had their biological effects investigated, suggesting interesting directions for further study. A recent study revealed that (3E,10Z)-oxacyclotrideca-3,10-diene-2,7-dione induced structural alerts and in vitro mutagenicity, which might be due to the ester and phenol groups that exist in its chemical structure [27]. Previous research has shown that when head and neck squamous carcinoma cell lines were exposed to nutrient-deprived circumstances, several macrolide antibiotics exhibited notable and deadly effects [28]. In the methanolic leaf extract of Catharanthus ovalis, carvacrol and its TBDMS derivative were found to be 12.586% [29]. TBDMS derivative carvacrol is an aromatic monoterpenoid with potent biological activity, including significant antibacterial, immune response-modulating, antioxidant, anti-inflammatory, anti-cancer, and antidiabetic properties [30,31]. Research has shown that carvacrol may specifically target cancer cells by preventing them from proliferating, migrating, or invading via DNA damage, cell-cycle arrest, and changes in the expression levels of many protein markers linked to either intrinsic or extrinsic apoptosis [32]. 2-Myristynoyl-glycinamide was found to be 19.51%. 2-Myristynoyl-glycinamide was found to be 19.51% in the ethanol antioxidant activity and identification of components in the extract of the outer layer of sea bamboo (Isis hippuris) [33]. (-)-Isolongifolol is a sesquiterpene alcohol with a methanoazulene skeleton that was extracted from Ocimum gratissimum L. essential oil that was collected from plants growing in Bangladesh [34]. It has been reported that isolongifolol may be a promising anticarcinogenic drug that has cytotoxic action against a number of solid tumor cell lines [35]. These compounds indicate that A. cucullata has potential as a natural antibacterial and anticancer agent. They are found in the extracts of the plant. To fully comprehend these drugs’ modes of action and therapeutic potential, both alone and in combination, further study is required.
The free radical scavenging activity of the DPPH and ABTS techniques has been frequently utilized to assess the antioxidant activity of natural products from plant and microbial sources because of their rapid analysis time compared to other techniques [36]. The free radical scavenging activity of the methanolic extract from the leaves and flowers of A. cucullata was quantitatively determined using DPPH and ABTS assays (Figure 3). The scavenging ability of the samples showed a concentration-dependent activity profile. DPPH radical scavenging activity had an IC50 value of 50.19 ± 1.43 for leaf extract and 55.94 ± 2.14 μg/mL for flower extract. In the ABTS technique, the IC50 values of leaves and flowers were 66.21 ± 2.42 and 69.21 ± 3.14 μg/mL, respectively. A prior study on the aerial parts of A. cucullata indicated that an ethanolic extract from the herbs had an IC50 value of 132.55 ± 0.026 μg/mL [12].
Phenolic and flavonoid compounds originating from a wide range of plants have several medicinal applications, including cardiovascular protection, anti-inflammatory and anticancer, antioxidant, antibacterial, feeding repellants, and light screening. The antioxidant capabilities of flavonoids have received a lot of interest since they can both scavenge and inhibit the formation of free radicals [37]. The present investigation revealed that a high concentration of phenolic compounds was indicated by the TPC values of the A. cucullata flower extract (89.54 ± 1.83 mg GAE/g dry weight of the dry extract) and the leaf extracts (57.34 ± 2.84 mg GAE/g dry weight of the dry extract). These phenolic substances are necessary to prevent damage to cells and tissues caused by oxidative stress and to scavenge free radicals. Furthermore, the TFC of A. cucullata flower extract (58 ± 2.57 mg QE/g dry weight of the dry extract) and leaves (49 ± 2.47 mg QE/g dry weight of the dry extract). TPC was 53.807 ± 0.059 (mg GAE/g) and TFC was 21.372 ± 0.026 (mg QE/g) for the aerial parts of A. cucullata that were gathered from the Ulaş region of Sivas, Turkey, according to prior research [12].
In the current research, the effects of A. cucullata leaf and flower extracts on the proliferation of MCF-7 and HepG2 were evaluated using the MTT assay, which is a common instrument for screening the cytotoxic or proliferative effects of plant extracts [38]. The MTT test findings showed a dose- and time-dependent reduction in MCF-7 and HepG2 cell viability as compared to untreated cells. The leaf extract caused IC50 values of 65 ± 3.13 μg/mL for MCF-7 and 45.27 ± 1.18 μg/mL for HepG2 cells. Flower extract had IC50 values of 40.35 ± 2.46 and 32.43 ± 3.56 μg/mL in MCF-7 and HepG2 cells, respectively. The apoptosis analysis validated these results. Caspase 3, 8, and 9 activities were significantly greater in cells treated with A. cucullata leaf or flower extracts compared to the control group. Furthermore, treated cells showed lower levels of the anti-apoptotic genes Bcl-xL and Bcl-2 than untreated controls. This demonstrates that both medicines cause apoptosis in cancer cells, which contributes to their deadly effects. Our findings were consistent with prior research on the toxicity of A. teretifolia Willd on post-cancer cell lines (DU145 and PC-3) and healthy human gingival fibroblast (HGF) cells. A. teretifolia extracts only showed cytotoxicity in DU145 and PC-3 cells. The methanol extract decreased cancer cell viability in DU145 cells in a dose-dependent manner, with determined IC50 values of 0.40 ± 0.05 mg/mL and 0.14 ± 0.04 mg/mL for 24 and 48 h, respectively. Furthermore, in prostate cancer cells, the levels of mRNA expression of the bax and caspase-3 genes were considerably up-regulated (p < 0.05), companies with the expression of bcl-2 were down-regulated (p < 0.05), whereas the extracts had no cytotoxic influence and caused apoptosis in HGF cells [39]. These investigations, as well as our findings, demonstrated that A. cucullata has therapeutic potential in cancer cells, as shown by dose-dependent cytotoxicity and apoptosis.
Agar diffusion methods are commonly used to test the antimicrobial activity of plant extracts, although this approach has limitations due to extracts having unclear components, which may result in false positive and negative findings [40]. In this study, the antibacterial activity of A. cucullata leaf and flower methanol extracts were assessed using a serial dilution technique in 96-well microplates. A. cucullata leaf and flower methanol extract significantly inhibited most examined microorganisms as compared to the positive control (ciprofloxacin, 25 μg/mL). The MIC values of the extracts against all the tested microorganisms varied from 3.12 ± 0.00 to 12.50 ± 0.00 μg/mL, and for the leaf extract, from 4.68 ± 2.21 to 25 ± 0.00 μg/mL (Table 1 and Table 2). A prior investigation found high antibacterial activity in 11 Achillea species flower head extracts, with MIC values below 250 μg/mL, supporting current results [41]. Another study found that the ethanolic extracts of A. cucullata aerial parts exhibited slight inhibitory effects against most investigated bacteria (S. aureus, E. coli, P. aeruginosa, and E. faecalis), with MIC values greater than 5 mg/mL [12].
We acknowledge the shortcomings and limitations in terms of the methodology we used in our present study. Two-Dimensional Gas Chromatography (GCxGC) dual-capillary polar and polar columns are needed to study complex mixtures. The retention indices and absolute concentration of the components should be calculated concerning the retention indices of a series of n-alkanes (two standard mixes, C8–C20 and C21–C40) using linear interpolation [42]. A further weakness of the study is the absence of in vivo examinations. In vivo studies are critical to supplementing in vitro data, especially if plant extracts exhibit potential biological effects against pathogenic bacteria/fungi and anti-proliferative activity against cell lines. The in vivo environment is far more complicated in terms of target organ delivery, efficacy, and possible adverse effects. Our group intends to go a step further and employ animal models to preclinically investigate the bioactivities of the A. cucullata leaf and flower extracts.
5. Conclusions
The complete GC/MS study of A. cucullata leaf and flower extracts showed a wide spectrum of phytochemical substances, including carvacrol, a TBDMS derivative; 2-Myristynoyl-glycinamide and acetylaminobenzothiazol-2-yl)-2-(adamantan-1-yl); and Isolongifolol; followed by (3E,10Z)-Oxacyclotrideca-3,10-diene-2,7-dione and others, underlining the extract’s potential for antibacterial and anticancer applications. A. cucullata leaf and flower extracts demonstrated antibacterial activity, supporting their prospective application as antibacterial agents. Furthermore, their anticancer actions showed enhanced caspase activity and reduced anti-apoptotic gene expression in treated cells, indicating apoptosis. In comparison to the leaf extracts, the A. cucullata flower extract exhibited increased TPC and TFC. Notably, the flower extract also demonstrated a somewhat stronger cytotoxic and antibacterial effect against both cell lines compared to the leaf extract. Overall, the research shows that A. cucullata leaf and flower extracts have a wide range of applications as natural antibacterial and cancer treatments. The revealed bioactivities warrant further investigation into the mechanisms of action and possible therapeutic applications of these compounds, both individually and in combination. Future research should concentrate on in vivo studies to assess the effectiveness and safety of these substances.
Author Contributions
Conceptualization, M.A.B. and I.M.A.; methodology, I.M.A.; software M.A.B.; validation, M.A.B. and I.M.A.; formal analysis, M.A.B.; investigation, I.M.A.; resources, M.A.B.; data curation, M.A.B.; writing—original draft preparation, I.M.A.; writing—review and editing, M.A.B.; visualization, M.A.B.; supervision, M.A.B.; project administration, M.A.B.; funding acquisition, M.A.B. All authors have read and agreed to the published version of the manuscript.
Funding
The authors thank the Researchers Supporting Project Number (RSPD2024R637), King Saud University, Riyadh, Saudi Arabia.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Selwal, N.; Rahayu, F.; Herwati, A.; Latifah, E.; Suhara, C.; Suastika, I.B.K.; Mahayu, W.M.; Wani, A.K. Enhancing secondary metabolite production in plants: Exploring traditional and modern strategies. J. Agric. Food Res. 2023, 14, 100702. [Google Scholar] [CrossRef]
- Marchev, A.S.; Yordanova, Z.P.; Georgiev, M.I. Green (cell) factories for advanced production of plant secondary metabolites. Crit. Rev. Biotechnol. 2020, 40, 443–458. [Google Scholar] [CrossRef]
- Osman, A.K.E.; Abdein, M.A.E.-H. Floristic diversity of Wadi Ar’ar, Saudi Arabia. J. Taibah Univ. Sci. 2019, 13, 772–789. [Google Scholar] [CrossRef]
- Palombo, E.A.; Semple, S.J. Antibacterial activity of traditional Australian medicinal plants. J. Ethnopharmacol. 2001, 77, 151–157. [Google Scholar] [CrossRef] [PubMed]
- Elshamy, A.; Abd-ElGawad, A.; Mohamed, T.; El Gendy, A.E.N.; Abd El Aty, A.A.; Saleh, I.; Moustafa, M.F.; Hussien, T.A.; Pare, P.W.; Hegazy, M.E.F. Extraction development for antimicrobial and phytotoxic essential oils from Asteraceae species: Achillea fragrantissima, Artemisia judaica and Tanacetum sinaicum. Flavour Fragr. J. 2021, 36, 352–364. [Google Scholar] [CrossRef]
- Abd-ElGawad, A.M.; Ahmed, R.F.; Elshamy, A.I.; Sadek, E.G.; Assaeed, A.M.; Bonanomi, G.; El Gendy, A.E.-N.G.; El-Amier, Y.A. Achillea fragrantissima Essential Oil, Wild Grown in Saudi Arabia and Egypt: Detailed Comparative Chemical Profiling, and Evaluation of Allelopathic, Antioxidant, and Antibacterial Activities. Chemistry 2023, 5, 2347–2361. [Google Scholar] [CrossRef]
- Elsharkawy, E.R.; Alghanem, S.M.; Elmorsy, E. Effect of habitat variations on the chemical composition, antioxidant, and antimicrobial activities of Achillea fragrantissima (Forssk) Sch. Bip. Biotechnol. Rep. 2021, 29, e00581. [Google Scholar] [CrossRef]
- Zengin, G.; Aktumsek, A.; Ceylan, R.; Uysal, S.; Mocan, A.; Guler, G.O.; Mahomoodally, M.F.; Glamočlija, J.; Ćirić, A.; Soković, M. Shedding light on the biological and chemical fingerprints of three Achillea species (A. biebersteinii, A. millefolium and A. teretifolia). Food Funct. 2017, 8, 1152–1165. [Google Scholar] [CrossRef]
- El Bouzidi, L.; Abbad, A.; Hassani, L.; Fattarsi, K.; Leach, D.; Markouk, M.; Legendre, L.; Bekkouche, K. Essential oil composition and antimicrobial activity of wild and cultivated Moroccan Achillea ageratum L.: A rare and threatened medicinal species. Chem. Biodivers. 2012, 9, 598–605. [Google Scholar] [CrossRef]
- Toker, Z.; Özen, H.Ç.; Clery, R.A.; Owen, N.E. Essential oils of two Achillea species from Turkey. J. Essent. Oil Res. 2003, 15, 100–101. [Google Scholar] [CrossRef]
- Toncer, O.; Basbag, S.; Karaman, S.; Diraz, E.; Basbag, M. Chemical composition of the essential oils of some Achillea species growing wild in Turkey. Int. J. Agric. Biol. 2010, 12, 527–530. [Google Scholar]
- Eruygur, N.; Koçyiğit, U.; Taslimi, P.; Ataş, M.; Tekin, M.; Gülçin, İ. Screening the in vitro antioxidant, antimicrobial, anticholinesterase, antidiabetic activities of endemic Achillea cucullata (Asteraceae) ethanol extract. S. Afr. J. Bot. 2019, 120, 141–145. [Google Scholar] [CrossRef]
- Wolfe, K.L.; Liu, R.H. Apple peels as a value-added food ingredient. J. Agric. Food Chem. 2003, 51, 1676–1683. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.-C.; Yang, M.-H.; Wen, H.-M.; Chern, J.-C. Estimation of total flavonoid content in propolis by two complementary colorimetric methods. J. Food Drug Anal. 2002, 10, 178–182. [Google Scholar]
- Mosmann, T. Rapid colorimetric assay for cellular growth and survival: Application to proliferation and cytotoxicity assays. J. Immunol. Methods 1983, 65, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Alkhudhayri, A.A.; Wahab, R.; Siddiqui, M.A.; Ahmad, J. Selenium nanoparticles induce cytotoxicity and apoptosis in human breast cancer (MCF-7) and liver (HEPG2) cell lines. Nanosci. Nanotechnol. Lett. 2020, 12, 324–330. [Google Scholar] [CrossRef]
- Al-Dhabi, N.A.; Valan Arasu, M. Quantification of phytochemicals from commercial Spirulina products and their antioxidant activities. Evid.-Based Complement. Altern. Med. 2016, 1, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Binobead, M.A.; Aziz, I.M.; Ibrahim, S.M.; Aljowaie, R.M. Chemical composition and bioactivities of the methanol root extracts of Saussurea costus. Open Chem. 2024, 22, 20240002. [Google Scholar] [CrossRef]
- Al-Dhabi, N.A.; Valan Arasu, M.; Vijayaraghavan, P.; Esmail, G.A.; Duraipandiyan, V.; Kim, Y.O.; Kim, H.; Kim, H.-J. Probiotic and antioxidant potential of Lactobacillus reuteri LR12 and Lactobacillus lactis LL10 isolated from pineapple puree and quality analysis of pineapple-flavored goat milk yoghurt during storage. Microorganisms 2020, 8, 1461. [Google Scholar] [CrossRef]
- Singh, P.; Singh, H.; Kim, Y.J.; Mathiyalagan, R.; Wang, C.; Yang, D.C. Extracellular synthesis of silver and gold nanoparticles by Sporosarcina koreensis DC4 and their biological applications. Enzym. Microb. Technol. 2016, 86, 75–83. [Google Scholar] [CrossRef]
- Basri, D.F.; Sandra, V. Synergistic interaction of methanol extract from Canarium odontophyllum Miq. Leaf in combination with oxacillin against methicillin-resistant Staphylococcus aureus (MRSA) ATCC 33591. Int. J. Microbiol. 2016, 1, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Gabrielson, J.; Hart, M.; Jarelöv, A.; Kühn, I.; McKenzie, D.; Möllby, R. Evaluation of redox indicators and the use of digital scanners and spectrophotometer for quantification of microbial growth in microplates. J. Microbiol. Methods 2002, 50, 63–73. [Google Scholar] [CrossRef] [PubMed]
- Veiga, A.; Maria da Graça, T.T.; Rossa, L.S.; Mengarda, M.; Stofella, N.C.; Oliveira, L.J.; Gonçalves, A.G.; Murakami, F.S. Colorimetric microdilution assay: Validation of a standard method for determination of MIC, IC50%, and IC90% of antimicrobial compounds. J. Microbiol. Methods 2019, 162, 50–61. [Google Scholar] [CrossRef] [PubMed]
- Aljeldah, M.M.; Yassin, M.T.; Mostafa, A.A.-F.; Aboul-Soud, M.A. Synergistic Antibacterial Potential of Greenly Synthesized Silver Nanoparticles with Fosfomycin Against Some Nosocomial Bacterial Pathogens. Infect. Drug Resist. 2022, 16, 125–142. [Google Scholar] [CrossRef] [PubMed]
- Aati, H.; El-Gamal, A.; Shaheen, H.; Kayser, O. Traditional use of ethnomedicinal native plants in the Kingdom of Saudi Arabia. J. Ethnobiol. Ethnomed. 2019, 15, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ullah, R.; Alqahtani, A.S.; Noman, O.M.; Alqahtani, A.M.; Ibenmoussa, S.; Bourhia, M. A review on ethno-medicinal plants used in traditional medicine in the Kingdom of Saudi Arabia. Saudi J. Biol. Sci. 2020, 27, 2706–2718. [Google Scholar] [CrossRef] [PubMed]
- Additives, E.P.o.; Feed, P.o.S.u.i.A.; Bampidis, V.; Azimonti, G.; Bastos, M.d.L.; Christensen, H.; Durjava, M.; Kouba, M.; López-Alonso, M.; López Puente, S.; et al. Safety and efficacy of feed additives consisting of essential oils derived from the flower buds or the leaves of Syzygium aromaticum (L.) Merr. & LM Perry (clove bud oil and clove leaf oils) for all animal species (FEFANA asbl). EFSA J. 2023, 21, e08183. [Google Scholar]
- Hirasawa, K.; Moriya, S.; Miyahara, K.; Kazama, H.; Hirota, A.; Takemura, J.; Abe, A.; Inazu, M.; Hiramoto, M.; Tsukahara, K. Macrolide antibiotics exhibit cytotoxic effect under amino acid-depleted culture condition by blocking autophagy flux in head and neck squamous cell carcinoma cell lines. PLoS ONE 2016, 11, e0164529. [Google Scholar] [CrossRef] [PubMed]
- Shahriar, S.; Shermin, S.A.; Hasnat, H.; Hossain, F.; Han, A.; Geng, P.; Alam, S.; Mamun, A.A. Chemico-pharmacological evaluation of the methanolic leaf extract of Catharanthus ovalis: GC–MS/MS, in vivo, in vitro, and in silico approaches. Front. Pharmacol. 2024, 15, 1347069. [Google Scholar] [CrossRef]
- Chen, Y.; Ba, L.; Huang, W.; Liu, Y.; Pan, H.; Mingyao, E.; Shi, P.; Wang, Y.; Li, S.; Qi, H. Role of carvacrol in cardioprotection against myocardial ischemia/reperfusion injury in rats through activation of MAPK/ERK and Akt/eNOS signaling pathways. Eur. J. Pharmacol. 2017, 796, 90–100. [Google Scholar] [CrossRef]
- Bansal, A.; Saleh-E-In, M.M.; Kar, P.; Roy, A.; Sharma, N.R. Synthesis of carvacrol derivatives as potential new anticancer agent against lung cancer. Molecules 2022, 27, 4597. [Google Scholar] [CrossRef] [PubMed]
- Fan, K.; Li, X.; Cao, Y.; Qi, H.; Li, L.; Zhang, Q.; Sun, H. Carvacrol inhibits proliferation and induces apoptosis in human colon cancer cells. Anti-Cancer Drugs 2015, 26, 813–823. [Google Scholar] [CrossRef] [PubMed]
- Sayuti, M.; Putri, W.D.R.; Yunianta, Y. Antioxidant Activity and Identification of Compounds in the Extract of Sea Bamboo’s (Isis hippuris) Outer Layer. Res. J. Pharm. Biol. Chem. Sci. 2017, 8, 884. [Google Scholar]
- Miyazawa, M.; Sakata, K.; Ueda, M. Microbial transformation of (−)-isolongifolol by plant pathogenic fungus Glomerella cingulata. J. Oleo Sci. 2010, 59, 243–246. [Google Scholar] [CrossRef] [PubMed]
- Jamal, R.K.; Jose, V. Determination of phytochemicals by GC-MS in methanol extract of Elephantopus scaber L. J. Pharmacogn. Phytochem. 2017, 6, 807–813. [Google Scholar]
- Chandra, P.; Sharma, R.K.; Arora, D.S. Antioxidant compounds from microbial sources: A review. Food Res. Int. 2020, 129, 108849. [Google Scholar] [CrossRef] [PubMed]
- Ullah, A.; Munir, S.; Badshah, S.L.; Khan, N.; Ghani, L.; Poulson, B.G.; Emwas, A.-H.; Jaremko, M. Important flavonoids and their role as a therapeutic agent. Molecules 2020, 25, 5243. [Google Scholar] [CrossRef] [PubMed]
- Boncler, M.; Różalski, M.; Krajewska, U.; Podsędek, A.; Watala, C. Comparison of PrestoBlue and MTT assays of cellular viability in the assessment of anti-proliferative effects of plant extracts on human endothelial cells. J. Pharmacol. Toxicol. Methods 2014, 69, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Bali, E.B.; Açık, L.; Elçi, P.; Sarper, M.; Avcu, F.; Vural, M. In vitro anti-oxidant, cytotoxic and pro-apoptotic effects of Achillea teretifolia Willd extracts on human prostate cancer cell lines. Pharmacogn. Mag. 2015, 11, S308. [Google Scholar]
- Klančnik, A.; Piskernik, S.; Jeršek, B.; Možina, S.S. Evaluation of diffusion and dilution methods to determine the antibacterial activity of plant extracts. J. Microbiol. Methods 2010, 81, 121–126. [Google Scholar] [CrossRef]
- Karaalp, C.; Yurtman, A.N.; Karabay Yavasoglu, N.U. Evaluation of antimicrobial properties of Achillea L. flower head extracts. Pharm. Biol. 2009, 47, 86–91. [Google Scholar] [CrossRef]
- Van Den Dool, H.; Kratz, P.D. A generalization of the retention index system including linear temperature programmed gas-liquid partition chromatography. J. Chromatogr. A 1963, 11, 463–471. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).